Abstract
Background and Aims:
Simulation is one of the important learning tools when it comes to skill acquisition and as a supplemental tool for training in high stake situations like COVID-19. The aim of this study is to meet the global requirements of knowledge on ventilatory management, prepare and to evaluate the effectiveness of the teaching module for non-anesthesiology trainees on COVID-19 patients.
Methods:
Quasi experimental cross sectional pilot study was conducted with a sample of twenty-six trainees. A teaching module was prepared and validated which consisted of lectures, audio-video sessions, demonstrations with hands-on training, debriefing, analytical-phase and reflection. Pre and Post evaluations from student t-test and direct observation of procedural skills (DOPS) were used for knowledge and skill assessment respectively and feedback obtained from Likert's score.
Results:
Pre- and Post-tests had a mean score of 7.42 ± 2.12 and 14.92 ± 2.9 respectively (P value 0.00001). DOPS included 16 point score, in which 23 trainees (88.4%) met the expectations and above expectations as per training objectives. A five-point Likert's score feedback revealed satisfactory and highly satisfactory scores of 100% (ABG), 96.1% (mechanical ventilation), and 84.6% (ventilation in COVID-19 patients). Overall satisfaction for the workshop among respondents was 100 per cent. Confidences of handling scores were 84.5% (interpreting ABG), 65.3% (maneuvering mechanical ventilation), and 96.15% (intubation in COVID-19 patients).
Conclusion:
A planned teaching module in ventilation management helps to train non-anaesthesiologists more effectively as a part of COVID-19 preparedness. Simulation with debriefing based training to the medical fraternity is the best alternative in the present pandemic and it will also ensure the safety of health care professionals.
Keywords: COVID 19, feedback, mechanical ventilation, pandemic, training support
INTRODUCTION
Simulation is one of the important learning tools when it comes to skill acquisition.[1] It also aids as a supplemental tool for training in high stake situations and life threatening events. This has the benefit of reducing patients' safety concerns and permitting repetitive practice, thus minimizing the margin of error. Rare conditions can be simulated for the trainees to practice in patient management before encountering these challenges in the clinical context.[2]
Corona Virus is one of the recent outbreaks that have gained global concern due to its rampant spread. Majority of the patients affected with COVID-19 requires admission, 14% have severe symptoms and 5% of them will be critically ill might need mechanical ventilation, which mandates preparedness.[3,4] Ventilator management requires highly trained professionals, typically intensive care physicians, anesthesiologists, and respiratory therapists. However, it makes the health care workers more vulnerable due to the spread of this disease, which in the worst situation increases the mortality rate. Hence, it is mandatory to have an experienced manpower with adequate knowledge on ventilator graphics to handle the ventilators.[2,3,5] Adequate exposure to patients will facilitate the medical students and doctors to acquire the necessary skills. Moreover, there is an obligation to provide optimal treatment and to ensure patients' safety and well-being. These two competing demands can sometimes pose a dilemma in medical education.[6]
The study was designed to meet the global requirements of knowledge on personal protective measures of health care workers and ventilatory management, as there is a paucity of literature about COVID-19 patients. In addition to this, it also provides an objective to prepare a module for non-anesthesiology trainees to handle ventilators in the management of these patients and to evaluate the effectiveness of the module.
METHODS
A quasi-experimental cross-sectional pilot study was conducted among 26 trainees for 4 days in the month of April. Participants were the residents from clinical specialties (General surgery-14, Dermatology-3, orthopedics-6, ophthalmology-3) without any prior experience with ventilators. They were selected by non-probability convenient sampling and the study was explained in detail following which consent was acquired. Institutional Ethical Committee clearance was obtained on before conducting this study.
A 7-hour teaching module was prepared and validated, which consisted 3 hours of lectures on arterial blood gases (ABG), basics of mechanical ventilation, ventilator strategy in COVID-19 patients and simulation guided ventilator graphics, one hour of audio-video sessions, one hour of demonstrations as well as hands-on training and two hours of assessment. A team of two experienced anesthesiologists coached the trainees to gain knowledge and skills with the help of the teaching module and human patient simulator (HPS) simulator. A total of 4 sessions were conducted where 26 trainees were grouped into 6 or 7.
The teaching tool i.e., the human patient simulator (HPS) is a human-sized high fidelity mannequin with features such as palpable pulses, chest wall expansion, audible breath sounds, and facility for intubation. Scenarios were created and respond to anesthetics and COVID pneumonia like picture was modeled through this simulator.
A debriefing session was carried out after each scenario, which started with the trainee reflecting up on what happened during the scenario. This was followed by an analytical phase in which the trainee was asked the successful aspects of the scenario and the factors that could have been improved. In the last phase of the debriefing session, participants were asked to reflect upon their training. Feedback was given to the participants.
A pre and post evaluation (total 20 questions each carrying 1 mark) was administered to assess the improvement in their knowledge and the effectiveness of the teaching module. Skill assessment was conducted by direct observation of procedural skills (DOPS) method to assess the preparation of checklist, donning and doffing of PPE, understanding the clinical scenarios, ABG interpretation, identifying the clinical problem and response, laryngoscope skill and precautions, application and maneuvering ventilator, understanding ventilator graphics, and weaning protocols [Table 1]. They were categorized as below expectations (score 1-4), borderline expectation (score 5-8), meeting the expectations (score 9-12) and above expectations (score 13-16). Feedback was taken from the participants in a five-point Likert's scale at the end of the teaching-learning session.
Table 1.
Skill assessment by DOPS
| DOPS variables |
|---|
| Preparation of checklist |
| Donning and Doffing of PPE |
| Understanding the clinical scenarios |
| ABG interpretation |
| Identifying the clinical problem & response |
| Laryngoscope skill & precautions |
| Application & maneuvering ventilator |
| Understanding ventilator graphics and weaning protocols |
Not accomplished=0, Partially accomplished=1, Completely accomplished=2
Statistical analysis was performed by using SPSS 20.0 and MS Excel 2010. Descriptive data was presented as Mean ± SD and percentages; data was tabulated, and graphically represented. Student paired t-test was done to compare the means of pre and post-test. For statistical analysis, P < 0.05 was considered statistically significant.
RESULTS
All 26 participants who were administered a pre-test, had a mean score of 7.42 ± 2.12. A post-test was also conducted to all the trainees to know the assessment of knowledge acquired which revealed a mean score of 14.92 ± 2.9 with a statistically significant P value of 0.00001 [Graph 1].
Graph 1.
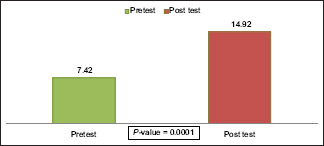
Comparison of Pre- and Post-test scores. *p- value less than 0.05 was considered as statistically significant
DOPS included 16 point score where 23 trainees (88.4%) met the expectations and above expectations as per the training objectives. Only 3 (11.6%) met the borderline expectations or below expectation [Graph 2].
Graph 2.
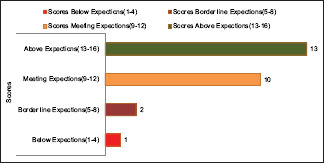
Skill assessment through DOPS
Feedback obtained from the respondents in a five-point Likert's score showed satisfactory and highly satisfactory of 100% for the session on ABG, 96.1% for the session on mechanical ventilation, and 84.6% for the session on ventilation in COVID-19 patient. Overall satisfaction for the workshop among respondents was 100%. Total 84.5% of trainees responded to be confident and very confident in interpreting ABG. For maneuvering mechanical ventilation, it was found that 65.3% were confident and 96.15% were very confident for using personal protective measures to be taken during intubation of COVID-19 patients [Tables 2 and 3].
Table 2.
Trainees satisfaction score (Feedback)
| Session | Highly unsatisfied (1) | Unsatisfied (2) | Neutral (3) | Satisfied (4) | Highly satisfied (5) |
|---|---|---|---|---|---|
| Work Shop | 0% | 0% | 0% | 42.3% | 57.8% |
| ABG | 0% | 0% | 0% | 34.6% | 65.4% |
| Basics of mechanical ventilation | 0% | 0% | 3.84% | 53.8% | 42.3% |
| Ventilation in COVID patients | 0% | 3.84% | 11.53% | 26.9% | 57.69% |
Table 3.
Feedback on acquired confidence
| How confident are you? | Not very confident (1) | Not confident (2) | Neutral (3) | Confident (4) | Very confident (5) |
|---|---|---|---|---|---|
| Interpreting ABG | 0% | 3.84% | 11.53% | 53.8% | 30.7% |
| Manoeuvre mechanical ventilation | 0% | 7.69% | 26.9% | 46.15% | 19.2% |
| About the Protective measures to be taken during intubation of COVID patient | 0% | 0% | 3.84% | 57.69% | 38.46% |
DISCUSSION
Simulation is a technique to replace real patient experiences which usually evokes substantial aspects of treating in a real scenario.[1] The level of acquiring more knowledge with high fidelity simulators and simulation-based training in addition to traditional didactic teaching will escalate the trainee's skills in a better way.[1,7] Few studies conducted by Jeniffer Yee and associates, and Ciullo A and colleagues proved that educating medical fraternity in mechanical ventilation is more successful with education initiatives incorporating new technical knowledge in simulation.[8,9] Safety of health care providers is utmost important in dealing patients with COVID-19, which has a very rapid transmission rate, and this makes them more susceptible while dealing with these patients. It has brought unprecedented challenges as the disease overwhelms health care systems and stresses the clinical workforce.[10,11] Simulation makes education safer especially in dealing with COVID-19 pandemic and useful in training an individual who would be able to maneuver ventilator.[7,12,13] Since there is a risk involved in patient exposure and to preserve the personal protective equipment (PPEs), bedside teaching becomes more arduous. To overcome this shortage we have come up with an alternative for teaching ventilatory management in non-anesthesiology residents.[5,7]
COVID-19 advisories mentioned that intubation to be attempted by most experienced anesthesiologists as it is the most aerosol generating procedure.[14,15] Laryngoscopy was a part of the teaching curriculum to teach the trainees ventilatory management apart from ABG and maneuvering ventilators. We attempted to conduct a training program among non-anaesthesiologists so that these trainees can be utilized as reserve resources during extreme situations of COVID-19.
We used a quasi-experimental cross-sectional pilot study design to estimate the causal impact of simulation based teaching in mechanical ventilation in managing COVID-19 patients among non-anesthesiology residents (n = 26) and planned to evaluate pre- and post-tests.[16,17,18] Knowledge and skill-based questionnaire was conducted on all the residents, to know the baseline knowledge which revealed a mean of 7.42 ± 2.12. Post-didactic lectures on ABG, Mechanical ventilation and ventilator strategy in COVID-19 patients – a simulation-based teaching on high fidelity human patient simulator as a part of the teaching module. We conducted debriefing sessions after every session that allowed participants to gain a clear understanding of their actions and thought process to promote learning outcomes and enhance future clinical performance. Kristian Krogh et al. and Lavett Jones stated simulation-based learning along with debriefing added extra benefit into the trainees even though there is less information about how debriefing sessions are being conducted.[19,20] An analytical phase, where successful aspects and improvisation were dealt, we found this phase acted as a positive reinforcement as far as knowledge based aspects is concerned for the trainees. In the final phase, we asked them to reflect upon where we could be able to self-analyze, manage to add a few extra points and clear doubts regarding the skill.
Masoumeh Erfani Khanghahi and colleagues conducted a systemic review on DOPS and concluded it to be one of the latest and effective method used for skills assessment of a trainee.[21] So we adopted DOPS into a study protocol which was a 16 point questionnaire of which 23 trainees (88.4%) met the expectations and above expectations which indicates that our teaching module is effective to teach ventilatory skills.
A post-test was conducted to check the outcome of training assessment amongst all the residents (20 questions carrying 20 marks) which revealed a mean of 14.92 ± 2.9, which was a good improvement as compared to pre-test 7.42 ± 2.12 with a statistically significant P value of 0.00001, where the adherence increased drastically due to knowledge improvement among trainees.
Agha Ssuccessfully used Likert's scale to get feedback in a five point scale.[22] We assessed trainee satisfaction by 5 point Likert's scale which has given overall satisfaction for the workshop among respondents was 100% (which includes satisfied and very satisfied). We believe the extra enthusiasm of the trainees to learn ventilation might be a confounding factor. As skills and knowledge needs a learning curve, we planned to repeat simulation workshops for the same residents in regular intervals similar to Sree Kumar EJ and Makani Purva and access residents acquisition of knowledge and skills.[23]
In our study, we had limitations as we considered only 26 subjects due to maintaining social distancing to manage COVID-19 spread. The same study with a higher sample size would have been more effective in exhibiting the effectiveness of the module. Our study is a single center study.
CONCLUSION
A planned teaching module in personal protection of health care workers and ventilation management helps to train non-anaesthesiologists more effectively as a part of COVID-19 preparedness. Simulation with debriefing based training to the medical fraternity is the best alternative in the present pandemic and will also ensure the safety of health care professionals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Dr. Pratap R Prof and HOD Department of Anesthesiology, GSL Medical College, Brig Dr. TVSP Murthy Medical superintendent, GSL medical college. Dr. SSC Chakra Rao Chairman Indian Resuscitation Council (IRC). Mr Ganapathi statistician GSL Medical College. Simulation Lab team and Management GSL Medical College.
REFERENCES
- 1.Bhagwat M. Simulation and anaesthesia. Indian J Anaesth. 2012;56:14–20. doi: 10.4103/0019-5049.93338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lorello GR, Cook DA, Johnson RL, Brydges R. Simulation-based training in anaesthesiology: A systematic review and meta-analysis. Br J Anaesth. 2014;112:231–45. doi: 10.1093/bja/aet414. [DOI] [PubMed] [Google Scholar]
- 3.Peng PWH, Ho PL, Hota SS. Outbreak of a new coronavirus: What anaesthetists should know. Br J Anaesth. 2020;5:497–501. doi: 10.1016/j.bja.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajwa SJ, Sarna R, Bawa C, Mehdiratta L. Peri-operative and critical care concerns in coronavirus pandemic. Indian J Anaesth. 2020;64:267–74. doi: 10.4103/ija.IJA_272_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khanduja PK, Bould MD, Naik VN, Hladkowicz E, Boet S. The role of simulation in continuing medical education for acute care physicians: A systematic review. Crit Care Med. 2015;43:186–93. doi: 10.1097/CCM.0000000000000672. [DOI] [PubMed] [Google Scholar]
- 6.Higham H, Baxendale B. To err is human: Use of simulation to enhance training and patient safety in anaesthesia. Br J Anaesth. 2017;119:106–14. doi: 10.1093/bja/aex302. [DOI] [PubMed] [Google Scholar]
- 7.Spadaro S, Karbing DS, Fogagnolo A, Ragazzi R, Mojoli F, Astolfi L, et al. Simulation training for residents focused on mechanical ventilation: A randomized trial using mannequin-based versus computer-based simulation. Simul Healthcare. 2017;12:349–55. doi: 10.1097/SIH.0000000000000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yee J, Fuenning C, George R, Hejal R, Haines N, Dunn D, et al. Mechanical Ventilation Boot Camp: A Simulation-Based Pilot Study. Crit Care Res Pract. 2016;2016:4670672. doi: 10.1155/2016/4670672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciullo A, Yee J, Frey JA, Gothard MD, Benner A, Hammond J, et al. Telepresent mechanical ventilation training versus traditional instruction: A simulation-based pilot study. BMJ Simul Technol Enhanced Learning. 2019;5:8–14. doi: 10.1136/bmjstel-2017-000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.La Cerra C, Dante A, Caponnetto V, Franconi I, Gaxhja E, Petrucci C, et al. Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: A systematic review and meta-analysis. BMJ Open. 2019;9:e025306. doi: 10.1136/bmjopen-2018-025306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: Experience from Jiangsu Province. Ann Intensive Care. 2020;10:1–4. doi: 10.1186/s13613-020-00650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green M, Tariq R, Green P. Improving patient safety through simulation training in anesthesiology: Where are we.?? Anesthesiol Res Pract. 2016;2016:4237523. doi: 10.1155/2016/4237523. doi: 10.1155/2016/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy CC, Cannon EK, Warner DO, Cook DA. Advanced airway management simulation training in medical education: A systematic review and meta-analysis. Crit Care Med. 2014;42:169–78. doi: 10.1097/CCM.0b013e31829a721f. [DOI] [PubMed] [Google Scholar]
- 14.Fuller BM, Ferguson IT, Mohr NM, Drewry AM, Palmer C, Wessman BT, et al. A quasi-experimental, before-after trial examining the impact of an emergency department mechanical ventilator protocol on clinical outcomes and lung-protective ventilation in acute respiratory distress syndrome. Crit Care Med. 2017;45:645–52. doi: 10.1097/CCM.0000000000002268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malhotra N, Bajwa SJ, Joshi M, Mehdiratta L, Trikha A. COVID operation theatre- advisory and position statement of indian society of anaesthesiologists (ISA National) Indian J Anaesth. 2020;64:355–62. doi: 10.4103/ija.IJA_454_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malhotra N, Joshi M, Datta R, Bajwa SJ, Mehdiratta L. Indian society of anaesthesiologists (ISA national) advisory and position statement regarding COVID-19. Indian J Anaesth. 2020;64:259–63. doi: 10.4103/ija.IJA_288_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janse B, Huijsman R, Fabbricotti IN. A quasi-experimental study of the effects of an integrated care intervention for the frail elderly on informal caregivers' satisfaction with care and support. BMC Health Serv Res. 2014;14:140. doi: 10.1186/1472-6963-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yan G, Chen J, Yang G, Duan G, Du Z, Yu Z, et al. Effects of patient-controlled analgesia with hydromorphone or sufentanil on postoperative pulmonary complications in patients undergoing thoracic surgery: A quasi-experimental study. BMC Anesthesiol. 2018;18:1–8. doi: 10.1186/s12871-018-0657-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krogh K, Bearman M, Nestel D. “Thinking on your feet”—A qualitative study of debriefing practice. Adv Simul. 2016;1:12. doi: 10.1186/s41077-016-0011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levett-Jones T, Lapkin S. A systematic review of the effectiveness of simulation debriefing in health professional education. Nurse Educ Today. 2014;34:58–63. doi: 10.1016/j.nedt.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 21.Khanghahi ME, Azar FE. Direct observation of procedural skills (DOPS) evaluation method: Systematic review of evidence. Med J Islam Repub Iran. 2018;32:45. doi: 10.14196/mjiri.32.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agha S, Alhamrani AY, Khan MA. Satisfaction of medical students with simulation based learning. Saudi Med J. 2015;36:731–6. doi: 10.15537/smj.2015.6.11501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.E J SK, Purva M, Chander M S, Parameswari A. Impact of repeated simulation on learning curve characteristics of residents exposed to rare life threatening situations. BMJ Simul Technol Enhanced Learning. 2019 doi: 10.1136/bmjstel-2019-000496. doi: 101136/bmjstel- 2019-000496. [DOI] [PMC free article] [PubMed] [Google Scholar]


