COVID-19 outbreak forced significant changes in the management of non-communicable diseases worldwide including cancer. The first COVID-19 case in Turkey was announced on March 10th, and the pandemic reached its peak in the last days of April 2020. Radiotherapy departments faced a unique challenge to provide a virus-free environment for both patients and staff while operating continuously.
In Turkey, Ministry of Health (MoH) was the primary government institute against the COVID-19 outbreak, which organized all health institutions with daily briefings, circulars, orders, recommendations and declarations. The most critical decision of the MoH was to declare all tertiary hospitals (public and private) in Turkey as “pandemic hospital”, which gave an ultimate authority to MoH to reorganize these hospitals for outbreak preparedness. This reorganization included postponement of elective surgeries, allocation of diagnostic services and inpatient wards for COVID-19 patients, rotation of all hospital staff in the COVID-19 clinics. Although cancer treatments was decided to proceed without interruption, since most hospitals having a radiotherapy facility were declared as pandemic hospital, this had an immediate effect on the functionality of the radiotherapy departments.
Several administrative changes were done in radiotherapy departments to prevent COVID-19 spread; these included the usage of face masks, gowns and gloves for all personnel, disinfection of treatment machines and equipment after every patient, providing social distancing measures, reducing the number of people in the department, and educating patients about COVID-19 disease and cancer. All these resulted in a reduction in the capacity of the services, furthermore manpower considerably reduced due to sick leave of COVID-19 positive staff members and rotations in COVID-19 clinics. Inevitable modifications were required in daily practice to tackle these problems including working in shifts as isolated teams to prevent contamination among staff, utilization of shorter treatment schemes to keep patients’ stay in the hospital as minimum, postponing radiotherapy as much as acceptable and preferring other treatment options over radiotherapy if possible.
Turkish Society for Radiation Oncology (TROD) immediately involved in the events upon the arrival of the virus to Turkey and collaborated with MoH. TROD informed its members with regular announcements, produced guidelines for management of radiotherapy departments and recommendations for site-specific treatment modifications, and prepared a document to inform cancer patients about the do’s and don’ts during the pandemic.
TROD conducted a national survey to evaluate the changes in radiotherapy practice in Turkey. The survey had 14 items questioning the number of radiotherapy personnel assigned in COVID-19 clinics, administrative changes in the departments, modifications to radiotherapy workflow, changes in the patient admissions and the statistics of COVID-19 infected staff and patients. The survey was performed in the last week of April 2020 when the COVID-19 patient numbers started to draw a plateau.
The survey was sent to 136 departments and the results were collected from 126 (92.6%). 107 departments were in a pandemic hospital and a total of 213 radiotherapy staff (139 RO, 34 nurses, 7 RTT, 12 secretaries and 21 others) were assigned to the COVID-19 clinics temporarily and keep working at radiotherapy units as well. TROD considered this policy extremely unsafe due to high risk of viral transmission from these staff to those cancer patients receiving radiotherapy who already have an enhanced risk of mortality from COVID-19 infection, and immediately alarmed the MoH for risks of the decision. On April 14th MoH announced that any personnel working in oncology departments should not be assigned to pandemic units [1]. This critical decision had a significant impact on protection of patients and staff from COVID-19 dissemination and contributed continuation of radiotherapy service without interruption.
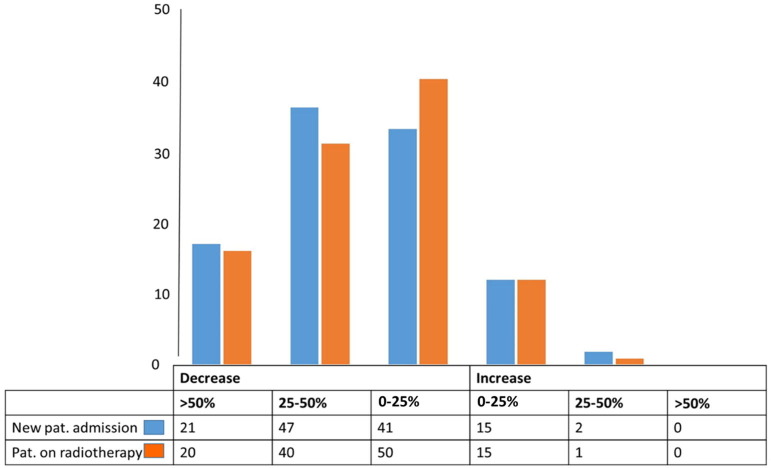
During the first two months of the outbreak a significant reduction – up to 50% - in new patient admissions occurred in 109 departments (Fig. 1 ). Comprehensive cancer centers in larger cities were affected more than the others, only a few stand–alone radiotherapy centers and departments in the smaller towns could kept the patient admissions at pre-pandemic levels. The lockdown and travel restrictions between the provinces prevented access of the patients to comprehensive cancer centers, and many patients decided to start treatment at their hometowns. Arrival of the international patients from neighboring countries stopped completely as well.
Fig. 1.
Change in patient statistics in radiotherapy centers during COVİD-19 pandemics.
Any kind of administrative arrangements were in place in 115 departments; most common were working in isolated radiotherapy teams and switching to shift system, postponement of treatment appointments, and cancellation of face-to-face follow-up clinics. Only one department stopped new patient admissions temporarily. Modifications to standard treatments were done in 117 departments; the most common were utilization of hypofractionated schedules, postponement of adjuvant radiotherapy, preference of surgery and/or chemotherapy over radiotherapy, and avoiding neoadjuvant radiotherapy schedules (Table 1 ). Almost all departments followed TROD recommendations along with other international guidelines (ESTRO, ASTRO) for treatment modifications during the COVID-19 pandemic.
Table 1.
Administrative arrangements and treatment modifications in radiation oncology centers of Turkey during COVID-19 pandemic.
| N | % | |
|---|---|---|
| Administrative arrangements | 115 | 91.2 |
|
96 | 76.2 |
|
76 | 66.1 |
|
59 | 46.8 |
|
7 | 6.1 |
|
2 | 1.7 |
|
2 | 1.7 |
|
1 | 0.8 |
| Treatment modifications | 117 | 92.8 |
|
114 | 97.4 |
|
76 | 64.9 |
|
31 | 26.4 |
|
12 | 10.3 |
Overall 47 radiotherapy staff was diagnosed with COVID-19; 20 were RO, 4 MP, 6 RTT, 7 nurses, and 10 other staff. Twenty of those were employed in a single department, as a consequence department was on the verge of ceasing radiotherapy service for 2 weeks [2]. In other notable events all 4 medical physicists had COVID-19 in a department; 4 nurses and 2 cleaning staff had COVID-19 in another department. These unfortunate examples were strong evidence for the benefit of working in separated teams during the outbreak. Almost all of those colleagues developed mild to moderate symptoms of the disease, none of them required intensive care management.
A total of 54 radiotherapy patients diagnosed with COVID-19 in the first 2 months of the outbreak; 38 of them completed treatment with or without interruption, but radiotherapy was abandoned in 13 and we lost 3 patients due to COVID-19 infection. The calculated death rate of 5.5% among the confirmed cases was within the range of other reports [3], [4].
Radiotherapy services were managed successfully during the first two months of the pandemic in Turkey. Most patients received radiotherapy without major interruptions thanks to significant re-organization and modifications in daily practice with the guidance of MoH directives and TROD recommendations which were announced swiftly and revised frequently on the initial days of the pandemic.
Conflicts of interest
None.
Acknowledgements
The authors would like to thank the all radiation oncology centers of Turkey which participated in the survey and closely collaborated with TROD during COVID-19 pandemic.
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
References
- 1.Sağlık Bakanlığı TC. Kanser hastaları tanı ve tedavi merkezlerinde alınması gereken enfeksiyon kontrol önlemleri. 2020, April 14. https://covid19bilgi.saglik.gov.tr/depo/enfeksiyon-kontorl-onlemleri/COVID19-KanserHastalariTaniVeTedaviMerkezlerindeAlinmasiGerekenEnfeksiyonKontrolOnlemleri.pdf.
- 2.Gemici C, Yaprak G. Covid-19 outbreak in a major radiation oncology department; which lessons should be taken? Radiother Oncol 2020. pii: S0167-8140(20)30178-X. DOI: 10.1016/j.radonc.2020.03.044. [DOI] [PMC free article] [PubMed]
- 3.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson E, Walker AJ, Bhaskaran KJ, et al. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. medRxiv 2020.05.06.20092999; DOI: https://doi.org/10.1101/2020.05.06.20092999.