Abstract
Severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) which causes coronavirus disease (COVID-19) is a highly contagious virus. The closed environment of the operation room (OR) with aerosol generating airway management procedures increases the risk of transmission of infection among the anaesthesiologists and other OR personnel. Wearing complete, fluid impermeable personal protective equipment (PPE) for airway related procedures is recommended. Team preparation, clear methods of communication and appropriate donning and doffing of PPEs are essential to prevent spread of the infection. Optimal pre oxygenation, rapid sequence induction and video laryngoscope aided tracheal intubation (TI) are recommended. Supraglottic airways (SGA) and surgical cricothyroidotomy should be preferred for airway rescue. High flow nasal oxygen, face mask ventilation, nebulisation, small bore cannula cricothyroidotomy with jet ventilation should be avoided. Tracheal extubation should be conducted with the same levels of precaution as TI. The All India Difficult Airway Association (AIDAA) aims to provide consensus guidelines for safe airway management in the OR, while attempting to prevent transmission of infection to the OR personnel during the COVID-19 pandemic.
Keywords: Airway, Coronavirus, COVID-19, operation room, pandemic, personal protective equipment, SARS-CoV-2
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which causes coronavirus disease (COVID-19) is a ribonucleic acid encapsulated virus.[1] It is a highly contagious virus which spreads by droplets and direct contact through fomites from infected individuals.[1] These patients may present to the operation room (OR) for an emergency surgery, tracheostomy or for cancer surgeries which are considered as a semi-emergency. When elective surgeries are resumed, asymptomatic patients or carriers of COVID-19 may also be scheduled for surgery. False negative reports have been seen in 30% of asymptomatic patients with the reverse transcription polymerase chain reaction (rT-PCR) assay;[2] thus mandating universal precautions to be taken for all cases presenting to the OR.
Airway management in the OR during the COVID-19 pandemic poses unique challenges. Airway interventions can cause a high amount of aerosolisation, making all the team members at a high risk of acquiring COVID-19 infection during the procedure.[3,4] During airway management, in addition to ensuring patient safety, additional measures to prevent aerosol generation and reduce viral spread are required to ensure safety of the airway manager and the other OR personnel.[4] Use of modified techniques, unfamiliar equipment like a customised intubation and extubation box (COVID box) or other barrier devices, make airway management more challenging. In addition the fear of contamination and infection may lead to cognitive overload which may affect the performance of the airway manager.
Vigilant precautionary measures are warranted during airway management in the OR to prevent the spread of infection among OR personnel. There is no robust evidence for a definite technique or strategy for airway management in OR during the COVID-19 pandemic. The All India Difficult Airway Association (AIDAA) aims to provide consensus guidelines for safe airway management in the OR during the COVID-19 pandemic. These consensus guidelines are based on the evidence from the recent literature and consensus opinion of the experts. These consensus guidelines should be used in conjunction with the recommendations for the general management of COVID patients in the OR.[5,6]
METHODS
A team of 10 airway experts was formed from the AIDAA members who were involved in perioperative airway management of COVID-19 patients. These experts reviewed all the existing literature related to airway management in general and in COVID-19 patients in English from 1st January 2015 until 30th April 2020 from search engines includingPubMed, Embase, Medline and Ovid and Google Scholar Databases. The keywords included: Airway, coronavirus, COVID-19, extubation, operation room, pandemic, personal protective equipment, SARS-CoV-2, tracheal intubation. Additional articles were retrieved by cross-referencing and hand searching. The experts discussed the existing literature using web based meetings and email communication to develop an algorithm and formulate consensus guidelines for airway management in the OR during the COVID-19 pandemic. Since definite evidence was lacking in most areas, recommendations were made by consensus and modifications of the existing AIDAA algorithm from the guidelines for the unanticipated difficult airway in adults.[7]
PLANNING AND PREPARATION
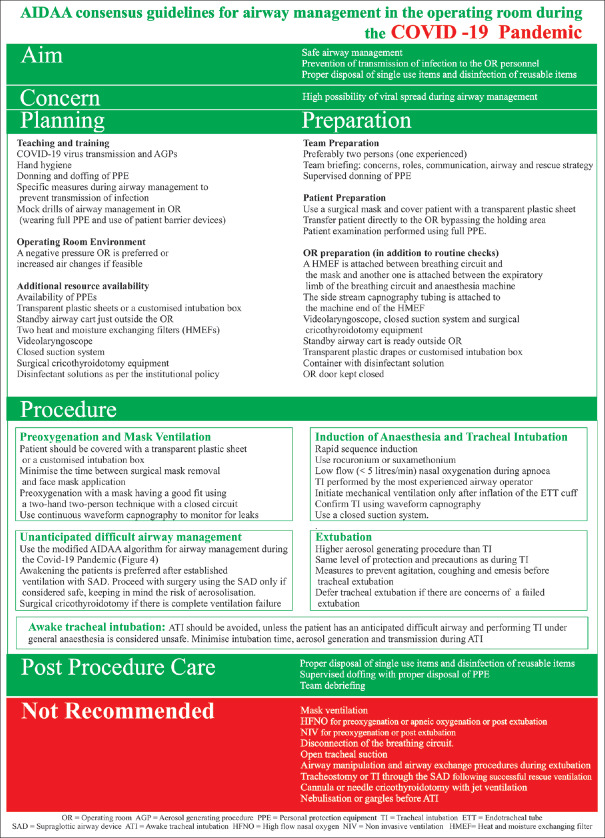
A basic understanding of the COVID-19 infection is paramount for appropriate planning and preparation for airway management in the OR. A thorough understanding of the mode of transmission, the procedures and factors that increase the risk of transmission and methods to break these transmission modalities is required. The key factors for various phases of airway management in the OR have been summarized in Figure 1.
Figure 1.
AIDAA consensus guidelines for airway management in operating room during the COVID-19 pandemic
Understanding theAerosol generating procedures (AGP)
AGPs include any medical and patient care procedure that results in the production of airborne particles (aerosols).[8] The virus spread occurs either because of droplets travelling up to 1-2 meters or from the contact of contaminated surface. Maximum viral load is present in respiratory tract and procedures involving respiratory tract cause major aerosolization of SARS-CoV-2.[9] Coronavirus remains active in the air for 2-3 hours and it also remains active on different surfaces for varying periods, even up to three days. The virus has been reported to be active for 48-72 hours on plastic and metal surfaces.[1] Airway management procedures are considered as the highest risk procedures for transmission of the COVID-19 disease. Mask ventilation, tracheal intubation (TI), tracheal extubation, open suctioning, tracheostomy, cricothyroidotomy, non-invasive ventilation (NIV), high flow nasal oxygen (HFNO) andbronchoscopy areall AGPs.[8] In addition to OR personnel protection during airway handling, cleaning and disinfection of all surfaces are required to decrease the viral load inthe OR.[10]
Teaching and training
Teaching and training in the proper performance of hand sanitisation, donning and doffing of personal protective equipment (PPE) are the most important measures for preventing cross contamination from COVID-19 patients.[11,12] Simulation based training in OR with full PPE and use of patient barrier devices is essential to prepare for airway management using unfamiliar and modified airway management techniques and plays a major role in preventing infection. Communication after donning the PPE, especially in the use of critical language, is challenging.[13] Training in use of sign language is useful to overcome this. Training in proper disposal of contaminated material and disinfection of reusable equipment is necessary to avoid inadvertent spread of the infection.[14]
Additional resource availability
Ensuring availability of essential additional resources is paramount before performing airway management in these patients. We may often need to modify our methods and use innovative alternate strategies to adapt in the event of a resource crunch to create optimum levels of protections against the infection [Table 1].
Table 1.
Additional resources required for airway management
| Mandatory requirements | Desirable requirements |
|---|---|
| Positive pressure avoided in the OR with the door kept closed Experienced airway manager Personal Protective Equipment Heat and moisture exchanging filters (HMEF) (2 in number) Videolaryngoscope Closed suction system Surgical cricothyroidotomy equipment Transparent plastic sheets Standby airway cart just outside the OR Container with disinfection solution |
Negative pressure OR Powered Air Purifying Respirators (PAPR) Customized intubation/extubation box (COVID Box) [Figures 2 and 3] |
Operating room environment
A negative pressure OR is preferred to avoid the spread of corona virus infection. The ORs are routinely positive pressure areas (5-10 cm H2O) which are not preferred.[5] Changes in an existing positive to a negative pressure system should be done in advance if feasible, as per the specification of the system after consultation with the engineers. Alternatively, increase in the air changes in the ORs may be considered. Switching off the centralised air conditioners during AGPs may be considered. Ensure scavenging of anaesthetic and expired gases from the anaesthesia machine to an appropriate exhaust. The OR door must be kept closed at all times.
Experienced airway operator
To increase the chance of first pass success during airway management, it is essential that the most experienced airway operator among the team members performs airway management. Individuals with co-morbidities, immunocompromised status, pregnancy, and advanced age should not be part of OR Team.
Personal protection equipment (PPE)
The availability of PPEs for all OR personnel should be ensured. If available, face shield respirators or Powered Air Purifying Respirators (PAPR) may be used for additional protection.[13] The PPE should include a fluid impervious coverall / gown, long shoe covers, a cap, goggles, a fit tested N95 mask, double layer of gloves, and a head hood or full face shield.[4,14,15,16] It is preferable to have two layers of protective clothing. Fogging of the goggles or the face shield is a concern and may be reduced by minimising the time gap between donning and performing TI, or use of anti-fog solutions.
Additional equipment
The following additional equipment needs to be arranged for airway management of COVID-19 patients:[10,16,17,18]
-
Airway Equipment
Two heat and moisture exchanging filters (HMEFs) are necessary to prevent contamination of the breathing circuit and the anaesthesia machine. A HMEF effectively filters viruses and bacteria
TI using a videolaryngoscope (VL) is preferred for higher first attempt success rate. In addition, TI can be accomplished by looking at the VL monitor, thus avoiding close proximity to the oral cavity for direct glottis visualisation. A closed suction system is recommended for tracheal suctioning. In the event of complete ventilation failure, surgical cricothyroidotomy using the ”scalpel-bougie technique” [scalpel with 11 number blade, bougie and size 6 endotracheal tube (ETT)] should be preferred)[6,8]
-
Standby Airway Cart
A standby airway cart needs to be kept ready just outside the OR for easy access to additional equipment, if required. This is to avoid contamination of additional airway equipment, such as alternate size ETTs, masks, oral/nasal airways, rescue airway equipment etc.
-
Barrier Devices
A method to cover a patient's face during airway management may help limit aerosol exposure and is encouraged in addition to PPE. A transparent plastic sheet, COVID box, plastic tent etc. may be used [Figures 2 and 3].[18] However, there is no evidence to recommend their efficacy in reducing aerosol spread. In addition, they may make the TI more difficult due to unfamiliarity with the device, restriction of hand movements and possible difficulty in visualisation. Hence, prior practice in airway management using these devices is essential. Monitoring devices including the monitor of the VL (if not attached to the device) may be covered using transparent plastic sheets to prevent contamination of the equipment.
Figure 2.

Tracheal intubation using a customised intubation tent
Figure 3.

Patient's face covered with a transparent plastic sheet during preoxygenation
Disinfection
Reusable items will need to be immersed immediately after its use into a disinfectant solution e.g., 1% sodium hypochlorite (or as per institutional policy) placed inside a container in the OR.[19] Disinfection of the OR and reusable items should be done as per institutional policy.
AIRWAY MANAGEMENT DURING GENERAL ANAESTHESIA
Patient preparation
All spontaneously breathing patients should wear a surgical face mask. They should be directly transferred to the OR bypassing the preoperative holding area.[20] Recent studies have shown that povidone iodine (0.23%-1%) gargles and nasal drops administered prior to transfer to the OR significantly reduces viral load in the oro and nasopharynx.[21,22,23] Patient examination, including airway evaluation, should be performed using full PPE.
Team preparation
Minimise the airway management team (preferably two persons). All team members should be briefed about specific patient concerns, their specific role, airway management strategy, and rescue strategy
The method of communication after donning PPE should be discussed.
Operating room preparation
In addition to the routine anaesthesia equipment checking, ensure that the following are available:[10,16,17]
An HMEFis attached between breathing circuit and the mask and another one is attached between the expiratory limb of the breathing circuit and anaesthesia machine. The side stream capnography tubing is attached to the machine end of the HMEF
VL, closed suction system and surgical cricothyroidotomy equipment
Standby airway cart is ready outside OR
Transparent plastic drapes or COVID box
Container with disinfectant solution.
Steps of tracheal intubation
Preoxygenation
The patients should be wearing a surgical mask and covered with a transparent plastic sheet or a COVID box on the OR table [Figure 3] Position the patient appropriately. Minimise the time between removal of the patient's mask and application of the face mask.
Check that the HMEF and the side stream capnography tubing are appropriately placed before preoxygenation
Preoxygenation with 100% oxygen for 3-5 minutes using a tight-fitting face mask and a two hand technique with tidal volume breathing using a closed circuit is recommended. HFNO and NIV should be avoided for preoxygenation as they have the potential to generate aerosols.[24]
trace or a low numerical EtCO2 value during preoxygenation may indicate a leak around the face mask and should prompt interventions to improve the seal.[25] The side stream capnograph should be connected towards the machine end of the HMEF.
Induction of anaesthesia
Based on the Wuhan experience and recently published recommendations, rapid sequence induction (RSI) is the preferred method to avoid mask ventilation and facilitate fasterTI.[3,16,26]
Appropriate doses of rapidly acting neuromuscular blocking drugs like rocuronium or suxamethonium should be used to achieve complete muscle relaxation. Cricoid pressure should be avoided if the patient is adequately fasted. Use of cricoid pressure encourages the assistant to lean closer to the patient's airway, thereby increasing the chance of exposure to aerosols.[25]
Apnoeicoxygenation
Avoid mask ventilation to prevent aerosol generation, unless the oxygen saturation (SpO2) goes below 95%. If mask ventilation is required it should be performed under a transparent plastic sheet. Mask ventilation if required should be done with a tight mask fit using a two-hand technique to prevent leaks around the face mask.[27]
Apnoeic oxygenation with HFNO should be avoided. Low flow nasal oxygenation less than 5 litres/min is recommended during apnoea. This is less aerosol generating and improves the non-hypoxic apnoea time during TI.[28]
Tracheal intubation
VL assisted TI is recommended. It is preferable to preload the ETT with a stylet or use a bougie as appropriate.
After TI, the ETT cuff should be inflated and the HMEF connected directly to the ETT. Ensure that there is no leak around the ETT cuff.
Mechanical ventilation should only be initiated after the ETT cuff is inflated.
A closed suction system should be used.
Confirm ETT placement in the trachea using waveform capnography, bilateral chest expansion or ultrasound, if available. Use of a stethoscope is not feasible while wearing PPE.
Disposal and decontamination of contaminated equipment
Single use items should be immediately discarded in the appropriate disposal bag and reusable items dropped in to the container with disinfectant solution without touching them elsewhere, to prevent contamination of the OR and health care workers.
UNANTICIPATED DIFFICULT AIRWAY MANAGEMENT
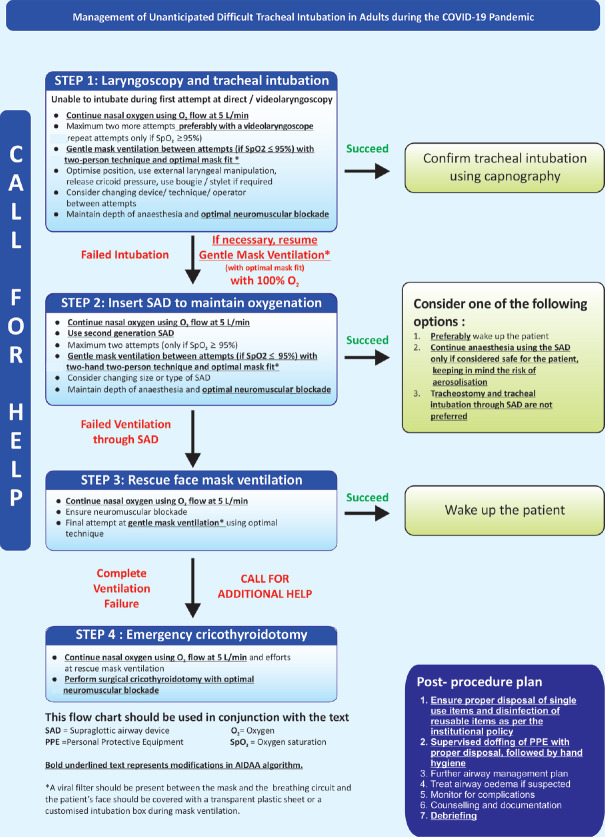
In case an unanticipated difficult airway is encountered during the first attempt at TI, the AIDAA[7] guideline for unanticipated difficult airway in adults with modification [Figure 4] may be followed to prevent cross infection with the virus. When faced with an unanticipated difficult airway, avoid using HFNO and face mask ventilation with a leak, as they may all lead to aerosol generation. A two-person two-hand technique should be preferred for mask ventilation. Two further attempts at TI are recommended only if the SpO2 is ≥95% with intermittent mask ventilation performed only if the SpO2 is <95%. Further attempts at TI should be done using a VL. Use of a second generation SGAis recommended in case of failedTI, however the plastic sheet or the COVID box over the patient's face, should not be removed to prevent aerosol spread. Awakening the patients should be preferred after established ventilation with a SGA. Proceed with the surgery with a well-placed SGA device in situ, only if it is considered safe, keeping in mind the risk of aerosolisation. Avoid TI through the SGA and performing a tracheostomy for elective surgeries as they are high AGPs. In the event of a complete ventilation failure, it is recommended to proceed with a surgical cricothyroidotomy. Avoid using jet ventilation with a needle cricothyrotomy as this may increase the chances of aerosol spread.
Figure 4.
Management of unanticipated difficult tracheal intubation in adults during the COVID-19 pandemic -Algorithm
TROUBLESHOOTING DURING GENERAL ANAESTHESIA
Avoid unnecessary disconnection of the ETT and the breathing circuit during mechanical ventilation to avoid aerosol spread.
If a circuit disconnection is required, put the anaesthesia machine on a standby mode. Keep the transparent plastic sheet or the COVID box over the patient's face to prevent spread of the virus. Always keep the HMEF connected to the ETT during disconnection. However, if a HMEF change or tracheal aspirate needs to be collected, clamping the ETT transiently may be considered. If a self-inflating bag needs to be used for manual ventilation, attach it to the machine end of the HMEF.
Tracheal suction should be done using a closed suction system at all times.
TRACHEAL EXTUBATION
Tracheal extubation is considered as a higher aerosol generating procedure than TI.[28,29]
Tracheal extubation should preferably not be performed in a light plane of anaesthesia. Pharmacological measures to prevent agitation and coughing are recommended before tracheal extubation.[29,30]
Tracheal suction should be performed only if required, using the closed suction system.
Prophylactic antiemetics should be administered towards the end of the procedure to reduce risk of vomiting and consequent viral spread.
Tracheal extubation should be performed under a transparent plastic sheet or COVID box. A face mask may be threaded over the ETT prior to tracheal extubation, to further prevent spread of aerosols.
Nebulisation with saline or bronchodilators should be avoided. Bronchodilators may be given using metered-dose inhalers and spacers.
Airway manipulation and airway exchange procedures should be avoided during extubation.
Tracheal extubation is an elective procedure, hence it may be deferred if there are any concerns of a failed extubation.
AWAKE TRACHEAL INTUBATION
Awake tracheal intubation (ATI) should be avoided as far as possible, unless the patient has an anticipated difficult airway and performing TI under general anaesthesia is considered unsafe. Managing an anticipated difficult airway is a challenging task for the anaesthesiologist, as ATI is a highly aerosol generating procedure.[31] Proper planning, preparation and execution of the procedure is required to ensure patient and operator safety. Modification of techniques to reduce aerosol generation and spread are required. The goal should be to minimize TI time, reduce aerosol generation and prevent aerosol transmission.
Prolonged duration of ATI increases exposure time to the aerosols. If feasible, awake VL aided TI should be preferred over TI using a flexible bronchoscope as it is associated with shorter TI time.[31] Meticulous planning, optimal preparation, pre procedural briefing and proper coordination among team members, reduces procedural time. Good counselling and optimal level of sedation increases the success rate and decreases the procedural time.
Anaesthetising the airway using local anaesthetic techniques are challenging. There is a potential risk of aerosol generation with all techniques. Thus, these should be performed only after weighing the benefits and the risks along with the use of PPE. Nebulisation is best avoided as it is considered as an AGP.
Use of a disposable flexible bronchoscope, disposable VL or a VL with disposable blades are recommended for performing ATI. Another advantage of an awake VL aided TI over using a flexible bronchoscope, is the feasibility of performing TI using the COVID box or tent. If a flexible bronchoscope is used, the patient's face should be covered with a transparent plastic sheet. For preventing viral spread, similar peri- procedural care should be undertaken as during TI under general anaesthesia.
POST-PROCEDURE CARE
The patient should be wearing a surgical face mask and be covered with a transparent plastic sheet, before transfer to the designated area after surgery. Ensure that proper disposal of single use items and disinfection of reusable equipment has been done as per the institutional policy.
Supervised doffing with proper disposal of PPE should be performed followed by adequate hand hygiene. The OR monitors, anaesthesia machine, other equipment, and all OR surfaces should be disinfected according to the institutional policy after each surgery. At the end of the procedure, all OR personnel should be debriefed about the procedure, disposal, and disinfection of contaminated equipment and proper personal protection.
FUTURE RESEARCH
Further research is required to identify the best tools and strategies to prevent aerosolisation, contamination and spread of the virus in the OR. Appropriate use of barrier devices and their utility in preventing contamination and spread, the best PPE for the health care worker and optimal decontamination techniques, need to be investigated. In addition, the psychological impact on the health care worker during airway management in such challenging circumstances, including measures to mitigate them, needs to be evaluated.
Disclaimer
These consensus guidelines are applicable for airway management of adult patients suspected or infected with coronavirus in the operation room (OR) and should be used in conjunction with recommendations for the general management of these patients in the OR. These recommendations should be adapted to the local policies prevalent at the workplace. With the emergence of new evidence, these guidelines may require modification.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Van-Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wikramaratna P, Paton RS, Ghafari M, Lourenco J. EstimatingEstimating false-negative detection rate of SARS-CoV-2 by RT-PCR. MedRxiv. 2020. Available from: https://doiorg/101101/2020040520053355 . Last cited on 2020 Apr 30. [DOI] [PMC free article] [PubMed]
- 3.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020;75:785–99. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook TM. Personal protective equipment during the COVID-19 pandemic – Anarrative review. Anaesthesia. 2020. https://doiorg/101111/anae15071 . Epub ahead of print. Last cited on 2020 Apr 30. [DOI] [PMC free article] [PubMed]
- 5.Malhotra N, Bajwa SJ, Joshi M, Mehdiratta L, Trikha A. COVID operation theatre- Advisory and position statement of Indian society of anaesthesiologists (ISA national) Indian J Anaesth. 2020;64:355–62. doi: 10.4103/ija.IJA_454_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bajwa SJ, Sarna R, Bawa C, Mehdiratta L. Peri-operative and critical care concerns in coronavirus pandemic. Indian J Anaesth. 2020;64:267–74. doi: 10.4103/ija.IJA_272_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. doi: 101001/jama 20203786 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: Operating room preparation and guidance. Can J Anaesth. 2020;67:756–8. doi: 10.1007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorbello M, El-Boghdadly K, Di Giacinto I, Cataldo R, Esposito C, Falcetta S, et al. The Italian coronavirus disease 2019 outbreak: Recommendations from clinical practice. Anaesthesia. 2020;75:724–32. doi: 10.1111/anae.15049. [DOI] [PubMed] [Google Scholar]
- 12.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020;67:568–76. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myatra SN, Patwa A, Divatia JV. Critical language during an airway emergency: Time to rethink terminology? Indian J Anaesth. 2020;64:275–9. doi: 10.4103/ija.IJA_214_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, et al. Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anesth. 2020 doi: 10.1007/s12630-020-01620-9. doi: 101007/s12630-020-01620-9 [Last cited on 2020 Apr 30] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meng L, Qiu H, Wan L, Ai Y, Xue Z, Guo Q, et al. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan's experience. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003296. doi: 101097/ALN0000000000003296 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao W, Wang T, Jiang B, Gao F, Wang L, Zheng H, et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: Lessons learnt and international expert recommendations. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.026. doi: 101016/jbja 202003026 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020 doi: 10.1056/NEJMc2007589. doi: 101056/NEJMc2007589 Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guidelines for disinfection of quarantine facility (for COVID-19) by National Centre for Disease Control. [Last cited on 2020 May 10]. Available from: https://ncdcgovin/WriteReadData/l892s/89168637271584172711pdf .
- 20.London MJ. Coronavirus disease 2019 (COVID-19) patients: Airway management, anesthesia machine ventilation, and anesthetic care [Internet] UpToDate 2020 Last updated: Apr 28, 2020. [Last cited on 2020 Apr 30]. Available from: https://wwwuptodatecom/contents/coronavirus-disease-2019-covid-19-patients-airway-manag ement-anesthesia-machine-ventilation-and-anesthetic-care/printsearch=coronavirus&source=search_result& selectedTitle=7~150&usage_type=default&display_rank=7 .
- 21.Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther. 2018;7:249–59. doi: 10.1007/s40121-018-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eggers M, Eickmann M, Zorn J. Rapid and effective virucidal activity of povidone-iodine products against Middle east respiratory syndrome Coronavirus (MERS-CoV) and Modified vaccinia virus Ankara (MVA) Infect Dis Ther. 2015;4:491–501. doi: 10.1007/s40121-015-0091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loftus RW, Dexter F, Parra MC, Brown JR. Importance of oral and nasal decontamination for patients undergoing anesthetics during the COVID-19 era. Anesth Analg. 2020 doi: 101213/ANE0000000000004854 [Epub ahead of print] [Google Scholar]
- 24.Respiratory Therapy Group, Respiratory Medicine Branch, Chinese Medical Association. Expert consensus on protective measures related to respiratory therapy in patients with severe and critical coronavirus infection. Chinese J Tuberc Respir Dis. 2020;17:E020. [Google Scholar]
- 25.Brewster DJ, Chrimes NC, Do TBT, Fraser K, Groombridge CJ, Higgs A, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020 doi: 10.5694/mja2.50598. doi: 105694/mja250598 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo M, Cao S, Wei L, Tang R, Hong S, Liu R, et al. Precautions for Intubating Patients with COVID-19. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003288. doi: 101097/ALN0000000000003288 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fei M, Blair JL, Rice MJ, Edwards DA, Liang Y, Pilla MA, et al. Comparison of effectiveness of two commonly used two-handed mask ventilation techniques on unconscious apnoeic obese adults. Br J Anaesth. 2017;118:618–24. doi: 10.1093/bja/aex035. [DOI] [PubMed] [Google Scholar]
- 28.Lockhart SL, Duggan LV, Wax RS, Saad S, Grocott HP. Personal protective equipment (PPE) for both anesthesiologists and other airway managers: Principles and practice during the COVID-19 pandemic. Can J Anesth. 2020 doi: 10.1007/s12630-020-01673-w. doi: 101007/s12630-020-01673-w [Last cited on 2020 Apr 30] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DG. Pharmacological methods for reducing coughing on emergence from elective surgery after general anesthesia with endotracheal intubation: Protocol for a systematic review of common medications and network meta-analysis. Syst Rev. 2019;8:1–7. doi: 10.1186/s13643-019-0947-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aminnejad R, Salimi A, Saeidi M. Lidocaine during intubation and extubation in patients with coronavirus disease (COVID-19) Can J Anaesth. 2020;67:759. doi: 10.1007/s12630-020-01627-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang J, Ma DX, Li B, Wu AS, Xue FS. Videolaryngoscopy versus fiberoptic bronchoscope for awake intubation – A systematic review and meta-analysis of randomized controlled trials. Ther Clin Risk Manag. 2018;14:1995–63. doi: 10.2147/TCRM.S172783. [DOI] [PMC free article] [PubMed] [Google Scholar]