Highlights
-
•
Students are comfortable with the adoption of innovative technologies.
-
•
The acceptability of Telemedicine Cabin was tested using the UTAUT2.
-
•
Telemedicine cabin could be an alternative in case of pandemic.
-
•
Results confirm the importance of Privacy Concern in the heath domain.
Keywords: Telemedicine Cabin, E-health, Digital natives, UTAUT, Smart health
Abstract
Telemedicine could solve the problem of the lack of infrastructure and insufficient number of qualified healthcare staff in many countries/regions. The aim of this research is to investigate the futures of such solution by having a better understanding of the acceptance of the Telemedicine Cabin by high-educated Millennials. To reach this goal, a survey was built using specific dimensions to measure the perception of Telemedicine Cabin, the Unified-Theory-of-Acceptance-and-Use-of-Technology 2nd version (UTAUT2) and finally the Personal Innovativeness and the Privacy Concern scales. Our sample was composed of 158 students from different Business Schools and data were analysed using a Partial Least Approach. Findings highlight the key role of all Telemedicine Cabin dimensions (Accessibility, Availability and Compatibility) on Performance Expectancy, the importance of three UTAUT2 constructs (Performance Expectancy, Price Value and Habit) and the negative impact of Privacy Concern on the Intention to Use a Telemedicine Cabin. In addition, results demonstrate that Personal Innovativeness does not affect the Intention to Use Telemedicine Cabin.
1. Introduction
Healthcare, as basic human need, has become a universal demand. It is probably one of the most important claims everywhere, in developed, developing and underdeveloped countries. Unfortunately, due to the lack of infrastructure and insufficient qualified healthcare staff, many countries cannot offer to their population enough quality healthcare services. To avoid or decrease the inequalities, the concept of e-health emerged. E-health refers to proposed health services using Internet (Lepore, Mettalo, Schiavone, & Landriani, 2018) and includes the use of many technologies such as computers, mobile phones, web sites, applications to give access to health care providers and care workforce (Alazzam et al., 2015). The purpose is to record and store administrative and medical information about patient (Bawack & Kamdjoug, 2018), to increase efficiency of physicians’ professional activities (Bruno et al., 2018), to improve quality of provided patient care and health outcomes and to decrease health costs (Farahani et al., 2018). Information and Communication Technology (ICT) in the domain of e-health integrates several concepts: (1) Telecare is using sensors to detect specific hazards or collect information which not necessary requires the users’ interventions (Duarte & Pinho, 2019); (2) Telehealth is using specific medical equipment from home to manage health by detecting potential problems or measuring physiological indices. Telehealth combines connected devices with cloud computing to improve the patient-centered practice and to reduce costs (Papa, Mital, Pisano, & Del Giudice, 2018); (3)Telemedicine or Teleconsultation (Gajanayake, Iannella, & Sahama, 2016) is focusing on the use of interactive audio-visual and data communications, that allows to reduce waiting time and health cost (Farahani et al., 2018), increase the quality of services provided to patients and the efficiency of medical staff (Jang, Kim, & Lee, 2016), and avoid inconveniences during travels to hospitals. Telemedicine is a good mean to control the elderly or individuals with specific diseases such as cardiovascular or diabetes issues to keep them at home instead of hospital. Nevertheless, using innovative technology, shouldn’t contribute to isolate them and increase the widening-digital-divide (Rogers & Mitzner, 2017).
Teleconsultation is a clinical act and cannot be considered as e-commerce (Simon & Lucas, 2014). Our research is focused on Telemedicine Cabin concept that presents diagnostic and treatment done remotely (Simon, 2016). This new domain of ICT in a health context provides two main benefits: a) to conduct an independent health check via telemetry; b) in case of emergency response to avoid the mobility’s limitations of patients or practitioners, and to reduce the waiting time of medical tests.
To use the technology, a patient enters inside the cabin, equipped with measuring devices and follows the different instructions on the screen. The functionalities allow to measure blood pressure (stethoscope) and saturation’s rate of blood oxygen, to verify weight, size and temperature, to test visual acuity and hearing, to make an electrocardiogram and finally to have a teleconsultation with a physician. Only few minutes are requested to collect and analyze data, the results are instantly forwarded to the physician connected with the patient. The physician can also ask and guide the patient for additional tests if needed. Students are part of the young adults (18–25 years old) who consult and make medical tests more rarely when they have minor health issues (Deeks, Lombard, Michelmore, & Teede, 2009).Thus, the implementation of Telemedicine Cabin within Business Schools and Universities could be one solution to enable medical consulting in the way that convinces digital natives.
Several models measure the acceptance of innovative technology such as the Technological-Acceptance-Model (TAM) developed by Davis (1989) and it’s extension TAM2 (Davis, Bagozzi, & Warshaw, 1989), the Unified-Theory-of-Acceptance-and-Use-of-Technology (UTAUT) developed by Venkatesh, Morris, Davis, and Davis (2003) and its extension UTAUT2 (Venkatesh, Thong, & Xu, 2012). For the purpose of this research, authors retained the UTAUT2 to measure the acceptance of Telemedicine Cabin based on the targeted population. Indeed, the UTAUT focusses more on employees’ acceptance when the UTUAT2 aims to predict innovative technology adoption by consumers (Venkatesh et al., 2012). UTAUT2 integrates new variables measuring the Habit, Hedonic Motivation and Price-Value, in addition of the UTAUT constructs (Performance-Expectancy, Effort-Expectancy, Social-Influence and Facilitating-Condition). Performance expectancies, referring to the utilitarian perception of a product or service, can be directly impacted by the functionalities proposed such as, in our study, following constructs: Availability, Compatibility and Accessibility. Current paper not only regards the acceptance of the Telemedicine by students with the Unified-Theory-of-Acceptance-and-Use-of-Technology 2nd version (UTAUT2), but also tests and discusses added variables to explain Digital Natives behaviour in the context of health such as Personal Innovativeness and Privacy Concern. The Personal Innovativeness construct measures user’s perception regarding his/her degree of innovation acceptance, the more individuals consider themselves as early adopters, the more they will be ready to adopt innovative technologies (Agarwal and Prasad, 1998). Privacy Concern is related to the fear about the potential disclosure of personal information regarding their health (Mcknight & Chervany, 2002).
To adress these subjects, following questions were raised:
R1
What dimensions of the Telemedicine Cabin impact the Performance-Expectancy?
R2
What constructs of UTAUT2 influence the Intention to Use Telemedicine Cabin by students?
R3
Is the Telemedicine cabin the future solution for student’s healthcare?
A survey was administered to students from different Business Schools and Universities in France. The article is organized as follow. First, we present the literature review on the mobilized constructs and the hypotheses. Second, we explain our methodology and analyse the sample. Third, we present the findings and discuss the results highlighting the theoretical and managerial implications. Finally, we suggest some limitations of the study and propositions for future research.
2. Theoretical background and hypotheses
During the past decade, a change of paradigm, within developed countries, was highlighted moving from the right of patients to be treated to their duty to stay healthy (Gille & Houy, 2014). Based on Hancock (1999) the health care system of the 21 st century must provide individual with solutions to maintain or improve their health fighting against inequalities in health management and insuring that hospital will be considered only as an emergency option. E-health concepts including Telecare, Telehealth, Teleconsultation and Telemedicine Cabin are summarized in the Table 1 .
Table 1.
Main concepts of e-healthcare.
| Dimension | Concept | References |
|---|---|---|
| Telecare | Use of sensors to improve security at home (including sensors to detect gas, smoke etc.). | Duarte & Pinho (2019) |
| Telehealth | Telehealth a sub-dimension of Telecare, using sensors to measure health. | Papa et al. (2018) |
| Teleconsultation | Remote consultation with a physician using devices such as a computer, tablet or mobile phone. | Gajanayake et al. (2016) |
| Telemedicine cabin | The Telemedicine Cabin is a combination of Telehealth (Medical equipment inside the cabin) plus a remote consultation with a physician (Teleconsultation) | Simon (2016) |
In previous research, the role of technology was highlighted to enhance independence & autonomy and improve quality of life (Rogers & Mitzner, 2017). From September 15th of 2018, the French Health Insurance has decided to reimburse medical consultations by videoconferences, using or not a Telemedicine Cabin at the same rate than a physical consultation. This strong signal demonstrates the importance of such solution for the French government. They expect the number of medical acts to move from 500 000 in 2019 to 1.4 million in 20221 . Indeed, Telemedicine solutions are already well implemented in United States of America, Canada but also in smaller European countries such as Switzerland with more than 4 million patients1. A survey realized by Ipsos (2018)2 , investigated the physicians and patients’ motivations to use Telemedicine solutions. Regarding the healthcare staff, more than ¾ of physicians and specialists are for the implementation of Telemedicine solutions and 68 percent of physicians already have remote interactions with their patients using mail, SMS or telephone. Regarding French patients, 60 percent admit they have sometimes decided not to consult mainly due to the waiting times too long for an appointment in relation with the urgency of the health problem encountered, the lack of time or the date proposed that didn’t fit with their agenda. Nevertheless, 38 percent considered that this difficulty to access to a physician could have been the cause of a worsening health problem. In addition, 1/3 of the French patients declare that they have already contacted their physician by phone for an advice.
Thus, based on this study, both physicians and patients considered that 50 percent of the consultation can be done using Telemedicine solutions.
2.1. Telemedicine Cabin dimensions
Telemedicine Cabin starts to be installed in Health centres, pharmacies, public places and even in working environment with the approvals of the Regional Health Agency (ARS), the National Union of complementary health insurance organizations (Unocam), and the National Commission for Informatics and Liberties (CNIL).
Nevertheless, this solution is not yet implemented in Business Schools or Universities. Telemedicine proposes benefits for young adults that represent digital natives, the generation of people born and grown up with digital technology (Baudier, Ammi, & Deboeuf-Rouchon, 2020). Digital natives are used to receive information fast (Prensky, 2001), so they can reduce time spent on medical tests and consultations with Telemedicine; they prefer graphics before text, and they work better by networking (Prensky, 2001), thus Telemedicine provides quick results and connects the patient and practitioner. The key benefits of a Telemedicine Cabin highlighted by the literature are (1) the capability to remotely and easily access to physician, (2) the availability of the services (time saving) and (3) the fact that using a Telemedicine Cabin can fit with their way of life and expectancies. (1) Accessibility for healthcare is related to the degree to which a patient believes the use of telemedicine service will simplify healthcare for individuals living far away from physicians or with mobility issues. (2) Availability is key for the adoption of healthcare solutions for both practitioners and patients answering their need to consult, when available (Bruno et al., 2018). (3) Compatibility is the degree to which technology is perceived by users as consistent with their values, experience, and needs. Compatibility is an important characteristic that positively influences the Performance Expectation of a technology (Jang et al., 2016). By using a Telemedicine Cabin, patients may consider that their performance can be enhanced by those three variables and thus have a positive impact on Performance-Expectancy.
Therefore, we hypothesize that
H1
The dimension of Accessibility of Telemedicine Cabin has a direct, positive and significant impact on Performance-Expectancy.
H2
Compatibility of Telemedicine Cabin has a direct, positive and significant impact on Performance-Expectancy.
H3
Availability of Telemedicine Cabin has a direct, positive and significant impact on Performance-Expectancy.
2.2. UTAUT (Unified-Theory-of-Acceptance-and-Use-of-Technology)
Several theories have been developed in order to measure the acceptance of new technologies. The UTAUT (Venkatesh et al., 2003) and its extension the UTAUT2 (Venkatesh et al., 2012) were based on different theories and models on technology acceptance such as the Innovation of Diffusion Theory (Rogers, 1962), the Technological-Acceptance-Model (Davis, 1989; Venkatesh & Davis, 2000) or the Theory of Reasoned Action (Fishbein & Ajzen, 1975). Many researchers examined the acceptance of e-health or telemedicine services using the UTAUT (Alazzam et al., 2015; Bawack & Kamdjoug, 2018; Duarte & Pinho, 2019; Gajanayake et al., 2016). The seven items of the UTAUT2 were mobilized to measure their impact on Intention-to-Use Telemedicine Cabin.
2.2.1. Effort-Expectancy
Effort-Expectancy is defined as the degree of simplicity associated with the use of a technology (Davis, 1989; Venkatesh & Davis, 2000; Venkatesh et al., 2012). Even if, according to Gao, Li, and Luo (2015)) Effort-Expectancy has no direct and significant impact on the Intention-to-Use wearable technology for fitness purposes, its impact is significant for medical reasons. Other researchers demonstrate that Effort-Expectancy can impact the Intention-to-Use new technologies in the health domain such as electronic health record (Pulidindi, Jinkab, & Priyac, 2016), telemedicine equipment (Kohnke, Cole, & Bush, 2014), mobile health (Sun, Wang, Guo, & Peng, 2013). We postulate that:
H4
Effort-Expectancy has a positive direct effect on Intention-to-Use Telemedicine Cabin.
2.2.2. Facilitating-Conditions
Facilitating-Conditions are defined as the degree to which an individual believes that an organizational and technical infrastructure exists to support the use of a technology (Venkatesh & Davis, 2000; Venkatesh et al., 2012). The construct includes aspects of the technological and/or organizational environment that are designed to remove barriers to use technology. Facilitating-Conditions have significant influence on the behavioral intention, but also direct impact on the use. According to Venkatesh et al. (2003) this predictor is strong in older generations, but on the other hand might be important for the medical context of use, when people even of younger generation are more worried about the technology performance (Duarte & Pinho, 2019; Schomakers, Lidynia, & Ziefle, 2018). We postulate that:
H5
Facilitating-Conditions has a positive direct effect on Intention-to-Use a Telemedicine Cabin
2.2.3. Habit
Habit has been defined as the extent to which people tend to perform behaviors automatically because of learning (Limayem, Hirt, & Cheung, 2007). Habit is important for the information technology use (Lally, Van Jaarsveld, Potts, & Wardle, 2010). Since individuals use today the information technology for shopping, payments, information, gaming, communication, we assume, that the targeted population (Digital Natives) has developed the habit for online (tele) communication and will adopt quickly the telemedicine services. Thus, Habit should positively influence Telemedicine Cabin’s adoption as demonstrated in recent studies on eHealth (Tavares & Oliveira, 2016). We suggest that:
H6
Habit has a positive direct effect on Intention-to-Use Telemedicine Cabin
2.2.4. Hedonic-Motivation
Hedonic-Motivation is defined as the fun or pleasure derived from using a technology, and it has been shown to play an important role in determining technology acceptance and use (Venkatesh et al., 2012). Nevertheless, users of technology related to health can be concerned about their health or be already impacted by health issues. Therefore, in such context, the influence of Hedonic-Motivation on the Intention-to-Use could be less important than for other technologies (Tavares & Oliveira, 2016). Nevertheless, due to the targeted population, the Telemedicine Cabin can arouse curiosity or the enjoyment of being in trend. We assume that:
H7
Hedonic-Motivation has a positive direct effect on Intention-to-Use Telemedicine Cabin
2.2.5. Performance-Expectancy
Originally, Performance-Expectancy is defined as the degree to which an individual believes that using a technology or system would improve his or her job performance (Venkatesh et al., 2003, 2012). In the context of this research, Performance-Expectancy presents the degree to which an individual believes that using a Telemedicine Cabin would improve his/her health and productivity by saving time.
Based on Gao et al. (2015), Intention to Use wearable technology for medical reasons is directly impacted by Performance-Expectancy seen as key for the adoption of e-health services (Lee & Lee, 2018; Sun et al., 2013). Therefore, we postulate that:
H8
Performance-Expectancy has a positive direct effect on Intention-to-Use Telemedicine Cabin.
2.2.6. Price-Value
The Price-Value is positive when the benefits of using a technology are perceived to be greater than the monetary cost and such Price Value has a positive impact on Intention-to-Use. Gao et al. (2015) demonstrate the direct, positive, and significant influence on Intention-to-Use Internet-of-thing (wearables) for wellbeing purposes. Thus, we hypothesize that:
H9
Price-Value has a positive direct effect on Intention-to-Use Telemedicine Cabin
2.2.7. Social-Influence
Social-Influence is defined as the degree to which an individual perceives that others believe he or she should use a technology (Davis, 1989; Venkatesh & Davis, 2000; Venkatesh et al., 2003, 2012). Social-Influence is a direct determinant of behavioral intention. Several studies confirmed the impact of Social-Influence on Intention-to-Use innovative products in the health domain such as healthcare telemedicine equipment (Kohnke et al., 2014), mobile health services (Sun et al., 2013), wearable technology (Gao et al., 2015). We suggest that:
H10
Social-Influence will have a positive direct effect on Intention-to-Use Telemedicine Cabin
2.3. Personal-Innovativeness
Personal-Innovativeness can be defined as an extent to which an individual is innovative by his or her perception of new idea or technology. This notion was introduced by Agarwal and Prasad (1998), who concluded that users whose personality can be described as innovative (e.g. people with interest towards innovation and/or new technologies) would rather try new technology as soon as possible (Baudier et al., 2020; Jackson, Mun, & Park, 2013). Since, the targeted population is comfortable with new smart technologies, we propose the following hypothesis:
H11
Personal-Innovativeness has a positive direct effect on Intention-to-Use Telemedicine Cabin
2.4. Privacy-Concern
The use of digital technology increases the level of uncertainty (Mcknight & Chervany, 2002) especially if individuals must disclose personal information. Privacy in telemedicine services refers to the extent to which using such services will disturb personal privacy (Tavares & Oliveira, 2016). Previous research showed that the Privacy-Concern differs between contexts and that users perceive the highest level of risk for a healthcare context influencing the behavioral intentions (Schomakers et al., 2018; Xu, 2019). The lack of confidence of patient on potential privacy issue could be a key issue for the adoption of telemedicine. Despite, all the advantages provided by such technology few studies focused on the Privacy-Concern issue. Thus, we postulate that:
H12
Privacy-Concern has a negative, direct, and significant impact on Intention-to-Use Telemedicine Cabin
3. Methodology
3.1. Sample and data collection
A sample of 159 valid answers was collected (Table 2 ). All respondents were from the digital native’s population, born after 1981 and considered as more sensitive to and knowledgeable about innovative technologies (Bennett, Maton, & Kervin, 2008) thus lest reluctant to adopt such technology (Howe & Strauss, 2000). The aim of the research was to analyse how they perceived the Telemedicine Cabin and how this new technology could address their expectations. Due to the size and the characteristics of the sample, the moderator effects cannot be analysed. Indeed, the male population (45) is to small compared to the female one (114). In addition, the respondents are from the same generation, students, preparing a master’s degree in Business Schools therefore age and experience don’t moderate the relationships of our model.
Table 2.
Sample Characteristics.
| Female | 77 % |
| Male | 23 % |
| 100 % | |
| Living in parents' home | 47 % |
| Living Alone | 53 % |
| 100 % | |
| Paris | 34 % |
| Suburbs of Paris | 66 % |
| 100 % |
3.2. Measures
A quantitative approach was selected, and the research model was built using and adapting existing scale (Appendix A) as the UTAUT2 variables measuring the acceptance of new technologies (Venkatesh et al., 2012), Personal-Innovativeness (Bloch, Brunel, & Arnold, 2003), Privacy-Concern (Featherman & Pavlou, 2003), Availability (Moores, 2012), Accessibility (Farahani et al., 2018), Compatibility (Taylor & Todd, 1995). The survey, using five-point Likert scale, was administrated to students from different Business Schools, preparing a master’s degree and volunteers to participate.
4. Results
A Partial Least Square approach was mobilized using SmartPLS3 to analyse the relationships between the constructs of the model.
4.1. Reliability and validities of the outer model
The loadings of the variables, the Composite Reliability and Cronbach’s Alpha, mobilized to control the reliability of the model, were above the recommended threshold of 0.7. The discriminant validity of all constructs was controlled by verifying that the square root of the Average Variance Extracted (AVE) of the construct was superior to the correlations of this construct with the other constructs. Convergent validity was confirmed as all the values of the AVE were above the recommended Threshold of 0.50. Thus, results of on the analysis of the outer model confirm the validity and reliability of the research model.
4.2. Inner model
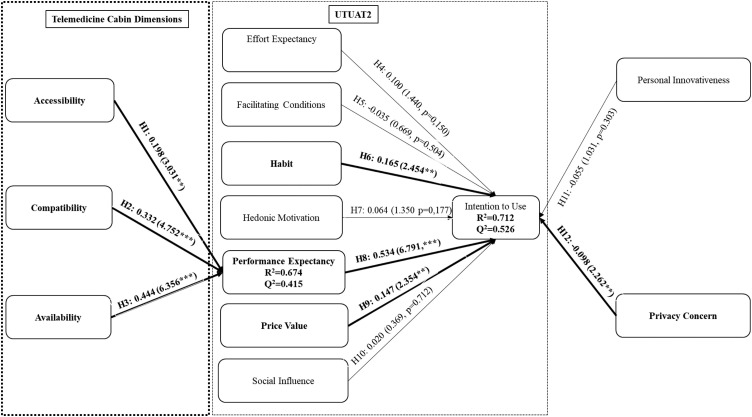
The inner model was tested by controlling the value of R2, f2, and Q2 of the endogenous variables. The relationships between constructs were controlled using the following parameters: t-value at more than the recommended threshold at 1.96, and p-value below 0.05 (Fig. 1 ). To explain the variance of the constructs, the R2 were examined. Our model explains 67.4 percent of Performance-Expectancy, determined by Accessibility (H1: Path-Coef = 0.198, t = 3.031, p = 0.002), Compatibility (H2: Path-Coef = 0.332, t = 4.752, p = 0.000) and Availability (H3: Path-Coef = 0.444, t = 6356, p = 0.000). The size effect (f2) confirm the huge impact of Availability (0.303) and Compatibility (0.213) on Performance-Expectancy. With a R2 at 0.712, our model explains 71.2 percent of Intention-to-Use determined by three of the UTUAT2 variables : Habit (H6: Path Coef = 0.165, t = 2.454, p = 0.014) and Price-Value (H9: Path-Coef = 0.147, t = 2.354, p = 0.019), both with a low impact (f2 =below 0.05) and by Performance-Expectancy (H8: Path-Coef = 0.534, t = 6.791, p = 0.000) with a huge impact on Intention-to-Use as f2 =0.404. Privacy-Concern impact negatively Intention-to-Use (H12: Path-Coef=-0.098, t = 2.262, p = 0.024). The other variables of the model such as Effort-Expectancy (H4), Facilitating-Conditions (H5), Hedonic-Motivation (H7), Social-Influence (H10), Personal-Innovativeness (H11) don’t impact Intention-to-Use Telemedicine Cabin, thus these hypotheses are rejected.
Fig. 1.
Research model with results.
The Blindfolding procedure was mobilized to calculate the Stone-Geisser's Q2. The Q2 of both Performance-Expectancy (0.415) and Intention-to-Use (0.526) greater than zero, indicate an acceptable predictive relevance of the model. Finally, the high value of the Goodness-of-Fit index at 0.71 confirms the quality of the model.
In summary, seven hypotheses were validated and five rejected.
5. Discussion
This study aimed to check the future of Telemedicine cabin and measure the acceptance of such solution on a specific target: The students from the digital native population. The findings of the current research demonstrate several unexpected effects giving a new vision on the Digital Natives behavior.
First, the results, that are aligned with previous studies, confirming that Compatibility positively influences the Perceived-Usefulness of a health technology and its Performance-Expectancy (Wu, Wang, & Lin, 2007; Lin, Tsai, Wang, & Chiu, 2011). Indeed, the use of a Telemedicine Cabin is considered as easy and obvious. Patients just need to integrate the distance aspect, as they must communicate with a physician remotely. Individuals can use this service, for example, when physicians are not available, when they have limited mobility, when they want to reduce waiting time (Lazar, Goldstein, & Taylor, 2015) or in case of major pandemic. The simplicity to use the Telemedicine Cabin has a positive effect on the digital accessibility and the degree of its Performance-Expectancy (Moser, 2006). Thus, Accessibility, one of the main advantages of telemedicine, affects positively the attractiveness of a medical product or service therefore also influences Performance-Expectancy. Furthermore, the reimbursement of the telemedical acts by the National French Social Security permits to offer these services without financial limitations (Stienstra, Watzke, & Birch, 2007). The availability of the Telemedicine Cabin (everywhere and anytime) is in adequation with the actual tendency to consume and to act without the limitations of time or location (Buchanan, Sainter, & Saunders, 2013) and is key to fit with patient’s Performance-Expectancy. Privacy-Concern, which refers to the potential disturbance of personal privacy (Schomakers et al., 2018; Tavares & Oliveira, 2016), has a direct and negative impact on the Intention-to-Use. Our results confirmed the prior research especially in the healthcare context (Bansal, Zahedi, & Gefen, 2015) particularly concerning vulnerable data.
Second, among the variables issued from the UTAUT2, the hypotheses regarding the impacts of Performance-Expectancy, Habit and Price-Value on the Intention-to-Use a Telemedicine Cabin have been validated and are consistent with previous research on same topics or on e-health domain. Thus, Performance-Expectancy has a considerable influence on the individual's Intention-to-Use Telemedicine cabin (Im, Hong, & Kang, 2011) confirming its utilitarian role. Habit is not limited to mere repetition of past behavior (Fischbein & Ajzen, 2010) and routine behavior but includes often characteristics such as unintentionality, uncontrollability, lack of awareness, and efficiency (Verplanken, 2010). In our study, the link between Habit and Intention-to-Use, validated by previous research (Ajzen, 2002), is also confirmed. Price-Value has usually a positive impact when the perception of the benefits of using a technology is greater than the cost. The Telemedicine Cabin is hindered by no additional cost following the compensation of the tele medical acts by the National French Social Security in 2018, therefore this hypothesis was validated in our study.
Third, the impact of fours variables of the UTAUT2 and Personal-Innovativeness on Intention-to-Use, often confirmed in the context of new technologies acceptance, is not validated for the adoption of the Telemedicine Cabin. We discuss these effects successively:
-
(1)
Effort-Expectancy (Davis, 1989) is key for the adoption of an innovative technology. Indeed, the convenience in using the technology and the compatibility of system influence positively the intent to use a technology (Prasanna & Huggins, 2016). The direct and positive relationship with the Intention-to-Use is, normally, validated especially for health products and services (Jang et al., 2016). This research was conducted among digital natives, who maybe do not feel that using such technology will need specific efforts. Thus, this variable seems not relevant for this population.
-
(2)
Based on several studies Facilitating-Conditions have a direct and positive relationship with the Intention-to-Use (Venkatesh & Davis, 2000; Venkatesh et al., 2012). Users are more motivated to adopt new technologies when they could have access to a technical expertise, training and a higher level of organizational support. Despite the confirmation of this relationship in many research, our results do not confirm a positive relation but are consistent with previous research (Baptista & Oliveira, 2015) supporting that Facilitating-Conditions has more influence in the case of actual usage rather than Intention-to-Use. Another reason provided by Venkatesh et al. (2003) is, linked to the profile of our sample, as Facilitating-Conditions are often stronger within older generation.
-
(3)
Research demonstrates the direct and positive impact of Social-Influence on the Intention-to-Use (Chang, 2015). Indeed, individuals could be influenced by relatives for the adoption of a new technology or a new technological product (Chaouali, 2016). In contrary of many previous research (Venkatesh et al., 2012), our results indicate a non-significant relation between Social-Influence and Intention-to-Use a Telemedicine Cabin. Even if digital natives are considered as “networked” generation (Prensky, 2001), who prefers to connect and support various social relations, the context of medical treatment is still the one that is very personal and individual, therefore Social-Influence has perhaps little or no impact.
-
(4)
Hedonic-Motivation has usually a positive link with Intention-to-Use (Childers, Carr, Peck, & Carson, 2001). Our results, which do not confirm this positive relationship, are supported by other research and could maybe be explained by the nature of the service from the health sector. A Telemedicine Cabin cannot be considered as a pleasure-oriented service but more perceived as an utilitarian solution. Prior research identified two types of central determinants of consumer buying behavior: Hedonic-Motivation focused on entertaining, fun and delightful aspects (Park, Kim, Funches, & Foxx, 2012; Verhagen & Van Dolen, 2011) and Utilitarian-Motivations (e.g. Telemedicine Cabin), focused in searching information about the usefulness of the product or service regarding the technology or the product (Babin, Chebat, & Michon, 2004).
-
(5)
Personal-Innovativeness, introduced by Agarwal and Prasad (1998), describes innovative people with strong interest towards innovation and/or new technologies (Baudier et al., 2020; Jackson et al., 2013). However, our results do not confirm this positive relationship for the Intention-to-Use Telemedicine Cabin. To explain this result, we can point out some research, which make the distinction between two levels of Innovativeness: (i) open-processing (or general) Innovativeness associated to a general predisposition to innovate from a cognitive perspective (Joseph & Vyas, 1984) and (ii) domain-specific Innovativeness limited to an area or a specific behavior (Goldsmith & Hofacker, 1991). Digital natives have a high degree of Innovativeness, but based on our findings, not on services related to e-health and Telemedicine Cabin. Moreover, our results are supported by the suggestions of Agarwal and Prasad (1998) who found specific relations between the individual’s weight of Innovativeness and the Effort-Expectancy. Our findings confirmed that both variables have been rejected.
Therefore, the implementation of Telemedicine Cabin within Business schools or Universities could be a good alternative.
6. Conclusion, limits and future research
According to Rees, Crampton, Gauld, and MacDonell (2018)), the future health systems will have to integrate social changes and health staff will have to change their working method. Despite of the growing interest in e-health, few studies focussed on the concept of the Telemedicine Cabin and its acceptance. The trending topic refers to the opportunity to consult a remote physician within Business Schools or Universities. The students, sometimes, need to face some specific problems such as finding (1) a physician in case they are far away from their region of origin (Accessibility issue) or (2) a gap in their agenda to visit him as they often have an active social daily life (Availability and Compatibility issues). Thus, they often wait until last minute before taking an appointment with a physician. Consequently, their health could be impacted, and the recovering cost could be higher for both the patient and the French administration. The results reveal that while Telemedicine Cabin can partially solve the issue of Government to reduce the health expenses by allowing student to easily and quickly access to medical care, deeper exploration regarding the acceptability of such solution need to be investigated. Indeed, the future of such solutions must be seriously studied as Telemedicine cabin or Teleconsultation could be a solution in case of pandemic period such as the COVID-19 where all contacts between physicians and patients need to be avoided and reserved to critical situations. In fact, in case of major contagion, hospitals cannot treat all patients and must focus on vital urgencies. Thus, the accessibility, availability and ease-of-use of Telemedicine cabin or Teleconsultation can be part of the Government plan to reduce the level of contamination by doing distant consultations even from home. Teleconsultation could protect all citizens. Indeed, the findings provide wide possibilities for the future research to check the perceptions of (1) Physicians (2) Hospital staff (3) Patients and (4) Government.
-
1
Physicians: In case of huge infection, physicians are often on the front line. Using distant solutions to consult could be for them an alternative to respect their Hippocratic Oath, to protect themselves against contamination in order to be available to treat a maximum of patients. Some companies offering remote consultation services through internet proposed free trail to French physicians to test their solution during the COVID19 infection. Thus, a study on their perception could be interesting as the more the physician will accept the technology and spread it, the more it will be accepted by individuals.
-
2
Hospital Staff: In case of major contagion, due to panic situations, contaminated people could go to the hospitals and contribute to extend the virus when staff must focus on patients in vital urgency. The physicians also need to protect themselves against a potential contamination, all medical staff must be on board. Therefore, an analysis of their perception of teleconsultation after the pandemic could be useful.
-
3
Patients: Individuals are scared because of pandemic. They try to avoid all contacts and are frightened to be obliged to stay in the physician waiting area for a consultation with other patients that could be infected especially if some of them demonstrate some symptoms of the illness (fever, cough). Even the more reluctant adopters could be interested by such solution. Thus, their perception is also key.
-
4
Government: As seen previously, French government already contribute to the extension of teleconsultation by reimbursing it. Nevertheless, the analysis of governments’ perception in different countries could provide comparison of the results. Thus, a cross- national study done at a government level could highlight the benefits and barriers of remote consultations.
Finding are aligned with the analysis published by Costa-Font and Sato (2012) on the health future systems. Indeed, their recommendations, to address future health challenges, were to increase the adoption of innovative health solutions, followed by the ability to prevent global diseases by improving prevention and finally to adjust financial models to healthcare insurances constraints. Indeed, research must considere the globalization’ effect especially in case of pandemic (Martens, 2002) and World Health Organization should reinforce the global surveillance of infectious diseases (Sapirie & Orzeszyna, 1995). Finally, the study has some limitations that can be regarded as opportunities for future research. First, the survey focused only on digital natives, and particularly students of French Business Schools or Universities, so the model should be tested using other samples such as other digital natives (Labor force) or digital immigrants (Labor force or retired). Indeed, Teleconsultation could enhance elderly autonomy (Rogers & Mitzner, 2017). In addition, due to the COVID19 infection, Future research should also control if after the pandemic period, the same population (students) reacts in the same way or if COVID19 had on impact on results. And secondly, it will be accurate to do an international study to check if results are the same depending on culture such as Asian or American cultures. This last point is critical especially due to the COVID-19 contamination at a worldwide level.
Acknowledgements
The authors would like to express their warmest thanks the Editor-in-Chief, Professor Ted Fuller, the Guest Editors, Professor Francesco Schiavone & Professor Marco Ferretti and the anonymous reviewers for their valuable comments that helped to improve drastically the quality of their article.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or Not-for-profit sectors.
Contributor Information
Patricia Baudier, Email: pbaudier@em-normandie.fr.
Galina Kondrateva, Email: gkondrateva@edcparis.edu.
Chantal Ammi, Email: Chantal.ammi@imt-bs.eu.
Appendix A. Questionnaire
Intention to Use (ITU)
ITU1: Using Telemedicine Cabin is worthwhile
IUT2: I intend to use Telemedicine Cabin in the future
ITU3: I predict I would use Telemedicine Cabin in the future
Performance Expectancy (PE)
PE1: I find the Telemedicine Cabin useful in my daily life
PE2: Using the Telemedicine Cabin would enable me to take care of my health faster.
PE3: Using the Telemedicine Cabin would increase my productivity
PE4: If I use the Telemedicine Cabin, I will increase my chances of improving my health
Effort Expectancy (EE)
EE1: My interaction with the Telemedicine Cabin would be clear and understandable
EE2: It would be easy for me to become skilful at using
EE3: I would find the telemedicine cabin easy to use
EE4: Learning to operate the system would be easy for me
Social Influence (SI)
SI1: People who are important to me think I should use the Telemedicine Cabin
SI2: My working environment influences my intention to use the Telemedicine Cabin
SI3: Using the Telemedicine Cabin would make me have a higher status than others who don’t
SI4: In general, the health staff encourages and supports the use of the Telemedicine Cabin in providing healthcare Services
Facilitating Conditions (FC)
FC1: I have the IT resources necessary to use the Telemedicine Cabin
FC2: I have the knowledge necessary to use the Telemedicine Cabin
FC3: Telemedicine Cabin uses similar technologies I’m familiar with
FC4: I can get assistance from others if I encounter difficulties with the use of the Telemedicine Cabin
Hedonic Motivation
HM1: Using the Telemedicine Cabin is fun
HM2: Telemedicine Cabin are enjoyable
HM3: Using the Telemedicine Cabin is very entertaining
Habit
HT1: Using the Telemedicine Cabin could become a habit for you
HT2: You could become « addict » using the Telemedicine Cabin
HT3: You could use a Telemedicine Cabin
HT4: Using the Telemedicine Cabin could become natural to you
Personal Innovativeness
PI1: You like to experiment with new information technologies
PI2: If you heard about a new technology, you would look for ways to experiment with it
PI3: Among your peers, you’re usually the first to try out new information technologies
Price Value
PR1: My social security card is accepted
PR2: My additional health insurance will reimburse the remaining cost
PR3: I don’t need to pay in advance as the Telemedicine Cabin accepts all my health insurance
PR4: The Telemedicine Cabin has a good price-performance ratio
PR5: The price is reasonable
Accessibility
AS1: The Telemedicine Cabin allows people living at distance to access care
AS2: The Telemedicine Cabin allows people who don’t see physicians often to take care of their health
AS3: The Telemedicine Cabin allows people with mobility problems to consult
Compatibility
COM1: I think the use of Telemedicine Cabin meets my expectations as to how to be treated
COM2: The use of the Telemedicine Cabin fits my lifestyle
COM3: Globally, the use of the Telemedicine Cabin is compatible with all the aspects of my life.
Availability
TIM1: Thanks to the Telemedicine Cabin, you could get the care needed on time
TIM2: With the Telemedicine Cabin, you could consult when you are available
TIM2: The Telemedicine Cabin will always be available when needed
Privacy Concerns
PC1: The use of Telemedicine Cabin could have some consequences such as the loss of control over the confidentially of your information
PC2: The use of Telemedicine Cabin could impact your private life as personal data could be used without your authorization
PC3: The use of Telemedicine Cabin is a direct access to your personal information
References
- Agarwal R., Prasad J. A conceptual and operational definition of personal innovativeness in the domain of information technology. Information Systems Research. 1998;9(2):204–215. doi: 10.1287/isre.9.2.204. [DOI] [Google Scholar]
- Ajzen I. Residual effects of past on later behavior: Habituation and reasoned action perspectives. Personality and Social Psychology Review. 2002;6(2):107–122. doi: 10.1207/S15327957PSPR0602_02. [DOI] [Google Scholar]
- Alazzam M.B., Basari A.S.H., Sibghatullah A.S., Doheir M., Enaizan O.M., Mamra A.H.K. Ehrs acceptance in Jordan hospitals by Utaut2 Model: Preliminary result. Journal of Theoretical and Applied Information Technology. 2015;78(3):473–482. [Google Scholar]
- Babin B.J., Chebat J.C., Michon R. Perceived appropriateness and its effect on quality, affect and behavior. Journal of Retailing and Consumer Service. 2004;11(5):287–298. doi: 10.1016/j.jretconser.2003.09.00. [DOI] [Google Scholar]
- Bansal G., Zahedi F.M., Gefen D. Do context and personality matter? Trust and privacy concerns in disclosing private information online. Information & Management. 2015;53(1) doi: 10.1016/j.im.2015.08.01. [DOI] [Google Scholar]
- Baptista G., Oliveira T. Understanding mobile banking: The unified theory of acceptance and use of technology combined with cultural moderators. Computers in Human Behavior. 2015;50:418–430. doi: 10.1016/j.chb.2015.04.024. [DOI] [Google Scholar]
- Baudier P., Ammi C., Deboeuf-Rouchon M. Smart home: Highly educated students’ acceptance. Technological Forecasting and Social Change. 2020;153:119355. doi: 10.1016/j.techfore.2018.06.043. [DOI] [Google Scholar]
- Bawack R.E., Kamdjoug J.R.K. Adequacy of UTAUT in clinician adoption of health information systems in developing countries: The case of Cameroon. International Journal of Medical Informatics. 2018;109:15–22. doi: 10.1016/j.ijmedinf.2017.10.016. [DOI] [PubMed] [Google Scholar]
- Bennett S., Maton K., Kervin L. The ‘digital natives’ debate: A critical review of the evidence. British Journal of Educational Technology. 2008;39(5):775–786. doi: 10.1111/j.1467-8535.2007.00793.x. [DOI] [Google Scholar]
- Bloch P.H., Brunel F.F., Arnold T.J. Individual differences in the centrality of visual product aesthetics: Concept and measurement. The Journal of Consumer Research. 2003;29(4):551–565. doi: 10.1086/346250. [DOI] [Google Scholar]
- Bruno E., Simblett S., Lang A., Biondi A., Odoi C., Schulze-Bonhage A. Wearable technology in epilepsy: The views of patients, caregivers, and healthcare professionals. Epilepsy & Behavior. 2018;85:141–149. doi: 10.1016/j.yebeh.2018.05.044. [DOI] [PubMed] [Google Scholar]
- Buchanan T., Sainter P., Saunders G. Factors affecting faculty use of learning technologies: Implication for models of technology adoption. Journal of Computing in Higher Education. 2013;25(1):1–11. doi: 10.1007/s12528-013-9066-6. [DOI] [Google Scholar]
- Chang C.C. Exploring mobile application customer loyalty: The moderating effect of use contexts. Telecommunication Policy. 2015;39(8):678–690. doi: 10.1016/j.telpol.2015.07.008. [DOI] [Google Scholar]
- Chaouali W. Once a user, always a user: Enablers and inhibitions of continuance intention of mobile social networking sites. Telematics and Informatics. 2016;33(4):1022–1033. doi: 10.1016/j.tele.2016.03.006. [DOI] [Google Scholar]
- Childers T.L., Carr C.L., Peck J., Carson S. Hedonic and utilitarian motivations for online retail shopping behavior. Journal of Retailing. 2001;77(4):511–535. doi: 10.1016/S0022-4359(01)00056-2. [DOI] [Google Scholar]
- Costa-Font J., Sato A. Health systems futures: The challenges of technology, prevention and insurance. Futures. 2012;44(7):696–703. doi: 10.1016/j.futures.2012.04.009. [DOI] [Google Scholar]
- Davis F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13(3):319–340. doi: 10.2307/249008. [DOI] [Google Scholar]
- Davis F.D., Bagozzi R.P., Warshaw P.R. User acceptance of computer technology: A comparison of two theoretical models. Management Science. 1989;35(8):982–1003. doi: 10.1287/mnsc.35.8.982. [DOI] [Google Scholar]
- Deeks A., Lombard C.B., Michelmore J., Teede H.J. The effects of gender and age on health related behaviors. BMC Public Health. 2009;9(213):1. doi: 10.1186/1471-2458-9-213. devo8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte P., Pinho J.C. A mixed methods UTAUT2-based approach to assess mobile health adoption. Journal of Business Research. 2019;102:140–150. doi: 10.1016/j.jbusres.2019.05.022. [DOI] [Google Scholar]
- Farahani B., Firouzi F., Chang V., Badaroglu M., Constabt N., Mankodiya K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and Healthcare. Future Generations Computer Systems: FGCS. 2018;78(2):659–676. doi: 10.1016/j.future.2017.04.036. [DOI] [Google Scholar]
- Featherman M.S., Pavlou P.A. Predicting e-Services adoption: A perceived risk facets perspective. International Journal of Human-computer Studies. 2003;59:451–474. doi: 10.1016/S1071-5819(03)00111-3. [DOI] [Google Scholar]
- Fishbein M., Ajzen I. Addison-Wesley Publishing Company; Don Mills: 1975. Belief, attitude, intention and behavior: An introduction to theory and research. [Google Scholar]
- Gajanayake R., Iannella R., Sahama T. An insight into the adoption of accountable-ehealth systems–an empirical research model based on the Australian context. IRBM. 2016;37(4):219–231. doi: 10.1016/j.irbm.2016.01.002. [DOI] [Google Scholar]
- Gao Y., Li H., Luo Y. An empirical study of wearable technology acceptance in healthcare. Industrial Management & Data Systems. 2015;115(9):1704–1723. doi: 10.1108/IMDS-03-2015-0087. [DOI] [Google Scholar]
- Gille L., Houy T. The future of Health care demand in developed countries: From the “right to treatment” to the “duty to stay healthy”. Futures. 2014;61:23–32. doi: 10.1016/j.futures.2014.04.013. [DOI] [Google Scholar]
- Goldsmith R.E., Hofacker C.F. Measuring consumer innovativeness. Journal of the Academy of Marketing Science. 1991;19(3):209–221. doi: 10.1007/BF02726497. [DOI] [Google Scholar]
- Hancock T. Health Care reform and reform for health: Creating a health system for communities in the 21st century. Futures. 1999;31(5):417–436. doi: 10.1016/S0016-3287(99)00003-8. [DOI] [Google Scholar]
- Howe N., Strauss W. Vintage Books; New York, NY: 2000. Millennials rising: The next great generation. [Google Scholar]
- Im I., Hong S.T., Kang M.S. An international comparison of technology adoption: Testing the UTAUT model. Information & Management. 2011;48(1):1–8. doi: 10.1016/j.im.2010.09.001. [DOI] [Google Scholar]
- Jackson J.D., Mun Y.Y., Park J.S. An empirical test of three mediation models for the relationship between personal innovativeness and user acceptance of technology. Information & Management. 2013;50(4):154–161. doi: 10.1016/j.im.2013.02.006. [DOI] [Google Scholar]
- Jang S.H., Kim R.H., Lee C.W. Effect of u-healthcare service quality on usage intention on a healthcare service. Technological Forecasting and Social Change. 2016;113:396–403. doi: 10.1016/j.techfore.2016.07.030. [DOI] [Google Scholar]
- Joseph B., Vyas S.J. Concurrent validity of a measure of innovative cognitive style. Journal of the Academy of Marketing Sciences. 1984;12(2):159–175. doi: 10.1007/BF02729494. [DOI] [Google Scholar]
- Kohnke A., Cole M.L., Bush R. Incorporating UTAUT predictors for understanding home care patients’ and clinician’s acceptance of healthcare telemedicine equipment. Journal of Technology Management & Innovation. 2014;9(2):29–41. doi: 10.4067/S0718-27242014000200003. [DOI] [Google Scholar]
- Lally P., Van Jaarsveld C.H., Potts H.W., Wardle J. How are habits formed: Modelling habit formation in the real world. European Journal of Social Psychology. 2010;40(6):998–1009. doi: 10.1002/ejsp.674. [DOI] [Google Scholar]
- Lazar J., Goldstein D.F., Taylor A. Morgan Kaufmann; 2015. Ensuring digital accessibility through process and policy. [Google Scholar]
- Lee S.Y., Lee K. Factors that influence an individual’s intention to adopt a wearable healthcare device: The case of a wearable fitness tracker. Technological Forecasting and Social Change. 2018;129:154–163. doi: 10.1016/j.techfore.2018.01.002. [DOI] [Google Scholar]
- Lepore L., Mettalo C., Schiavone F., Landriani L. Cultural orientations and information systems success in public and proviavte hostitals: Preliminary evidences from Italy. BMC Health ser. Res. 2018;18(1):554. doi: 10.1186/s12913-018-3349-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limayem M., Hirt S.G., Cheung C.M.K. How habit limits the predictive power of intention: The case of information systems continuance. MIS Quarterly. 2007;31(4):705–737. doi: 10.2307/25148817. [DOI] [Google Scholar]
- Lin C.P., Tsai Y.H., Wang Y.J., Chiu C.K. Modeling IT relationship quality and its determinants: A potential perspective of network externalities in e-service. Technological Forecasting and Social Change. 2011;78:171–184. doi: 10.1016/j.techfore.2010.04.015. [DOI] [Google Scholar]
- Martens P. Health transitions in a globalizing world: towards more disease or sustained health? Futures. 2002;34(7):635–648. doi: 10.1016/S0016-3287(02)00005-8. [DOI] [Google Scholar]
- Mcknight D.H., Chervany N.L. What trust means in e-commerce customer relationships: An interdisciplinary conceptual typology. International Journal of Electronic Commerce. 2002;6(2):35–59. doi: 10.1080/10864415.2001.11044235. [DOI] [Google Scholar]
- Moores T.T. Towards an integrated model of IT acceptance in healthcare. Decision Support Systems. 2012;53(3):507–516. doi: 10.1016/j.dss.2012.04.014. [DOI] [Google Scholar]
- Moser I. Disability and the promises of technology: Technology, subjectivity and embodiment within an order of the normal. Information, Communication and Society. 2006;9(3):373–395. doi: 10.1080/13691180600751348. [DOI] [Google Scholar]
- Papa A., Mital M., Pisano P., Del Giudice M. E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technological Forecasting and Social Change. 2018 doi: 10.1016/j.techfore.2018.02.018. [DOI] [Google Scholar]
- Park E.J., Kim E.Y., Funches V.M., Foxx W. Apparel product attributes, web browsing, and e-impulse buying on shopping websites. Journal of Business Research. 2012;65(11):1583–1589. doi: 10.1016/j.jbusres.2011.02.043. [DOI] [Google Scholar]
- Prasanna R., Huggins T.J. Factors affecting the acceptance of information systems supporting emergency operation centres. Computers in Human Behaviour. 2016;57:168–181. doi: 10.1016/j.chb.2015.12.013. [DOI] [Google Scholar]
- Prensky M. Digital natives, digital immigrants part 1. Horizon: A Magazine of the Arts. 2001;9(5):1–6. [Google Scholar]
- Pulidindi V., Jinkab S., Priyac S.A. User acceptance of electronic health records: Cross validation of utaut model. Global Management Review. 2016;10(3):42–54. [Google Scholar]
- Rees G.H., Crampton P., Gauld R., MacDonell S. Rethinking health workforce planning: Capturing health system social and power interactions through actor analysis. Futures. 2018;99:16–27. doi: 10.1016/j.futures.2018.03.009. [DOI] [Google Scholar]
- Rogers E.M. The Free Press of Glencoe; New York: 1962. Diffusion of innovations. [Google Scholar]
- Rogers W.A., Mitzner T.L. Envisioning the future for older adults: Autonomy, health, well-being, and social connectedness with technology support. Futures. 2017;87:133–139. doi: 10.1016/j.futures.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapirie S.A., Orzeszyna S. WHO’s health futures consultation. Futures. 1995;27(9/10):1077–1085. doi: 10.1016/0016-3287(95)00071-2. [DOI] [Google Scholar]
- Schomakers E.M., Lidynia C., Ziefle M. Exploring the acceptance of mHealth applications-do acceptance patterns vary depending on context? International Conference on Applied Human Factors and Ergonomics. 2018:53–64. [Google Scholar]
- Simon P. Des pratiques de Télémédecine pour structurer le projet médical partagé d’un groupement hospitalier du territoire. European Research in Telemedicine. 2016;5:71–75. doi: 10.1016/j.eurtel.2016.06.001. [DOI] [Google Scholar]
- Simon P., Lucas J. La télémédecine n’est pas du e-commerce mais de la médecine Clinique. European Research in Telemedicine. 2014;3:27–34. doi: 10.1016/j.eurtel.2014.01.030. [DOI] [Google Scholar]
- Stienstra D., Watzke J., Birch G.E. A three-way dance: The global public good and accessibility in information technologies. The Information Society. 2007;23(3):149–158. doi: 10.1080/01972240701323564. [DOI] [Google Scholar]
- Sun Y., Wang N., Guo X., Peng Z. Understanding the acceptance of mobile health services: A comparison and integration of alternative models. Journal of Electronic Commerce Research. 2013;14(2):183–200. [Google Scholar]
- Tavares J., Oliveira T. Electronic health record patient portal adoption by health care consumers: An acceptance model and survey. Journal of Medical Internet Research. 2016;18(3):1–17. doi: 10.2196/jmir.5069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Todd P.A. Understanding information technology usage: A test of competing models. Information System Research. 1995;6(2):144–176. doi: 10.1287/isre.6.2.144. [DOI] [Google Scholar]
- Venkatesh V., Davis F.D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Management Science. 2000;46(2):186–204. doi: 10.1287/mnsc.46.2.186.11926. [DOI] [Google Scholar]
- Venkatesh V., Morris M.G., Davis G.B., Davis F.D. User acceptance of information technology: Toward a unified. MIS Quarterly. 2003;27(3):425–478. doi: 10.2307/30036540. [DOI] [Google Scholar]
- Venkatesh V., Thong J.Y., Xu X. Consumer acceptance and use of information technology: Extending the unified theory of acceptance and use of technology. MIS Quarterly. 2012;36(1):157–178. doi: 10.2307/30036540. [DOI] [Google Scholar]
- Verhagen T., Van Dolen W. The influence of online store beliefs on consumer online impulse buying: A model and empirical application. Information & Management. 2011;48(8):320–327. doi: 10.1016/j.im.2011.08.001. [DOI] [Google Scholar]
- Verplanken B. Beyond frequency: Habit as mental construct. The British Journal of Social Psychology. 2010;45(3):639–656. doi: 10.1348/014466605X49122. [DOI] [PubMed] [Google Scholar]
- Wu J.H., Wang S.C., Lin L.M. Mobile computing acceptance factors in the healthcare industry: A structural equation model. International Journal of Medical Informatics. 2007;76(1):66–77. doi: 10.1016/j.ijmedinf.2006.06.006. [DOI] [PubMed] [Google Scholar]
- Xu Z. An empirical study of patient’s privacy concerns for health informatics as a service. Technological Forecasting and Social Change. 2019;143:297–306. doi: 10.1016/j.techfore.2019.01.018. [DOI] [Google Scholar]