Abstract
Disasters, including infectious disease outbreaks, are inevitable. Hospitals need to plan in advance to ensure that their systems can adapt to a rapidly changing environment if necessary. This review provides an overview of 10 general principles that hospitals and health-care systems should consider when developing disaster plans. The principles are consistent with an “all-hazards” approach to disaster mitigation. This approach is adapted to planning for a multiplicity of threats but emphasizes highly relevant scenarios, such as the coronavirus disease 2019 pandemic. We also describe specific ways these principles helped prepare our hospital for this pandemic. Key points include acting quickly, identifying and engaging key stakeholders early, providing accurate information, prioritizing employee safety and mental health, promoting a fully integrated clinical response, developing surge plans, preparing for ethical dilemmas, and having a cogent exit strategy for post-disaster recovery.
Key Words: review, stress, topics in practice management, viral disease
Abbreviations: CDC, Centers for Disease Control and Prevention; COVID-19, coronavirus disease 19; HCW, health-care worker; ICC, Incident Command Center; PPE, personal protective equipment; SARS, severe acute respiratory syndrome; WHO, World Health Organization
In December 2019, clustered cases of unusual pneumonia developed among individuals exposed to the Huanan Seafood Market in Wuhan, China. The etiology was subsequently identified as a novel coronavirus (CoV), similar to the severe acute respiratory syndrome (SARS)-CoV outbreak in 2002 to 2003.1 In 4 months, SARS-CoV-2, the virus that causes CoV disease 2019 (COVID-19), spread around the globe, challenging the ability of governments and health-care systems to respond. The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020.2
Health-care systems are usually prepared for endemic, or typical, levels of disease in the population. During an epidemic, hospitals may need to increase capacity to accommodate surges in clinical demand. This scenario has been especially true with COVID-19.
The Centers for Disease Control and Prevention (CDC) estimates that the 2009 H1N1 pandemic infected 60.8 million individuals. Approximately 275,000 individuals were hospitalized and 12,500 individuals died.3 COVID-19 has surpassed H1N1 in scope and tested the capacity of health care in most regions of the world.4 We propose 10 principles that hospitals and health-care systems should consider when developing disaster plans. The principles fit into an “all-hazards” approach that addresses a multiplicity of threats but emphasizes highly relevant scenarios such as COVID-19. We also describe specific ways our hospital applied the principles in response to COVID-19.
Principle 1: Do Not Wait
The most effective time for disaster planning is prior to a surge of demand on a health-care system. The WHO advocates using an all-hazards approach to emergency preparedness and program design before a disaster is imminent,5 based on the observation that preparedness strategies for most disasters require similar coordination and planning. Hospitals should create general disaster preparedness plans with contingencies for specific threats based on the likelihood and impact to their institution.
Most of the WHO recommendations grew out of the response to the 2014 Ebola outbreak. Since we rehearsed extensively for that threat and debriefed thoroughly following it, we were better positioned for COVID-19. One example was our communication strategy. One of the first steps in our preparations was the deployment of a COVID-19 toolkit on our institutional intranet. The toolkit used existing infrastructure and was easily accessible and centrally managed. Providers could search and identify critical information about COVID-19, policies, procedures, training, and other resources. Despite COVID-19’s novelty, utilizing the structures already in place let us move quickly in addressing COVID-19-specific issues.6
Principle 2: Engage Key Stakeholders
Many planners make the mistake of limiting early engagement to executive leadership. Although qualified leadership is essential, a command structure that engages the full array of hospital operations is essential.7 Input from many partners allows for delegation of workload, refinement of ideas, and accountability across large teams (Table 1 ).6
Table 1.
Examples of Key Stakeholders
| Emergency management |
| Infection control |
| Infectious disease |
| Surgery |
| Critical care |
| Internal medicine |
| Pharmacy |
| Nursing |
| Respiratory therapy |
| Laboratory medicine |
| Microbiology |
| Palliative medicine |
| Medical education |
| Supply chain |
| Security |
| Spiritual care |
| Environmental services |
| Food services |
| Occupational health |
| Human resources |
| Employee wellness |
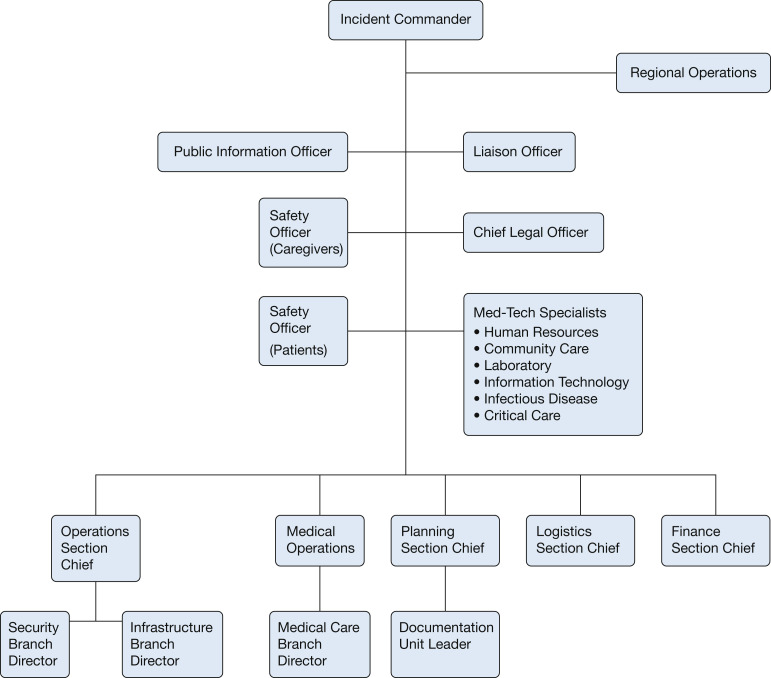
In our institution, we used incident command models to achieve these goals. At the enterprise level, the Incident Command Center (ICC) was activated early in the course of planning for the crisis. The ICC comprises key clinical and operational leaders within the health system (Fig 1 ). The ICC convened several working groups to identify, develop, and maintain communication and collaboration among key institutional, local, and state stakeholders as well as other local hospitals and the public. Regular planning and communication among these entities allowed us to coordinate strategy at the regional and local levels and to escalate high-priority items for rapid resolution.
Figure 1.
Incident management team for coronavirus disease 2019. Med-Tech = medical technology.
Within the health system, multiple smaller incident command models were also established to address specific issues. Within the respiratory institute, a twice-daily call was convened for caregivers leading the ICU and infectious disease responses. These calls offered a granular view of key operational issues and offered real-time feedback regarding opportunities and threats to COVID-19 preparations and ongoing care.
The incident command forums were also a great opportunity to share stories of inspiration and hope in the high-stress environment. These messages are frequently the final element of meetings. They have provided unity, camaraderie, pride, and motivation throughout the COVID-19 crisis.
Principle 3: Identify Sources of Truth
Misinformation is common during disasters. Although social media has provided a rapid way to disseminate information, distinguishing fact from speculation can be difficult. Although most contributors are well intentioned, the rapid, unregulated nature of these platforms carries risk.8 Misinformation can be harmful in many ways, especially as people in a spirit of panic adopt ill-advised practices to protect themselves or ignore genuinely helpful measures that would protect them.9 COVID-19 misinformation has been so widespread that the CDC formed a Webpage titled “Stop the Spread of Rumors.”10 It is important to identify trustworthy and accessible “sources of truth” to guide individuals to accurate and reliable information. Governmental organizations such as the CDC function as reliable sources of information during infectious outbreaks and other health crises. We identified the CDC as our “source of truth,” reiterated on our COVID-19 toolkit Website, reinforced in meetings, and referenced in educational materials. When other sources were used, they were clearly referenced.
Despite guidance from reputable sources, there remain areas of uncertainty in a disaster. To foster discussion of these issues, we set up internal discussion forums among our providers. These served to vet areas of uncertainty, propose new ideas, and reinforce best practices. The first forums were created as text messaging groups and were monitored by a designated “content expert.” Later, we used an internal, Web-based chat board. In many cases, these discussions clarified uncertain areas within the enterprise response, which were then communicated more broadly via the COVID-19 toolkit.
Health-care workers (HCWs) are often considered experts in such a crisis. Our institution has benefited from the expertise of many, who through internal debate and discussion were able to help generate institution-specific guidelines, especially when national guidelines were ambiguous or rapidly changing. However, we caution our caregivers from relying on, or propagating on social media, nonvalidated information that might be interpreted as “official” by others using these platforms.
Principle 4: Promote Creativity
It is challenging to envision all the details that allow a hospital to function on a daily basis and still more challenging to model how these details will be affected by a disaster. One way to encourage innovative thinking is scenario simulation. A scenario is presented (eg, during a surge, a certain resource is exhausted) to a group of stakeholders. Targeted questions help the team identify operational barriers, pathways, and policies that need to be revised.
During 2014, the spread of Ebola outside of Western Africa led hospitals to plan for possible cases.11 Leaders at Ottawa Hospital in Ontario, Canada (a dedicated Ebola patient care site), held focus groups and performed walk-throughs of patient care areas, identifying important themes to improve safety and enhance health-care delivery.
Recognizing the benefits of these exercises, we convened a multidisciplinary team of physicians, nurses, therapists, unit coordinators, and quality improvement specialists, and created a simulated ICU room. In multiple simulations, providers ran through scenarios for both COVID-19 patient care and “normal” patient care, highlighting ways in which caring for patients with COVID-19 differs from routine ICU care. Hundreds of potential interventions were explored, and the impact, cost, and effort for each were analyzed. We then incorporated high-impact, low-cost initiatives into clinical care, such as banning white coats from the ICU, using tablets with videoconference capabilities in patient rooms, and disconnecting the control displays from our ventilators so they could be accessed without entering the room. Using a “plan, do, study, act” cycle, we improved on initial ideas. Teams of clinician educators went to our regional hospitals to implement these “best practices” throughout the health-care system.
Principle 5: Prioritize Hospital Employee Safety and Well-being
Safety of personnel is critically important during an outbreak, both for their personal well-being and for the role these individuals play in managing the disaster. Adequate supply and proper use of personal protective equipment (PPE) is a priority. Poor PPE utilization affects caregiver safety and confidence. During the 2009 H1N1 outbreak,12 the CDC’s priorities to prevent infections among HCWs included appropriate PPE use. Despite this, an estimated 50% of HCWs infected with H1N1 acquired it through workplace exposure, with a majority reporting poor adherence with PPE protocols.13
We believe the well-being of everyone depends on prioritizing caregiver safety. Early on, we created videos demonstrating proper donning and doffing of PPE when treating COVID-19 patients. All providers were required to watch the videos and attend in-person simulation training to reinforce appropriate techniques. Compliance with proper donning and doffing improved, but overall adherence was still not ideal. Analysis showed that caregivers thought they were donning and doffing correctly even if they were not. This led to a “buddy system” within our COVID-19 units in which employees were trained to observe each other donning or doffing and give immediate feedback.
Beyond enforcing proper PPE, multiple additional wellness initiatives have been adopted. Resources, including stress management and counseling, are available and publicized on the COVID-19 toolkit site and elsewhere. Coffee and individually wrapped snacks are available for HCWs throughout the day and night. Capitalizing on a temporary restriction against visitors in our hospitals, we expanded caregiver work spaces into unused visitor waiting areas to enhance social distancing among providers. Caregivers possibly infected with COVID-19 can receive expedited drive-through testing and counseling with a simple telephone call. Virtual rounding with video conference technology allows team members to communicate while maintaining safe distances. Each measure helps build an environment in which providers feel they are part of a team where their safety is prioritized.
Principle 6: Prioritize Collaboration
Most HCWs want to work during disasters, but lack of early coordination and collaboration can be catastrophic.9 After Hurricane Katrina in 2006, thousands of medical volunteers presented to the Gulf Coast to assist but failure to engage them impaired an effective response.14 Early organization, direct communication, and clarity of roles allow for effective mobilization of workers as a unified team and prevent duplicate or conflicting efforts.
Similar to Hurricane Katrina, COVID-19 has created interest among HCWs and local communities to assist. Early in our planning process, education leaders began creating a platform to educate physicians in COVID-19 care and to provide training for noninternists who might be redeployed to internal medicine wards or ICUs. Other provider groups were interested in creating training resources as well. To avoid duplicative efforts and internal competition, we recruited leaders from interested groups to assist with the design and coordinate implementation of our learning platform. Together, we created a comprehensive, multidisciplinary platform with a COVID-specific care resource, 41 pre-deployment video-based training modules, and >110 disease-specific topic guides for practitioners to access while deployed (healthcareedu.ccf.org). Keys to our success were setting clear expectations of each group’s role and a clear vision of the end product.
We also used this crisis to collaborate with our local communities. For example, after the CDC recommended the use of cloth masks in public settings, we partnered with local Amish communities in Northeast Ohio who sewed thousands of cloth masks for hospital employees to wear in non-COVID areas of the hospital.
Principle 7: Anticipate Resource Needs
Disasters are inherently resource-limited settings because of inadequate planning, scarcities created by the disaster itself, or both. This applies to material resources and to personnel. Hospitals should anticipate staffing needs for all roles involved in patient care. This includes ancillary providers such as laboratory support, information technology, and pharmacy services. Elective surgeries and procedures can be canceled to allow space, personnel, and material flexibility. Existing patients should be transferred as needed, based on the appropriate level of care.12
With COVID-19, hospitals have struggled to maintain adequate PPE, including N95 masks. An inventory audit showed we had sufficient N95 masks for 1 year under normal circumstances; however, hospitals should assume higher rates of PPE utilization during respiratory virus outbreaks. A significant increase in use and fractured supply chains forced us to conserve masks. Data on droplet transmission of COVID-19 allowed us to conserve N95 masks by initially using them only for high-risk procedures (eg, intubation, bronchoscopy). Following our transition to COVID-19 cohort units, providers were taught how to reuse N95 masks on those units. Entry to patient rooms was minimized to one provider per clinical team, whose physical examination served as the basis for consultant examinations in most cases. In light of ongoing supply chain shortages, we partnered with a local company to sterilize used N95 masks. These efforts reduced concerns around N95 availability and highlight a multimodal approach to ensuring adequate material supplies during a disaster.
Material resources are only one element of the essential resources hospitals rely on. In a disaster situation such as COVID-19, hospital employee shortages occur for many reasons. In March, one article reported on a hospital in Italy where > 450 nurses were unable to work.15 Several of these nurses were incapacitated for reasons other than COVID-19 infection. Examples such as these highlight the need for employees to be flexible in their roles. We anticipated potential shortages by embedding non-ICU nurses and physicians within existing ICU teams to learn skills and workflows should they be redeployed. Feedback suggests this strategy has improved communication and lowered anxiety among redeployed providers.
Principle 8: Prioritize Mental Heath
Outbreaks are stressful for HCWs and their families. Fears include the risk of personal illness, spreading it to others, inability to continue working, and potential stigmatization, all of which contribute to psychological distress.16 Fears for personal safety are not unfounded. During the SARS outbreak, infections among HCWs were common, despite use of PPE.17 A survey of HCWs during the H1N1 pandemic found that fear of infection was associated with absenteeism, restriction of social contacts, and psychological distress.18
Although institutional counseling resources are helpful, caregiver support does not necessarily require funded support from institutions. For example, we created a COVID Peer Support Task Force to assist hospital employees during the COVID-19 crisis. These volunteer employee groups from various departments are available via telephone to talk through concerns with their peers. This program exists in addition to professional counseling but was rapidly deployable and required minimal institutional investment beyond granting time for the activities. Another effort identified providers according to where they live and established small neighborhood-based support groups. These have been a welcome addition to providers with child care issues, who are quarantined or otherwise need support near home.
In addition to peer support, it is important for hospital leaders to acknowledge the stress and fears of HCWs. The institution can act to address those fears. Following the SARS outbreak, studies did not find increased mental health disorders among HCWs but rather increased stress, absenteeism, and professional burnout. Caregivers who felt adequately trained and supported by their hospitals were less likely to experience long-term stress.19 A key concern among our health-care providers has been fear of disease transmission to loved ones. To address this concern, caregivers working in COVID-19 units or who have been infected with COVID-19 can access free alternative housing provided through partnership between our hospital and local hotels. Actions such as these address real needs and bolster workforce engagement both during a crisis and long afterward.
Principle 9: Anticipate Ethical Dilemmas
Disasters create ethical dilemmas unique from everyday practice. Medical ethics are based on the four principles of beneficence, non-maleficence, autonomy, and justice. The priority placed on each of these values may need to shift during a disaster, as the good of individuals comes into conflict with the good of society.20 Triage of patients and allocation of resources may make HCWs unfamiliar with working in resource-limited settings uncomfortable. According to the 2017 World Medical Association’s Statement on Medical Ethics in the Event of a Disaster, strategies for triage should prioritize saving the “maximum number of individuals” while maintaining compassion and respect for the dignity of all patients. Guidelines from the American College of Chest Physicians emphasize the need for appropriate triage planning, as modeling data show that selecting appropriate patients for critical care interventions, rather than on a “first come, first serve basis,” saves lives and increases overall access to care.21 These decisions should be based on individual patients’ “medical status and predicted response to treatment,” and should be compliant with local, regional, and national guidelines.20 , 22
During an infectious outbreak, difficult decisions are often required regarding allocation of care. Institutions must have a plan for resource allocation and triage. The Italian College of Anesthesia, Analgesia, Resuscitation, and Intensive Care issued recommendations specific to COVID-19 to alleviate the emotional burden of triaged care and provide allocation criteria for health-care resources.23 We recommend having a team (palliative care, legal, clinicians, and administration) perform tabletop exercises to develop recommendations on resource allocation. Ideally, general discussions should occur prior to an actual disaster, as part of an all-hazards planning process. Guidance from these discussions can then be tailored to an immediate disaster scenario.
Principle 10: Plan for Recovery
One of the most difficult issues to imagine in the early stages of disaster planning is how to transition back to a “new normal.” This piece is often overlooked but is essential.24 The Federal Emergency Management Agency and other organizations provide resources for hospitals and communities to navigate this unfamiliar territory.25 Keys to recovery planning include many of the same principles used in planning for the actual disaster. These include collaboration, effective communications through an incident command structure, identifying potential system failures or resource limitations, and coordinating local, regional, and national resources.
In our hospital, task forces have convened to advise on topics such as how to resume elective surgical procedures, how to modify the physical space for long-term social distancing, and how to optimize virtual health care as a long-term option for patients. For example, we have implemented cell phone-based virtual check-in for outpatient appointments to allow people to avoid crowded waiting areas and lines.
Early consideration of long-term recovery issues can help shape initial disaster planning. Peer support and mental health capabilities can scale for immediate and long-term needs. Changes in hospital workflow offer opportunities to address pre-disaster concerns, and investments in technology may anticipate both short- and long-term needs. For example, prior to this pandemic, virtual visits were encouraged, but many providers avoided them as the video platform was slow and cumbersome to use. In response to COVID-19, the health-care system was forced to rapidly expand the use of virtual visits, and we decided to replace the old system with a new platform with direct integration with our electronic medical record. The hope in these changes is to leverage spending from a short-term crisis to the benefit of long-term systemic improvement.
Conclusions
Disasters and outbreaks have coexisted with humanity since antiquity and will continue to remain an inevitable part of human existence.26 Disaster preparedness planning should be incorporated into routine hospital functioning. An integrated clinical and operational response will allow hospitals to mobilize available resources at the time of an incident to provide the highest standard of care to critical patients. Although preparedness for all disasters share common themes, our understanding of any specific disaster evolves as the disaster unfolds. These principles are derived from the literature on disaster management and our own hospital’s experiences managing the COVID-19 pandemic. Although this outbreak is still unfolding, we believe these principles have prepared and empowered our health-care workforce, and we offer them as an aid to those who are working to adapt to the current emergency, as well as to those who will work similarly in the future.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General’s opening remarks at the media briefing on COVID-19, 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3.Centers for Disease Control and Prevention H1N1 flu, CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the United States, April 2009-January 16, 2010. https://www.cdc.gov/h1n1flu/estimates_2009_h1n1.htm
- 4.ProPublica Are hospitals near me ready for coronavirus? Here are nine different scenarios. https://projects.propublica.org/graphics/covid-hospitals
- 5.World Health Organization Global assessment of national health sector emergency preparedness and response. https://www.who.int/publications-detail/global-assessment-of-national-health-sector-emergency-preparedness-and-response
- 6.Daugherty E.L., Carlson A.L., Perl T.M. Planning for the inevitable: preparing for epidemic and pandemic respiratory illness in the shadow of H1N1 influenza. Clin Infect Dis. 2010;50(8):1145–1154. doi: 10.1086/651272. [DOI] [PubMed] [Google Scholar]
- 7.Subbarao I., Lyznicki J.M., Hsu E.B. A consensus-based educational framework and competency set for the discipline of disaster medicine and public health preparedness. Disaster Med Public Health Prep. 2008;2(1):57–68. doi: 10.1097/DMP.0b013e31816564af. [DOI] [PubMed] [Google Scholar]
- 8.Homeland Security Science and Technology. Countering false information on social media in disasters and emergencies. https://www.dhs.gov/publication/st-frg-countering-false-information-social-media-disasters-and-emergencies
- 9.Cone D.C., Cummings B.A. Hospital disaster staffing: if you call, will they come? Am J Disaster Med. 2006;1(1):28–36. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Stop the spread of rumors. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/share-facts.html
- 11.Sarti A.J., Sutherland S., Robillard N. Ebola preparedness: a rapid needs assessment of critical care in a tertiary hospital. CMAJ Open. 2015;3(2):E198–E207. doi: 10.9778/cmajo.20150025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hick J.L., Christian M.D., Sprung C.L. Chapter 2. Surge capacity and infrastructure considerations for mass critical care. Inten Care Med. 2010;36(suppl 1) doi: 10.1007/s00134-010-1761-4. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Intervention. Novel influenza A (H1N1) virus infections among health-care personnel—United States, April–May 2009. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5823a2.htm [PubMed]
- 14.Franco C., Toner E., Waldhorn R., Maldin B., O’Toole T., Inglesby T.V. Systemic collapse: medical care in the aftermath of Hurricane Katrina. Biosecurity Bioterrorism. 2006;4(2):135–146. doi: 10.1089/bsp.2006.4.135. [DOI] [PubMed] [Google Scholar]
- 15.The New York Times ‘It’s Like a War.’. https://www.nytimes.com/2020/03/17/podcasts/the-daily/italy-coronavirus.html
- 16.Maunder R.G., Lancee W.J., Rourke S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosomatic Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 17.Ofner M., Lem M., Sarwal S., Vearncombe M., Simor A. Cluster of severe acute respiratory syndrome cases among protected health care workers—Toronto, April 2003. Can Commun Dis Rep. 2003;29(11):93–97. [PubMed] [Google Scholar]
- 18.Goulia P., Mantas C., Dimitroula D., Mantis D., Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maunder R.G., Leszcz M., Savage D. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008;99(6):486–488. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozge Karadag C., Kerim Hakan A. Ethical dilemmas in disaster medicine. Iran Red Crescent Med J. 2012;14(10):602–612. [PMC free article] [PubMed] [Google Scholar]
- 21.Maves R.C., Downar J., Dichter J.R. Triage of scarce critical care resources in COVID-19 An implementation guide for regional allocation: an Expert Panel Report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest. 2020;158(1):212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WMA, The World Medical Association WMA statement on medical ethics in the event of disasters. https://www.wma.net/policies-post/wma-statement-on-medical-ethics-in-the-event-of-disasters/ [PubMed]
- 23.Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382(20):1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 24.Schultz C.H., Koenig K.L., Whiteside M., Murray R. Development of national standardized all-hazard disaster core competencies for acute care physicians, nurses, and EMS professionals. Ann Emerg Med. 2012;59(3):196–208.e1. doi: 10.1016/j.annemergmed.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Essential Functions and Considerations for Hospital Recovery. https://www.urmc.rochester.edu/MediaLibraries/URMCMedia/flrtc/documents/Essential-Functions-and-Considerations-of-Hospital-Recovery.pdf
- 26.Dara S.I., Ashton R.W., Farmer J.C., Carlton P.K. Worldwide disaster medical response: an historical perspective. Critical Care Med. 2005;33(suppl):S2–S6. doi: 10.1097/01.ccm.0000151062.00501.60. [DOI] [PubMed] [Google Scholar]