Abstract
Fear of acquiring severe acute respiratory syndrome coronavirus-2 infection is a major contributor to underutilization of the health care system during the current pandemic. In this report, we describe 4 cases of unexpected deaths that occurred within a short time period in patients with adult congenital heart disease without warning symptoms. (Level of Difficulty: Intermediate.)
Key Words: awareness, cardiac risk, congenital heart defect, shortness of breath
Abbreviations and Acronyms: ACHD, adult congenital heart disease; ED, emergency department; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2
Graphical abstract
Fear of acquiring severe acute respiratory syndrome coronavirus-2 infection is a major contributor to underutilization of the health care system…
As the prevalence of adult congenital heart disease (ACHD) increases, awareness of these patients’ unique risk factors for adverse health outcomes and the need for ongoing care in adulthood is critical (1,2). Caring for this population requires understanding of the dichotomy that underlies their interaction with health care: patients with ACHD often have complex disease that requires frequent contact with their providers, but they simultaneously have frequent gaps in their care. Common etiologies for these times away from care include poor insight into disease severity, financial or health insurance issues, and decreased parental oversight in adulthood (2). By recognizing increased acute-setting mortality rates among patients with ACHD during the mandated stay-at-home period, in this report we seek to demonstrate the effect of the ongoing severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2)–related pandemic on mortality even in uninfected patients with ACHD.
Learning Objectives
-
•
Unexpected mortality among patients with ACHD appears to have acutely increased at a single academic ACHD center during the SARS-CoV-2 pandemic.
-
•
The ongoing SARS-CoV-2 pandemic appears to be contributing to increased ACHD mortality by delaying patient contact with health care.
-
•
Routine follow-up care for high-risk groups, including those with congenital heart disease, during the SARS-CoV-2 pandemic is critical to ensure appropriate triage and care for vulnerable populations. Even with prior clinical stability, these populations remain at risk for acute cardiovascular complications and increased mortality.
Over the 12-month period preceding the SARS-CoV-2-related stay-at-home order, a total of 4 patients followed by the ACHD service at the University of Washington Medical Center with defects of various severities died in an acute setting. In this report we describe a series of 4 acute-setting ACHD deaths that occurred within a single week at the time of the effective stay-at-home order. Acute-onset death was defined as death that occurred either out of the hospital or within 24 h of presentation to a medical facility. With the exception of 1 patient (case 4) who was called but did not answer the phone 2 days prior to being found dead at home, none of the patients had a missed clinic appointment since the initiation of the stay-at-home order, and none had made contact with the medical system to report concerning symptoms prior to their deaths.
Case 1
A 46-year-old woman with a history of aortic coarctation who underwent surgical repair at 28 years of age using an extra-anatomic Dacron graft arrived to the emergency department (ED) because of a witnessed out-of-hospital arrest. The documented rhythm on the defibrillator during resuscitation was a narrow-complex tachycardia. Cardiopulmonary resuscitation was performed by her husband and emergency medical services, with eventual return of spontaneous circulation. Her admission laboratory studies revealed mildly elevated troponin I, N-terminal pro–B-type natriuretic peptide, and white blood count and markedly elevated lactic acid and liver transaminase levels. Renal function was normal, and results of rapid SARS-CoV-2 testing were negative. Noncontrast head computed tomography was unrevealing, and chest computed tomography demonstrated normal post-surgical findings and a patent Dacron graft. Transthoracic echocardiogram showed mild to moderate right ventricular dysfunction. A cooling protocol was initiated, but the patient subsequently developed status epilepticus refractory to therapy. Brain magnetic resonance imaging revealed diffuse anoxic brain injury. The patient’s family elected to transition to comfort-care measures.
Case 2
A 31-year-old man with a history of congenital aortic stenosis presented to the ED with rapidly worsening confusion and lethargy. Surgical history consisted of valvotomy in infancy with known asymptomatic mild residual valve stenosis and regurgitation. Upon arrival, his mentation continued to deteriorate. He ultimately became unresponsive and developed ventricular fibrillation. Resuscitation and intubation were performed, and return of spontaneous circulation was achieved. Head computed tomography demonstrated obstructive hydrocephalus from a 1.9-cm colloid cyst at the anterior aspect of the third ventricle at the level of the interventricular foramina. Bedside transthoracic echocardiography showed new severe global left ventricular dysfunction without significant change in the valvular hemodynamic status. Chest computed tomographic angiography showed evidence of small right sided aspiration, but was otherwise unrevealing. Post-resuscitation, the patient was unresponsive to stimuli. Despite invasive measures to reduce his intracranial pressures in the form of an external ventricular drain, follow-up imaging demonstrated profound cerebral edema and cerebellar herniation. A neurological examination was performed and was consistent with brain death, so supportive measures were withdrawn.
Case 3
A 59-year-old man with a history of tetralogy of Fallot, hypertrophic cardiomyopathy, and atrial fibrillation presented to the ED with chest pain and syncope. His surgical history consisted of patch closure of the ventricular septal defect and right ventricular outflow tract enlargement during childhood, followed by repeat pulmonary valvuloplasty 19 years prior to his presentation. In the ED, the implantable cardioverter-defibrillator was interrogated, and no events in the preceding 2 months were seen. Serial troponin levels were within the normal limits, B-type natriuretic peptide was elevated at 2,400 pg/ml, and creatinine was elevated to more than twice the patient’s baseline. The patient was monitored and was given a diuretic agent for volume overload. He was being prepared for discharge when he experienced asystolic cardiac arrest. Code blue was called, and more than 20 min of resuscitation attempts were performed. Asystole persisted without return of spontaneous circulation, and he was pronounced deceased.
Case 4
A 48-year-old man with a history of congenital aortic stenosis was found deceased at home. His surgical history consisted of childhood aortic valvotomy followed by a Bentall procedure with a 23-mm mechanical valve. Two years prior to his death, he had an episode of ventricular tachycardia and was found to have moderate to severe left ventricular systolic dysfunction. He underwent implantable cardioverter-defibrillator placement, and ventricular function normalized on guideline-directed medical therapy. Three months prior to his death he underwent transcatheter ventricular tachycardia and atrial flutter ablation because of recurrent arrhythmic episodes. On echocardiography performed following the ablation procedure, left ventricular and mechanical aortic valve function was normal. Two days prior to being found, the patient’s cardiologist had called him regarding a missed clinic visit but never received a return call.
Discussion
Several news reports from across the United States and early publications internationally on the SARS-CoV-2 pandemic highlight the decline in ED visits. In Portugal, March 2020 brought 48% fewer ED visits than forecast (3). ED visits in England were down by 49% in the third week of March 2020 compared to the final week of February 2020 (4). Similarly, early reports from 6 institutions in the Seattle area (not including ours) showed that although there had been an increase in ED visits for respiratory illnesses, there was a 10% to 40% decline in overall ED visits (5). Patients with chronic medical illnesses and those at risk for acute cardiac compromise have remained at risk throughout the SARS-CoV-2 pandemic, and this case series highlights this reality.
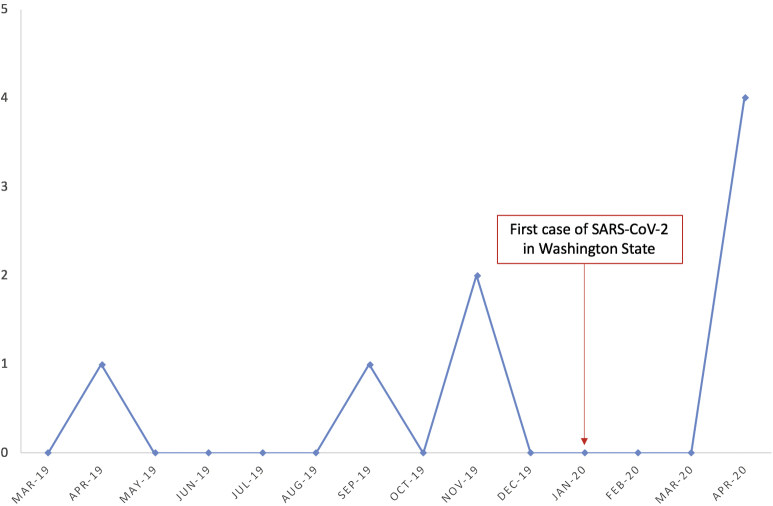
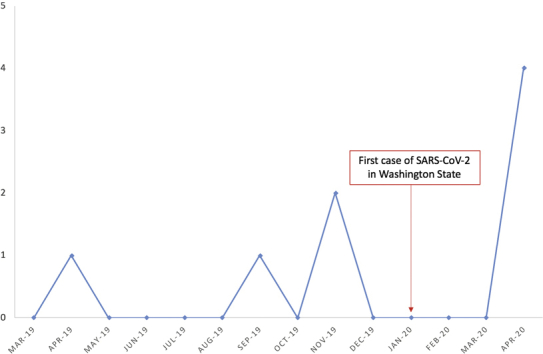
Although ACHD mortality at our institution varies from month to month and year to year, 4 out-of-hospital deaths in a single week is equal to the cumulative number of hospital deaths in our ACHD population over the preceding year (Figure 1). What is even more concerning is that none of these patients had high-risk features that would put them at increased risk compared with other patients with ACHD. No patient had residual cyanotic heart disease, single-ventricle physiology, or concurrent pulmonary hypertension that would put him or her at even higher risk for complications during a respiratory pandemic. These patients had clinically stable conditions and were receiving routine follow-up care at an established ACHD center. None had sought care prior to their presentations or expressed symptoms to medical providers. This case series highlights the need for close follow-up, particularly in high-risk populations, even if their disease burden has remained stable. Although we are unable to definitively say that fear of SARS-CoV-2 led to delayed hospital presentations in these cases, we believe that they do reflect a growing trend of health care avoidance by cardiology patients with non-SARS-CoV-2 emergencies and potentially life-threatening consequences of these delays in care.
Figure 1.
Known Out-of-Hospital Deaths Among Patients With Adult Congenital Heart Disease at the University of Washington Medical Center Between March 1, 2019, and April 25, 2020
Conclusions
The SARS-CoV-2 pandemic and associated shelter-in-place orders, combined with public fear of contracting the virus, have led to an overall reduction in ED visits despite increasing visits for respiratory illnesses. We believe that this change in ED volume, combined with the acute increase in mortality reported in this case series, emphasizes the potential adverse outcomes of delayed presentations among medically complex patients. This includes our ACHD population. These cases highlight the need for public education regarding the imperative to present for medical care when symptoms would have merited emergency treatment prior to the pandemic, particularly among our most vulnerable populations. They also highlight the need for routine follow-up care for patients with congenital heart disease, even in the presence of clinical stability, to assess for subclinical symptom burdens that may herald future acute presentations.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Benziger C.P., Stout K., Zaragoza-Marcias E., Bertozzi-Villa A., Flaxman A.D. Projected growth of the adult congenital heart disease population in the United States to 2050: an integrative systems modeling approach. Popul Health Metr. 2015;13:1–8. doi: 10.1186/s12963-015-0063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gurvitz M., Valente A.M., Broberg C. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (the Health, Education, and Access Research Trial) J Am Coll Cardiol. 2013;61:2180–2184. doi: 10.1016/j.jacc.2013.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santana R., Sousa Joana S., Soares P., Lopes S., Boto P., Rocha João V. The demand for hospital emergency services: trends during the first month of COVID-19 response. Port J Public Health. https://www.karger.com/Article/FullText/507764 Available at:
- 4.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ. 2020;369:m1401. doi: 10.1136/bmj.m1401. [DOI] [PubMed] [Google Scholar]
- 5.Miller G.A., Buck C.R., Kang C.S. COVID-19 in Seattle—early lessons learned. J Am Coll Emerg Phys Open. 2020;1:85–91. doi: 10.1002/emp2.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]