Abstract
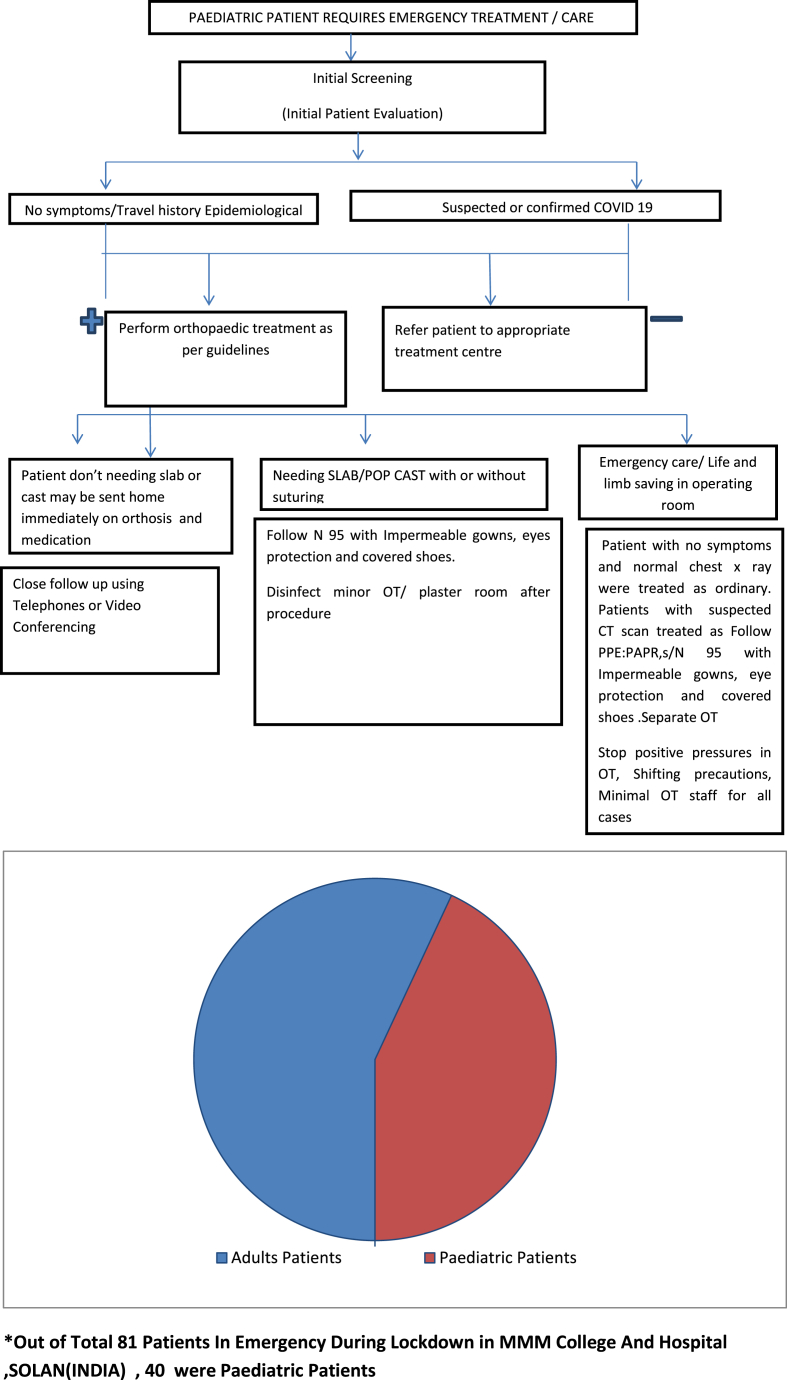
The recent spread of severe acute respiratory syndrome coronavirus (SARS-CoV2) and its associated coronavirus disease has gripped the entire international community and has caused widespread public health concerns due to the unavailability of treatment to this deadly disease. The COVID -19 has affected healthcare workers badly in the world with front line health care providers has a mortality rate of 1.4%. But in countries like Italy, it has gone up to 9%. To this date, there are no universal guidelines for musculoskeletal (MSK) care in the face of the coronavirus pandemic. Health care professionals, including orthopedic surgeons may encounter patients with suspected or confirmed COVID -19 infections and will have to act diligently not only to provide care but at the same time to prevent the spread of infection. During the lockdown period in INDIA we collected data of patients who came to an emergency in our hospital. Out of 81 patients, 40 patients were of pediatric trauma with a percentage of 49% making it highly significant. Thus, in this article, we tried to summarize current recommendations and our institutional guidelines for diagnosing and managing a pediatric orthopedic patient in the COVID-19 pandemic.
Keywords: Covid-19, Paediatricorthopaedic, COVID 19, SARS-CoV2
1. Introduction
The flare-up of coronavirus illness 2019 (COVID-19) in the region of Wuhan, China has advanced quickly into a public health crisis1 and has spread exponentially to different parts of the world.2 The coronavirus belongs to a group of single-stranded RNA viruses known as Coronaviridae.3 This group of virus spread infections; which are known to be zoonotic (transmitted from creatures to people). These incorporate extreme intense respiratory disorder coronavirus (SARS-CoV), first distinguished in 2002, and later after ten years recognized as Middle East respiratory disorder coronavirus (MERS-CoV),.4 As the distributed genome succession for this novel coronavirus has a nearby similarity with other beta-coronaviruses, for example, SARS-CoV and MERS-CoV, the Coronavirus Study Group of the International Committee on Taxonomy of Viruses have given it the logical and scientific name as SARS-CoV-2, despite this fact it is famously called the COVID-19 virus.5,6
The transmission characteristics of COVID-19 are as follows.
-
1.
Infection sources- The main sources of infection are patients infected by COVID-19 with or without clinical symptoms. The incubation period is between 1 and 14 days, with a median incubation period of 3 days and a maximum of 24 days.7
-
2.
Transmission route- The novel virus is spread through direct contact (with an infected person) or indirect contact(with surfaces in the immediate environment or with objects used on an infected person), Droplet transmission (eg respiratory droplets when patients cough, sneeze and talk loudly.), Airborne transmission.
Given the boundless transmission of SARS-CoV-2 and reports of its spread to health care services providers4,8; they are at high risk for this virus contamination and can become potential bearers of the infection. These dangers can be ascribed to the special idea of intercessions, which incorporate patient examination, surgical interventions, and proximity of the health care provider to the patient. So if adequate precautions are not taken, OPD(outpatient department) and OR(operating room) can potentially expose patients as well as health care providers to cross - contaminations.
The COVID −19 has effected badly on healthcare workers in the world and front line health care providers have a mortality rate of 1.4%. But in countries like Italy, it has gone up to 9%.9 PUNE[ a metro city INDIA] faced an outbreak of COVID -19 due to the operation of an orthopedic trauma case,10 which became symptomatic after surgery.
Data of patients have been collected from the orthopedic emergency of our institute in this lockdown period, Out of 81 patients, 40 patients were of pediatric trauma with a percentage of 49% making it a significant. Children may have mild clinical symptoms after infection.11 Nevertheless, medical personnel still need to pay more attention, closely monitor, and strive for early identification and timely treatment. So in this article we tried to summarize the outline in the manner which helps and direct us to make pediatric orthopedic patient care safer for everyone.
2. Literature consensus with review
During COVID 19 pandemic in INDIA [from 25 march to 25 May 2020], we collected data of patients who came to our hospital for an orthopedic emergency. Out of 40 patients, 9 patients were needed operative intervention. Though there was no symptom or sign suggestive of COVID-19 in any of the cases but we made guidelines for treating pediatric emergency cases after consulting relevant national authority and took guidance from the advisory group to prevent further cross-contamination as there are reports of false -negative Covid-19 test.12 We also reference guidelines of BRITISH13 and INDIAN ORTHOPAEDIC ASSOCIATION.14 All patients were discharged asymptomatic with no COVID positive cases detected in our area.
Guidelines were made with an aim-
-
1.
To protect medical staff, paramedical and supporting staff (high -risk subjects) from cross-infection
-
2.
Indications for hospitalization and emergency surgical intervention should be strictly controlled; the elective procedure was not allowed.
-
3.
Decrease hospitalization days by proper pre-operative planning to prevent Intraoperative complications
-
4.
Minimal invasive procedures were integrated to prevent exposure and reduce hospitalization stay.
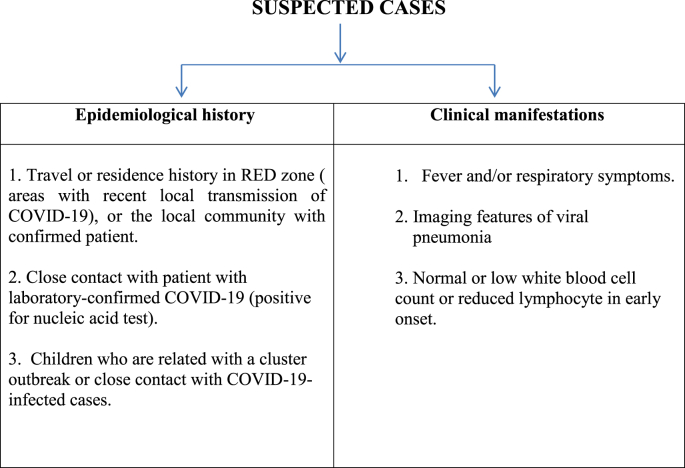
Principal of first contact and clinic
Based on the above information the paramedical support staff (with N95 mask, disposable gown, and sanitization) in emergency service measured patients' temperature and ask epidemiological history, fever, respiratory symptoms at first, filled the epidemiological survey, and make a record about children and their accompanying guardians’ identity card information, containing contact number, address and possible close contact with SARS-CoV-2 carriers after they passing the incubation period. After initial screening patients with suspected, confirmed, or a history of COVID-19 infection referred to appropriate treatment centres with COVID 19 treatment facility. Normal patients (unsuspected) were sent for orthopedic consultation.
Guidelines for orthopedic consultation are as follows-
|
NON−OPERATIVE MANAGEMENT
|
In the plaster room or while doing primary suturing, there should be one surgeon, nursing officer, and supporting staff. The patient should wear a face mask always while the medical team should wear a gown(non disposable), N 95 mask, face shield, cap, and latex gloves. Minor OT and plaster room should be disinfected after the procedure. For patients needing operative procedure and hospitalization should follow below guidelines.
OPERATIVE MANAGEMENT -1
Most children who require operative management may have surgery as a day care procedure are
|
OPERATIVE MANAGEMENT -2
The small number of patients require inpatient treatment with anesthesia and operative management
|
PREOPERATIVE WORKUP
|
As reference if CT findings are positive, one should go for formal RT-PCR even if asymptomatic; and if RT/PCR findings are negative with negative history, one can proceed as with normal OT precautions. But N95 mask/tape sealed surgical mask with face shield & waterproof gowns/waterproof aprons must in all aerosol-generating procedures, irrespective of Covid-19 status during a pandemic.
| HOW TO PLAN OT LIST |
|---|
|
|
|
|
|
|
| Intraoperative consideration |
|
|
|
|
|
|
| Post-operative considerations |
|
|
|
|
|
| OT and instruments cleaning |
|
|
|
|
|
4. Discussion and conclusion
The unrestrained spread of highly contagious SARS-CoV-2 worldwide increases the likelihood that all health care professionals will encounter this subset of the patient population. Universal precautions are required to minimize the spread of this virus as well as we have to save our resources for the management of COVID- 19 confirmed cases in the future. As presented in this article, we have come across a higher amount of pediatric trauma cases as compare to other cases due to the playful nature of children even during restrictions and lockdown. There is no literature available on COVID-19 in the pediatric age group but in this scenario we aim to triage priority cases to prevent future deformity as well as to save young age group and health care providers from cross-infection.
As mentioned above, we followed guidelines by BRITISH and INDIAN ORTHOPAEDIC ASSOCIATION and modified them to manage 40 pediatric emergencies in our hospital (Table 1).
Table 1.
Shows protocol for managing paediatric cases in COVID-19 pandemic era.2
First we took a detailed history of fever, cough, breathlessness, and other things relevant to COVID-19 to find out suspected cases. None of our patients had any sign suggestive of COVID-19 Than we triaged 9 cases for operative intervention. After admission to the ward, we advised a chest x-ray with other relevant investigations. Patients with normal x-ray were treated a normal case but we used N 95 mask, face shield, and normal disposable gown as per guidelines. As in our setup, there is no COVID-19 rapid test kit available, so we did a CT screening of children with suspected X -ray findings. Patients with abnormal findings were operated following full precaution with PPE kit in the separate Operative room. By following these protocols, we were able to manage these cases efficiently. These guidelines may help in the management of emergency cases in a set up where the COVID 19 test facility is not available and there is minimal availability of PPE kits.
Current recommendations suggest surgeons worldwide to defer elective treatment for the next four weeks and focus on emergency care to preserve resources. As there is a surge in the number of COVID-19 cases, this deferment might be extended until we get definitive treatment of this infection. Therefore, to help surgeons during this period, we have put together a set of recommendations for the management of pediatric emergencies and MSK care. It is advisable to assess the emergencies on a case-by-case basis and use clinical judgment to aid in decision making.
Orthopedic surgeons are in a unique circumstance as they may be called upon for the assessment and management of any trauma patients with pain and swelling. And there is a probability that anyone might treat some of the patients with asymptomatic COVID-19 infections since the incubation period can range from 0 to 24 days and most patients only develop mild symptoms. These days every patient should be considered as potentially infected by this virus, and all treatment practices need to review their infection control policies. Health care providers must keep themselves up-to-date about this evolving disease and provide adequate training to their team to promote many levels of screening and preventive measures, allowing essential care to be provided while mitigating the spread of this viral infection.
In conclusion, health care professionals have the obligation to protect the public and maintain high standards of care and infection control. So precautions are necessary that include careful pre-screening of patients and additional measures for the treatment of patients with suspected COVID-19 if deemed necessary. In our set up we treated patients with abnormal CT findings as suspected COVID 19 positive and treated with full PPE precaution and separate OT. While all other patients were treated as normal and were treated in the same guideline advised by various Orthopaedic associations. Above mentioned guideline helps to give efficient and resource-saving management to each patient as well to control cross-infection.
Source of funding
My on foundation for literature grant
CRediT authorship contribution statement
Amit Lakhani: Writing - original draft, Conceptualization, Methodology. Ena Sharma: Writing - review & editing, Supervision, Visualization.
Declaration of competing interest
Yes, first author and second author both received literature grant from my on foundation.
Acknowledgements
The publication (ON project number-20-050) was supported by a literature grant from the ON Foundation Kapellplatz 1 | Switzerland- CH-6004 Lucerne.
Contributor Information
Amit Lakhani, Email: dramitlakhani@gmail.com.
Ena Sharma, Email: dr.sharma_ena@yahoo.co.in.
References
- 1.Centres for Disease Control and Prevention. Transmission of Coronavirus Disease 2019 (COVID-19). (Accessed 18 March, 2020) Available at:: https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html.
- 2.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gorbalenya A.E., Baker S.C., Baric R.S. The species Severe acute respiratory syndrome related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbial. 2020 doi: 10.1038/s41564-020-0695-z. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wax R.S., Christian M.D. Practical recommendations for critical care and anaesthesiology team scaring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01591-x. Accessed 18 March, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2019;382:727–733. doi: 10.1056/NEJMoa2001017. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorbalenya A.E. 2020. Severe Acute Respiratory Syndrome-Related Coronavirus – the Species and its Viruses, a Statement of the Coronavirus Study Group. BioRxiv. [DOI] [Google Scholar]
- 7.Wei G., Zhang N., Yu H. 2020. Clinical characteristics of 2019 novel Coronavirus in China. medRxiv. [Google Scholar]
- 8.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.High Proportion of Healthcare Workers with COVID-19 in Italy www.icn.ch›news›high-proportion-healthcare-work.
- 10.Coronavirus: 92 Staffers of Pune Hospital under Quarantine www.livemint.Com › Companies' › News › Coronavirus-.
- 11.Zhonghua Er Ke Za Zhi Recommendations for the diagnosis, prevention and control of the 2019 novel coronavirus infection in children. Soc. Pediatr. Chinese Med. Assoc. Editor. Board, Chin. J. Pediatr. 2020;58:E004. doi: 10.3760/cma.j.issn.0578-1310.2020.0004. [DOI] [PubMed] [Google Scholar]
- 12.Xiao Ai Tang, Tong Yi Xing. False-negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J Med Virol. 2020 April 9 doi: 10.1002/jmv.2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.https://www.boa.ac.uk/resources/covid-19-boasts-combined.html
- 14.www.ioaindia.org
- 15.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases Published Onlineaheadofprint,2020Feb26. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lei S. EClinicalMedicine; 2020. Clinical Characteristics and Outcomes of Patients Undergoing Surgeries during the Incubation Period of COVID-19 infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nathan N. Waste not, want not: the Re-usability of N95 masks Published online Ahead of print, 2020 Mar 31. Anesth Analg. 2020 doi: 10.1213/ANE.0000000000004843. 10.1213/ANE.000000000000484. [DOI] [PMC free article] [PubMed] [Google Scholar]