The shortage of ventilators due to present COVID-19 pandemic is a great challenge for India. New ventilators are not available in the market. To face the upcoming situation, a device has been prepared which can help to ventilate 5 patients at a time with minimal damage to lung mechanics. Manufacturing of this device is very easy and can be made at the local marketplace.
We need 2 large diameter copper pipes and 10 small diameter copper pipes which must be welded, so as to prepare an inspiratory and expiratory extension device, which is then attached to the ventilator as shown in Figure 1. Bacterial and viral filters are attached to the individual expiratory ports to check cross infection. Up to 2 meters of extension can be easily attached to the breathing circuit [Figure 2].
Figure 1.
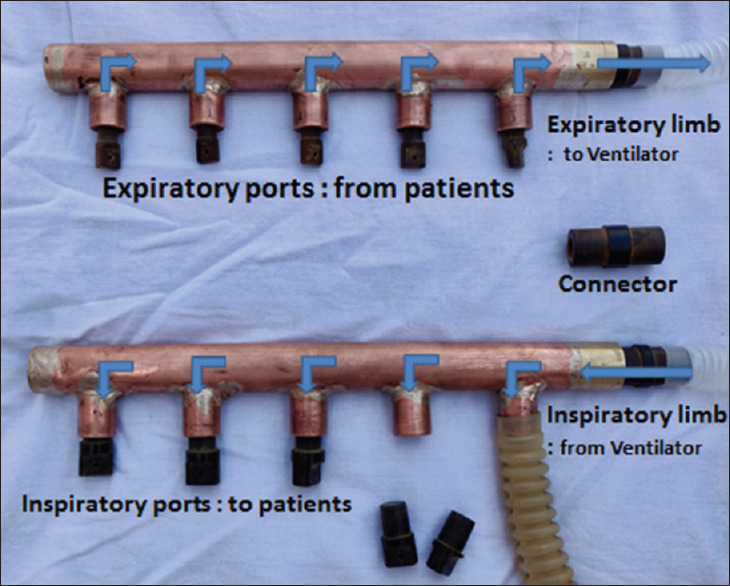
This image demostrates the extension device for the ventilator with inspiratory and expiratory limbs
Figure 2.
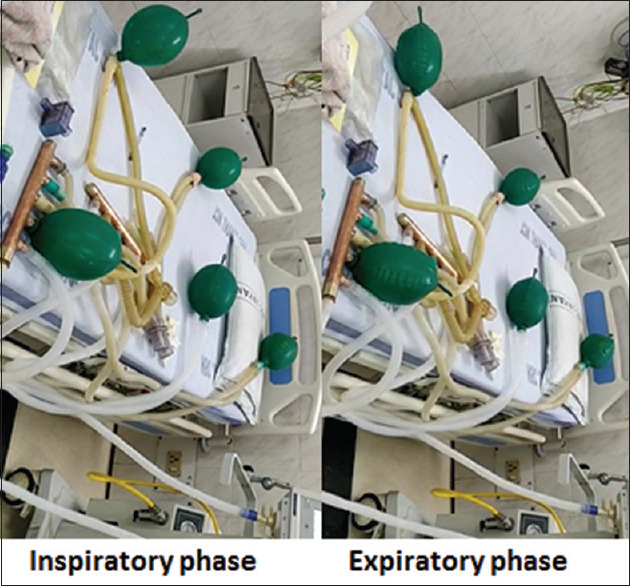
This image demostrates different phases of respiration with image on the left showing inspiratory phase and the right image showing expiratory phase
In COVID-19 pneumonia, patients can present as ARDS with hypoxemia refractory to oxygen therapy requiring mechanical ventilation.[1] We are staring at potential ventilator shortage as patients requiring ventilation may be far more than the available ventilators. With this device one ventilator can be modified to provide ventilatory support to 5 patients or more of similar lung physiology.
Ventilator is to be set in SIMV (PCV) + PSV mode to prevent volutrauma and barotrauma. Level of pressure support should be set so that plateau pressure of system should not go beyond 30 cm of H2O.[2] This will ensure minimal damage to lung. If higher plateau pressure is required, it is better to increase PEEP of the system. Individualised deep sedation with midazolam, propofol or fentanyl infusions are recommended to curb patient's respiratory drive and prevent dyssynchrony.[2] The lung physiology of each patient is monitored frequently. Intensive closed monitoring by dedicated multi parameter monitors for each patient will continuously display SpO2, Respiratory rate (RR), EtCO2, ECG, Heart rate and Blood Pressure indicating adequacy of ventilation. If there is change in lung mechanics of any patient, the trend of monitored parameters of the patient will fall out of allowed range such as in case of bronchospasm or deterioration of ARDS. The trend of EtCO2 is good indicator of individual patient's minute ventilation. The patient is then shifted to a ventilator dedicated to him after plugging the exhalation and inhalation port of that patient.
There have been studies in the past as well which successfully demonstrated that one ventilator can be used in 4 patients in setting of disaster management. Richard D Branson et al.[3] also published similar article.
COVID-19 pneumonia, despite falling in most of the circumstances under the Berlin definition of ARDS, is a specific disease whose distinctive features are severe hypoxemia often associated with near normal respiratory system compliance.[4]
Patients with COVID-19 may not tolerate traditional modes of ventilation such as volume-limited, low tidal volume ventilation. Pressure-limited modes or volume targeted pressure-controlled ventilation may be required.[5]
Indian Society of Critical Care Medicine (ISCCM) in its position statement has mentioned that alternative methods may be used in situations when demand for ventilator exceeds ventilators available in ICU. It has suggested that non-invasive ventilators can be used for patients not requiring high FiO2 and for recovering patients.[6] In such situations and in view of associated NIV shortage, patient may be intubated and SIMV (PCV) can be used with same settings for multiple patients.
In our setting, we used SIMV (PCV) with pressure in the range of 25-26 cm of H2O with PEEP 8-12 cm of H2O. We tried to keep Peak inspiratory pressure below 35 cm of H2O and Plateau pressure below 30 cm of H2O. The bed arrangement of the patients will be in radial pattern and standard distancing of 1 m should be followed.
This type of respiratory therapy should be used only when the patients requiring emergency ventilator support outnumber the available ventilators during disaster surge involving multiple casualty with respiratory failure, and as a last resort, to buy time for a limited period. The patient should be shifted on single ventilator as early as possible.
Academics and research fields including that of health sciences are recognized globally by how much significant impact they exert in real practice.[7] Devices like these may prove to be life-saving in case there is an acute shortages of ventilators due to sudden patient surge.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bajwa SJ, Sarna R, Bawa C, Mehdiratta L. Peri-operative and critical care concerns in coronavirus pandemic. Indian J Anaesth. 2020;64:267–74. doi: 10.4103/ija.IJA_272_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malhotra N, Joshi M, Datta R, Bajwa SJ, Mehdiratta L. Indian society of anaesthesiologists (ISA national) advisory and position statement regarding COVID-19. Indian J Anaesth. 2020;64:259–63. doi: 10.4103/ija.IJA_288_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Branson RD, Blakeman TC, Robinson BH, Johannigman JA. Use of a single ventilator to support 4 patients: Laboratory evaluation of a limited concept. Respir Care. 2012;57:399–403. doi: 10.4187/respcare.01236. [DOI] [PubMed] [Google Scholar]
- 4.Gattinoni L, Coppola S, Cressoni M, Busana M, Chiumello D. COVID-19 does not lead to a “Typical” acute respiratory distress syndrome. ATS Journals. 2020 doi: 10.1164/rccm.202003-0817LE. doi: https://doiorg/101164/rccm 202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel M, Hyzy R. Ventilator management strategies for adults with acute respiratory distress syndrome UpToDate 2020 [Google Scholar]
- 6.Mehta Y, Chaudhry D, Abraham OC, Chacko J, Divatia J, Jagiasi B, et al. Critical care for COVID-19 affected patients: Position statement of the Indian society of critical care medicine. Indian J Crit Care Med. 2020 doi: 10.5005/jp-journals-10071-23395. 105005/jp-journals-10071-23395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajwa SJ, Mehdiratta L. Ensuring practical feasibility and sustainability of research work: Need of the hour. Indian J Anaesth. 2020;64:264–6. doi: 10.4103/ija.IJA_285_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


