Abstract
Rationale and Objectives
The COVID-19 pandemic has forced rapid evolution of the healthcare environment. Efforts to mitigate the spread of the virus through social distancing and shelter-at-home edicts have unintended consequences upon clinical and educational missions and mental well-being of radiology departments. We sought to understand the impact of the COVID-19 pandemic on radiology residencies with respect to the educational mission and perceptions of impact on well-being.
Materials and Methods
This study was IRB exempt. An anonymous 22 question survey regarding the impact of COVID-19 pandemic on educational and clinical missions of residencies, its perceived impact upon morale of radiologists and trainees and a query of innovative solutions devised in response, was emailed to the Association of Program Directors in Radiology membership. Survey data were collected using SurveyMonkey (San Mateo, California).
Results
Respondents felt the COVID-19 pandemic has negatively impacted their residency programs. Regarding the educational mission impact, 70.1% (75/107) report moderate/marked negative impact and 2.8% (3/107) that educational activities have ceased. Regarding the pandemic's impact on resident morale, 44.8% (48/107) perceive moderate/marked negative effect; perceived resident morale in programs with redeployment is significantly worse with 57.1% (12/21) reporting moderate/marked decrease. Respondents overwhelmingly report adequate resident access to mental health resources during the acute phase of the pandemic (88.8%, 95/107). Regarding morale of program directors, 61% (65/106) report either mild or marked decreased morale. Program innovations reported by program directors were catalogued and shared.
Conclusion
The COVID-19 pandemic has markedly impacted the perceived well-being and educational missions of radiology residency programs across the United States.
Key words: COVID-19, Radiology resident, Program director, Association of Program Directors in Radiology, Well-being
INTRODUCTION
As the world grapples with the new realities of life in the setting of the COVID-19 pandemic, daily practices in healthcare are rapidly evolving. Out of necessity, radiology residencies and departments are implementing changes to the clinical and educational environments (1, 2, 3, 4). Wide implementation of social distancing and shelter-at-home edicts intend to “flatten the curve” of spread of COVID-19. While these efforts have yielded their intended effect, there are wide-reaching unintended consequences, specifically on imaging case volumes and case mix, resident education sessions, and well-being of radiologists; faculty and residents alike are impacted (1,3,5). For instance, outpatient imaging volumes have decreased more than 70% in some centers and inpatient volumes have decreased as much as 50% (6, 7, 8).
Similarly, the educational landscape in radiology residencies has the potential to be markedly impacted now and into the future. With decreased volume of imaging studies, trainees’ education through exposure to clinical work is impacted and social distancing measures alter how resident-faculty case readouts occur (1,2,4). Social distancing measures will likely alter the face of didactic and case-based educational content of radiology residencies (1,2,4).
With its attendant added stressors, the COVID-19 pandemic has the potential to impact the physical and emotional well-being of radiologists. For instance, symptoms of depression, anxiety, and distress were reported in 50%, 45%, and nearly 75% respectively of surveyed health care workers in China during the COVID-19 pandemic (9). Prior to the COVID-19 pandemic, nearly half of practicing radiologists reported symptoms of burnout in the 2020 Medscape survey (10), nearly 80% of radiologists, midlevel providers, and physicists reported burnout as a significant workplace issue in the 2018 American College of Radiology Human Resources Commission Workforce survey, and only 21% of survey respondents felt that they had effective means to address burnout (11). At baseline, radiology trainees are also prone to burnout, with up to 85% of radiology residents and fellows reporting symptoms indicative of burnout (12, 13, 14). Given these extraordinary baseline rates of burnout in radiology trainees, it stands to reason that we might expect to see further issues emerge in our radiology residents as we navigate through, and beyond, the COVID-19 pandemic.
The Well-Being Subcommittee of the Association of Program Directors in Radiology (APDR) Common Program Requirements Ad Hoc Committee and prior collaborative APDR committee members conducted a study of APDR members to better understand the impact of the COVID-19 pandemic on radiology residencies with respect to the educational mission and perceptions on impact on well-being.
METHODS
The study protocol was deemed compliant with the Health Insurance Portability and Accountability Act and was exempted from further review and monitoring by the institutional review board of the lead author's institution.
Members of the Well-Being subcommittee of APDR Common Program Requirements Ad Hoc Committee and co-author program directors from prior collaborative APDR committee experiences developed a short survey regarding the impact of COVID-19 pandemic on the clinical and educational missions of residencies, its perceived impact upon morale of radiologists and trainees, including innovative solutions departments have devised to address pandemic challenges. The survey was reviewed and vetted by the APDR Survey Committee establishing face validity and a pilot test was undertaken before survey distribution. On April 16, 2020, a link to the approved anonymous online survey was distributed to the membership of APDR. A single email reminder was sent 14 days later; a total of 4 weeks was allowed to complete the online survey. Survey data were collected using SurveyMonkey (San Mateo, California).
The full survey instrument can be viewed as an appendix to this article (Appendix A). Twenty-two total questions were administered: eighteen survey questions which included items to gauge program directors’ perceptions of the impact of the COVID-19 pandemic on educational, clinical, and well-being missions of their department, three questions sought data on the educational role of the respondent and characteristics of the respondent's radiology residency. Respondents were encouraged to provide free-text comments as a component of open-ended questions employed in 20 of the 22 survey questions. In an attempt to remove barriers to participation, survey respondents were not required to respond to every question to contribute.
Simple comparative statistics were performed.
RESULTS
Of the 312 APDR members who received the survey, 108 responded, yielding an overall response rate of 34.6%. The characteristics of the survey respondents and the programs they represent are shown in Table 1 . Accreditation Council for Graduate Medical Education Pandemic Stage 1 is defined as routine clinical and educational operations, Stage 2 as clinical demands increased beyond routine, and Stage 3 as pandemic emergency status (15). Overwhelmingly, respondents felt that the COVID-19 pandemic has negatively impacted their residency programs with respect to educational, clinical, and well-being matters.
Table 1.
Demographics of 108 Survey Respondents and Their Programs. Accreditation Council for Graduate Medical Education (ACGME)
| Department Role | |
| Program director | 81.5% (88/108) |
| Associate program director | 12.0% (13/108) |
| Department chair | 2.8% (3/108) |
| Education vice-chair | 2.8% (3/108) |
| Faculty | 0.9% (1/108) |
| Program Size | |
| Small (≤12 residents) | 13.9% (15/108) |
| Medium (13–35 residents) | 53.7% (58/108) |
| Large (≥35 residents) | 32.4% (35/108) |
| Institutional Type | |
| Academic medical center | 79.3% 85/108) |
| Community-based | 11.3% (12/108) |
| Hybrid | 1.9% (2/108) |
| ACGME Pandemic Stage | |
| Stage 1 | 12.8% (12/94) |
| Stage 2 | 44.7% (42/94) |
| Stage 3 | 42.6% (40/94) |
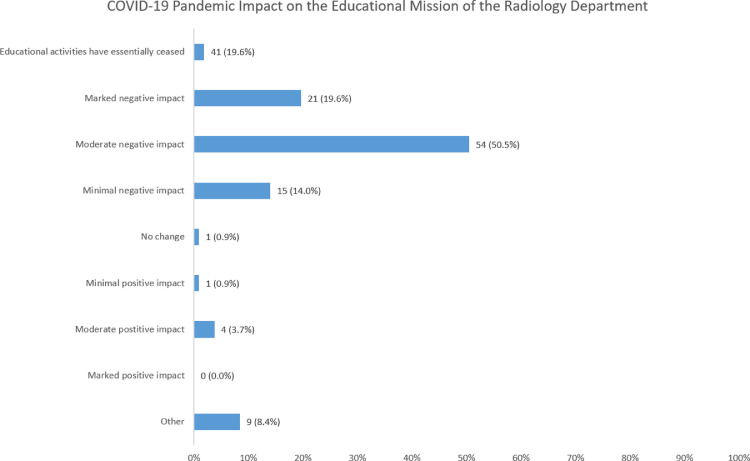
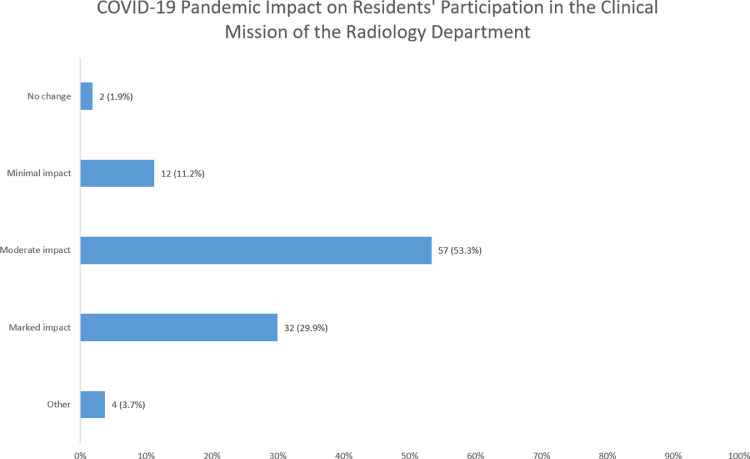
Regarding the educational mission, 70.0% (75/107) report either a marked or moderate negative impact (Fig 1 ). Regarding the impact on resident's participation in the clinical mission, 83.2% (89/107) report either marked or moderate impact (Fig 2 ). Table 2 lists the ways formal educational sessions and clinical activities have been affected, and Table 3 offers a thematic summary with specific examples of innovative educational and clinical solutions reported by the respondents.
Figure 1.
Impact of COVID-19 pandemic upon the educational mission of the radiology department. One hundred and seven respondents completed this question. All of the free-text responses associated with the response of “other” indicated that the pandemic has had a mixed impact upon the educational mission of the radiology department. (Color version of figure is available online.)
Figure 2.
Impact of COVID-19 pandemic upon residents’ participation in the clinical mission of the radiology department. 107 respondents completed this question. All of the free-text responses associated with the response of “other” indicated the pandemic has had a mixed impact upon the residents’ participation in the clinical mission of the radiology department. (Color version of figure is available online.)
Table 2.
Impact of the COVID-19 Pandemic on Resident Education and Clinical Activities
| Educational Sessions | |
| Didactic, case-based and hot-seat conferences are web-based/streamed, but presented in real-time by local faculty | 80.4% (86/107) |
| Prerecorded conferences and live webinars available through radiology societies and the APDR | 79.4% (85/107) |
| Prerecorded didactic conferences available for review by residents at their leisure | 36.5% (39/107) |
| Didactic conferences on hold indefinitely | 7.5% (8/107) |
| Other | 9.4% (10/107) |
| Clinical Activities | |
| Clinical-related, nonimage-based activities | 35.5% (38/107) |
| Interpret clinical studies from home | 29.0% (31/107) |
| Sent home and not helping clinically | 24.3% (26/107) |
| Redeployed | 22.4% (24/107) |
Table 3.
Innovative Solutions to Maintain the Educational Mission of the Department. Themes Extracted From-Free-Text Survey Responses. Associate of Program Directors in Radiology (APDR), Radiologic Society of North America (RSNA), American Roentgen Ray Society (ARRS), Picture Archiving and Communication System (PACS)
| Educational Initiatives | |
| Residents creating teaching material | Create educational content for junior residents and medical students |
| Present virtual tumor boards | |
| Compile and organize interesting cases | |
| Develop videos to orient residents to new clinical rotations | |
| Virtual journal clubs | |
| Social media | Faculty and residents utilize social media to create and collaborate on educational conferences |
| Timing | Increase flexibility in conference start times to boost attendance and engagement of the residents |
| Gamification and nonlecture educational projects | Flipped classroom |
| Virtual escape rooms and educational puzzles | |
| Team-based educational challenges | |
| National curricula | Online resources from APDR, RSNA, ARRS and subspecialty societies |
| Clinical Teaching | |
| Clinical-related, nonimage-based activities | List of curated cases from PACS to mirror cases that would typically be seen on the specialty rotation. |
| Home study curricula | |
| Distribution of shared interesting cases of the day/week | |
| Virtual face to face clinical instruction/readout | Utilize video conferencing platforms for virtual read outs |
| Utilize screen sharing or embedded PACS software to facilitate remote review of cases | |
| Daily check-ins and huddles with attendings/fellows/residents on service | |
| Monitor educational activity/progress | Documentation of activities through activity logs integrated into websites |
| Educational management software to distribute and document required educational activities | |
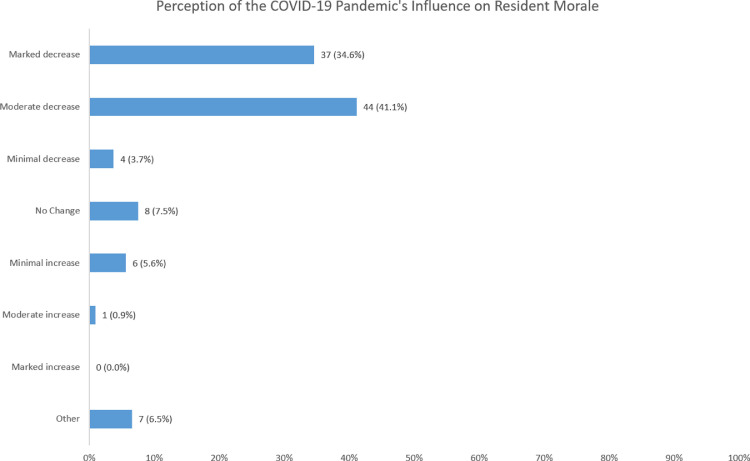
Regarding the pandemic's impact on perceived resident morale, 75.7% (81/107) perceive either a moderate or marked decrease sense of morale (Fig 3 ). Factors influencing morale are shown in Table 4 .
Figure 3.
Perception of the COVID-19 pandemic's impact on resident morale. One hundred and seven respondents completed this question. All of the free-text responses associated with the response of “other” indicated that it was difficult to perceive resident morale or the respondents felt that there was a mixed impact on resident morale. (Color version of figure is available online.)
Table 4.
Factors Influencing Resident Morale During the COVID-19 Pandemic. Respondents Were Asked to Select All That Apply
| Survey Choices | |
| Fear of contracting the virus | 78.5% (84/107) |
| Fear of loved ones contracting the virus | 75.7% (81/107) |
| Feelings of isolation | 74.8% (80/107) |
| Sorrow for lost block or elective opportunities | 63.6% (68/107) |
| Increased sense of camaraderie | 15.9% (41/107) |
| Desire to have more direct impact on clinical care of patients | 19.6% (17/107) |
| Other | 10.3% (13/107) |
| Free-Text Responses | |
| Delay in ABR Core exam | |
| Lost educational opportunities due to decreased clinical volumes | |
| Uncertainty about the future | |
| Cancellation of in-person graduation ceremonies | |
| Concern about job prospects | |
| Anxiety about potential redeployment (redeployment not yet in place) | |
| Unfairness of redeployment of radiology residents but not faculty |
When specifically questioned about resident redeployment, 66.4% (71/107) of programs confirm residents have not been redeployed. Of the 46 respondents describing redeployment of their residents, 13.0% (6/46) were redeployed into nonclinical roles outside of the department of radiology, 46.6% (21/46) into clinical roles outside of the department of radiology, and 41.3% (19/46) into other roles within the department of radiology. The perceived resident morale of the respondents reporting resident redeployment into clinical roles outside of the radiology department is significantly worse (p= 0.008) than the perceived morale of the residents from programs reporting no resident redeployment or redeployment into nonclinical roles outside of the radiology department. Of the 21 respondents reporting resident redeployment into clinical roles outside of the department of radiology, 57.1% (12/21) reported either moderate or marked decrease perceived sense of morale, 4.8% (1/21) with no perceived change, and none with any degree of perceived increased sense of morale. On the other hand, of the 86 respondents with either no resident redeployment or resident redeployment into nonclinical roles outside of the department, 41.9% (36/86) reported either moderate or marked decrease perceived sense of morale, 8.1% (7/86) no change, and 8.1% (7/86) either minimal or moderate increased perceived sense of morale.
Respondents overwhelmingly report adequate resident access to mental health resources during the acute phase of the pandemic (Table 5 ). Table 6 offers innovative solutions reported by the respondents to foster resident well-being.
Table 5.
Mental Health and Well-Being Resources. Respondents Were Asked to Select All That Apply
| Access | |
| Adequate | 88.8% (95/107) |
| Limited | 9.4% (10/107) |
| Inadequate | 0% (0/107) |
| Unsure | 1.9% (2/107) |
| Mental Health Resources Available | |
| Access to virtual counseling | 83.2% (89/107) |
| Counseling on site | 67.3% (72/107) |
| Formal institutional peer support | 46.7% (50/107) |
| Counseling outside the health system | 40.2% (43/107) |
| Other | 3.7% (4/107) |
| Free-Text Responses | |
| App-based mental health resources | |
| Resources posted to an internal website | |
| Professional coaches | |
| Well-Being Resources Available | |
| Guided meditations and/or breath-work podcasts | 71.4% (65/91) |
| On-line individual fitness resources | 49.5% (45/91) |
| On-line group fitness resources | 48.4% (44/91) |
| Estate planning resources | 14.3% (13/91) |
| Other | 12.1% (11/91) |
| Free-Text Responses | |
| Financial well-being and career planning lectures by faculty | |
| Free yoga by video conference, 3× per week, led by a faculty member | |
| Department wellness coordinator emails suggestions and resources | |
| Institutional wellness team | |
Table 6.
Resident Well-Being Concerns and Solutions. Themes Extracted From Free-Text Survey Responses. Program Director (PD), Graduate Medical Education (GME), Accreditation Council for Graduate Medical Education (ACGME), Personal Protective Equipment (PPE)
| Communication | |
| Virtual PD-resident meetings | Routine check-ins between Residents and PD allow residents to hear most up-to-date information and serves as a forum to allow residents to bring up issues and concerns |
| Combats feeling of isolation for those on home isolation or quarantine | |
| Disseminate meeting minutes from virtual PD resident meeting | |
| Share various well-being support thoughts, ideas, websites, and software apps | |
| Employee health | Partner with GME to ensure frequent posting and resident access to employee health |
| Team with Psychiatry department in hosting resident-led support groups. | |
| Fears | |
| Graduation requirements | Share and discuss most up-to-date information and communications from the ACGME |
| Work with department leadership, section heads, and residents to provide additional opportunities to meet graduation targets | |
| Resident redeployment | Partner with GME to ensure radiology residents are appropriately utilized, supervised, and provided PPE to perform redeployment tasks |
| Work with GME to protect high risk or remediating residents from redeployment | |
| Unique resident situations | |
| childcare | Ensure residents have knowledge of and access to childcare support by the hospital and community |
| Maintain maximum flexibility regarding rotations and call to minimize the impact of resident's loss of childcare | |
| Pregnancy | Adhere to national, state, and hospital guidelines regarding pregnancy and patient exposure |
| Provide ample emotional support and rotation flexibility for pregnant residents to minimize patient exposure | |
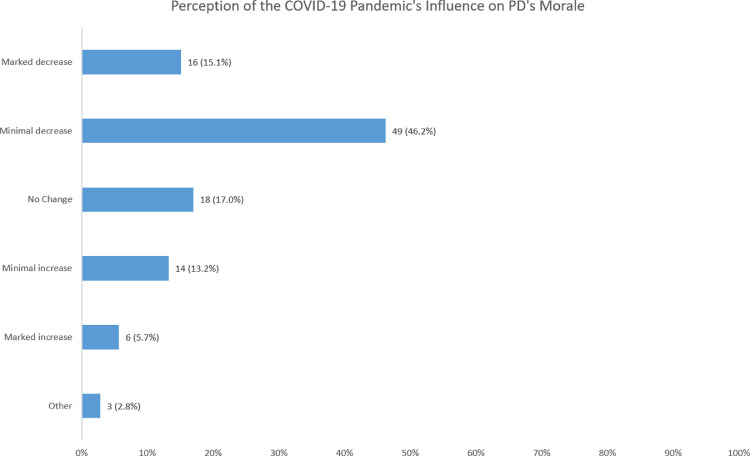
Regarding morale of program directors, over 61% (65/106) report either mild or marked decreased morale resulting from the COVID-19 pandemic (Fig 4 ). Factors influencing morale are shown in Table 7 .
Figure 4.
Impact of COVID-19 pandemic upon program director's (PD) morale. One hundred and six respondents completed this question. (Color version of figure is available online.)
Table 7.
Factors Influencing Program Director (PD) Morale During the COVID-19 Pandemic. Respondents Were Asked to Select All That Apply
| Factors Negatively Influencing PD Morale | |
| Fear of loved ones contracting the virus | 75% (78/104) |
| Fear contracting the virus | 56% (58/104) |
| Feelings of isolation | 52% (54/104) |
| Feeling disproportionate burden as PD | 39% (41/104) |
| Feeling of guilt of not being front line provider | 29.8% (31/104) |
| Lack of adequate public health measures | 22.1% (23/104) |
| Lack of guidance from departmental leadership | 18.2% (19/104) |
| Lack of guidance from institutional leadership | 12.5% (13/104) |
| Other | 9.6% (10/104) |
| Factors Positively Influencing PD Morale | |
| Support and resolve of family/friends | 74/5% (79/106) |
| Internal motivation to lead in difficult times | 74.5% (79/106) |
| Personal efforts toward well-being | 68.9% (73/106) |
| Support and resolve of community | 62.3% (66/106) |
| Support and guidance from departmental leadership | 57.6% (61/106) |
| Solidarity and resolve of residents | 51.9% (55/106) |
| Other | 7.6% (8/106) |
DISCUSSION
Clinical and educational impacts of COVID-19 described in several publications in the radiology literature have been based upon anecdotal experience from single or small groups of 2–5 institutions (1, 2, 3, 4, 5, 6, 7, 8). Our study is the first to report broadly the experiences and perceptions of program directors and to specifically focus upon the well-being of radiology residencies during this pandemic. In keeping with recent publications, our survey confirms that 75% of respondents believe the educational mission of their radiology department has been negatively impacted to a moderate or marked degree or has essentially ceased, with 84% of respondents indicating resident involvement in the clinical mission has been moderately to markedly negatively impacted or has essentially ceased.
In light of social distancing mandates, the traditional didactic conference has been impacted, with survey respondents incorporating prerecorded material; it remains to be seen if using prerecorded lectures for didactic content, supplemented with subsequent video conference-based case sessions translates into improved educational content retention by radiology residents. Lectures administered via interactive video conferencing have been shown to be as effective or more effective than traditional in-person lectures in preparing medical students for objective structured clinical examination type tests (16,17). Radiology residents have reported recorded didactic lectures are extremely useful, and faculty report that the preparation time compared to traditional lectures is similar (18). The combined use of enduring learning materials, such as prerecorded lectures, question banks, and video conference-based case conferences resembles the concepts of “flipped learning” (19,20). Flipped learning is a technique whereby concepts are introduced to learners outside of the classroom space through asynchronous educational materials and the in-personal educational time is dedicated to an in-depth exploration and application of the topic(s). Flipped learning techniques are integrated from grade schools through college and graduate programs and are also finding traction in undergraduate medical education (19,20). Specifically related to undergraduate medical education in radiology, flipped learning and blended learning techniques have been shown to increase academic achievement compared to traditional didactic lectures in a radiology clerkship (19).
Since residents are participating in fewer clinical examinations/procedures during the pandemic, many respondents innovated by tasking the residents with creating novel teaching materials. Solutions include creation of a resident-authored library of basic lectures to be used in future introductory months for first-year radiology residents and medical students and assignment of residents to create exam questions based upon review articles. These educational activities engage residents in the academic mission in ways they may not otherwise have had opportunities to participate. Guenette et al showed that radiology residents in New England scored higher in measures of personal accomplishment when they felt the skills and knowledge being built are important to society (21). While our study was not designed to measure residents’ sense of personal accomplishment, one might conjecture that these alternative educational activities impart a sense of personal accomplishment through contribution to local educational landscapes; these activities come at a time when residents may otherwise feel that they have fewer contributions in the clinical realm.
Our survey was not designed to measure burnout, but respondents overwhelmingly perceive decreased resident morale, with the majority also relating personal diminished morale. The long-term psychological toll of COVID-19 is likely to be profound. Post-traumatic stress symptoms (PTSS) ensue after a traumatic event(s) beyond the normal range of common human experience. During the severe acute respiratory syndrome (SARS) outbreak of 2003, up to 50% of healthcare workers experienced PTSS (22). A study of residents of Hubei Province, including its capital city, Wuhan, the region of China hardest hit by the COVID-19 pandemic found that 7% of 285 assessed individuals experienced PTSS in the acute phase of the study; the authors postulate that this number will become higher as the pandemic carries on and through the recovery process (23). Though it is encouraging that our survey shows widespread access to mental health services for residents, we do not know if the resources are being used. We found that the perceived morale of residents was worse in programs whose residents were deployed to clinical roles outside of the radiology department. The risk of PTSS may be heightened in those residents redeployed to clinical work outside of radiology, those in hospitals with large numbers of COVID patients who may have experienced repeated codes, and those who contracted, or whose loved ones contracted, the virus.
Cultivating gratitude and resilience may mitigate the effects of PTSS; this has been demonstrated when young adults experience traumatic events such as a campus shooting (24). In addition to its potentially therapeutic effects, gratitude has long been felt to play a crucial role in building interpersonal relationships (25). Bartlett et al found supporting evidence that gratitude enhances inclusive community building (25). Activities promoting gratitude may be impactful in the near term by helping our radiology departments build and maintain a sense of community and in the long term by mitigating the emotional impact of potential PTSS resulting from the COVID-19 pandemic. In the current survey, some programs endorse this practice of gratitude by providing free food and acknowledging the positive aspects of residents’ personal lives via daily photos of residents with their pets, children, and being otherwise engaged in cherished activities.
Open communication between institution and staff was successful during the SARS outbreak (26). In the aftermath of Hurricane Katrina, open and regular communication helped maintain continuity and community within a psychiatry residency program at Louisiana State University (27). Spalluto et al discuss the importance of regular, bi-directional, transparent communication between leadership and all radiology department members in engendering trust and decreasing stress during the COVID-19 pandemic (28). Daily command center briefings are included among the policies successfully implemented at the University of Washington during their pandemic acute phase response (8). Since transparent communication by institutional leaders has been correlated with decreased physician burnout and increased workplace engagement (29), it is likely that a recurring opportunity for trainees in the department of radiology to hear updates from departmental and institutional leaders and to ask questions serves to mitigate some of the pandemic negative impacts upon well-being. England et al describe implementing frequent virtual huddles between program leadership and residents to keep residents apprised of departmental and institutional operations during the COVID-19 (4). The need to maintain frequent open communication between the institution and department and its residents may be one way to mitigate decreasing morale. Many of our survey respondents report they have incorporated regular meetings to discuss the state of the response with their residency training programs.
Maintaining a sense of community and co-resident social support is important to radiology resident well-being (21,30). Video conferencing was a successful means to maintaining morale in the wake of Hurricane Katrina (27). In addition to recreating conventional side-by-side image read-outs within the constraints of social distancing, video conferencing is a common theme employed by responding program directors to virtually check in with the resident cohorts and facilitate various virtual social gathering amongst the trainees. In those 33% of programs whose residents were deployed, 43% report negative impact on resident well-being; this underscores the importance of maintaining a sense of community for residents redeployed from their routine environments. Similarly, of the features positively impacting morale, 20% of respondents perceive an increased sense of camaraderie influencing residents’ morale during the COVID-19 pandemic with a sense of being part of the greater community.
The pandemic's impact on program directors’ well-being must not be overlooked. Previously published studies of anesthesia, surgery, and radiation oncology indicate PDs have a high level of burnout and emotional exhaustion (31, 32, 33). In our survey, nearly two-thirds of PDs report diminished morale; one half of respondents also reported feeling isolated. PDs found support by looking inward (75%), to loved ones (74%), community (62%), department leadership (57%), and residents (51%).
While members of radiology departments have maintained connection via video conferences to conduct meetings, virtual social gatherings, real-time teaching sessions and multidisciplinary conferences, it is important to remain cognizant of the limitations of these technologies. For instance, video conferencing can introduce distortions into routine interpersonal interactions, particularly with respect to nonverbal cues we are unconsciously accustomed to receive such as direction of gaze and eye contact (34). When we try to mentally reconcile altered gaze and eye contact, video conferencing results in a higher cognitive load than traditional face-to-face conversations. Additionally, interruptions in video feeds and incongruities between video and audio feeds occur during video conferencing (34). Taken in sum, the various distortions and altered nonverbal cues have been found to negatively impact trust formation (34). While widely-used video conferencing is reported by many survey respondents as solution for hurdles they encountered in clinical case read-outs, educational conferences, multidisciplinary tumor boards, and social community-building, we must recognize that this very solution may also introduce emotional fatigue.
This study has several limitations. As with any survey study, the response rate directly affects the survey's generalizability of findings. The 34.6% response rate is in line with other APDR surveys (35,36). Small residency programs and residency programs outside of academic medical centers may be underrepresented. This survey was distributed in the midst of the acute phase of the COVID-19 pandemic, which may have precluded some PDs from responding. As the pandemic continues, programs are likely to evolve the reported coping strategies and devise additional innovations. Because geographic location of the respondents was not collected, it is not possible to draw conclusions about the impact of local pandemic severity.
In sum, the COVID-19 pandemic has markedly impacted the perceived well-being and educational missions of radiology residencies across the United States. The well-being of the residents who have been redeployed into clinical roles outside of the radiology department may be more significantly negatively impacted. We have identified themes of innovative solutions radiology residencies have implemented to mitigate the negative effects on our trainees and discuss some potential pitfalls to these solutions. Although we may be emerging from the acute phase of the first wave of the COVID-19 pandemic, the themes and lessons herein remain applicable.
Footnotes
This manuscript is being submitted solely to Academic Radiology and there is no overlap with previously published works.
Appendix: Survey questions
-
1.What best describes your practice environment?
-
a.Academic medical center
-
b.Hospital affiliated
-
c.Community based
-
d.Other (free text)
-
a.
-
2.What best describes your role?
-
a.DR Program Director
-
b.Integrated DR/IR Program Director
-
c.DR Associate Program Director
-
d.Integrated DR/IR Associate Program Director
-
e.Other (free text)
-
a.
-
3.What is the size of your radiology residency program (inclusive of DR and integrated DR/IR)?
-
a.Small (≤12 residents)
-
b.Medium (13–35 residents)
-
c.Large (≥ residents)
-
a.
-
4.What is the current GME level classification at your institution?
-
a.Stage 1 (“Business as Usual”)
-
b.Stage 2 (Increased Clinical Demands Guidance)
-
c.Stage 3 (Pandemic Emergency Status Guidance)
-
d.I don't know
-
a.
-
5.How has COVID-19 impacted the educational mission of your radiology department?
-
a.No change
-
b.Minimal negative impact
-
c.Moderate negative impact
-
d.Marked negative impact
-
e.Educational activities have essentially ceased
-
f.Minimal positive impact
-
g.Moderate positive impact
-
h.Marked positive impact
-
i.Other (free text)
-
a.
-
6.How are you managing didactic educational conferences in light of social distancing (choose all that apply)?
-
a.Continue with the status quo; in person didactic conferences remain unchanged
-
b.Didactic conferences are now web-based/streamed, but are presented in real-time by local faculty
-
c.Previously recorded didactic conferences are available for review by residents at their leisure.
-
d.Residents are directed to prerecorded conferences and live webinars available through radiology societies (eg: SSR, STR, APDR-sponsored Zoom conferences)
-
e.Didactic conferences are on hold indefinitely
-
f.Other (free text)
-
a.
-
7.How are you managing case-based or hot-seat conferences in light of social distancing (choose all that apply)?
-
a.Continue with the status quo; in person case conferences remain unchanged
-
b.Case-based conferences are now web-based and presented real-time by local faculty
-
c.Residents are directed to use on-line question banks
-
d.Case conferences are on hold indefinitely
-
e.Other (free text)
-
a.
-
8.
What are innovative solutions your department has developed to maintain the educational mission of your radiology department during the COVID-19 pandemic? (Free text answer)
-
9.To what degree has COVID-19 impacted the residents’ participation in the clinical mission of your radiology department?
-
a.No change
-
b.Minimal impact
-
c.Moderate impact
-
d.Marked impact
-
e.Resident clinical activities in radiology have essentially ceased
-
f.Other (free text)
-
a.
-
10.How have you adapted your clinical coverage in the COVID-19 pandemic? (choose all that apply)
-
a.No change to routine rotations and resident coverage
-
b.Residents read clinical studies from home
-
c.Residents assist with clinical-related, nonimage-based, activities (such as phone consultations, study protocoling, etc)
-
d.Residents have been sent home and are not helping clinically
-
e.Residents were redeployed
-
f.Other (free text)
-
a.
-
11.Regarding resident redeployment, where have your residents been placed? (choose all that apply)
-
a.No redeployment
-
b.Into nonclinical roles within the department of radiology
-
c.Into nonclinical roles outside the department of radiology
-
d.Into clinical roles outside the department of radiology
-
a.
-
12.If your residents have been redeployed or are imminently awaiting redeployment, to what degree do you perceive that their redeployment onto clinical services is impacting their current wellbeing?
-
a.No change
-
b.Minimal negative impact
-
c.Moderate negative impact
-
d.Marked negative impact
-
e.Minimal positive impact
-
f.Moderate positive impact
-
g.Marked positive impact
-
h.Other (free text)
-
a.
-
13.Do your residents have adequate access to mental health resources during the acute phase of the COVID-19 pandemic?
-
a.Yes, access is adequate
-
b.Some, but limited/inadequate access
-
c.No, access is inadequate
-
d.Do not know/unaware
-
a.
-
14.What mental health resources are available to your residents during the COVID-19 pandemic? (choose all that apply)
-
a.On-site counseling
-
b.Outside of the residency's health system counseling
-
c.Virtual/phone-based counseling service
-
d.Peer support (formal program sponsored by institution)
-
e.Do not know/unaware
-
f.Other: (free text)
-
a.
-
15.Do your residents have adequate access to other wellbeing resources (healthy lifestyle, financial advice, estate planning, etc) during the COVID-19 pandemic? (choose all that apply)
-
a.Yes, access is adequate
-
b.Some, but inadequate access
-
c.No, access is inadequate
-
a.
-
16.What self-care, fitness, and other resources are available to your residents during the COVID-19 pandemic? (choose all that apply)
-
a.Guided meditations and/or breath-work podcasts
-
b.On-line individual fitness resources (i.e. subsidized/free membership to fitness websites, institutional fitness resources, etc)
-
c.Group on-line fitness resources (i.e. group yoga class by web-chat client, etc)
-
d.Estate planning resources
-
e.Other (free text)
-
a.
-
17.What is your perception of the COVID-19 pandemic's influence upon resident morale in your department?
-
a.No change
-
b.Perceived minimal decreased sense of morale
-
c.Perceived moderate decreased sense of morale
-
d.Perceived marked decreased sense of morale
-
e.Perceived minimal increased sense of morale
-
f.Perceived moderate increased sense of morale
-
g.Perceived marked impact increased sense of morale
-
h.Other (free text)
-
a.
-
18.What do you think are the factors influencing resident morale during the COVID-19 pandemic? (choose all that apply)
-
a.Fear of contracting the virus
-
b.Fear of loved ones contracting the virus
-
c.Feelings of isolation
-
d.Sorrow for lost elective opportunities
-
e.Desire to make more of an impact upon the clinical mission of direct patient care
-
f.Increased sense of comradery
-
g.Renewed sense of purpose for the practice of medicine
-
h.Other (free text)
-
a.
-
19.Regarding YOUR morale, what is your perception of the COVID-19 pandemic influence?
-
a.Perceived marked increased sense of morale
-
b.Perceived mild increased sense of morale
-
c.No perceived difference in morale
-
d.Perceived mild decreased sense of morale
-
e.Perceived marked decreased sense of morale
-
a.
Comment box:
-
1.What are the factors negatively influencing your morale during the COVID-19 pandemic? (choose all that apply)
-
a.Fear of contracting the virus
-
b.Fear of loved ones contracting the virus
-
c.Feeling of isolation
-
d.Lack of guidance from departmental leadership
-
e.Lack of overall public health planning
-
f.Feeling of disproportionate burden on you as a program director
-
g.Other (free text)
-
a.
-
2.What are the factors positively influencing your morale during the COVID-19 pandemic? (choose all that apply)
-
a.Support and resolve of community
-
b.Support and resolve of family and/or friends
-
c.Support and guidance from departmental leadership
-
d.Solidarity and resolve of residents
-
e.Internal motivation to lead in difficult times
-
f.Efforts at maintaining personal wellbeing, eg. Exercise, hobbies, time with family, etc.
-
g.Other (free text)
-
a.
-
3.
Please share additional thoughts you may have regarding resident wellbeing during the COVID-19 pandemic. Have wellbeing issues arisen that you or your program didn't anticipate? What advice do you have for other programs? (free text)
REFERENCES
- 1.Alvin M.D., George E., Deng F. The Impact of COVID-19 on Radiology Trainees. Radiology. March 2020 doi: 10.1148/radiol.2020201222. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chong A., Kagetsu N.J., Yen A. Radiology Residency Preparedness and Response to the COVID-19 Pandemic. Acad Radiol. 2020;27(6):856–861. doi: 10.1016/j.acra.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mossa-Basha M., Meltzer C.C., Kim D.C. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Panel. Radiology. March 2020 doi: 10.1148/radiol.2020200988. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.England E.K., Kanfi A., Flink C. Radiology Residency Program Management in the COVID Era - Strategy and Reality. Acad Radiol. May 2020 doi: 10.1016/j.acra.2020.05.001. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallagher T.H., Schleyer A.M. "We Signed Up for This!" - Student and Trainee Responses to the Covid-19 Pandemic. N Engl J Med. April 2020 doi: 10.1056/NEJMp2005234. online ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Cavallo J.J., Forman H.P. The Economic Impact of the COVID-19 Pandemic on Radiology Practices. Radiology. April 2020 doi: 10.1148/radiol.2020201495. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walach E.COVID-19 Impact on CT Imaging Volume aidoc.com blog [updated April 24, 2020]. Available from: https://www.aidoc.com/blog/ct-imaging-volumes-covid19/?utm_content=125056050&utm_medium=social&utm_source=linkedin&hss_channel=lis-xca2IgYf3G.
- 8.Mossa-Basha M., Medverd J., Linnau K. Policies and Guidelines for COVID-19 Preparedness: Experiences from the University of Washington. Radiology. April 2020 doi: 10.1148/radiol.2019201326. online ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Lai J., Ma S., Wang Y. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kane L.Medcape National Physician Burnout & Suicide Report 2020: The Generational Divide: Medscape; 2020 [updated January 15, 2020]. Available from: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460
- 11.Kruskal J.B., Shanafelt T., Eby P. A Road Map to Foster Wellness and Engagement in Our Workplace-A Report of the 2018 Summer Intersociety Meeting. J Am Coll Radiol. 2019;16(6):869–877. doi: 10.1016/j.jacr.2018.10.025. [DOI] [PubMed] [Google Scholar]
- 12.Guenette J.P., Smith S.E. Burnout: Prevalence and Associated Factors Among Radiology Residents in New England With Comparison Against United States Resident Physicians in Other Specialties. AJR Am J Roentgenol. 2017;209(1):136–141. doi: 10.2214/AJR.16.17541. [DOI] [PubMed] [Google Scholar]
- 13.Holmes E.G., Connolly A., Putnam K.T. Taking Care of Our Own: A Multispecialty Study of Resident and Program Director Perspectives on Contributors to Burnout and Potential Interventions. Academic psychiatry: the journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry. 2017;41(2):159–166. doi: 10.1007/s40596-016-0590-3. [DOI] [PubMed] [Google Scholar]
- 14.Porrino J., Mulcahy M.J., Mulcahy H. Emotional Wellness of Current Musculoskeletal Radiology Fellows. Acad Radiol. 2017;24(6):682–693. doi: 10.1016/j.acra.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 15.ACGME. Three Stages of GME During the COVID-19 Pandemic Accreditation Council of Graduate Medical Edcuation (ACGME) 2020 Available from: https://acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic.
- 16.Vaccani J.P., Javidnia H., Humphrey-Murto S. The effectiveness of webcast compared to live lectures as a teaching tool in medical school. Med Teach. 2016;38(1):59–63. doi: 10.3109/0142159X.2014.970990. [DOI] [PubMed] [Google Scholar]
- 17.Bertsch T.F., Callas P.W., Rubin A. Effectiveness of lectures attended via interactive video conferencing versus in-person in preparing third-year internal medicine clerkship students for Clinical Practice Examinations (CPX) Teach Learn Med. 2007;19(1):4–8. doi: 10.1080/10401330709336616. [DOI] [PubMed] [Google Scholar]
- 18.Kircher M.F., Hines-Peralta A., Boiselle P.M. Implementation of screen-capture video recordings of resident conferences in an academic radiology department: pilot experience. Acad Radiol. 2010;17(2):255–263. doi: 10.1016/j.acra.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 19.O'Connor E.E., Fried J., McNulty N. Flipping Radiology Education Right Side Up. Acad Radiol. 2016;23(7):810–822. doi: 10.1016/j.acra.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Belfi L.M., Bartolotta R.J., Giambrone A.E. "Flipping" the introductory clerkship in radiology: impact on medical student performance and perceptions. Acad Radiol. 2015;22(6):794–801. doi: 10.1016/j.acra.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Guenette J.P., Smith S.E. Burnout: Job Resources and Job Demands Associated With Low Personal Accomplishment in United States Radiology Residents. Acad Radiol. 2018;25(6):739–743. doi: 10.1016/j.acra.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 22.Maunder R.G., Leszcz M., Savage D. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008;99(6):486–488. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu N., Zhang F., Wei C. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vieselmeyer J., Holguin J., Mezulis A. The Role of Resilience and Gratitude in Posttraumatic Stress and Growth Following a Campus Shooting. Psychol Trauma-Us. 2017;9(1):62–69. doi: 10.1037/tra0000149. [DOI] [PubMed] [Google Scholar]
- 25.Bartlett M.Y., Condon P., Cruz J. Gratitude: Prompting behaviours that build relationships. Cognition Emotion. 2012;26(1):2–13. doi: 10.1080/02699931.2011.561297. [DOI] [PubMed] [Google Scholar]
- 26.Maunder R., Hunter J., Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Cmaj. 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 27.Griffies W.S. Post-Katrina stabilization of the LSU/Ochsner Psychiatry Residency Program: caveats for disaster preparedness. Academic psychiatry: the journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry. 2009;33(5):418–422. doi: 10.1176/appi.ap.33.5.418. [DOI] [PubMed] [Google Scholar]
- 28.Spalluto L.B., Planz V.B., Stokes L.S. Transparency and Trust During the Coronavirus Disease 2019 COVID-19 Pandemic. Journal of the American College of Radiology. May 2020 doi: 10.1016/j.jacr.2020.04.026. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shanafelt T.D., Gorringe G., Menaker R. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432–440. doi: 10.1016/j.mayocp.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 30.Mendoza D., Bertino F.J. Why Radiology Residents Experience Burnout and How to Fix It. Acad Radiol. 2019;26(4):555–558. doi: 10.1016/j.acra.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 31.De Oliveira G.S., Jr., Almeida M.D., Ahmad S. Anesthesiology residency program director burnout. J Clin Anesth. 2011;23(3):176–182. doi: 10.1016/j.jclinane.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Aggarwal S., Kusano A.S., Carter J.N. Stress and Burnout Among Residency Program Directors in United States Radiation Oncology Programs. Int J Radiat Oncol Biol Phys. 2015;93(4):746–753. doi: 10.1016/j.ijrobp.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 33.Anderson K.D., Mavis B.E., Dean R.E. Feeling the stress: perceptions of burnout among general surgery program directors. Curr Surg. 2000;57(1):46–50. doi: 10.1016/s0149-7944(00)00138-0. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen D., Canny J., Multiview . Improving trust in group video conferencing through spatial faithfulness. Conference paper. University of California Berkely; 2007. pp. 1465–1474.http://bid.berkeley.edu/files/papers/multiview07.pdf available from: Accessed on 6/17/2020. [Google Scholar]
- 35.Rozenshtein A., Heitkamp D.E., Muhammed T.L. “What Program Directors Think” III: Results of the 2014/2015 Annual Surveys of the Association of Program Directors in Radiology (APDR) Acad Radiol. 2016;23(7):861–869. doi: 10.1016/j.acra.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 36.Jordan S.G., Robbins J.B., Sarkany D. The Association of Program Directors in Radiology Well-Being 2019 Survey: Identifying Residency Gaps and Offering Solutions. J Am Coll Radiol. 2019;16(12):1702–1706. doi: 10.1016/j.jacr.2019.06.017. [DOI] [PubMed] [Google Scholar]