Abstract
Objective
The coronavirus disease-2019 (COVID-19) pandemic has strained all levels of healthcare and it is not known how chiropractic practitioners have responded to this crisis. The purpose of this report is to describe responses by a sample of chiropractors during the early stages of the COVID-19 pandemic.
Methods
We used a qualitative-constructivist design to understand chiropractic practice during the COVID-19 pandemic, as described by the participants. A sample of chiropractic practitioners (doctors of chiropractic, chiropractors) from various international locations were invited to participate. Each described the public health response to COVID-19 in their location and the actions that they took in their chiropractic practices from April 20 through May 4, 2020. A summary report was created from their responses and common themes were identified.
Results
Eighteen chiropractic practitioners representing 17 locations and 11 countries participated. A variety of practice environments were represented in this sample, including, solo practice, mobile practice, private hospital, US Veterans Administration health care, worksite health center, and group practice. They reported that they recognized and abided by changing governmental regulations. They observed their patients experience increased stress and mental health concerns resulting from the pandemic. They adopted innovative strategies, such as telehealth, to do outreach, communicate with, and provide care for patients. They abided by national and World Health Organization recommendations and they adopted creative strategies to maintain connectivity with patients through a people-centered, integrated, and collaborative approach.
Conclusion
Although the chiropractors in this sample practiced in different cities and countries, their compliance with local regulations, concern for staff and patient safety, and people-centered responses were consistent. This sample covers all 7 World Federation of Chiropractic regions (ie, African, Asian, Eastern Mediterranean, European, Latin American, North American, and Pacific) and provides insights into measures taken by chiropractors during the early stages of the COVID-19 pandemic. This information may assist the chiropractic profession as it prepares for different scenarios as new evidence about this disease evolves.
Key Indexing Terms: Health Occupations, Chiropractic, COVID-19 [Supplementary Concept], Pandemics
Introduction
Coronavirus disease-2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was discovered in late 2019.1 In January 2020, details about the disease were still unknown making public health decisions challenging. By early March, the disease spread rapidly with the number of cases increasing by 1000-fold and the World Health Organization (WHO) declaring a pandemic on March 11, 2020.2, 3, 4 By April 20, there were 2.42 million confirmed cases and 166 235 deaths and by May 4, 2020 there were 3.58 million cumulative confirmed cases and 250 687 deaths due to COVID-19 globally.5, 6, 7
WHO published its Strategic Response and Preparedness Plan that provided recommendations for both the public and health care providers.8 It was estimated that approximately 20% of COVID-19 cases were severe or critical8 and that COVID-19 had a globally estimated average fatality rate of 3%; however, rates varied by country.8 For example, on May 5, 2020 the observed case-fatality ratio for the United Kingdom was 15%, while for the Netherlands it was 12.6%, Brazil was 6.9%, and the United States (US) was 5.9%.9
The rapid spread of COVID-19 has had tremendous impact but especially on healthcare resources and personnel around the world.8 , 10 , 11 During the early phase of the COVID-19 pandemic, health care providers faced difficult situations screening for this high-threat pathogen while caring for those who were infected and trying to mitigate spread of the virus. Measures to control the novel disease created additional burdens on the health and social care systems.8 Medical providers and first responders faced difficult life and death decisions in the midst of a severe supply shortage at the same time that they were putting their own lives at risk. To protect the health of the community, all people around the world were asked to join together in solidarity to fight COVID-19 using various measures.4 , 8 , 10 , 12 , 13 Along with other health professionals, chiropractic practitioners (ie, doctors of chiropractic (DC), chiropractors) faced unknown territory as they navigated health care in the context of unprecedented governmental restrictions and public health responses.
Chiropractic is a recognized and licensed health care profession in many world regions.14 Each country, state, or province has its own regulations for the chiropractic profession. However, depending on preceding historical and social factors, local regulations and scopes of practice vary.15, 16, 17 As of 2017, the World Federation of Chiropractic (WFC) estimates that there are nearly 104 000 chiropractors in the world.14 Although the majority of chiropractors (74%) currently practice in the US, the number of chiropractors in other countries is growing.18
Patients typically have direct access to chiropractors and do not require a referral to receive chiropractic care. Chiropractors often function as primary contact practitioners (ie, in some areas this is known as portal of entry) and work at the primary level in healthcare.16 , 17 , 19 , 20 Chiropractors are part of the healthcare workforce and collaborate with other providers to deliver the safest and most effective care possible to their patients and the public. 21 , 22
One view of chiropractic is that it “is one of the healing professions dedicated to conservative and natural methods of health care and recognizes the body's innate ability to heal.”22 Chiropractic primarily focuses on physiological and biomechanical aspects of health, including spinal, musculoskeletal, and neurological components, but also includes consideration of psychological, social, and environmental relationships, which is congruent with the biopsychosocial model of care.23, 24, 25, 26 It has been suggested that chiropractic care “offers potential for cost‐effective management of neuromusculoskeletal disorders.”16 Thus, chiropractors may contribute to reducing the global burden of back and neck pain.25, 26, 27, 28, 29
According to the WHO Guidelines on Basic Training and Safety in Chiropractic, chiropractic “is one of the most popularly used forms of manual therapy.”16 The chiropractic profession is known for high rates of patient satisfaction and a hands-on approach to care.20 , 30, 31, 32, 33, 34 People seek out chiropractic care for a variety of reasons, but commonly for musculoskeletal concerns, such as back and neck pain.17 , 35 , 36 The median 12-month utilization of chiropractic services has been estimated to be 9.1% globally.37 Therefore, due to its common use, taking a closer look at this health profession in the context of response to the COVID-19 pandemic is warranted.
Pandemics create challenging circumstances for all health care providers. Regulations for physical distancing and other measures to control the spread of COVID-19 has disrupted daily life and routine health care practices.10 Clinical practice is especially challenging for those professionals who routinely use their hands as a part of their assessment and treatment for managing patients. Currently, it is unknown how individual chiropractic practitioners have responded at the time of physical distancing and stay-at-home orders. Therefore, the purpose of this qualitative report is to describe actions by an international sample of practicing chiropractors during the early stages of the COVID-19 pandemic.
Methods
This is a qualitative, narrative research study using chronological, story-oriented reporting.38 Because qualitative research is focused on the perceptions and experiences of people,39 we used a qualitative-constructivist approach to understand chiropractic practice during the COVID-19 pandemic as described by the participants. This approach strives to understand the complexities of experience from the point of view of the participant.40 Inherent to the constructivist-qualitative approach, we made no attempt to control variables and accepted the complexity of the phenomenon as a whole.41
This descriptive report includes chiropractors' actions during the early COVID-19 pandemic between the dates of April 20 to May 4, 2020. The primary author (CJ) was responsible for the research design and analysis, and invited chiropractic practitioners from different international locations to participate in this report. As far as the first author was aware, none of the chiropractors reporting actions taken in their practices had regular communications with one another (except KS and CL who are married). The only connection among the practicing chiropractors was that they were known by the primary author. The invitee list was blinded so that no one knew who else was invited initially. It was presumed that practitioners in each location acted independently in their actions and responses to the pandemic. Anyone who was invited but declined or did not respond was excluded from this report.
The role of the researcher is an integrated part of qualitative research.42 Therefore, the investigator's influence on the research setting is seen as a benefit and not a detriment to the process.39 Thus, each author's interpretation of their experience during the pandemic is considered enriching to the methods.39
The constructivist approach typically utilizes broad and general questions to capture the richness of the participants’ experiences and how each navigates the cultural and social influences on their lives.39 Accordingly, each participant was asked to answer 2 open-ended questions with a limitation of 500 words: (1) provide a description of the public health response to COVID-19 in their local area and (2) provide a brief synopsis of actions that they took in their chiropractic practices in response to COVID-19. The first author collected and collated the responses and drafted a summary report. All contributors reviewed the full manuscript for accuracy and approved the final contents. All communications were completed by email. Each coauthor consented to participate and contributed as a co-author, as defined by the International Council of Medical Journal Editors criteria for authorship.43
For this report, we followed the Standards for Reporting Qualitative Research according to O'Brien et al.44 This was not an experimental study. This was a retrospective, self-descriptive report. No private health information was included, and each participant consented and contributed as an author; thus, no ethics review was sought.
Results
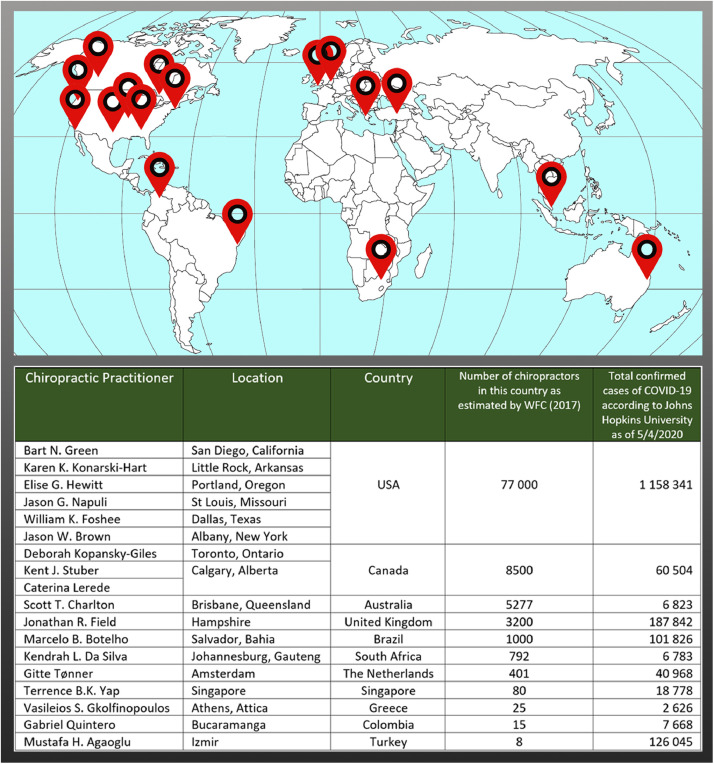
Eighteen chiropractors representing 17 locations in 11 countries participated. Their location, number of chiropractors in their country, and number of confirmed cases of COVID-19 are represented in figure 1 .5 , 6 , 14 The following summaries from the individual chiropractic practitioners describe their locations and how each responded to the COVID-19 crisis.
Fig 1.
Locations of the sample chiropractic practices on a global map. 5,6,14
California, USA
On January 26, 2020, the first case of COVID-19 in California was reported.45 Following this, the first known fatality in the US occurred in Northern California on February 6.46 The Governor of California declared a state of emergency and a statewide stay-at-home order on March 1947 when the number of confirmed COVID-19 cases in California exceeded 1000.48 Businesses were closed unless they were considered to be part of the critical infrastructure, such as healthcare.49 However, the state's Director of Public Health recommended that routine or elective health services be rescheduled to a later date. Health care providers were encouraged to use telehealth, rather than in-person visits.49 Some California counties issued requirements for all citizens to wear face coverings when they were in proximity to anyone other than family members.50
Bart Green
I provide chiropractic services and am integrated in an interprofessional, collaborative team at a worksite health center. Services provided at this location include primary medical care, behavioral health, physical therapy, acupuncture, nutritional counseling, optometry, and chiropractic. We serve an ethnically diverse population with an international demographic. This patient population frequently travels domestically and internationally for business or family visits, particularly to Southern and Eastern Asia.
In the health center, I normally use standard infection control measures,51 such as wiping down treatment tables with antiseptic cleaners in between patient visits, hand washing before and after each patient encounter, and regular office hygiene and safety protocols, as recommended by The Joint Commission.52 In the first week of March, when the COVID-19 outbreak was increasing in prevalence and spreading in distribution in California, infection control measures were enhanced to additionally include wiping down door handles, seat arm rests, and other frequently touched areas in between each patient visit. As recommended by WHO and the US Centers for Disease Control and Prevention, we began to practice physical distancing between patients and between staff members.53 , 54 Patients were asked screening questions before scheduling and when checking in for an appointment. Only 1 patient was allowed in the reception area at a time; others waited outside of the health center.
In response to the state mandated stay-at-home order, other providers at the health center and I transitioned from in-office visits to telehealth encounters. Patients scheduled for in-office appointments were called and invited to reschedule to telehealth visits at their discretion. Since March 19, all chiropractic visits were performed using real time video conferencing, secure messaging, and other telehealth mechanisms deployed from my home office. Telehealth patient visits were done using a secure video platform that was integrated within the electronic health record. Both new patient consultations and follow-up visits were conducted. Many of the exam procedures that were normally done in the health center were done through videoconferencing through verbal instruction or by having the patient mimic what I was doing. This approach was also used for home exercises. Video visits allowed me to spend more time on patient education and my patients seemed to like this format. Using the electronic health record program, after visit self-care and home exercise instructions were sent via a secure messaging system. No patients presenting during this time had any severe health problems requiring referral. However, appropriate resources were in place in case referral was necessary. Thus far, patients have provided positive feedback about the use of video visits. Many expressed gratitude that they were able to receive care remotely and avoid community exposure to coronavirus.
Arkansas, USA
On March 11, 2020, the first case of COVID-19 was confirmed in Arkansas.55 On March 23, the Arkansas Department of Health and the Arkansas State Board of Chiropractic Examiners stated that individual chiropractic physicians were to determine whether their office remain open.56 This recommendation was subject to change at the discretion of the Governor and Secretary of Health. The Arkansas Department of Health recommended that patient care that could be safely postponed be rescheduled to a future date. The following criteria were recommended by the Department of Health to determine if a patient should be rescheduled: (1) temperature of 100.4⁰ F or greater, cough, or other symptoms of COVID-19; (2) aged 65 years or older; (3) immunocompromised and/or had chronic disease; or (4) returned from international travel within the past 14 days. Strict adherence to universal precautions were recommended to minimize disease transmission. It was thought that by rescheduling patients, DCs could contribute to preventing community spread and preserving the limited supply of personal protective equipment (PPE) that was critical for frontline healthcare personnel responding to this pandemic.
The Arkansas Department of Health recommended that chiropractic offices consider several prevention measures.56 The first was to remove items such as magazines and children's toys from patient waiting areas. It also advised that a single sign-in sheet per patient be used or to sanitize digital sign-in screens and styluses after each patient used them. Sanitizing exam tables and rooms after each patient encounter was recommended. Patients and staff were asked to practice social distancing in the waiting room, patients were encouraged to wait in their cars until called in for appointments, or that an alternative waiting room procedure be offered to patients. Employers were to inform sick employees to stay home and employees who became ill were to be sent home. Respiratory etiquette and hand hygiene were advised for all employees. The Department also recommended that clinic staff perform routine environmental cleaning.
Karen Konarski-Hart
My chiropractic practice is a home office in Little Rock, the capitol city of Arkansas, located within 4 miles of several local hospitals. Many of my patients are employed in the local healthcare system and also are caretakers of family members. During the early period of the pandemic, we did not have a shelter-in-place order. During the first weeks of the outbreak, many people with possible COVID symptoms presented at healthcare facilities. As these numbers grew, hospitals became short-staffed and staff were working long shifts. Health and government officials discouraged the use of emergency or urgent care facilities except for medical necessity.
During that time, many patients who presented to my office with acute musculoskeletal concerns did not want to go to a medical facility for fear of COVID-19 exposure. I saw an increase in patients who were caregivers for their families. They often had symptoms of mental stress because of the additional duties of protecting and caring for their loved ones during the pandemic. Signs and symptoms of stress included new onset of muscle spasms, headaches, or temporomandibular joint issues. For some patients, their desire for social contact, conversation and reassurance seemed as great as the need for treatment for their musculoskeletal symptoms. Patients who were sheltering in place and no longer had social contact from their churches or social groups commented on how happy they were to see and talk face-to-face with another person during their treatment visits.
My practice normally offers random urine drug sampling for professionals who are in a program to maintain their license. Many healthcare workers in these programs frequently test at their worksite's emergency department. However, because of the fear of COVID-19 exposure, I saw an increase in these clients. Thus, my clinic was helping as an alternate location for these services.
My clinic followed the Arkansas public health recommendations. We asked patients COVID screening questions when they called for an appointment. If they were suspected of having a COVID infection, they were referred to the medical center for screening and testing. Patients were expected to enter the clinic alone unless they needed assistance. I met them wearing a gown and mask, walked them directly to the treatment room and walked them directly out after treatment. Any forms were filled out by me in the treatment room so there was minimal sharing of pens or clipboards. We kept patient appointments scheduled apart from each another to avoid contact between patients. If someone arrived early, they were asked to wait in their car or on the open porch. The treatment room had all smooth surfaces, and chair and treatment table arm rests were wrapped with disposable plastic film, which made wipe downs and spraying easier between appointments. Paper napkins were inserted in the facepiece crease and patients were gowned. I washed my hands before and after treatment and used sanitizing gel within the patients’ view. I also sprayed and wiped the table so the patients witnessed that the surfaces were clean.
Oregon, USA
The governor of Oregon increased restrictions as a response to COVID-19 starting on March 12, 2020.57 Restrictions included closing schools for 2 weeks and limiting gatherings to less than 250 people. On March 17, school closures were extended for 4 more weeks, gatherings were limited to less than 25 people, and all restaurants and bars were closed. On March 23, a mandatory shelter-in-place order banned all non-essential travel.58 Health care was considered an essential service and DCs were included as essential healthcare providers. On March 19, the governor prohibited any non-essential (ie, non-life-threatening) healthcare procedures that required the use of PPE, to conserve PPE for critical care.59
Elise G. Hewitt
My chiropractic practice includes 6 DCs (ie, 4 general chiropractic practitioners and 2 chiropractic pediatric specialists.) The clinic has an office manager and 2 receptionists. To address the community's concerns about the COVID-19 pandemic, my staff and I communicated with patients about the extra safety measures we are took to protect their health. These procedures were posted on the office web page, office Facebook (Menlo Park, CA) page, and emailed to each patient. Since much remained to be discovered about COVID-19, I continued to monitor the latest developments and modified procedures as new information warranted.
My goal was to provide chiropractic care that contributed to patients’ well-being in an office that had low risk for infection. To this end, a hospital-grade air purification system was installed on the office HVAC units. This system uses an ozone and hydroperoxides oxidation technology to eradicate 99.9% of all airborne and surface pathogens capable of eradicating the droplets of a sneeze at a 3 feet distance. We instituted additional protocols to further limit exposure. Patients were screened to identify if they were ill or were exposed to anyone ill when they scheduled an appointment and were screened again when they arrived at the office. We limited those entering the office to only those who would be treated. For pediatric patients, we asked that only 1 parent or caregiver attend the visit and that siblings who were not being treated be left home.
Once patients arrived, they were asked to remain in their cars until their treatment room was cleaned and ready, at which time they received a call from the receptionist, who opened the front door for them. Upon entering, patients were asked to clean their hands with hand sanitizer located on the front counter or with soap and water in the reception area bathroom. After this, they were escorted to their treatment room. The receptionists controlled the flow of patients so that only 1 patient was in the reception area at a time. In the treatment room, I wore a mask and took the patient's temperature before commencing with the history. Any patient with a fever was asked to go home and re-schedule once they were well. Patients were provided with COVID-19 information if needed.
Upon leaving the treatment room, if no one else was in the reception area, patients re-scheduled at the front desk. We instituted a modified method for payment in which the patient inserted and removed their own card into and from the card reader, and the receptionist completed the payment transaction. Alternatively, patients had the choice of returning immediately to their cars and then calling from their car to re-schedule, receive charges, and provide credit card information over the phone. Once the treatment was complete, surfaces touched by the patient were disinfected, such as treatment tables and door handles. At the beginning and end of every day, and hourly during the day, bathrooms and other common areas were disinfected. While these measures were necessary, they were cumbersome. As a result, we increased the length of each treatment visit to accommodate the extra time required and to keep patient overlap inside the office to a minimum.
My patients expressed gratitude for creating a safe environment in the clinic. “We are so grateful that you are open.” “I am so grateful that I can come!” “Thank you so much for being here!” I feel it is my responsibility as a health care provider to continue to provide the care my patients consider essential to their health. I and the others in my clinic strive to do this in an environment that protects the health of our patients, our staff, and the community in which we all live.
Missouri, USA
The Missouri Governor issued a stay-at-home order on April 6, 2020 that remained in effect until May 3 with the county of St Louis extending the deadline for an indefinite period of time.60 In the State of Missouri, DCs are considered essential healthcare workers as outlined in the US Department of Homeland Security memorandum on identification of essential critical infrastructure.61 Additionally, the Missouri Chiropractic Physicians Association made a statement to encourage DCs to make an educated decision about what is best for their patients, their practice, and their loved ones with their decision to continue seeing patients.62
Jason Napuli
I am a chiropractor within the Veterans Administration (VA) St. Louis Health Care System. This location serves 70 000 US veterans throughout the Eastern Missouri and Western Illinois regions. Chiropractic service is aligned with the VA's Whole Health initiative locally and within Rehabilitation and Prosthetic Services nationally.63 Chiropractic providers work closely with the veteran's primary medical provider and complimentary and integrated health teams in an effort to improve quality of life, function, and self-management strategies.
Starting on April 1, 2020, all health care at this location focused on emergent and urgent care. Many of the providers either shifted to inpatient care or screening stations while at the same time providing telehealth for their other patients. To reduce the risk of exposure to patients, my in-person visits were converted to telehealth visits. The interface I used was VA Video Connect, which is a VA technology that connects VA providers with veterans using live video in a secure appointment virtual room.64 For those veterans who were unable to connect via VA video connect, we called them by telephone.
During chiropractic telehealth visits, I took health histories, completed a limited examination, and provided patients with appropriate education, exercise, ergonomic recommendations, lifestyle instruction, and reassurance/compassion. Patient recommendations included simple movement activities, directionally preferred exercises, self-mobilizations, nutritional guidance, and overall lifestyle changes to help them self-manage their conditions. During these visits, I was able to link veterans to a variety of Whole Health virtual offerings, which included information to maintain healthy living with complimentary and integrated health self-management strategies including mindfulness, meditation, nutrition, coaching and peer support, and videos on yoga, tai chi, acupressure, postural advice, and nutritional support. Veterans indicated a high level of satisfaction with these modalities and self-management strategies. I encountered some challenges with technology including user ability, bandwidth, and dropped calls. However, veterans expressed their appreciation for the telehealth care that I was able to provide during the pandemic.
Texas, USA
On March 12, 2020, a public health disaster due to COVID-19 was declared in Dallas County.65 On March 19, Dallas County, Texas Judge Clay Jenkins issued more restrictive requirements with earlier interventions than at the state level jurisdiction to mitigate transmission.66 The Texas Governor issued an executive order closing schools, limiting statewide gatherings to less than 10 people, limiting food and beverage operations to carry-out/delivery, and closure of non-essential businesses.67 Dallas County was put under shelter-in-place orders until April 30, 2020 where Dallas County residents were advised that tiered openings of businesses would occur incrementally, dependent on county capacity for testing and tracing of positive cases. Health care operations, which included chiropractic practices, were deemed as essential businesses, where employees and patients were required to wear masks to cover the mouth and nose. Homemade coverings, bandanas, and scarves were permissible.
The Texas Board of Chiropractic Examiners confirmed chiropractic care as an essential service.68 The Texas Board of Chiropractic Examiners issued guidelines on appropriateness of chiropractic care through April 30 that stated, “Licensees should only provide essential chiropractic services for patients with current or recurrent complaints of pain or disability which adversely affects the patient's ability to engage in the essential activities of daily living or work, or adversely affects the patient's quality of life, and with anticipation of material improvement under chiropractic care.”69 As of May 1, updated orders included that licensed chiropractors could provide wellness care but, “should continue to adhere to safety and prevention best practices specified in the most current advice from the Centers for Disease Control.”70
William Foshee
My chiropractic practice is in Dallas, Texas, which is a city of 1.345 million people. I am an employee in a group practice with up to 2 chiropractors working on any given day before the pandemic began. My patients often begin care with a musculoskeletal complaint and transition to wellness care depending on patient preferences. Many of my patients are ethnic minority. I regularly treat patients who primarily speak Spanish. I also serve a large portion of the sexual minority population, which is represented by those whose sexual identity, orientation or practices differ from the majority, such as lesbian, gay, bisexual, or transgender. Sexual minorities may have different risk factors and experience poorer health outcomes and therefore may be at greater risk.71 I also have a small, solo practice where my patients are almost exclusively sexual minorities. I limit patients in my solo practice to active care.
During the early response to COVID-19, clinic intake procedures included screening patients for fever, symptomatology, and travel history. Assessment and treatment were limited to individuals who denied international or out-of-state travel in the previous 2 weeks, infection or known contact with a person experiencing COVID-19, and history of fever, cough, shortness of breath, dysgeusia, or hyposmia in the previous 2 weeks. All of this information was noted in patient records. Prospective and existing patients were delayed care for 2-weeks or until their responses were compatible with the screening requirements. I disinfected the treatment table between patients and sanitized frequently touched surfaces. I asked patients to wait in their cars until the time of treatment. Alcohol-based hand sanitizer and tissues were available in all spaces accessible to patients. There were no other items for patients to touch, as pens were sanitized between patients and all other material, magazines, and water cooler were removed. Spinal manipulation was limited to prone and instrument assisted techniques to better control the direction and velocity of forced expiratory projection.
New and existing patients presented with musculoskeletal complaints such as radiculopathy, tension pattern headache, posture induced musculoskeletal pain from working at home, injuries related to home improvement projects, and exacerbations of chronic or ongoing complaints. I noticed that patients seemed to be more sensitive and had a lower pain tolerance, possibly due to the additional mental stress because of the pandemic.
New York, USA
New York (NY) state was an epicenter of the US COVID-19 pandemic. Executive orders in NY state limited business activity to essential business, later clarified to include emergency chiropractic services.72 This guidance allowed chiropractic practices to remain open. The impact of COVID-19 varied widely throughout the state. Many chiropractors in NY voluntarily closed their practices out of service to public health, patient protection, or due to risks to providers/staff. For those practices that remained open, emergency chiropractic services included management of urgent and necessary neuromusculoskeletal conditions to avoid overwhelming emergency care settings. Services provided to essential front-line workers allowed them to continue necessary functions. When face to face care was not possible, an executive order allowed NY chiropractors to provide telemedicine services so that patients could access clinical advice in self-care, home exercise, ergonomics, nutrition, and stress management.73 , 74
New York agencies advised that by April 15 PPE was required to be provided to all workers in essential businesses that had contact with the public.75 This included office staff with patient contact and clinical providers. Beginning on April 17, the general public was required to wear protective masks whenever they were in public and could not social distance; attending an office visit fit this description.76
Jason Brown
My practice is in a suburban setting near Albany, NY. The practice has 2 chiropractors and 2 staff members. We modified the schedule so that only 1 practitioner and 1 staff member were working at any given time to lessen exposure and maximize space and distancing in the office. During that time, patients who received wellness and supportive care were advised to delay care until the crisis passed. For some patients needing supportive care and who would have severe progression of symptoms, care was delivered judiciously. The practice operated at a small fraction of normal volume, with most care provided to essential front-line workers, such as those in healthcare, first responders, and other essential business functions. Acute and urgent musculoskeletal conditions were triaged and managed with an emphasis on self-care so patients could recover while maximizing their ability to remain at home.
Patients were scheduled with extra time between visits to minimize patient-to-patient contact in the reception area. Increased time between visits also provided opportunity for a thorough disinfecting of all treatment surfaces and equipment and periodic disinfecting of commonly contacted surfaces such as countertops and doorknobs. Steps were taken to reduce or eliminate exchanges between patients and staff.
I noticed an increase in repetitive strain injuries. Work-from-home orders for non-essential workers throughout NY state led many people to use makeshift home office arrangements. An often less than ideal ergonomic environment seemed to contribute to increased reporting of postural and repetitive strain injuries. Therefore, I found that advice for home office ergonomics was helpful for patients. Further, social isolation as well as fear and anxiety around both the infectious and financial aspects of COVID-19 heightened patients’ needs for psychosocial interventions.
To address patient concerns, we worked to establish procedures for managing disease symptoms or exposures. We gathered state and national resources to provide patients with accurate and actionable information. We provided access to home resources including yoga and meditation apps or Internet sites, home exercise options, and financial resources.
Ontario, Canada
On April 11, 2020, Canada implemented the COVID-19 Emergency Response Act, enabling government to make sweeping changes for the protection of the public.77 In March, Ontario implemented an emergency order shutting down all non-essential workplaces as required by the Directive from the Chief Medical Officer of Health.78 Chiropractors were required to close their offices, except for limited weekly hours for treating only patients with urgent musculoskeletal needs. The federal government implemented economic measures (ie, wage and business subsidies) to enable businesses and employers, including chiropractors, to apply for specified monthly income benefits to help offset business costs and also to cover 75% of employee wages during the period of ‘pause’ to minimize layoffs and lost jobs. On March 24, closures of public places followed.79 Self-isolation, social distancing, frequent hand-washing, working from home, the use of cloth masks when shopping for groceries were implemented. The chiropractic regulatory authorities enabled chiropractors to provide telehealth visits, outlining standards for virtual practice.80 Professional liability insurance was assured for virtual chiropractic visits. The Canadian Chiropractic Association created an evidence-based Telehealth Best Practice Guide, for chiropractors.81
Deborah Kopansky-Giles
I coordinate chiropractic practices at St. Michael's Hospital in the family medicine program. During that time, most ambulatory in-person health services were cancelled, except for essential medical visits. All chiropractic patients were notified by phone that in-person visits were not allowed. However, care continued through telehealth visits provided on a ministry of health supported platform enabling both audio and visual interactivity, depending on the patient's available technology.
Through virtual visits, patients reported their concerns, progress, demonstrated prescribed exercises and ranges of motion, performed functional tests, and received instructions for exercises. Chiropractic care included providing reassurance, advice (such as pacing strategies, pain coping techniques), and COVID-19 prevention education. Collaboration with patients’ medical physicians, pharmacists, or other health team members was facilitated through the electronic medical record or by phone. New patients with urgent musculoskeletal complaints were screened by telephone and provided with advice and education as indicated. If these patients requested an in-person visit, they were referred to a local, collaborating chiropractor who provided this care. We monitored patients who used telehealth to better understand the musculoskeletal conditions that may have resulted from isolation due to COVID-19.
This practice serves the inner city of Toronto, reaching the poorest and most vulnerable populations in Ontario. At my location, chiropractors participated in Wellness Check-Ins, which is a department-wide initiative. We identified individuals who were vulnerable or high risk for severe COVID-19 impact and contacted them by phone to see how they were doing and to linked them with people and resources. Over 4700 of the patients in our clinic database met the criteria for this initiative. By keeping people informed and feeling connected to their health team, particularly for seniors and low-income quintile patients, we hoped to minimize the impact of the COVID-19 pandemic on their physical and mental health.
Alberta, Canada
Alberta Canada's first case of COVID-19 was reported on March 5, 2020.82 On March 17, a public health state of emergency was declared for the province.83 Alberta's public health response included restricting mass gatherings to fewer than 15 people, restricting visitation to health and senior care facilities, canceling international travel, and closing schools and non-essential businesses, facilities, and services.84 Citizens were strongly encouraged by the government to stay at home, abide by social distancing rules, do frequent handwashing, and wear masks in public spaces.
Effective March 23, the Alberta College and Association of Chiropractors (ACAC) suspended mobile visits (ie, any visit that does not take place in a clinical environment) and strongly recommended that chiropractors only engage in urgent care.85 The ACAC Council approved a temporary permission for chiropractors to engage in telehealth with authorization from the Registrar. On March 27, the Chief Medical Officer of Health of the Government of Alberta ordered the closure of close contact businesses, including chiropractic services, with the exception of urgent, critical, and emergency care.86
Kent Stuber
My practice is a mobile practice, which means I do not practice in a traditional clinic. Instead, I provide chiropractic care at the patient's location. After mobile visits were suspended, I communicated with my patients and updated them on practice status by telephone, text messaging, videoconference, or e-mail. I informed them to contact me if they had any questions. I encouraged them to follow the advice of provincial and national public health officials. I advised patients to continue their active care plans for their musculoskeletal conditions, to be active on a daily basis, and to engage in mental health self-care, such as relaxation or meditation exercises. I obtained permission from the Registrar to engage in telehealth visits. I maintained contact with patients to provide ongoing encouragement and follow-up. Patients who required urgent care were referred to local chiropractors for in-person care. Patients with stress, depression, anxiety, or grief were referred to mental health services for counselling.
Caterina Lerede
My chiropractic practice is in a multiprofessional clinic, which includes other providers who are in the fields of physical therapy, massage therapy, and naturopathic medicine. I obtained permission from the Registrar to engage in telehealth visits. Beginning March 23, non-urgent chiropractic visits were cancelled. Communications occurred primarily by telephone, text messaging, and e-mail. I saw patients with pain and disability who were unable to self-manage any longer. Patients who met the criteria for an urgent, critical, or emergency visit were scheduled for an in-person visit. If they did not meet the criteria, I provided home care options. If patients met the criteria, they were screened for signs or symptoms of COVID-19 or for any risks of possible exposure. Patients who passed screening criteria were booked for an appointment; any who did not were referred to public health services for evaluation. I contacted patients to provide advice and encouragement. Steps to reduce exposure risk to patients and staff included disinfection of all examination and treatment surfaces and instruments between all patients, and social distancing. For example, we reduced the number of chairs and increased the distance between them in the waiting room. We staggered appointments to minimize risk of patient exposure in passing and installed a plexiglass shield at the front desk between the receptionist and the patients.
Queensland, Australia
During that time, the Australian federal and state governments enacted restrictions including closing of international and state borders, closing of “non-essential” businesses, restrictions on gatherings, strict physical distancing, and orders to stay at home.87 For Australian citizens, social contact was limited to visiting a romantic partner, supporting a family member, providing compassionate care and visiting a terminally ill friend. Exceptions to the stay-at-home rules included shopping for essentials, work or education, medical (including allied health) appointments and exercise. Inconsistency in state and federal rules meant we ceased all remedial massage therapy.
Scott Charlton
My practice consists of myself, a massage therapist, and 3 administrative and rehabilitation support staff. We are located on the edge of the city of Ipswich, approximately 30 miles from Brisbane, the capital city of Queensland. My practice is in between a small city and rural area, serving both those nearby and from surrounding rural communities.
I restricted my practice to patients with acute pain and actively discouraged at-risk populations from attending. All patients were screened for whether they recently participated in overseas travel, had close contact with confirmed cases and if they had any flu like symptoms. All staff in the practice completed and were certified in the department of health online COVID-19 infection control training.88 Large signs were posted before and at the entry to the practice outlining the clinic procedures. Hand sanitizer was provided in various stations throughout the clinic. The lack of reliable supply of basic cleaning products led me to use a specialist dental sanitizer that was effective against COVID-19. We sanitized all surfaces in treatment rooms and all touch points in the clinic between each patient.
Appointments were modified to ensure strict physical distancing. Physical distancing rules in businesses evolved at that time to limit the number of people within a premise or a meeting room to no more than 1 per 4 square meters.89 My office size permitted 22 people at any given time, though we elected to allow a maximum of 8 including staff. We removed most seating and provided measured compliant distances to reduce potential patient exposure. We removed all magazines and pamphlets as well as all toys, books, and furniture from the children's area. We posted government endorsed signage throughout the practice that reinforced public health messages. All patients and staff were temperature scanned, observed for signs of being unwell and asked screening questions by the chiropractor in addition to administrative staff on each visit.
The advice from the Australian government and WHO was that PPE was in limited supply and should be reserved for front-line workers either with symptoms or treating those with symptoms.11 , 13 , 54 , 90 For this reason, we elected not to use face masks at all times. Masks were available for patients to use or have me use if requested. I modified history taking to be at a minimum 2 meter distance from the patient. Examination and treatment procedures were modified to minimize droplet transmission wherever possible.
In my practice, we serve a portion of a lower socioeconomic population including many older patients and those with mental health illness. For those at likely higher risk due to COVID-19 (eg, elderly, immunocompromised), we actively provided outreach by calling and advising patients not to attend unless their need was particularly urgent. I provided patients with regular electronic communications including updates on government recommendations and the approaches being used to help keep the clinic safe. I offered phone and telehealth consultations to patients as a means of easing their anxiety and answering any concerns.
Hampshire, United Kingdom
In late January 2020, SARS-CoV-2 first arrived in the United Kingdom (UK) carried by returning travelers.91 At that time, the national health authorities produced advice on physical distancing and hygiene in a public health campaign. New laws were introduced (The Health Protection (Coronavirus) Regulations 2020) in March, which provided the Government with powers to control movement of potentially infected individuals.92
In the second week of March, anyone with a new continuous cough or a fever was told to self-isolate for 7 days and vulnerable groups (ie, aged over 70, or with certain medical conditions or other risk factors) were advised to self-isolate at home. The following week, the UK Prime Minister curtailed all non-essential travel and contact with others. Elective hospital activity was stopped and schools were closed, other than where needed to look after children who were considered vulnerable or children of key workers.93 Places where people might gather, such as non-food shops, pubs and cinemas, were shut down.94 Work began at several large venues in key locations to convert them into temporary hospitals to provide an additional 10 000 specialist beds.
Chiropractic clinics were considered exempt from closure. However, on March 24, the Royal College of Chiropractors, the British Chiropractic Association, and the McTimoney Chiropractic Association published advice stating that provision of clinic-based care was incompatible with government guidance on social distancing and safe practice, effectively closing the chiropractic profession to face-to-face care.95, 96, 97
Jonathan Field
I work as a chiropractic first contact practitioner in a state funded National Health Services primary care facility, and work in a Chiropractic Research Council funded university fellowship role for 2 days a week. In the second week of March, all medical services within the practice moved to telephone or video consultations for vulnerable groups, with this extending to all but those with critical health needs by the end of the month. On March 23, I was released from my research activity, which enabled me to take on additional clinical duties to help free up a medical doctor to work at the hospital. Since the enacting of emergency information technology system protocols within the clinic we had remote access to patients’ electronic health records. This meant whilst conducting a full schedule of telehealth consultations 5 days a week, I was able to isolate with my family and, along with others in the population, leave home only for 1 period of exercise a day and 1 shopping trip a week.
Many members of the chiropractic profession in the UK responded to the Health Protection (Coronavirus) Regulations by exploring new ways to engage with and support their patients. Some implemented virtual appointments, while others volunteered to help in other roles within the national response to the current crisis. I created a support group using Slack (Slack Technologies, San Francisco, CA, USA) to help chiropractors in the UK learn about how to set up practice for remote consultations, including the technology and differences in the way consultations are conducted including the care that can be provided and the way we communicate.
Bahia, Brazil
As of April 28, 2020, Brazil had the second largest number of people infected with coronavirus in North and South America, second to the US.98 The first confirmed COVID-19 case in Brazil was on February 26, 2020.99 The first COVID-19 related death in Brazil was on March 17.100 From that point on, some states and cities implemented lockdown measures. On March 18, a national state of emergency was declared by the Brazilian national congress, and lockdown and social distancing measures were widely recommended and implemented, following ministry of health recommendations.101 Initial lockdown recommendations were set to last for 15 days but were extended with adherence, depending on location. Healthcare providers were considered vital in this coping process and were not included in any lockdown measures. Telehealth consultations were provisionally accepted and recommended as an important tool to assist patients.102
Social distancing and transmission preventive measures were adopted by the Brazilian authorities.103 The use of face masks was mandatory for any worker in direct contact with the public. Some major cities extended this as mandatory for anyone outdoors. Due the lack of surgical masks available, double layer cloth homemade individual masks were considered acceptable by the ministry of health. People were to wash their hands for 20 seconds or use hand sanitizer (70% alcohol). People were not to share personal items (eg, towels, tableware, glasses). Citizens were to implement social distancing of 2 m between individuals in any public space and avoid going outdoors. Places where people may crowd were closed (eg, shopping malls, gyms, stores, clubs, and restaurants that now only work in a delivery basis) Essential services such as health, food industry, transportation, and others were allowed to remain open.
Marcelo Botelho
My chiropractic practice is located inside a private hospital. On March 29, the first reported COVID-19 related death in my state (Bahia) was at this hospital. Some chiropractors nationwide decided to close their clinics in the first 2-3 weeks after the state of emergency was declared. I continued to see patients who had ongoing treatment needs and who were in severe pain but avoided new patient admissions. I reestablished front office services approximately 4 weeks after the state of emergency was declared. To increase the efficacy of transmission prevention, the following measures were implemented in my clinic: Face mask use was mandatory for myself, all staff members and other health care providers in the hospital. All patients were asked to wear face masks. If the patient presented without a mask, the clinic provided a mask. Patients were asked to use hand sanitizer when arriving and before leaving the clinic. Patients were informed, by cell phone message, about relevant information regarding prevention and relevant updates. These messages included the need to inform the clinic of suspected symptoms prior of clinical attendance, and to reschedule their appointments for a later date if it was the case. I modified the treatment schedule to have patient appointments at double-spaced intervals to avoid contact between patients. In between patient visits, my staff and I carefully cleaned the treatment tables with 70% alcohol, and also chairs, desk and any other surfaces the patient may have contacted. Full clinic cleaning with antiseptic material was done every 4 hours.
Gauteng, South Africa
On March 15, 2020, the South African (SA) leadership declared a state of disaster due to COVID-19.104 After this, citizens were placed on a lockdown beginning March 27.105 The regulations governing the state of disaster dictated only essential services could continue, including emergency medical treatment.
During that time, SA had comparatively few cases, few deaths, and large numbers of people who recovered from COVID-19. The minister of health, Dr Zweli Mkhize, reported daily to the nation, warning that the worst was yet to come, and complacency would not be tolerated. Because of the reduced demand on the health care system, SA was able to secure PPE, ventilators, and test kits. The National Department of Health had set up community test centers and secured 60 vehicles for mobile screening particularly in high risk areas such as townships. The National Institute for Communicable Diseases (NICD) monitored the COVID-19 pandemic in SA.106 Although there were some areas that did not have enough PPE or sufficient testing facilities, this was minimal. Dedicated wards in hospitals were allocated. The homeless were sheltered, and the food package scheme gained momentum. The gap that needed attention was relief funding. Chiropractors in SA were only allowed to register as sole proprietors, but the relief funding for such sole proprietors was extremely limited. This was concerning, as many chiropractors were challenged to sustain a lockdown for an extended period of time. There were relief funds for registered businesses, however, with little to no relief funding for practitioners, there was a concern that many would not be able to practice once the lockdown was lifted. Registered businesses only had the option of loans, but no chiropractor was able to register as a business.
All registered health care providers, including chiropractors, were permitted to consult emergency patients. Those essential to the COVID–19 pandemic (ie, the front-line staff for screening, testing, and treating) were permitted to be at work. Chiropractors were permitted to consult in person only for patients with emergencies (eg, the patient may lose life or limb, or seriously deteriorate, if they did not receive intervention). To see patients, all health care providers required a permit as issued by their regulatory authority. The regulations for the Allied Health Professions Council of South Africa and the Health Professions Council of South Africa registered professions was amended to allow telemedicine. Malpractice insurance and medical aid administrators were mobilized to bring policy in line with the amended regulations.
The Chiropractic Association of South Africa (CASA) issued an advisory to its members to adhere to the regulations and to close their practices. Chiropractors were informed that they were allowed only to consult with patients with emergency conditions and to adhere to strict PPE protocol. The CASA initiated a series of webinars, to educate chiropractors on the topics of COVID-19 as well as telehealth, and a presentation on the increase and change in hygiene protocol which needs to be followed. These courses allowed practitioners to gain continuing education credits at that time.
Kendrah L Da Silva
I served on the advisory team for the medical response to the COVID–19 pandemic in SA. My practice is located in an urban area. I have a solo practice and do not employ any staff, other than cleaning staff. Since the state of disaster began, I kept my practice open for telehealth consults. I use the Medici platform (Medici Technologies, LLC, Austin, TX, USA) to participate in telehealth consultations with my patients. Most patients expressed that they wished to wait for the face-to-face consult once the lockdown orders have been removed. Patients who participated in telehealth visits responded positively about the encounter and many experienced a reduction in their chief complaint, such as pain.
Before the lockdown was implemented, when I was seeing patients with face-to-face visits, I put out hand sanitizer for the patients. I have always sanitized before each patient, and handwashing after each patient. Therefore, these practices continued. I wore a surgical mask and a coat, which was washed at the end of each day. Most patients at that time wore their own masks. All touch surfaces were sanitized between patients. Patients were booked with sanitization gaps in between. I informed my patients through electronic communications. Information sent to patients originated from the South African COVID–19 response, the WFC, and CASA. For patients needing more personal attention, I helped by telephone or by video teleconsultations.
Amsterdam, Netherlands
Starting March 16, 2020, on orders of the Dutch government, schools, day care centers and restaurants closed, and working from home was encouraged.107 A week later, government leaders announced a partial lockdown to allow hospitals to cope with increasing presentations of patients with COVID-19 and to allow a level of herd immunity to develop. Essential shops were allowed to remain open, however everything else was closed. Citizens were not allowed to gather in a group of more than 3 in a public space and had to keep 1.5 meter distance apart from others at all times. All cultural and sporting events in the Netherlands were cancelled until September 1.108
In the Netherlands, chiropractic is an unregulated profession. However, patients do not need a referral to see a chiropractor.109 On March 23, the Netherlands National Institute for Public Health and the Environment (ie, known as Rijksinstituut voor Volksgezondheid en Milieu (RIVM)) increased public protection and limited health care provision for hands-on and para-medical professions. Thus, only telehealth visits were allowed.110 , 111 On April 15, the Netherlands Chiropractors Association (NCA) aided clarification that chiropractors were allowed to treat severe cases using PPE measures. Thus, chiropractic care was opened back up, “in exceptional cases if the patient has a medical indication for this, the care cannot be given remotely or cannot be postponed and the practitioner during the treatment can comply with all advice from RIVM regarding personal protective equipment.”111 On April 29, the RIVM changed the regulations again, resulting in chiropractors and other alternative care providers to be limited to only telehealth visits through May 11.112
Gitte Tønner
I practice chiropractic in a small solo practice in Amsterdam. My patients have predominantly chronic and complex concerns with a variety of co-morbidities. Following the governmental regulations, I saw patients with severe symptoms from March 16 to 23, which was followed by not seeing patients between March 23 and April 15. Between April 15 and 29, I saw patients again. I was very selective to which patients I saw since the risk of patients contracting the COVID-19 could potentially increase when patients were traveling to and from the appointment. To answer their questions and concerns, I offered email consultations for my patients.
When I was seeing patients, as per the NCA hygiene standards, I wore an N95 mask, gloves, and a shirt exclusively for seeing patients. Patients were asked to wash their hands thoroughly when they entered my clinic. My chiropractic table was outfitted with disposable layers for each patient. After each session, all disposables were thrown out. The chiropractic table and surfaces that were touched were cleaned. To avoid touch transactions, payment and receipts occurred electronically. After the visit, I cleaned the door handles as patients exited. I indicated in the patient clinical record the level of urgency of the patient's concern and the hygiene measures provided. Three days after the treatment I emailed the patients to ascertain how they responded to chiropractic care and if they developed any symptoms of COVID-19.
Singapore
On January 23, 2020, the first case of the COVID-19 infection infiltrated the shores of Singapore.113 Prior to that, the government was already keeping a close eye on the spread of disease at ground zero, Wuhan, China as the number of Chinese travelers for leisure and business to Singapore, hit 3.6 million visits in 2019.114 Hence, it was not a matter of if the disease would reach the shores of Singapore, but a matter of when. On April 7, 2020, the government implemented restraints to contain the spread of the disease.115 Jobs that the government deemed as non-essential were required to cease and people to work from home. The chiropractic profession was initially regarded as an essential occupation but was later removed for unknown reasons. Then, it was reinstated but then removed again. The Chiropractic Association (Singapore) penned an email to the Ministry of Health (Singapore) to appeal for reinstatement but this appeal was rejected. Even though we were disappointed, chiropractors abided by the Ministry of Health's decision that they should remain closed at that time.
Terrance B.K. Yap
My practice is in Singapore, which is a multiracial and multicultural country. Prior to closing my clinic on April 7, I took the proper hygiene measures such as social distancing, wearing a face mask, and temperature reading for all staff and patients. The air was regularly sanitized and clinic equipment disinfected after each patient. Additionally, patients were required to answer and sign a travel declaration at every visit, enabling contact tracing if necessary. Patients were to rest at home or seek medical attention if they had flu symptoms. These preventive measures were to safeguard patients and staff as well as to assure the public.
Athens, Greece
On February 26, 2020, COVID-19 first appeared in Greece.116 Through early March, state authorities issued precautionary guidelines and recommendations were implemented locally to include the closure of schools and the suspension of cultural and sports events in the affected geographical regions. On March 10, with 89 confirmed cases and no deaths yet in the country, the government suspended the operation of all educational institutions nationwide117 and on March 13 all parades, cafes, bars, restaurants, museums, shopping centers, and sports facilities in the country were closed.118 On March 16, all retail shops were closed and all services for religious worship of any religion were suspended.119 Following this, the government announced a series of financial support measuring 10 billion Euros to support the economy, including chiropractors.120
On March 23, restriction on all non-essential citizen movement throughout Greece was imposed.121 Since that date, movement outside the house is permitted only for 7 reasons, including going to the pharmacy or visiting a health care practitioner. Police identity or passport, as well as a signed attestation in which the purpose or category of movement is stated is required in order to move in public. The Greek law enforcement authorities are empowered to enforce restrictions and can issue fines for each offense. These measures were considered among the most proactive and strict in Europe and were reported by international press as the reason behind slowing the spread of the disease and having kept the number of deaths among the lowest in Europe.122 , 123
Chiropractic practices had not been asked to shut down by the authorities. However, on March 15, due to the lack of chiropractic legislation, regulation, and malpractice insurance, the Hellenic Chiropractors’ Association recommended that its’ members enact a complete shutdown of chiropractic practices in the name of public safety. In the absence of any recognition and or communication between the health care authorities and the chiropractic profession, it was prioritized to act responsibly and take no unnecessary risks in contributing to the spread of the disease.
Vasileios S Gkolfinopoulos
My chiropractic practice is a general practice. My practice was one of the first in the country shut down on March 12. Before closing and since March 2, my office was operating with strict precaution measures in place in the form of: spacing out of appointments; repetitive disinfection of all surfaces during the day; toilet disinfection after each use; hand sanitizer available in the reception area and treatment rooms; use of mask and gloves by practitioner; thorough disinfection of treatment benches before and after every treatment. Patients were screened by telephone and if they exhibited any known symptoms of COVID-19 they were advised to stay at home. Following the government orders for shutdown, I provided services by phone. These included advice on self-care, reassurance, psychological support, ergonomics, recommendations for diet/supplements, and rehabilitative exercises.
Bucaramanga, Colombia
On March 6, 2020, the first 3 COVID-19 cases were reported in Colombia. On March 12, the government declared a state of emergency.124 On March 24, mandatory confinement started and was extended until May 11.125 Health workers initially were only allowed to work if they worked with concerns related to COVID-19 patients. However, on April 27, general practices were allowed to open with strict bio-safety protocols.126 Other restrictions were reduced to include 35 other economic activities, such as construction, manufacture, and agriculture. Adults could exercise outside while practicing social distancing during early morning. Air and ground transportation were restricted only for passengers.
Gabriel Quintero
My chiropractic practice is in the city of Bucaramanga. I practice solo with 1 chiropractic assistant, 1 accountant, and the clinic manager. When the outbreak started, I followed increased safety procedures in my practice, which included increased hand washing, wearing a mask, and no hand shaking to welcome patients. The doors and windows were opened to let air circulate. On March 19, I closed my practice following government recommendations. Since that time, I informed my patients via telehealth using WhatsApp (Menlo Park, California) and e-mail to stay home following government orders. I provided patients with important information in response to COVID-19. I advised them about improving posture, maintaining lumbar support when sitting, especially for those who are working at home. I educated them about using an orthopedic pillow when in bed, proper hydration, good nutrition, decreasing refined sugar intake, and proper breathing methods. For those who had musculoskeletal complaints, I provided recommendations depending on their need, such as information about ice, exercise, and stretching. I emphasized the importance of mobility since sedentary life has negative consequences for the spine and general health.
I have a general practice that normally sees about 40 patients per day, 5 days a week. Once general practice was allowed to reopen, I followed strict sanitary protocols. My staff and I took the COVID-19 test. If a test was positive and the person was asymptomatic, that person stayed home isolated in quarantine until the next COVID-19 test was negative. If positive and symptomatic, the person would have been hospitalized for treatment. No more than 4 patients were scheduled per hour in the clinic, each patient participated with disinfection and temperature measurement when entering the clinic. Patients wore masks. My staff and I wore gloves, masks and disposable gowns. Areas of contact by the patient, such as treatment tables and areas in the reception room, were disinfected after each patient.
Izmir, Turkey
The first cases of COVID-19 in the Eastern Mediterranean and Middle East region was reported on February 19, 2020 in İran.127 The first case of COVID-19 in Turkey was detected on March 11.128 Since then, the Turkish authorities took systematic measures to control the spread of the coronavirus. The office of the Deputy Prime Ministry and Ministry of Foreign Affairs of the Turkish Republic of Northern Cyprus extended a partial curfew and travel ban to try to mitigate the spread of the disease.129 All people who were infected were sent to a designated hospital for testing, treatment, and observation under quarantine guidelines for 14 days. There were restrictions in travel to and from provinces that were most affected. There was a partial curfew on leaving home during the weekdays and a complete curfew on weekends. All museums, archaeological sites and public gathering places, including cafes, parks, swimming pools, barber shops and sports centers were closed. Restaurants were closed except for take-away or delivery services. Residents under the age of 20, and aged 65 and above, were directed not to leave their homes. All individuals were to wear cloth face coverings in supermarkets and workplaces as well as in all forms of transportation including private vehicles with at least 2 persons inside. Local authorities could put in place additional COVID-19 restrictions with little or no advanced notice.130
Mustafa H. Agaoglu
As a chiropractor and a law-abiding citizen, I support the decisions of the national authorities. My office was closed except for 1 day of the week to support patients with noncomplicated, acute spine pain causing daily disability. One of my priorities was to care for health care providers working in local hospitals caring for patients with COVID-19.
Patient communication in my office was by telephone. I recommended home care, such as exercises. When caring for patients in person, the patients were required to have government issued N-95 face masks. Patients were required to take off their shoes outside of the office. We provided surgical overshoes for patients. Patients were required to thoroughly wash their hands before entering the chiropractic treatment space. Payments for care were accepted through bank account wire. Chiropractic tables were sanitized between each patient visit. Patients were provided with standard government issued flyers with public health information for how to keep themselves and their family clean and sanitized. The hazards of smoking and positives of not smoking were shared extensively. Patients were directed to the WHO and Turkish health ministry updates for information and advised to stay away from social media news agencies on the matter to prevent the spread of misinformation. Any patients who showed signs of anxiety or panic were given reassurance and empathy. As a policy of my clinic, I always have shown empathy to the urgent needs of my patients and the public. I aim to provide the best available service and unconditional caring is always a priority. Those in economic hardship have always been dealt with humanely.
Discussion
As far as the authors are aware, this is the first published report that describes individual chiropractic practitioners’ experiences and responses to the COVID-19 pandemic. This study was based on a constructivist and naturalistic position and each practitioner was bound by their local regulations; therefore, some degree of variation was expected. The experiences represented here, as of May 4, ranged from the country with the greatest number of confirmed cases of COVID-19 to other countries with fewer cases. This sample covers all 7 WFC regions (ie, African, Asian, Eastern Mediterranean, European, Latin American, North American, and Pacific) and provides insights into measures being taken by chiropractors around the world during the COVID-19 pandemic.
As demonstrated in this sample, chiropractors work in a variety of settings,17 each of which may have an influence on responses during a disaster or pandemic. Environments in this report include solo practice, health care teams in hospitals, care in the VA health system, a worksite health center, group practice, and a solo mobile practice.17 Each work environment has its own unique requirements for day-to-day operations, but these may be especially different when facing a natural disaster or pandemic.
For the chiropractors who practiced in solo practice, they assumed responsibility for the function of the office, including patient care, communications, and sanitation. Solo practitioners may have had fewer resources but were able to respond quickly. In group private practice, chiropractors worked with each other and contributed to the practice. Coordination among group practitioners regarding emerging clinic policies provided consistency of care. In other settings, chiropractors worked with other health professionals, such as medical providers, physical therapists, acupuncturists, massage therapists, or other health providers. In a worksite health center, the practitioners provided care for employees of a company and therefore the company's policies may have influenced processes, such as policies for hygiene or if employees were requested to work from home. Hospital-based care (eg, private hospital, VA hospital) provided chiropractors with access to resources, such as staff and supplies. However, hospitals had their own regulations in addition to local government regulations, such as for infection control and which providers on the workforce may continue care face-to-face. Thus, those in more integrated practice settings or hospitals may have had more resources but needed to consider additional policies and mandates that resulted from the more complex infrastructure.
Themes were observed among these independent reports. A primary theme was that the practitioners focused on their primary duty, which is to serve others. They took great efforts to protect the health of their staff, patients, and the public. Some transitioned from in-office visits to telehealth visits, when that was available, or shut down their practices if the government required this or if they felt that it was prudent. Others continued to see patients in their clinic complying with public health regulations. For those continuing to practice, they established a safe working environment so that their services could continue. Many modified their practices by increasing the use of available technology to reach patients who needed care. This included using telehealth, which provides health care remotely through telecommunications technology (eg, email, phone, and video conferencing.) And, many focused their care to serve front-line health care workers, who were responsible for taking care of patients who were acutely sick with COVID-19.
Another theme was responsiveness. Each practitioner responded to unique timelines, government regulations, and regional restrictions as COVID-19 increased in prevalence. Chiropractors witnessed regulations that changed frequently, which sometimes resulted in contradicting instructions. Despite these challenges, these chiropractors complied with local regulations and health boards and adhered to the recommendations of global and national bodies, such as WHO and the Centers for Disease Control and Prevention. They monitored changes in regulations and modified their practices to be compliant.
Another theme was the application of person-centered care, which is when a practitioner has respect for patients’ preferences and values and provides them with information to help decide when to seek care and when to engage in self-care.26 The chiropractors communicated with their patients about the pandemic situation, including what care was available, how to access care, and other helpful health information about COVID-19. They viewed their patients’ needs from their patients’ points of view, such as reducing potential exposure within the clinic and in other environments, such as traveling to and from the clinic or while waiting for their appointments.
Their observations were congruent with the biopsychosocial model. In addition to the typical physical concerns that patients present to for chiropractic care, such as neck and back pain, the chiropractors observed that the pandemic likely resulted in their patients experiencing increased mental health concerns and physical signs and symptoms due to stress. The association of mental health and musculoskeletal pain and dysfunction is an important part of the biopsychosocial model of health care.26 These observations of mental health symptoms and the COVID-19 pandemic are congruent with the observations of WHO.131
These chiropractors demonstrated collaborative behaviors. They worked with others within their local regulations. Those in solo practice who did not offer in-person visits, referred patients to other practitioners. Those in group practices or hospitals coordinated with and supported other providers. They demonstrated teamwork with other health care providers across disciplines and by doing so potentially helped to reduce redundancy of consultations and provide more effective and safer care.26
In summary, even though most of the participants were in different countries or types of practices, their responses were relatively consistent. They abided by national and WHO recommendations and they adopted innovative strategies to maintain connectivity with patients through a people-centered, integrated, and collaborative approach. They described that providing care was especially challenging when the evidence needed to make decisions and local regulations continued to change. They focused first on serving their patients, including front-line healthcare personnel, and continued to monitor the COVID-19 situation and responded accordingly as new regulations and information became available.
Limitations
Each practitioner's report was limited in length. Thus, a detailed recount of each practitioner's operating procedures during the early phase of the COVID-19 pandemic was not possible. This report is limited to the individuals who responded during a 2-week period in the early months of the COVID-19 pandemic. The statements must be taken in a retrospective context and not applied to future practice. Future behaviors will likely change as new information is learned, as government and local restrictions are modified, and as situations change. Some settings included in this report may not necessarily be considered typical practice environments for other chiropractors. For example, we recognize that chiropractic practice in a private hospital may differ from an independent practitioner working in a solo practice. However, the aim was to provide breadth of view instead of demonstrating similar samples. The invitation list of providers was created by the primary author without the knowledge or input of the other coauthors thus, the participants reflects the bias of this author. There may be non-responder bias since those who did not reply were not included. Due to space and time, not all locations or countries are represented. Thus, it is not known what response practitioners from other countries may have had and how those responses may have influenced the themes noted. Those represented here do not necessarily represent everyone in their region or the entire profession, however this information can provide some insight into how some chiropractors responded. The information provided here was the best available at the time of writing. Regulations have likely changed since the time of capture of this information.
Conclusion
Although the chiropractors in this report practice in different cities and countries, their compliance with changing local regulations, concern for staff and patient safety, and people-centered responses were consistent. They did outreach and communicated with patients and they observed increased stress and mental health issues. They recognized and abided by changing governmental regulations and they adopted innovative strategies to communicate with and provide care for patients. This sample covers all 7 WFC regions (i.e., African, Asian, Eastern Mediterranean, European, Latin American, North American, and Pacific) and provides insights into measures being taken by chiropractors during the early stages of the COVID-19 pandemic. This information may assist the chiropractic profession as it prepares for different scenarios as new information about this disease evolves.
Funding Sources and Conflicts of Interest
The authors received no funding or support for this study. The views and opinions expressed in this paper are those of the authors and do not necessarily reflect the official policy or position of any agency, educational institution, or association (eg, American Chiropractic Association (ACA), European Chiropractors’ Union (ECU), National Chiropractic Mutual Insurance Company (NCMIC), National University of Health Sciences, New York State Chiropractic Association (NYSCA), Royal College of Chiropractors, St Louis VA Health Care System, Stanford Health Care, Unity Health Toronto, St. Michael's Hospital, University of Southampton). Author C.D.J. is the editor-in-chief of the Journal of Manipulative and Physiological Therapeutics and a board member of the NCMIC, however, she received no directive or remuneration for this paper. Author B.N.G. is the associate editor of the Journal of Manipulative and Physiological Therapeutics and received no funding for participation in this project. Author K.K.K. is a member of the NCMIC Speakers Bureau and on the ACA Board of Governors. Author E.G.H. is a member of the NCMIC Speakers Bureau and Adjunct Faculty at the University of Western States. Author J.W.B. declares that he is the President of the NYSCA and that the statements in the paper do not necessarily reflect the position of the NYSCA. Author V.S.G. declares that he is the president of the European Chiropractors’ Union. Each author has disclosed their affiliations and no other conflicts of interest were reported.
Contributorship Information
Concept development (provided idea for the research): C.D.J.
Design (planned the methods to generate the results): C.D.J.
Supervision (oversight, organization and implementation, writing of the manuscript): C.D.J.
Data collection/processing (experiments, organization, or reporting data): C.D.J.
Analysis/interpretation (statistical analysis, evaluation, and presentation of the results): C.D.J.
Literature search (performed the literature search): C.D.J., B.N.G.
Writing (responsible for writing a substantive part of the manuscript): C.D.J., B.N.G., K.K.K., E.G.H., J.G.N., W.K.F., J.W.B., D.K.G., K.J.S., C.L., S.T.C., J.R.F., M.B.B., K.L.D., G.T., T.B.K.Y., V.S.G., G.Q., M.H.A.
Critical review (revised manuscript for intellectual content, not spelling, grammar): C.D.J., B.N.G., K.K.K., E.G.H., J.G.N., W.K.F., J.W.B., D.K.G., K.J.S., C.L., S.T.C., J.R.F., M.B.B., K.L.D., G.T., T.B.K.Y., V.S.G., G.Q., M.H.A.
Practical Applications.
-
•
Chiropractic practitioners in this sample demonstrated patient-centered behaviors to serve their patients, including front-line healthcare personnel
-
•
They modified their practices to comply with unique timelines, government regulations, and regional restrictions.
-
•
They reported increasing sanitation measures and modified patient interactions to reduce spread of the contagion.
-
•
They monitored the COVID-19 situation and responded accordingly as new regulations and information became available.
-
•
They modified practice and patient encounters to include telehealth.
Alt-text: Unlabelled box
References
- 1.Chen N, Zhou M, Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuchat A. Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69 doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahase E. Coronavirus covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. doi: 10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Coronavirus disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Published 2020. Accessed April 14, 2020.
- 5.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html. Published 2020. Accessed May 4, 2020.
- 7.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report – 91.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200420-sitrep-91-covid-19.pdf?sfvrsn=fcf0670b_4. Published April 20, 2020. Accessed May 4, 2020.
- 8.World Health Organization. Strategic preparedness and response plan. https://www.who.int/publications-detail/strategic-preparedness-and-response-plan-for-the-new-coronavirus. Published April 14, 2020. Accessed April 20, 2020.
- 9.Johns Hopkins University. Mortality Analysis. https://coronavirus.jhu.edu/data/mortality. Published May 5, 2020. Accessed May 5, 2020.
- 10.World Health Organization. COVID-19 strategy update - 14 April 2020. https://www.who.int/publications-detail/covid-19-strategy-update—14-april-2020. Published April 14, 2020. Accessed April 20, 2020.
- 11.World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Published March 19, 2020. Accessed May 4, 2020.
- 12.United Nations Foundation. We're all navigating new realities brought on by the COVID-19 pandemic. https://unfoundation.org/blog/post/coming-together-for-the-covid-19-solidarity-response-fund/. Published March 20, 2020. Accessed May 4, 2020.
- 13.World Health Organization. Shortage of personal protective equipment endangering health workers worldwide. https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide. Published March 3, 2020. Accessed May 4, 2020.
- 14.Stochkendahl MJ, Rezai M, Torres P. The chiropractic workforce: a global review. Chiropr Man Therap. 2019;27:36. doi: 10.1186/s12998-019-0255-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang M. The chiropractic scope of practice in the United States: a cross-sectional survey. J Manipulative Physiol Ther. 2014;37(6):363–376. doi: 10.1016/j.jmpt.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization . World Health Organization; Geneva: 2005. WHO Guidelines on Basic Training and Safety in Chiropractic. [Google Scholar]
- 17.Himelfarb I, Hyland JK, Ouzts NE. National Board of Chiropractic Examiners; Greeley: 2020. Practice Analysis of Chiropractic 2020.https://www.nbce.org/practice-analysis-of-chiropractic-2020/ [Google Scholar]
- 18.Green BN, Johnson CD, Brown R. An international stakeholder survey of the role of chiropractic qualifying examinations: A qualitative analysis. J Chiropr Educ. 2020;34(1):15–30. doi: 10.7899/JCE-19-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Houweling TA, Braga AV, Hausheer T, Vogelsang M, Peterson C, Humphreys BK. First-contact care with a medical vs chiropractic provider after consultation with a swiss telemedicine provider: comparison of outcomes, patient satisfaction, and health care costs in spinal, hip, and shoulder pain patients. J Manipulative Physiol Ther. 2015;38(7):477–483. doi: 10.1016/j.jmpt.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Weeks WB, Goertz CM, Meeker WC, Marchiori DM. Characteristics of US adults who have positive and negative perceptions of doctors of chiropractic and chiropractic care. J Manipulative Physiol Ther. 2016;39(3):150–157. doi: 10.1016/j.jmpt.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Johnson C, Baird R, Dougherty PE. Chiropractic and public health: current state and future vision. J Manipulative Physiol Ther. 2008;31(6):397–410. doi: 10.1016/j.jmpt.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Johnson C, Rubinstein SM, Cote P. Chiropractic care and public health: answering difficult questions about safety, care through the lifespan, and community action. J Manipulative Physiol Ther. 2012;35(7):493–513. doi: 10.1016/j.jmpt.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Johnson CD LC, Sterling TA, Gojkovich S, Boghosian K, Ciolfi MA. Response of chiropractic organizations to the COVID-19 pandemic: A descriptive report. J Manipulative Physiol Ther. 2020 doi: 10.1016/j.jmpt.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green BN, Johnson CD. Establishing a theoretical basis for research in musculoskeletal epidemiology: a proposal for the use of biopsychosocial theory in investigations of back pain and smoking. J Chiropr Humanit. 2013;20(1):1–8. doi: 10.1016/j.echu.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Green BN, Johnson CD, Haldeman S. A scoping review of biopsychosocial risk factors and co-morbidities for common spinal disorders. PLoS One. 2018;13(6) doi: 10.1371/journal.pone.0197987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson CD, Haldeman S, Chou R. The Global Spine Care Initiative: model of care and implementation. Eur Spine J. 2018;27(Suppl 6):925–945. doi: 10.1007/s00586-018-5720-z. [DOI] [PubMed] [Google Scholar]
- 27.Hurwitz EL, Randhawa K, Yu H, Cote P, Haldeman S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. 2018;27(Suppl 6):796–801. doi: 10.1007/s00586-017-5432-9. [DOI] [PubMed] [Google Scholar]
- 28.Foster NE, Anema JR, Cherkin D. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 29.Buchbinder R, van Tulder M, Öberg B. Low back pain: a call for action. The Lancet. 2018;391(10137):2384–2388. doi: 10.1016/S0140-6736(18)30488-4. [DOI] [PubMed] [Google Scholar]
- 30.Gaumer G. Factors associated with patient satisfaction with chiropractic care: survey and review of the literature. J Manipulative Physiol Ther. 2006;29(6):455–462. doi: 10.1016/j.jmpt.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 31.Gemmell HA, Hayes BM. Patient satisfaction with chiropractic physicians in an independent physicians' association. J Manipulative Physiol Ther. 2001;24(9):556–559. doi: 10.1067/mmt.2001.118980. [DOI] [PubMed] [Google Scholar]
- 32.Brown BT, Bonello R, Fernandez-Caamano R, Eaton S, Graham PL, Green H. Consumer characteristics and perceptions of chiropractic and chiropractic services in Australia: results from a cross-sectional survey. J Manipulative Physiol Ther. 2014;37(4):219–229. doi: 10.1016/j.jmpt.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Hawk C, Long CR. Factors associated with patient satisfaction with chiropractic care: survey and review of the literature. J Manipulative Physiol Ther. 2007;30(4):331. doi: 10.1016/j.jmpt.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 34.Weeks WB, Goertz CM, Meeker WC, Marchiori DM. Public perceptions of doctors of chiropractic: results of a national survey and examination of variation according to respondents' likelihood to use chiropractic, experience with chiropractic, and chiropractic supply in local health care markets. J Manipulative Physiol Ther. 2015;38(8):533–544. doi: 10.1016/j.jmpt.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 35.Coulter ID, Hurwitz EL, Adams AH, Genovese BJ, Hays R, Shekelle PG. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine (Phila Pa 1976) 2002;27(3):291–296. doi: 10.1097/00007632-200202010-00018. discussion 297-298. [DOI] [PubMed] [Google Scholar]
- 36.Hurwitz EL, Coulter ID, Adams AH, Genovese BJ, Shekelle PG. Use of chiropractic services from 1985 through 1991 in the United States and Canada. Am J Public Health. 1998;88(5):771–776. doi: 10.2105/ajph.88.5.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beliveau PJH, Wong JJ, Sutton DA. The chiropractic profession: a scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Therap. 2017;25:35. doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clandinin DJ, Connelly FM. Jossey-Bass; San Francisco: 2000. Narrative Inquiry: Experience and Story in Qualitative Research. [Google Scholar]
- 39.Creswell JW. 3rd ed. Sage Publications; Thousand Oaks: 2009. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. [Google Scholar]
- 40.Schwandt TA. Constructivist, interpretivist, approachs to human inquiry. In: Denzin NK, Lincoln YS, editors. The Landscape of Qualitative Research. Sage Publications; Thousand Oaks: 1998. pp. 221–259. [Google Scholar]
- 41.Creswell JW, Hanson WE, Clark Plano VL, Morales A. Qualitative research designs: Selection and implementation. Counsel Psycholo. 2007;35(2):236–264. [Google Scholar]
- 42.Denzin NK, Lincoln YS. Entering the field of qualitative research. In: Denzin NK, Lincoln YS, editors. The Landscape of Qualitative Research: Theories and Issues. Sage Publications; Thousand Oaks: 1998. pp. 1–34. [Google Scholar]
- 43.International Committee of Medical Journal Editors. Defining the Role of Authors and Contributors. http://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html. Published 2020. Accessed May 4, 2020.
- 44.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 45.Orange County Health Care Agency. OC Health Care Agency Confirms First Case of Novel Coronavirus in Orange County, California, January 25, 2020. https://mailchi.mp/ochca/novelcoronavirus. Published 2020. Accessed May 4, 2020.
- 46.Hanna J, Moon S, Stella Chan. 2 Californians died of coronavirus weeks before previously known 1st US death. CNN. April 22, 2020: https://www.cnn.com/2020/2004/2022/us/california-deaths-earliest-in-us/index.html. Accessed May 4, 2020.
- 47.Newsom G, Executive Department State of California . N-33-20. Office of the Governor; Sacramento: 2020. Executive Order.https://covid19.ca.gov/img/Executive-Order-N-33-20.pdf Available from: Accessed May 4, 2020. [Google Scholar]
- 48.California Department of Public Health. State Officials Announce Latest COVID-19 Facts. The Department. Published 2020. https://www.cdph.ca.gov/Programs/OPA/Pages/NR20-028.aspx. Accessed April 12, 2020.
- 49.Director of the California Department of Public Health. Stay home except for essential needs. California Department of Public Health. https://covid19.ca.gov/img/EssentialCriticalInfrastructureWorkers.pdf. Published 2020. Updated April 26. Accessed April 26, 2020.
- 50.Cadiao K. 2 Additional COVID-19 Deaths Reported; Face Coverings Mandatory Starting May 1. County News CEnter. April 24, 2020: https://www.countynewscenter.com/2-additional-covid-19-deaths-reported-face-coverings-mandatory-starting-may-11/?utm_source=rss&utm_medium=rss&utm_campaign=12-additional-covid-19-deaths-reported-face-coverings-mandatory-starting-may-11.
- 51.Centers for Disease Control and Prevention. Infection Control in Healthcare Facilities. https://www.cdc.gov/sars/guidance/i-infection/healthcare.html. Published May 3, 2005. Accessed May 4, 2020.
- 52.The Joint Commission. Infection Prevention and Control. https://www.jointcommission.org/en/resources/patient-safety-topics/infection-prevention-and-control/. Published 2020. Accessed May 4, 2020.
- 53.Centers for Disease Control and Prevention. Coronavirus Disease 2019. https://www.cdc.gov/. Published 2020. Accessed May 4, 2020.
- 54.World Health Organization. Guidance for health workers. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/health-workers. Published 2020. Accessed May 4, 2020.
- 55.Arkansas Democrat Gazette. Tracking Coronavirus. The latest information on covid-19 cases in Arkansas, the U.S. and the world. https://www.nwaonline.com/arvirus/. Published 2020. Accessed May 4, 2020.
- 56.Arkansas Department of Health. Arkansas Department of Health, March 23, 2020. https://www.healthy.arkansas.gov/images/uploads/pdf/ChiropracticCOVID19Guidance3.22.20_revised.pdf. Published 2020. Accessed April 20, 2020.
- 57.Brown J, Sparks D. New restrictions to curb COVID-19 send Oregon communities into uncharted territory. The Register-Guard Web site. https://www.registerguard.com/news/20200312/new-restrictions-to-curb-covid-19-send-oregon-communities-into-uncharted-territory. Published March 12, 2020. Accessed May 4, 2020.
- 58.VanderHart D. Gov. Kate Brown Issues Order Directing Oregonians To 'Stay Home' Published March 23, 2020. https://www.opb.org/news/article/oregon-stay-at-home-order-coronavirus-covid-19-kate-brown/. Accessed May 4, 2020.
- 59.Office of the Governor State of Oregon. Executive order no. 2010. https://www.oregon.gov/gov/Documents/executive_orders/eo_20-10.pdf. Published 2020. Accessed April 20, 2020.
- 60.Missouri Governor. Governor Parson Issues Statewide “Stay Home Missouri” Order to Control, Contain, and Combat Covid-19, April 3, 2020. https://governor.mo.gov/press-releases/archive/governor-parson-issues-statewide-stay-home-missouri-order-control-contain. Published 2020. Accessed May 4, 2020.
- 61.Cybersecurity & Infrastructure Security Agency. Advisory Memorandum on Identification of Essential Critical Infrastructure Workers During COVID-19 Response. https://www.cisa.gov/sites/default/files/publications/CISA_Guidance_on_the_Essential_Critical_Infrastructure_Workforce_Version_2.0_Updated.pdf. Published March 28, 2020. Accessed April 14, 2020.
- 62.Missouri Chiropractic Physicians Association. COVID-19 Update. https://www.mscainfo.com/. Published 2020. Accessed May 4, 2020.
- 63.US Department of Veterans Affairs. Rehabilitation and Prosthetic Services. Chiropractic Service. https://www.rehab.va.gov/chiro/. Published 2020. Accessed April 20, 2020.
- 64.US Department of Veterans Affairs. VA Video Connect. https://www.mobile.va.gov/app/va-video-connect. Published 2020. Accessed May 4, 2020.
- 65.Jenkins C. Declaration of Local Disaster for Public Health Emergency. Filed with Dallas County. https://www.dallascounty.org/Assets/uploads/docs/judge-jenkins/covid-19/031220-FinalDisasterDeclaration.pdf. Published 2020. Accessed April 20, 2020.
- 66.Hellerstedt J. Declaration of Public Health Disaster in the State of Texas. Filed with Texas Secretary of State. https://gov.texas.gov/uploads/files/press/DECLARATION_of_public_health_disaster_Dr_Hellerstedt_03-19-2020.pdf. Accessed April 20, 2020
- 67.Abbott G. Executive Order. Filed with Texas Secretary of State. GA-14. https://gov.texas.gov/uploads/files/press/EO-GA-14_Statewide_Essential_Service_and_Activity_COVID-19_IMAGE_03-31-2020.pdf.Accessed April 20, 2020.
- 68.Association TC. TBCE Interprets Health Orders. https://web.chirotexas.org/news/newsarticledisplay.aspx?ArticleID=270. Published March 23, 2020. Accessed May 4, 2020.
- 69.Texas Board of Chiropractic Examiners. Recommended Guidelines for DCs During COVID-19 Pandemic, April 13, 2020. https://www.tbce.state.tx.us/. Accessed April 20, 2020.
- 70.Texas Chiropractic Association. COVID-19 Updates. https://chirotexas.org/covid-19-updates. Published 2020. Accessed May 3, 2020.
- 71.Hsieh N, Ruther M. Sexual Minority Health and Health Risk Factors: Intersection Effects of Gender, Race, and Sexual Identity. Am J Prev Med. 2016;50(6):746–755. doi: 10.1016/j.amepre.2015.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.New York State. Guidance for Determining Whether a Business Enterprise Is Subject to a Workforce Reduction Under Recent Executive Orders. https://esd.ny.gov/guidance-executive-order-2026. Published 2020. Accessed April 20, 2020.
- 73.New York State Department of Health. Medicaid Update March 23, 2020, Volume 36, Number 5. Comprehensive Guidance Regarding Use of Telehealth including Telephonic Services During the COVID-19 State of Emergency. https://health.ny.gov/health_care/medicaid/program/update/2020/docs/mu_no05_2020-03-21_covid-19_telehealth.pdf. Published 2020. Accessed April 20, 2020.
- 74.New York State. Emergency Adoption of Amendments to 12 NYCRR 325-1.8, 329-1.3, 329-4.2, 333.2, and 348.2 (COVID-19 Telemedicine) Section 325-1.8 of Title 12 NYCRR (amended). http://www.wcb.ny.gov/content/main/wclaws/Covid-19/text.pdf. Published 2020. Accessed April 20, 2020.
- 75.New York Department of Health. Interim Guidance on Executive Order 202.16 Requiring Face Coverings for Public and Private Employees Interacting with the Public During the COVID-19 Outbreak. https://coronavirus.health.ny.gov/system/files/documents/2020/04/doh_covid19_eo20216employeefacecovering_041420.pdf. Published April 14, 2020. Accessed May 4, 2020.
- 76.Ferré-Sadurní L, Cramer M. New York Orders Residents to Wear Masks in Publichttps://www.nytimes.com/2020/04/15/nyregion/coronavirus-face-masks-andrew-cuomo.html. Published April 15, 2020. Accessed May 4, 2020.
- 77.Government of Canada. Coronavirus disease (COVID-19): For health professionals. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals.html?topic=tilelink. Published 2020. Accessed April 20, 2020.
- 78.Government of Ontario. List of Essential Workplaces. https://www.ontario.ca/page/list-essential-workplaces. Published 2020. Accessed April 20, 2020.
- 79.Office of the Premier. Ontario Orders the Mandatory Closure of All Non-Essential Workplaces to Fight Spread of COVID-19. https://news.ontario.ca/opo/en/2020/03/ontario-orders-the-mandatory-closure-of-all-non-essential-workplaces-to-fight-spread-of-covid-19.html. Published March 23, 2020. Accessed May 4, 2020.
- 80.College of Chiropractors of Ontario. President's Message #6 re: COVID-19 – Friday, April 17, 2020. https://www.cco.on.ca/2020/03/16/presidents-message-covid-19-march-16-2020/. Published 2020. Accessed April 20, 2020.
- 81.Canadian Chiropractic A. Canadian Federation of Chiropractic Regulatory B. Clinical Practice Guidelines Development I Chiropractic clinical practice guideline: evidence-based treatment of adult neck pain not due to whiplash. J Can Chiropr Assoc. 2005;49(3):158–209. [PMC free article] [PubMed] [Google Scholar]
- 82.Labine J. Calgary-area woman in her 50s is Alberta's first presumptive case of coronavirus. https://edmontonjournal.com/news/local-news/albertas-chief-medical-officer-of-health-assures-coronavirus-response-plan-is-solid-urges-public-to-plan/. Published March 6, 2020. Accessed May 4, 2020.
- 83.Hinshaw D. Record of Decision - CMOH Order 02-2020. https://www.alberta.ca/assets/documents/covid-cmoh-public-health-emergency-declaration.pdf. Published March 17, 2020. Accessed May 4, 2020.
- 84.Government of Alberta. Restrictions on gatherings. https://www.alberta.ca/restrictions-on-gatherings.aspx. Published March 25, 2020. Accessed.
- 85.Alberta College and Association of Chiropractors. COVID-19 update: member FAQs. https://albertachiro.com/ACAC/Communications/2020/03_March/Notice_to_members__March_23__4_p.m._COVID-19_update.aspx. Published March 23, 2020. Accessed May 4, 2020.
- 86.Alberta Government. CMOH order 07-2020: 2020 COVID-19 response. https://open.alberta.ca/publications/cmoh-order-07-2020-2020-covid-19-response. Published March 27, 2020. Accessed May 4, 2020.
- 87.Australian Government Department of Health. Coronavirus (COVID-19) health alert. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert. Published 2020. Accessed May 4, 2020.
- 88.Australian Government Department of Health. COVID-19 infection control training. https://www.health.gov.au/resources/apps-and-tools/covid-19-infection-control-training. Published 2020. Accessed April 24, 2020.
- 89.Queensland Health. Non-essential business, activity and undertaking Closure Direction (No. 7). https://www.health.qld.gov.au/system-governance/legislation/cho-public-health-directions-under-expanded-public-health-act-powers/non-essential-business-closure-direction. Published 2020. Accessed April 24, 2020.
- 90.Australian Government Department of Health. Guidance on the use of personal protective equipment (PPE) in hospitals during the COVID-19 outbreak. https://www.health.gov.au/sites/default/files/documents/2020/04/guidance-on-the-use-of-personal-protective-equipment-ppe-in-hospitals-during-the-covid-19-outbreak.pdf. Published April 24, 2020. Accessed April 24, 2020.
- 91.Reid D. UK confirms its first coronavirus cases. UK confirms its first coronavirus cases Web site. https://www.cnbc.com/2020/01/31/uk-confirms-two-cases-of-coronavirus.html. Published January 31, 2020. Accessed May 4, 2020.
- 92.UK Statutory Instruments. The Health Protection (Coronavirus) Regulations 2020. http://www.legislation.gov.uk/uksi/2020/129/contents/made. Accessed May 4, 2020.
- 93.BBC News. Coronavirus: Key workers revealed ahead of school shutdown. https://www.bbc.com/news/uk-51972793. Published March 20, 2020. Accessed April 20, 2020.
- 94.Jones A, Sheridan D. Boris Johnson announces closure of all 'non-essential shops' in UK lockdown. https://www.telegraph.co.uk/politics/2020/03/23/boris-johnson-coronavirus-speech-update-lockdown-uk/. Published March 23, 2020. Accessed May 4, 2020.
- 95.British Chiropractic Association. Coronavirus (COVID-19). https://chiropractic-uk.co.uk/coronavirus-covid-19/. Published March 2, 2020. Accessed May 4, 2020.
- 96.McTimoney Chiropractic Association Coronavirus (COVID-19). https://www.mctimoney-chiropractic.org/home.aspx. Published March 27, 2020. Accessed May 4, 2020.
- 97.The Royal College of Chiropractors. Coronavirus (Covid-19): Information and guidance for clinics. https://rcc-uk.org/tag/covid-19/. Published March 24, 2020. Accessed May 4, 2020.
- 98.Ministério da Saúde. Brasil registra 71.886 casos de coronavírus e 5.017 mortes da doença. https://www.saude.gov.br/noticias/agencia-saude/46806-brasil-registra-71-886-casos-de-coronavirus-e-5-017-mortes-da-doenca. Published 2020. Accessed April 28, 2020.
- 99.DeSousa M, Savarese M. Brazil confirms first coronavirus case in Latin America. https://apnews.com/fd3d0d0120dd10f3d09bad78a4dd9539. Published February 26, 2020. Accessed May 4, 2020.
- 100.Marshall E. First Covid-19 death confirmed in Brazil. https://brazilian.report/coronavirus-brazil-live-blog/2020/03/17/first-covid-19-death-confirmed-in-brazil/. Published March 17, 2020. Accessed May 4, 2020.
- 101.MercoPress. Bolsonaro asks Congress to declare state of emergency to free federal funds from spending caps. https://en.mercopress.com/2020/03/18/bolsonaro-asks-congress-to-declare-state-of-emergency-to-free-federal-funds-from-spending-caps. Published March 18, 2020. Accessed May 4, 2020.
- 102.Library of Congress. Brazil: Ministry of Health Authorizes Telemedicine During Coronavirus Pandemic. Global Legal Monitor. https://www.loc.gov/law/foreign-news/article/brazil-ministry-of-health-authorizes-telemedicine-during-coronavirus-pandemic/. Published April 15, 2020. Accessed May 4, 2020.
- 103.Oliveira WK, Duarte E, Franca GVA, Garcia LP. How Brazil can hold back COVID-19. Epidemiol Serv Saude. 2020;29(2) doi: 10.5123/s1679-49742020000200023. [DOI] [PubMed] [Google Scholar]
- 104.Roelf W. South Africa's Ramaphosa Declares State of Disaster Over COVID-19. https://www.usnews.com/news/world/articles/2020-03-15/south-africas-ramaphosa-declares-state-of-disaster-over-covid-19. Published March 15, 2020. Accessed May 4, 2020.
- 105.Brown M. South Africa Begins Nationwide Coronavirus Lockdown. VOA News. https://www.voanews.com/science-health/coronavirus-outbreak/south-africa-begins-nationwide-coronavirus-lockdown. Published March 27, 2020. Accessed May 4, 2020.
- 106.National Institute for Communicable Diseases. COVID-19 Weekly Epidemiology Brief: Week 18, 2020. https://www.nicd.ac.za/wp-content/uploads/2020/05/2020-04-30-COVID-19WklyEpiBriefFinal_Week18.pdf. Published Week 18, 2020. Accessed May 4, 2020.
- 107.Government of the Netherlands. Prime Minister Rutte addresses the country about COVID-19. https://www.government.nl/documents/speeches/2020/03/16/television-address-by-prime-minister-mark-rutte-of-the-netherlands. Published March 16, 2020. Accessed May 4, 2020.
- 108.Government of the Netherlands. Coronavirus COVID-19. https://www.government.nl/topics/coronavirus-covid-19. Published 2020. Accessed May 4, 2020.
- 109.Nederlandse Chiropractoren Associatie. Nederlandse Chiropractoren Associatie. https://www.nca.nl/. Published 2020. Accessed May 4, 2020.
- 110.Misérus M, Dirks B, Kreling T. No King's Day and premier league, hefty fines and strict enforcement. https://www.volkskrant.nl/. Published March 23, 2020. Accessed May 4, 2020.
- 111.Netherlands Chiropractors Association. Update COVID-19 Chiropractic Practices. https://www.nca.nl/nieuws/u. Published 2020. Accessed May 3, 2020.
- 112.Rijksoverheid. Questions about the coronavirus and paramedical care. https://www.rijksoverheid.nl/onderwerpen/coronavirus-covid-19/zorg/paramedische-zorg. Published 2020. Accessed May 3, 2020.
- 113.Channel News Asia. Singapore confirms first case of Wuhan virus. https://www.channelnewsasia.com/news/singapore/wuhan-virus-pneumonia-singapore-confirms-first-case-12312860. Published January 23, 2020. Accessed May 4, 2020.
- 114.Singapore Tourism Board. STB unveils targeted measures to support tourism businesses affected by 2019-nCoV. https://www.stb.gov.sg/content/stb/en/media-centre/media-releases/stb-unveils-targetedmeasurestosupporttourismbusinessesaffectedby.html.html. Published February 2, 2020. Accessed May 4, 2020.
- 115.Kam A. Singapore has banned all social gatherings. https://www.cnn.com/world/live-news/coronavirus-pandemic-04-08-20/h_fc3a7650598cbb15fc6affdc264ac7cf. Published April 8, 2020. Accessed.
- 116.Reuters. Greece confirms first coronavirus case, a woman back from Milan. https://www.reuters.com/article/us-china-health-greece-idUSKCN20K1IA. Published February 3, 2020. Accessed May 4, 2020.
- 117.CNN Greece. Koronoios: All schools and universities in the country are closing. https://www.cnn.gr/news/ellada/story/210695/koronoios-kleinoyn-ola-ta-sxoleia-tis-xoras. Published March 10. 2020. Accessed May 4, 2020.
- 118.iefimerida. Koronoios: 99 cases in Greece - Parades are canceled. https://www.iefimerida.gr/ellada/koronoios-99-kroysmata-stin-ellada-akyronontai-oi-parelaseis-diaggelma-mitsotaki-stis-1900. Published March 12, 2020. Accessed May 4, 2020.
- 119.ekathimerini. Government suspends all services at all places of worship until March 30. https://www.ekathimerini.com/250719/article/ekathimerini/news/government-suspends-all-services-at-all-places-of-worship-until-march-30. Published March 16, 2020. Accessed May 4, 2020.
- 120.Reuters. Greece to inject 10 billion euros to support economy as coronavirus spreads. https://www.reuters.com/article/us-health-coronavirus-greece-pm/greece-to-inject-10-billion-euros-to-support-economy-as-coronavirus-spreads-idUSKBN2163EG. Published March 19, 2020. Accessed May 4, 2020.
- 121.Reuters. Greece bans flights from UK, Turkey as coronavirus cases rise. https://www.reuters.com/article/uk-health-coronavirus-greece-lockdown-idUKKBN21A1H0. Published March 23, 2020. Accessed May 4, 2020.
- 122.Athens News Agency. Greece Tops List of Countries Successfully Flattening Coronavirus Curve in Europe. The National Herald Web site. https://www.thenationalherald.com/298501/greece-tops-list-of-countries-successfully-flattening-coronavirus-curve-in-europe/. Published April 17, 2020. Accessed April 20, 2020.
- 123.Fallon K. How Greece managed to flatten the curve. https://www.independent.co.uk/news/world/europe/coronavirus-greece-cases-deaths-flatten-curve-update-a9455436.html. Published April 8, 2020. Accessed April 20, 2020.
- 124.Ministry of Health and Social Protection. Colombia confirms its first case of COVID-19. https://www.minsalud.gov.co/Paginas/Colombia-confirma-su-primer-caso-de-COVID-19.aspx. Published March 6, 2020. Accessed May 4, 2020.
- 125.Cobb J. Colombia to hold 19-day quarantine to fight coronavirus. https://www.reuters.com/article/us-health-coronavirus-colombia-quarantin/colombia-to-hold-19-day-quarantine-to-fight-coronavirus-idUSKBN218068. Published March 20, 2020. Accessed May 4, 2020.
- 126.Gobierno de Colombia. What will happen after April 27?https://coronaviruscolombia.gov.co/Covid19/acciones/acciones-20-abril.html. Published April 20, 2020. Accessed May 4, 2020.
- 127.Wood G. Iran Has Far More Coronavirus Cases Than It Is Letting On. The Atlantic. https://www.theatlantic.com/ideas/archive/2020/03/irans-coronavirus-problem-lot-worse-it-seems/607663/. Published March 9, 2020. Accessed May 4, 2020.
- 128.McKernan B. Turkey announces its first case of coronavirus. The Guardian. https://www.theguardian.com/world/2020/mar/11/turkey-announces-its-first-case-of-coronavirus. Published March 11, 2020. Accessed May 4, 2020.
- 129.Turkish Republic of Northern Cyprus. The Curfew Has Been Extended Until 30 April 2020. https://mfa.gov.ct.tr/the-curfew-has-been-extended-until-30-april-2020/. Published April 18, 2020. Accessed May 4, 2020.
- 130.US Embassy and Consulates in Turkey. COVID-19 Information. https://tr.usembassy.gov/covid-19-information-2/. Published 2020. Accessed May 4, 2020.
- 131.World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf. Published 2020. Accessed May 4, 2020.