Abstract
Combination antiprogrammed death 1/programmed death‐ligand 1 Ab and platinum‐based chemotherapy is standard first‐line treatment for advanced non‐small‐cell lung cancer without targetable oncogene alterations. We describe the long‐term safety and efficacy data from a previously reported phase Ib study of nivolumab and chemotherapy. Japanese patients with non‐small‐cell lung cancer were assigned to a treatment arm based on histology and treatment history. Nivolumab (10 mg/kg, i.v.) and chemotherapy (4 arms) were given every 3 weeks: arm A, 4 cycles of cisplatin and gemcitabine (first‐line); arm B, 4 cycles of cisplatin and pemetrexed followed by pemetrexed maintenance therapy (first‐line); arm C, 4‐6 cycles of carboplatin, paclitaxel, and bevacizumab followed by bevacizumab (first‐line); and arm D, docetaxel (second‐ or third‐line). Study treatments were continued every 3 weeks as maintenance therapy until disease progression. Minimum follow‐up period was 57.9 months. Median progression‐free survival (median [range, plus sign indicates censored data]) was 6.3 (0.7+‐47.8), 11.8 (1.4‐65.1+), 40.7 (5.3‐60.8+), and 3.2 (1.9‐10.9) months, and 5‐year progression‐free survival was observed in 0/6, 1/6, 1/6, and 0/6 patients in arms A, B, C, and D, respectively. Median overall survival was 13.2 (11.0‐55.4), 28.5 (14.6‐66.2+), not reached (24.2‐67.4+), and 12.5 (9.8‐16.9) months; the number of patients surviving 5 years were 0/6, 1/6, 4/6, and 0/6 in arms A, B, C, and D, respectively. No unexpected severe adverse events or treatment‐related deaths occurred. Nivolumab and platinum‐based chemotherapy combinations showed long‐term tolerability. A moderate proportion of patients in arm C showed 5‐year progression‐free and overall survival.
Keywords: chemotherapy, combination drug therapy, nivolumab, non‐small‐cell lung cancer, programmed cell death 1 receptor
The 5‐year long‐term safety and efficacy data from a previously reported phase Ib study of nivolumab (10 mg/kg, i.v.) and platinum‐based chemotherapy every 3 weeks in Japanese patients with non‐small‐cell lung cancer showed no unexpected severe adverse events or treatment‐related deaths. A moderate proportion of patients from arm C (first‐line carboplatin, paclitaxel, and bevacizumab; 4‐6 cycles nivolumab) showed 5‐year progression‐free survival and overall survival.

Abbreviations
- AE
adverse event
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- DLT
dose‐limiting toxicity
- EGFR
epidermal growth factor receptor
- ICI
immune‐checkpoint inhibitor
- irAE
immune‐related adverse event
- NSCLC
non‐small‐cell lung cancer
- OS
overall survival
- PD‐1
programmed death 1
- PD‐L1
programmed death‐ligand 1
- PFS
progression‐free survival
- PS
performance status
1. INTRODUCTION
Combination therapies comprising an Ab targeting PD‐1/PD‐L1 and platinum‐based chemotherapy are standard first‐line treatment for patients with advanced NSCLC without targetable oncogene alterations. When first available, anti‐PD‐1/PD‐L1 Abs such as nivolumab, pembrolizumab, and atezolizumab were used as second‐line monotherapy in advanced NSCLC, with better efficacy and safety than docetaxel. 1 , 2 , 3 , 4 Several early‐phase studies 5 , 6 , 7 reported the safety and potency of combination therapy with an anti‐PD‐1/PD‐L1 Ab and platinum‐doublet chemotherapy; randomized phase III studies confirmed the clinical benefits. Progression‐free survival and OS improved when anti‐PD‐1/PD‐L1 (pembrolizumab/atezolizumab) were combined with platinum‐doublet chemotherapy. 8 , 9 , 10 Findings from these trials resulted in the use of combination treatment as the current standard first‐line therapy.
Assessing long‐term efficacy and safety is important to understanding the clinical benefit of treatment including an ICI. The absolute clinical benefit of conventional chemotherapy can be assessed during the stated phase III study period; however, this is not sufficient to evaluate the clinical benefit of treatment including an ICI, because ICIs yield exceptionally long progression‐free and overall survival in a certain proportion of patients. 11 , 12 When treatment including an ICI is compared with conventional chemotherapy, long‐term follow‐up is required to detect durable responses. Similarly, long‐term follow‐up is necessary for safety analyses as irAEs could appear late in the treatment period.
At present, there are limited long‐term safety and efficacy data for combination therapy with an anti‐PD‐1/PD‐L1 Ab and standard platinum‐based chemotherapy. To address this, we report on the long‐term follow‐up data from a published phase Ib study. 5 This single‐center, open‐label study evaluated tolerability, efficacy, and safety data of nivolumab and several types of chemotherapy in patients with advanced NSCLC in Japan.
2. MATERIALS AND METHODS
2.1. Patients
Patients with advanced NSCLC who met the following criteria were eligible: diagnosed as stage IIIB NSCLC without indication for definitive thoracic radiotherapy, stage IV or recurrent NSCLC, age 20 years or older, ECOG PS score of 0 or 1, and measurable lesions as defined by RECIST version 1.1. Patients were excluded if any of the following applied: history of infusion reactions (Ab therapies), current/prior interstitial lung disease or pulmonary fibrosis, coexisting autoimmune disease, or receiving systemic corticosteroids or immune suppressants.
2.2. Study design and treatment
This single‐center, open‐label phase Ib study included 4 treatment arms, with at least 6 patients planned per arm, as described in the prior publication. 5 The study comprised a DLT evaluation phase (cycle 1), an extended treatment phase (cycles 2 to 4‐6), and a subsequent maintenance treatment phase. Nivolumab was given i.v. for 60 minutes before the other chemotherapeutic agents. Selection of the 10 mg/kg dose of nivolumab every 3 weeks was based on results from a Japanese phase I study 13 and pharmacokinetic modeling from a US phase I study. 14
Patients were assigned to an arm based on tumor histology, treatment history, and underlying medical conditions as follows: arm A, chemotherapy‐naïve with either squamous or nonsquamous cancer; arm B, chemotherapy‐naïve with nonsquamous cancer; arm C, chemotherapy‐naïve with nonsquamous cancer and had no episodes of hemoptysis (10 mL/day or more) within 28 days prior to enrollment; and arm D, previously treated with 1 prior chemotherapy including platinum‐doublet or 2 prior chemotherapies including platinum‐doublet and an EGFR or anaplastic lymphoma kinase tyrosine kinase inhibitor and either squamous or nonsquamous cancer.
The study was carried out in accordance with the Declaration of Helsinki and with Good Clinical Practice guidelines and approved by the institutional review board. The study was registered with Japanese Pharmaceutical Information Center Clinical Trials Information (JapicCTI‐132071). All patients provided written informed consent.
2.3. Efficacy assessments
Tumor response was evaluated with computed tomography every 6 weeks according to RECIST version 1.1. The following efficacy end‐points were evaluated: overall response rates, disease control rate, median PFS, the numbers of patients achieving PFS at 3 and 5 years, median OS, and the numbers of patients surviving at 3 and 5 years.
2.4. Tolerability and safety assessments
Dose‐limiting toxicities were evaluated during the first cycle according to the AE criteria described previously. 5 In each treatment arm with 10 mg/kg nivolumab, the number of patients and/or nivolumab dose was adjusted as follows: if 2 or fewer of the 3 patients experienced a DLT, 3 additional patients were enrolled in that arm; if 2 or fewer of the 6 patients experienced a DLT, the treatment arm was considered tolerable; and if 3 or more patients experienced a DLT, a dose reduction of nivolumab to 5 or 2 mg/kg was considered. Adverse events were graded according to the Common Terminology Criteria for AEs version 4.0.
2.5. Programmed death‐ligand 1 immunohistochemistry
Exploratory assessment of tumor PD‐L1 protein expression was undertaken with biopsy specimens collected at the study start (archival or recent). Tissues were evaluated using a PD‐L1 immunohistochemistry 22‐8 pharmDX (Dako) kit (Agilent Technology) at a central laboratory. The PD‐L1 expression scores were calculated from the staining of tumor‐cell membranes at any intensity. We also evaluated the correlation between PD‐L1 protein expression and clinical outcomes.
3. RESULTS
3.1. Patients and treatment
Patients were enrolled between April 2013 and March 2014. Clinical data were collected up to December 2018. Six patients were enrolled in each of the 4 treatment arms. One patient in arm A experienced a DLT (ALT increased, grade 3); 10 mg/kg nivolumab was tolerable in all 4 arms. The minimum follow‐up period was 57.9 months.
Baseline patient characteristics were described previously. 5 Briefly, the median (range) age was 63 (34‐73) years. Seventeen patients (70.8%) were male. There were 19 (79.2%) former and 1 (4.2%) current smoker(s). Eleven (45.8%) and 13 (54.2%) patients had ECOG PS scores of 0 and 1, respectively. Four patients (16.7%; 2 in arm A and 2 in arm D) had squamous cell carcinoma. One patient in arm D (4.2%) had NSCLC not otherwise specified, and the others had adenocarcinoma (79.2%). Four patients (16.7%) had an EGFR mutation (3 in arm B and 1 in arm D).
3.2. Efficacy
Overall response rates were 3/6 (50.0%), 3/6 (50.0%), 6/6 (100%), and 1/6 (16.7%) in arms A, B, C, and D, respectively, with disease control rates in 5/6 (83.3%), 5/6 (83.3%), 6/6 (100%), and 4/6 (66.7%), respectively. The median PFS (range, plus sign indicates censored data) was 6.3 (0.7+‐47.8), 11.8 (1.4‐65.1+), 40.7 (5.3‐60.8+), and 3.2 (1.9‐10.9) months in arms A, B, C, and D, respectively. Three‐year PFS was observed in 1/6, 1/6, 3/6, and 0/6 patients, and 5‐year PFS was observed in 0/6, 1/6, 1/6, and 0/6 patients in arms A, B, C, and D, respectively. The median survival time (range) was 13.2 (11.0‐55.4), 28.5 (14.6‐66.2+), not reached (24.2‐67.4+), and 12.5 (9.8‐16.9) months in arms A, B, C, and D, respectively (Figure 1). The numbers of patients surviving 3 years were 2/6, 2/6, 5/6, and 0/6, and the numbers surviving 5 years were 0/6, 1/6, 4/6, and 0/6 patients, in arms A, B, C, and D, respectively. As of the current data cut‐off, 5 of 24 patients (20.8%) had survived (1 and 4 in arms B and C, respectively), and 1 patient (8.3%) in arm C was continuing study treatment.
FIGURE 1.
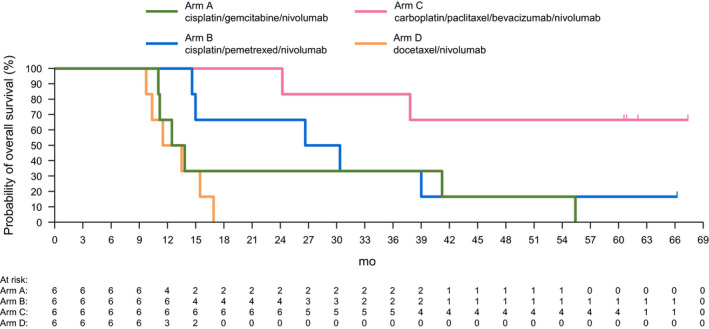
Kaplan‐Meier curves of overall survival among patients with advanced non‐small‐cell lung cancer treated with combinations of nivolumab and chemotherapy (treatment arms A‐D)
Response and treatment duration (arms A, B, C, and D) and treatment delivery with reasons for treatment discontinuation (arms A, B, and C) for each patient are shown in Figures 2 and 3, respectively.
FIGURE 2.
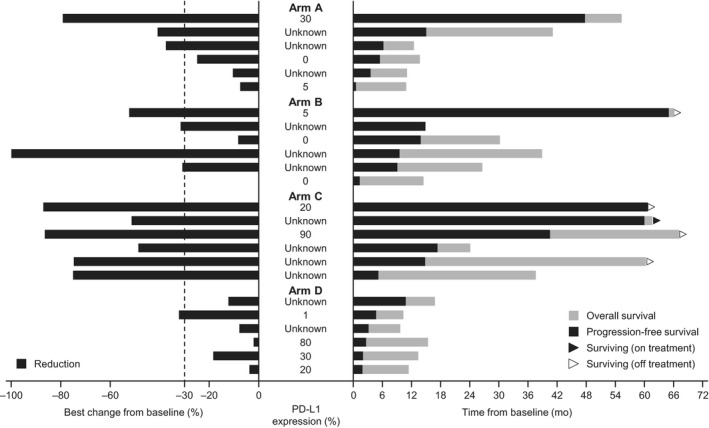
Best response in target lesions from baseline, programmed cell death‐ligand 1 (PD‐L1) expression, and survival outcome of all patients with advanced non‐small‐cell lung cancer treated with combinations of nivolumab and chemotherapy (treatment arms A‐D). Nivolumab (10 mg/kg, i.v.) and chemotherapy were given every 3 weeks: arm A, 4 cycles of cisplatin and gemcitabine (first‐line); arm B, 4 cycles of cisplatin and pemetrexed followed by pemetrexed maintenance therapy (first‐line); arm C, 4‐6 cycles of carboplatin, paclitaxel, and bevacizumab followed by bevacizumab (first‐line); arm D, docetaxel (second‐ or third‐line)
FIGURE 3.
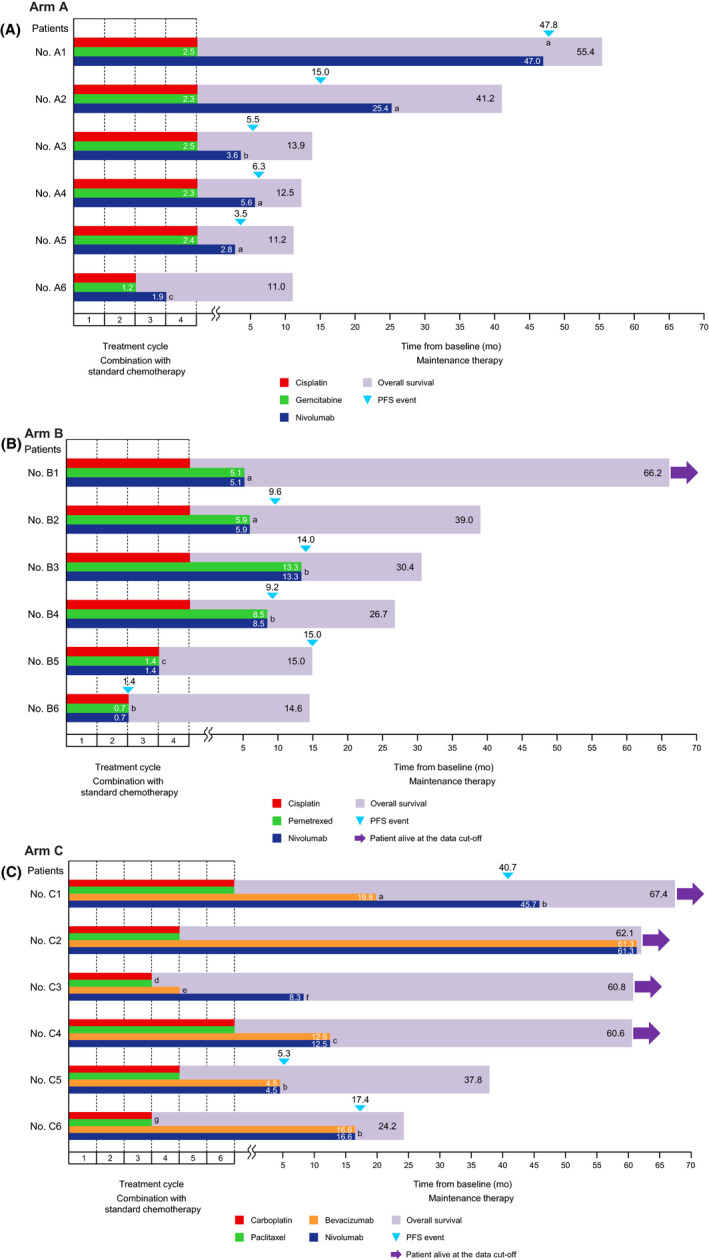
Status of treatment continuation/discontinuation by patient with advanced non‐small‐cell lung cancer assigned to treatment arm (A) A, (B) B, and (C) C. Reason for treatment discontinuation in arm A: a, progressive disease; b, adverse event (AE) (hypophysitis and thyroid disorder); c, AE (allergic reaction). Reason for treatment discontinuation in arm B: a, AE (interstitial lung disease); b, progressive disease; c, AE (depression). Reason for treatment discontinuation in arm C: a, AE (hypertension); b, progressive disease; c, cataract surgery; d, AE (sensory disorder); e, AE (epistaxis), f, AE (interstitial lung disease); g, AE (peripheral sensory neuropathy). PFS, progression‐free survival
3.3. Safety
The 4 treatments were tolerable; DLT was observed in only 1 patient in arm A during the first 3 weeks of the study (the DLT phase). There were no treatment‐related deaths. The incidences of hematological AEs (Table 1) over the length of the study did not change from the incidence observed in the previously reported study period. 5
TABLE 1.
Hematologic toxicities and antiangiogenic adverse events among patients with advanced non‐small‐cell lung cancer treated with nivolumab and chemotherapy
|
Arm A N = 6 |
Arm B N = 6 |
Arm C N = 6 |
Arm D N = 6 |
|||||
|---|---|---|---|---|---|---|---|---|
| Regimen |
Cisplatin Gemcitabine Nivolumab |
Cisplatin Pemetrexed Nivolumab |
Carboplatin Paclitaxel Bevacizumab Nivolumab |
Docetaxel Nivolumab |
||||
| Adverse event | Any grade | Grade 3‐4 | Any grade | Grade 3‐4 | Any grade | Grade 3‐4 | Any grade | Grade 3‐4 |
| Hematologic toxicities | ||||||||
| White blood cell count decreased | 6 (100) | 0 (0.0) | 5 (83.3) | 0 (0.0) | 6 (100) | 3 (50.0) | 6 (100) | 5 (83.3) |
| Neutrophil count decreased | 6 (100) | 1 (16.7) | 5 (83.3) | 1 (16.7) | 6 (100) | 6 (100) | 6 (100) | 6 (100) |
| Lymphocyte count decreased | 4 (66.7) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 4 (66.7) | 1 (16.7) | 5 (83.3) | 3 (50.0) |
| Anemia | 6 (100) | 0 (0.0) | 4 (66.7) | 0 (0.0) | 4 (66.7) | 1 (16.7) | 4 (66.7) | 0 (0.0) |
| Platelet count decreased | 6 (100) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 6 (100) | 2 (33.3) | 0 (0.0) | 0 (0.0) |
| Antiangiogenic adverse events | ||||||||
| Hypertension | 1 (16.7) | 0 (0.0) | 1 (16.7) | 1 (16.7) | 4 (66.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Proteinuria | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 1 (16.7) | 0 (0.0) |
| Epistaxis | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (66.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Data are presented as n (%), with n referring to the number of events.
Patients with irAEs and those receiving systemic corticosteroid therapy are shown in Table 2; the time to onset of first irAEs is shown in Figure 4 by arm, across all patients, and across arms A, B, and C combined. Forty‐six irAEs were observed in 21 of 24 (87.5%) patients. Hepatic irAEs were observed in 13 patients (4, 3, 3, and 3 in arms A, B, C, and D, respectively), and systemic corticosteroid therapy was given to 1 patient in arm A. Interstitial lung disease was reported in 3 patients (2 in arm B and 1 in arm C), and these patients were treated with systemic corticosteroids. Renal irAEs were observed in 2 patients (1 in arm B and 1 in arm C) and none required systemic corticosteroids. Skin irAEs, all less than grade 3 in severity, appeared in 13 patients (2, 4, 5, and 2 in arms A, B, C, and D, respectively). One patient in arm C required systemic corticosteroid therapy. Severe irAEs (grade 3 or higher) were observed in 1 patient in arm A (AST increase, ALT increase) and 1 patient in arm D (AST increase). As AE onset in patients receiving an ICI could theoretically be delayed, the relative timing of select AEs by system organ class, as well as timing of DLTs, is illustrated in Figure 4.
TABLE 2.
Immune‐related adverse events (irAEs) by grade and need for corticosteroid therapy (CS) among patients with advanced non‐small‐cell lung cancer treated with nivolumab and chemotherapy
|
Arm A N = 6 |
Arm B N = 6 |
Arm C N = 6 |
Arm D N = 6 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Regimen |
Cisplatin Gemcitabine Nivolumab |
Cisplatin Pemetrexed Nivolumab |
Carboplatin Paclitaxel Bevacizumab Nivolumab |
Docetaxel Nivolumab |
||||||||
| irAE grade or CS | Any | 3‐4 | CS | Any | 3‐4 | CS | Any | 3‐4 | CS | Any | 3‐4 | CS |
| Any irAE | 6 (100) | 1 (16.7) | 2 (33.3) | 4 (66.7) | 0 (0.0) | 2 (33.3) | 6 (100) | 0 (0.0) | 2 (33.3) | 5 (83.3) | 1 (16.7) | 1 (16.7) |
| Skin toxicity | 2 (33.3) | 0 (0.0) | 0 (0.0) | 4 (66.7) | 0 (0.0) | 0 (0.0) | 5 (83.3) | 0 (0.0) | 1 (16.7) | 2 (33.3) | 0 (0.0) | 0 (0.0) |
| Rash maculopapular | 2 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pruritus | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Rash erythematous | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Rash | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 5 (83.3) | 0 (0.0) | 1 (16.7) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Urticarias | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Gastrointestinal toxicity | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Diarrhea | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Endocrine disorders | 1 (16.7) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Hypophysitis | 1 (16.7) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hypothyroidism | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Blood thyroid‐stimulating hormone decreased | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) |
| Hyperthyroidism | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hepatotoxicity | 4 (66.7) | 1 (16.7) | 1 (16.7) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 1 (16.7) | 0 (0.0) |
| AST increased | 4 (66.7) | 1 (16.7) | 1 (16.7) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 1 (16.7) | 0 (0.0) |
| ALT increased | 4 (66.7) | 1 (16.7) | 1 (16.7) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 0 (0.0) |
| Blood bilirubin increased | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Bilirubin conjugated increased | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pulmonary toxicity | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 2 (33.3) | 1 (16.7) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Interstitial lung disease | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 2 (33.3) | 1 (16.7) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Renal toxicity | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Blood creatinine increased | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hypersensitivity | 2 (33.3) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 0 (0.0) | 1 (16.7) | 2 (33.3) | 0 (0.0) | 1 (16.7) |
| Hypersensitivity | 2 (33.3) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Infusion related reaction | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (33.3) | 0 (0.0) | 1 (16.7) | 2 (33.3) | 0 (0.0) | 1 (16.7) |
Data are presented as n (%).
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase.
FIGURE 4.
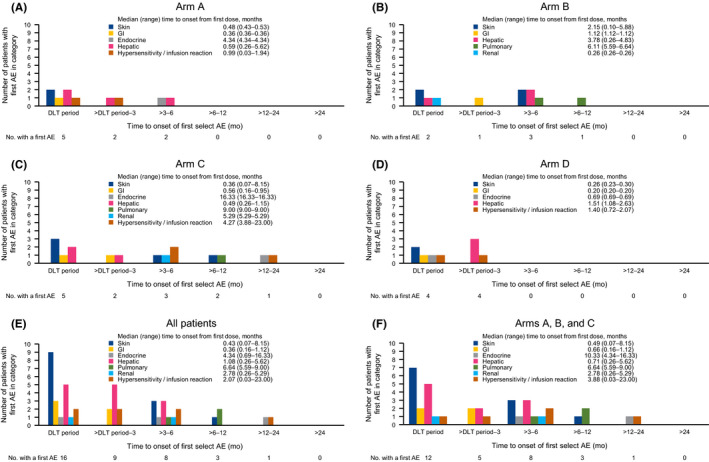
Time to onset of first adverse events (AEs) for patients with advanced non‐small‐cell lung cancer assigned to (A) treatment arm A, (B) arm B, (C) arm C, (D) arm D, (E) all patients, and (F) combined arms A, B, and C. Nivolumab (10 mg/kg, i.v.) and chemotherapy (4 arms) were given every 3 weeks: arm A, 4 cycles of cisplatin and gemcitabine (first‐line); arm B, 4 cycles of cisplatin and pemetrexed followed by pemetrexed maintenance therapy (first‐line); arm C, 4‐6 cycles of carboplatin, paclitaxel, and bevacizumab followed by bevacizumab (first‐line); and arm D, docetaxel (second‐ or third‐line). DLT, dose‐limiting toxicity; GI, gastrointestinal
Hypertension (n = 4, any grade) and proteinuria (n = 2, any grade) were primarily observed in arm C (Table 1).
3.4. Programmed death‐ligand 1 immunohistochemistry
Expression of PD‐L1 in tumor specimens was evaluable in 12 patients (3, 3, 2, and 4 in arms A, B, C, and D, respectively). Correlations between PD‐L1 expression and clinical outcome for each patient are shown in Figures 2 and 5. No clear relationship was observed between tumor PD‐L1 protein expression and clinical outcomes in this study.
FIGURE 5.
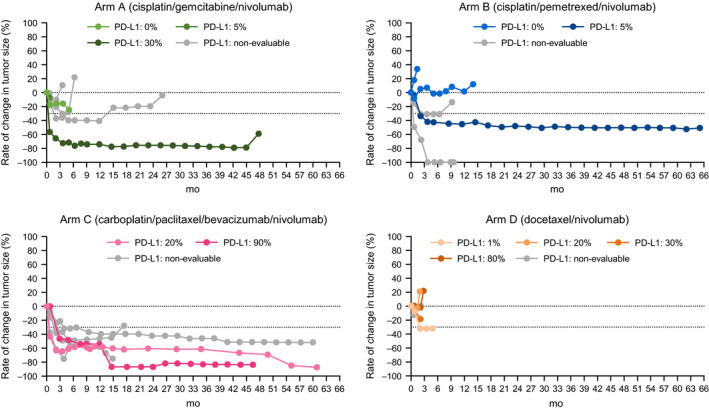
Rate of change in tumor size from baseline in patients with advanced non‐small‐cell lung cancer according to programmed cell death‐ligand 1 (PD‐L1) expression by treatment arm
4. DISCUSSION
In a Japanese phase I trial initiated in 2008, 13 nivolumab monotherapy resulted in successful responses and good tolerability in NSCLC patients. Based on this, the present phase I combination trial of nivolumab and standard chemotherapy was initiated in 2013 in NSCLC patients to confirm whether combination treatment would be a viable treatment option. The 3 combination therapies of nivolumab and platinum‐based chemotherapy reported in the present study were tolerable based on these long‐term observations. No additional safety concerns were noted in the timeframe between the previous report and the present study. Hematological toxicities occurred at a frequency consistent with that reported previously. 5 Given the possibility that immune‐related events occur late after treatment with ICIs, it is notable that most irAEs occurred within 6 months of the protocol treatment; few irAEs, none severe, were observed more than 6 months after treatment start. Hypertension and proteinuria primarily occurred in arm C, a treatment arm with bevacizumab, in line with previous reports of bevacizumab treatment. 15 Hepatic irAEs were observed in 13 patients, but only 1 required systemic corticosteroid therapy (arm A). Renal irAEs were observed in 2 patients; these events were mild. We acknowledge the potential of renal irAEs requiring systemic corticosteroid therapy, which has been reported in other clinical studies evaluating anti‐PD‐1/PD‐L1 Ab. Pulmonary, hepatic, and renal toxicities could arise due to the combined use of platinum‐doublet chemotherapy and anti‐PD‐1/PD‐L1 Ab; however, most other AEs do not overlap between these 2 therapies. No irAEs were observed for more than 24 months after the first dose of nivolumab; however, this result is limited by the small number of patients who continued nivolumab treatment for more than 24 months.
Long PFS and OS were observed in several patients who received combination treatment of nivolumab and platinum‐doublet chemotherapy in the first‐line setting, despite the small sample size. Recent studies of combination therapy (anti‐PD‐1/PD‐L1 Ab and platinum‐based chemotherapy) in patients with treatment‐naïve advanced NSCLC showed improvements in PFS and OS compared with chemotherapy alone. 8 , 9 , 10 However, these pivotal phase III studies were too immature to describe long‐term efficacies; the median follow‐up periods were 10.5 months in KEYNOTE‐189 (pembrolizumab plus platinum/pemetrexed), 8 15.4‐15.5 months in IMpower150 (atezolizumab plus carboplatin/paclitaxel/bevacizumab), 9 and 7.8 months in KEYNOTE‐407 (pembrolizumab plus carboplatin/paclitaxel or nab‐paclitaxel). 10 Results for KEYNOTE‐021 Cohort G (phase I/II study to evaluate pembrolizumab plus carboplatin and pemetrexed) were reported with a median follow‐up period of 23.9 months. 16 However, time to onset of irAEs with long‐term follow‐up was not reported. In comparison, the present study reported a long‐term follow‐up of over 57.9 months, allowing for the observation of 5‐year PFS and survival in patients with advanced NSCLC treated with an anti‐PD‐1/PD‐L1 Ab and platinum‐doublet chemotherapy.
We did not observe a combination effect for nivolumab and docetaxel in the second‐ or third‐line setting (arm D). The benefits of combined anti‐PD‐1/PD‐L1 Ab and chemotherapy, such as docetaxel, are still unclear; further clinical studies to evaluate this setting are warranted.
Carboplatin/paclitaxel/bevacizumab plus nivolumab showed the highest response rate of the 3 arms in the first‐line setting, and had a relatively large number of patients with 5‐year PFS and 5‐year survival, although the inclusion of patients for whom bevacizumab treatment is indicated could have resulted in the selection of patients with a better prognosis. Antivascular endothelial growth factor agents such as bevacizumab might encourage clinical efficacies of chemotherapy and anti‐PD‐1/PD‐L1 Ab by decreasing immunosuppressive cytokines, inhibiting immunosuppressive cells, and improving tumor delivery of cytotoxic agents, nivolumab, and lymphocytes. 17 , 18 However, the sample size of this study was insufficient to evaluate clinical efficacy. Our observations are hypothesis‐generating and should be further explored in additional trials. A randomized phase III study (NCT03117049) to confirm the benefits of nivolumab combined with carboplatin/paclitaxel/bevacizumab is ongoing in East Asia.
Although IMpower150 reported the survival benefit of adding atezolizumab to carboplatin/paclitaxel/bevacizumab, the risk reduction of death was modest and long‐term survival efficacy remains unknown. We expected better clinical efficacy with anti‐PD‐1 Ab (nivolumab) plus carboplatin/paclitaxel/bevacizumab than anti‐PD‐L1 based on the strength of preclinical findings and previously described clinical studies. Preclinical studies indicated that combined PD‐L1/PD‐L2 blockade on dendritic cells augmented T cell proliferation and cytokine production more effectively than PD‐L1 blockade alone, 19 and that anti‐PD‐1 Abs might be more effective, by blocking the interaction between PD‐1 and both PD‐L1/PD‐L2, than anti‐PD‐L1 Abs, which only block the PD‐1/PD‐L1 interaction. 20
In conclusion, the combination therapy of nivolumab and platinum‐based chemotherapy was tolerable and safe when assessed over a long term and showed long‐term efficacy in a subset of patients. No new or incremental safety concern was observed in any of the study arms. The regimen of nivolumab plus platinum‐based chemotherapy, especially the combination of carboplatin/paclitaxel/bevacizumab and nivolumab, could be promising because of the observed reduction in risk of death and improved long‐term survival rates.
DISCLOSURE
S. Kanda has received research funds from AstraZeneca, Bristol‐Myers Squibb, Ono Pharmaceutical, and MSD, and lecture fees, honoraria, or other fees from AstraZeneca, Bristol‐Myers Squibb, and Ono Pharmaceutical. Y. Ohe has received research funds from AstraZeneca, Bristol‐Myers Squibb, Ono Pharmaceutical, MSD, and Chugai Pharmaceutical, and lecture fees, honoraria, or other fees from AstraZeneca, Ono Pharmaceutical, and Chugai Pharmaceutical. Y. Goto has received research funds from Eli Lilly, Taiho Pharmaceutical, Ono Pharmaceutical, Bristol‐Myers Squibb, Pfizer, Novartis, Kyorin, Chugai Pharmaceutical, AbbVie, Daiichi Sankyo, and Guardant Health, and lecture fees, honoraria, or other fees from AstraZeneca, Boehringer Ingelheim, and Pfizer. H. Horinouchi has received research funds from Ono Pharmaceutical, MSD, Chugai Pharmaceutical, Bristol‐Myers Squibb, Daiichi Sankyo, AstraZeneca, Novartis, and Genomic Health, and lecture fees, honoraria, or other fees from Eli Lilly, AstraZeneca, MSD, Ono Pharmaceutical, and Bristol‐Myers Squibb. Y. Fujiwara has received lecture fees, honoraria, or other fees from AstraZeneca. H. Nokihara has received research funds from Pfizer, Novartis, Daiichi Sankyo, GlaxoSmithKline, Quintiles, Astellas Pharma, Regeneron, Taiho Pharmaceutical, Eisai, Chugai Pharmaceutical, Eli Lilly, AstraZeneca, Boehringer Ingelheim, Ono Pharmaceutical, and PAREXEL, and lecture fees, honoraria, or other fees from Chugai Pharmaceutical. N. Yamamoto has received research funds from Bristol‐Myers Squibb, Chugai Pharmaceutical, Eisai, Pfizer, Boehringer Ingelheim, Ono Pharmaceutical, Takeda, Astellas, Daiichi Sankyo, Kyowa Kirin, Novartis, Taiho Pharmaceuticals, Bayer, Janssen Pharma, MSD, Merck, AbbVie, and GlaxoSmithKline, and lecture fees, honoraria, or other fees from Sysmex, Bristol‐Myers Squibb, Pfizer, Eli Lilly, Ono Pharmaceutical, Chugai Pharmaceutical, and AstraZeneca. T. Yamamoto has declared personal fees as an employee of Ono Pharmaceutical. T. Tamura has received lecture fees, honoraria, or other fees from Eli Lilly and Chugai Pharmaceutical.
ACKNOWLEDGEMENTS
The authors would like to thank the patients who participated in this study and their families. The authors also would like to thank Helen M Wilfehrt, PhD, and Sarah Bubeck, PhD, of Edanz Medical Writing for providing medical writing services, which were funded by Ono Pharmaceutical Co., Ltd. through EMC, in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). This work was supported by Ono Pharmaceutical Co., Ltd. and Bristol‐Myers Squibb. Ono Pharmaceutical Co., Ltd., provided the study drug and contributed to the study design, data interpretation, and statistical analysis. Bristol‐Myers Squibb was not involved in the conduct of the study or preparation of the manuscript.
Kanda S, Ohe Y, Goto Y, et al. Five‐year safety and efficacy data from a phase Ib study of nivolumab and chemotherapy in advanced non‐small‐cell lung cancer. Cancer Sci. 2020;111:1933–1942. 10.1111/cas.14410
Clinical trial registration: Japanese Pharmaceutical Information Center Clinical Trials Information (JapicCTI)‐132071.
DATA AVAILABILITY STATEMENT
Additional deidentified patient data and supporting documents related to this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous‐cell non‐small‐cell lung cancer. N Engl J Med. 2015;373:123‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Borghaei H, Paz‐Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non‐small‐cell lung cancer. N Engl J Med. 2015;373:1627‐1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Herbst RS, Baas P, Kim D‐W, et al. Pembrolizumab versus docetaxel for previously treated, PD‐L1‐positive, advanced non‐small‐cell lung cancer (KEYNOTE‐010): a randomised controlled trial. Lancet. 2016;387:1540‐1550. [DOI] [PubMed] [Google Scholar]
- 4. Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non‐small‐cell lung cancer (OAK): a phase 3, open‐label, multicentre randomised controlled trial. Lancet. 2017;389:255‐265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kanda S, Goto K, Shiraishi H, et al. Safety and efficacy of nivolumab and standard chemotherapy drug combination in patients with advanced non‐small‐cell lung cancer: a four arms phase Ib study. Ann Oncol. 2016;27:2242‐2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rizvi NA, Hellmann MD, Brahmer JR, et al. Nivolumab in combination with platinum‐based doublet chemotherapy for first‐line treatment of advanced non‐small‐cell lung cancer. J Clin Oncol. 2016;34:2969‐2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non‐squamous non‐small‐cell lung cancer: a randomised, phase 2 cohort of the open‐label KEYNOTE‐021 study. Lancet Oncol. 2016;17:1497‐1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gandhi L, Rodríguez‐Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non‐small‐cell lung cancer. N Engl J Med. 2018;378:2078‐2092. [DOI] [PubMed] [Google Scholar]
- 9. Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first‐line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378:2288‐2301. [DOI] [PubMed] [Google Scholar]
- 10. Paz‐Ares L, Luft A, Vicente D, et al. Pembrolizumab plus chemotherapy for squamous non‐small‐cell lung cancer. N Engl J Med. 2018;379:2040‐2051. [DOI] [PubMed] [Google Scholar]
- 11. Horn L, Spigel DR, Vokes EE, et al. Nivolumab versus docetaxel in previously treated patients with advanced non‐small‐cell lung cancer: two‐year outcomes from two randomized, open‐label, phase III trials (CheckMate 017 and CheckMate 057). J Clin Oncol. 2017;35:3924‐3933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vokes EE, Ready N, Felip E, et al. Nivolumab versus docetaxel in previously treated advanced non‐small cell lung cancer (CheckMate 017 and CheckMate 057): 3‐year update and outcomes in patients with liver metastases. Ann Oncol. 2018;29:959‐965. [DOI] [PubMed] [Google Scholar]
- 13. Yamamoto N, Yamada Y, Nokihara H, et al. Phase I study of ONO‐4538 (BMS‐936558), an anti PD‐1 antibody, in Japanese patients with advanced solid tumors. Ann Oncol. 2012;23:ix152‐ix174,459P. [Google Scholar]
- 14. Brahmer JR, Drake CG, Wollner I, et al. Phase I study of single‐agent anti‐programmed death‐1 (MDX‐1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167‐3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Niho S, Kunitoh H, Nokihara H, et al. Randomized phase II study of first‐line carboplatin‐paclitaxel with or without bevacizumab in Japanese patients with advanced non‐squamous non‐small‐cell lung cancer. Lung Cancer. 2012;76:362‐367. [DOI] [PubMed] [Google Scholar]
- 16. Borghaei H, Langer CJ, Gadgeel S, et al. 24‐month overall survival from KEYNOTE‐021 cohort G: pemetrexed and carboplatin with or without pembrolizumab as first‐line therapy for advanced nonsquamous non‐small cell lung cancer. J Thorac Oncol. 2019;14:124‐129. [DOI] [PubMed] [Google Scholar]
- 17. Roland CL, Lynn KD, Toombs JE, Dineen SP, Udugamasooriya DG, Brekken RA. Cytokine levels correlate with immune cell infiltration after anti‐VEGF therapy in preclinical mouse models of breast cancer. PLoS ONE. 2009;4:e7669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shrimali RK, Yu Z, Theoret MR, Chinnasamy D, Restifo NP, Rosenberg SA. Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res. 2010;70:6171‐6180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hobo W, Maas F, Adisty N, et al. siRNA silencing of PD‐L1 and PD‐L2 on dendritic cells augments expansion and function of minor histocompatibility antigen‐specific CD8+ T cells. Blood. 2010;116:4501‐4511. [DOI] [PubMed] [Google Scholar]
- 20. Umezu D, Okada N, Sakoda Y, et al. Inhibitory functions of PD‐L1 and PD‐L2 in the regulation of antitumor immunity in murine tumor microenvironment. Cancer Immunol Immunother. 2019;68:201‐211. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Additional deidentified patient data and supporting documents related to this study are available from the corresponding author upon reasonable request.


