Abstract
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) a pandemic, and in the weeks following, public health organizations, medical associations, and governing bodies throughout the world recommended limiting contact with others to “flatten the curve” of COVID-19. Although both ischemic and hemorrhagic strokes have been reported with COVID-19, there has been anecdotal suggestion of an overall decrease in stroke admissions. To date, the effects of any pandemic on telestroke service lines have not been described. The purpose of this cross-sectional analysis of telestroke activations in the 30 days before and after the declaration of the COVID-19 pandemic is to describe the difference in case volumes of telestroke activations, the characteristics of patients, and treatment recommendations between the 2 time frames. We found a 50.0% reduction in total telestroke activations between the predeclaration group (142 patients) and the postdeclaration group (71 patients). There were no statistically significant differences in age (P=.95), sex (P=.10), diagnosis (P=.26), or regional variations (P=.08) in activation volumes. The percentage of patients for whom we recommended urgent stroke treatment with intravenous alteplase, mechanical thrombectomy, or both decreased from 44.4% (28 of 63) to 33.3% (11 of 33). The reasons for the sunstantial decrease in telestroke activations and urgent stroke treatment recommendations are likely multifactorial but nevertheless underscore the importance of continued public health measures to encourage patients and families to seek emergency medical care at the time of symptom onset.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; ED, emergency department; IV-tPA, intravenous tissue plasminogen activator; NIHSS, National Institutes of Health Stroke Scale; WHO, World Health Organization
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) a pandemic on March 11, 2020. The ultimate magnitude of impact from COVID-19 has yet to be seen in the United States. Neurologic manifestations of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been reported in 36.4% of the Wuhan cohort of patients with COVID-19, with ischemic and hemorrhagic stroke occurring in 5.7% of patients.1
Anecdotally, the volumes of stroke admissions in some communities in the United States have recently decreased.2 Prior studies during epidemics such as the Middle East respiratory syndrome epidemic have documented decreased emergency department (ED) utilization collectively.3 , 4 This finding brings into question whether patients may feel dissuaded from presenting to the hospital with mild or rapidly resolving symptoms—a situation that could be reflective of patients’ anxieties during this daunting time. With this scenario, we would anticipate that the volume of patients with stroke who have more severe deficits would still remain stable. However, Zhao et al5 reported a 50% reduction in thrombectomies in Shanghai in the first month after the Spring Festival when compared with the same time period in 2019. Whether this decline reflects a reduction in patient volume, decreased eligibility due to delayed presentation, reluctance to perform a procedure that could potentially result in contamination or exposure, unavailability of specialized staff who may be ill or redeployed to another specialty, or simply the lack of resources or hospital capacity to carry out the procedures is unknown.
Because of the relatively new technology offered through current telestroke practices, the effects of a global pandemic on a telestroke service line have yet to be described. We aimed to analyze the patterns of our telestroke population in the 30 days preceding the WHO declaration of the COVID-19 pandemic on March 11, 2020, compared with the 30 days following this declaration through a retrospective review of all telestroke activations from February 10, 2020, until April 9, 2020, at our 27 Mayo Clinic–affiliated telestroke spoke hospitals.
Methods
We retrospectively reviewed data collected for ED telestroke activations for 30 days before the pandemic declaration (February 10 to March 10, 2020) and 30 days after the declaration (March 11 to April 9, 2020) from the Mayo Clinic telestroke network. This telestroke network provides 24-hour synchronous audio-video telestroke service to 27 hospitals located in Arizona, Florida, Iowa, Minnesota, and Wisconsin and is activated when an ED physician or advanced practice practitioner recognizes patients presenting with acute stroke symptoms and signs who may be amenable to urgent stroke treatment. Data reviewed included patient age, sex, telestroke service location, time of symptom onset or last known normal, time of telestroke activation, diagnoses, National Institutes of Health Stroke Scale (NIHSS) score, and recommendations for treatment with intravenous tissue plasminogen activator (IV-tPA) and/or endovascular thrombectomy.
Telestroke activation criteria for our institution are (1) presence of any persistent focal neurologic deficits presenting within 6 hours of stroke onset or last known normal or (2) persistent neurologic deficits in patients with an NIHSS score of 6 or greater presenting within 6 to 24 hours from stroke onset or last known normal time.
Continuous variables are reported as mean ± SD. Continuous variables were compared using a Student t test. Categorical variables are repor ted as number and percentage and compared using a χ2 test. All analyses were performed using JMP Pro statistical software, version 14.1 (SAS Institute).
Results
There were 142 stroke activations in the pre–pandemic declaration period and 71 in the post–pandemic declaration period—a 50.0% reduction in volume. The average number of telestroke activations per day decreased from 4.7 to 2.4. The number of patients in whom a telestroke video visit was completed with stroke as the final diagnosis decreased by 50.8%, from 65 to 33. There were no differences in age, sex, diagnosis, or regional variation in volume (Table 1 ).
Table 1.
| Variable | Before pandemic declaration | After pandemic declaration | P value |
|---|---|---|---|
| Total cases | 142 | 71 | NA |
| Age (y) | 67.6±12.3 | 67.7±15.1 | .95 |
| Female sex | 77 (54.2) | 30 (42.3) | .10 |
| Primary diagnosis | .26 | ||
| TIA | 13 (9.2) | 8 (11.3) | |
| Ischemic stroke | 63 (44.4) | 33 (46.5) | |
| Intracranial hemorrhage | 2 (1.4) | 4 (5.6) | |
| Stroke mimic | 64 (45.1) | 26 (36.6) | |
| Telestroke region | .08 | ||
| Arizona | 14 (9.9) | 9 (12.7) | |
| Florida | 45 (31.7) | 32 (45.1) | |
| Midwest region | 83 (58.5) | 30 (42.3) |
NA = not applicable; TIA = transient ischemic attack.
Data are presented as mean ± SD or No. (percentage) of patients.
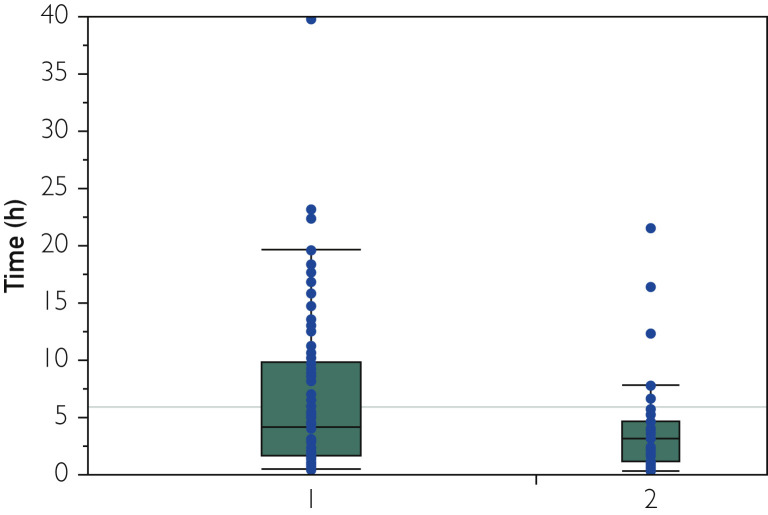
Table 2 summarizes the clinical variables in patients with diagnosis of ischemic stroke only. Although the proportion of ischemic stroke diagnosis volumes was similar before and after the pandemic declaration, the last known normal/symptom onset time to telestroke activation in the ED was significantly shorter (6.8 hours vs 4.2 hours, P=.04) for the post–pandemic declaration group (Figure ). Recommendation for acute stroke intervention (IV-tPA and/or thrombectomy) occurred at a lower rate for our post–pandemic declaration group, despite the findings of similar stroke severity in the 2 groups. Notably, however, all patients who did not receive urgent stroke treatment in the post–pandemic declaration group had an NIHSS score of 6 or less, with the majority of patients having an NIHSS score of 3 or less (21 of 24 [87.5%]).
Table 2.
| Variable | Before pandemic declaration | After pandemic declaration | P value |
|---|---|---|---|
| Total ischemic stroke | 63 (44.4) | 33 (46.5) | NA |
| Last known normal (h) | 6.8±7.3 | 4.2±4.7 | .04 |
| NIHSS score | 6.9±7.0 | 4.8±5.5 | .10 |
| Severity (NIHSS score) | .18 | ||
| Mild (≤4) | 31 (49.2) | 21 (63.6) | |
| Moderate to severe (>4) | 32 (50.8) | 12 (36.4) | |
| Treatment | .29 | ||
| No treatment | 35 (56.6) | 22 (66.7) | |
| Treatment | 28 (44.4) | 11 (33.3) | |
| Treatment type | .16 | ||
| tPA only | 17 (27.0) | 3 (9.1) | |
| Endovascular only | 6 (9.5) | 4 (12.1) | |
| tPA + endovascular | 4 (6.4) | 4 (12.1) | |
| None | 36 (57.1) | 22 (66.7) |
NA = not applicable; NIHSS = National Institutes of Health Stroke Scale; tPA = tissue plasminogen activator.
Data are presented as No. (percentage) of patients or mean ± SD.
Figure.
Last known normal time to telestroke activation. Horizontal lines within boxes indicate medians, and top and bottom borders of boxes indicate 75% and 25% quantiles. The whiskers above and below the boxes represent 1.5 times the interquartile range. Points beyond the whiskers are outliers 1 = pre–pandemic declaration group (February 10, 2020, until March 10, 2020); 2 = post–pandemic declaration group (March 11, 2020, until April 9, 2020).
Discussion
Anecdotally from stroke centers internationally, overall stroke volumes appear to have decreased.6 Several questions regarding this phenomenon include (1) if the true incidence of stroke has decreased, (2) if patients with stroke or transient ischemic attack are staying home due to COVID-19 exposure concern, (3) if patients are presenting too late for urgent therapies and thus staying at their local hospital without telestroke activation or being transferred to a stroke center, (4) if decreased travel for medical appointments result in fewer stroke admissions, and (5) if fewer patients with stroke mimics are presenting to the ED.
This retrospective review describes the telestroke activation patterns of the Mayo Clinic telestroke network in the 30 days preceding the declaration of the COVID-19 pandemic and the 30 days following the declaration. There was a notable reduction in average telestroke utilization from 4.7 to 2.4 activations per day, which was observed across all geographic regions of the telestroke network. The observed decrease in volumes at our spoke sites argues against a phenomenon that could be attributed to reluctance of community hospitals to refer to tertiary referral centers or decreased acceptance of patients from the receiving tertiary centers. However, it remains unclear if the overall reduction in volume of telestroke activations was due to a reduced incidence of stroke, patient-related factors, or a reduction in utilization by ED physicians. It is notable that similar reductions in volume have been seen for percutaneous coronary interventions in the setting of ST-elevation myocardial infarction in the United States as well as reports from Spain.7 , 8
We found that the median time from reported symptom onset or last known normal time to telestroke activation was decreased in the post–pandemic declaration group compared with the pre–pandemic declaration group. This finding could potentially be explained by local stay-at-home orders that resulted in more strokes witnessed at home by family members, resulting in earlier presentation to the ED. Potentially, an overall decreased ED utilization for all medical conditions could also contribute to earlier telestroke activation. Additionally, there could be late-presenting patients who were not captured in our cohort due to presentation after 24 hours, thus not meeting criteria for telestroke activation. Despite this decreased time to telestroke activation, there was a reduction in the percentage of patients who received urgent stroke interventions (IV-tPA and/or thrombectomy). We noted that most of the patients who did not receive treatment had low NIHSS scores, suggesting mild stroke symptoms. The data in this regard were difficult to interpret because details on potential exclusion factors were not included as part of this review, and the number of patients in this group was small. However, this remains an area that may require further exploration to determine if urgent stroke treatment patterns are affected by the pandemic.
There were no other statistically significant variables between the pre–pandemic declaration and post–pandemic declaration groups. Interestingly, age did not appear to differ between the 2 groups despite the increased morbidity associated with COVID-19 in the elderly population. Based on reports of reduced ED presentations for less severe conditions during the Middle East respiratory syndrome epidemic, one may expect a reduction in the proportion of stroke mimics and transient ischemic attacks compared with ischemic stroke diagnoses.3 However, such reduction was not observed in our cohort. Although we did see a reduction in the proportion of stroke mimics in the post–pandemic declaration group, it did not achieve statistical significance. Likewise, among patients with a stroke diagnosis, the NIHSS score did not appear to be significantly different between the 2 groups.
Conclusion
A clinically important reduction in telestroke activations was seen in the 30 days following the WHO declaration of the COVID-19 pandemic. This reduction mirrors early data regarding reduction of ST-segment elevation myocardial infarction as well as single-center reports of reduced stroke volumes and interventions globally. At this early stage, it is difficult to identify the underlying cause of this change, and it may very well be multifactorial. Moving forward, it will be important to identify patient and physician factors that may contribute to underutilization of stroke emergency services.
Footnotes
Potential Competing Interests: The authors report no competing interests.
References
- 1.Mao L., Wang M., Chen S. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. medRxiv website. https://www.medrxiv.org/content/10.1101/2020.02.22.20026500v1 Published February 25, 2020. Accessed April 24, 2020.
- 2.Lyden P. American Heart Association/American Stroke Association Stroke Council Leadership. Temporary emergency guidance to US stroke centers during the COVID-19 pandemic. Stroke. 2020;51(6):1910–1912. doi: 10.1161/STROKEAHA.120.030023. [DOI] [PubMed] [Google Scholar]
- 3.Lee S.Y., Khang Y.-H., Lim H.-K. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60(8):796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paek S.H., Kim D.K., Lee J.H., Kwak Y.H. The Impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017;32(10):1576–1580. doi: 10.3346/jkms.2017.32.10.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao J., Rudd A., Liu R. Challenges and potential solutions of stroke care during the coronavirus disease 2019 (COVID-19) outbreak. Stroke. 2020;51(5):1356–1357. doi: 10.1161/STROKEAHA.120.029701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morelli N., Rota E., Terracciano C. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era [letter; published online ahead of print April 14, 2020] Eur Neurol. 2020 doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [letter] J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]