Abstract
Paraviral eruptions, such as the papular-purpuric gloves and socks syndrome or eruptive pseudoangiomatosis, share the following features that distinguish them from a classic viral eruption: they are highly recognizable; the eruption usually lasts a few weeks; many different viruses and sometimes other agents can trigger them; on microscopic examination, there is no specific cytopathogenic viral effect. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can induce both a classic viral eruption and a paraviral eruption, the meaning of which in terms of pathophysiology and prognosis is very different. Some patients infected with coronavirus disease 2019 (COVID-19) have a papulovesicular eruption involving mainly the trunk. Those patients have active viremia, and some have developed pneumonia and died. Biopsy of the eruption revealed cytopathogenic viral effect, and thus there is a direct interaction of the virus with the skin; it is, therefore, a classic viral exanthema. Others, mainly young patients, developed chilblains of the fingers and toes 3 or 4 weeks after minor signs of COVID-19 or after contact with a diseased person. They did not develop severe COVID-19. Biopsy revealed classic findings of chilblains without cytopathogenic viral effect. Most of those patients did not develop specific antibodies. Those chilblains can be considered as paraviral. Classic viral manifestations are the consequence of a direct interaction of the skin with the virus, whereas paraviral manifestations result from the activation of the immune system. In the case of paraviral chilblains, I hypothesize that it is the innate immune system that rejects SARS-CoV-2. Chilblains are also observed in rare monogenic disorders called type 1 interferonopathies, where antiviral innate imunity is abormally activated. This would explain why these individuals do not develop specific antibodies, because they are probably naturally resistant to SARS-CoV-2 infection via their innate immuen system.
Introduction
Seventeen years ago, while updating the fourth edition of the French standard textbook Dermatologie et Infections Sexuellement Transmissibles, I had some difficulties classifying a few entities, such as eruptive pseudoangiomatosis, Gianotti-Crosti syndrome, pityriasis rosea, acute perifluxural exanthema of childhood, and the papular-purpuric gloves and socks syndrome.
Although these eruptions are thought of as being of viral origin, they have been reported to be triggered by many different viruses and not a single virus, and sometimes even by other agents, such as drugs. The papular-purpuric gloves and socks syndrome, for example, was initially described in patients with parvovirus B19 infection, but a similar clinical appearance was then reported with many other viruses: Epstein-Barr virus, cytomegalovirus, hepatitis B, measles, varicella, human herpes virus 6, human immunodeficiency virus, and others. When organizing knowledge in a textbook, or when teaching students, it would thus have been wrong to classify the papular-purpuric gloves and socks syndrome as a manifestation of parvovirus B19. To address this nosologic vacuum, the term “paraviral eruptions” was coined, introduced in the textbook and shared with the medical community.1 , 2
While carefully examining those entities, it became clear that they had many similarities and that they substantially differed from classic viral exanthems. A classic viral exanthem is usually short-lived, lasting only a few days, typically associated with one virus or family of viruses; microscopic evaluation of the eruption shows a cytopathogenic viral effect, demonstrating a direct interaction between the virus and the skin.
Paraviral eruptions on the contrary have the following characteristics. They are highly recognizable by an experienced physician; the physician will name them and will not refer to the causal agent (“this is a Gianotti-Crosti syndrome”). They are thus defined by morphology and not etiology. Many different viruses can trigger the same type of eruption. They usually persist for a few weeks. On microscopic examination, there is no cytopathogenic viral effect.
One basic difference between a classic viral eruption and a paraviral eruption is that the skin lesions result from a direct interaction between the virus and the skin in the former, and they are a consequence of an immune reaction triggered by the virus in the latter.
Since the concept was created, it has gained wide acceptance in the French nosography. Table 1 summarizes the entities that are included in the current edition (sixth edition) of our textbook.2 Of note, many dermatologic entities that are already otherwise classified in nosography, such as vasculitides, urticaria, and erythema nodosum, can also be considered in some instances as paraviral eruptions.
Table 1.
Paraviral eruptions2
| Clinical syndrome | Main associated virus | Other viruses | Nosology |
|---|---|---|---|
| Otherwise undefined nosology | |||
| Papular acrodermatitis (Gianotti-Crosti syndrome) | Hepatitis B | Multiple | Paraviral eruption |
| Papular-purpuric gloves and socks syndrome | Parvovirus B19 | Multiple | Paraviral eruption |
| Pityriasis rosea | HHV7 | HHV6 | Paraviral eruption |
| Acute periflexural exanthema of childhood | Unknown | Parvovirus B19, HHV7 | Paraviral eruption |
| Eruptive pseudoangiomatosis | Unknown | Parvovirus B19, enterovirus, EBV | Paraviral eruption |
| Defined nosology | |||
| Erythema multiforme | Herpes simplex | Not established | Bullous disorder |
| Erythema nodosum | None | Multiple | Septal panniculitis |
| Sweet syndrome | None | Multiple | Neutrophilic dermatosis |
| Acute exanthematic generalized pustulosis | Enterovirus | Parvovirus B19 | Neutrophilic dermatosis |
| Urticaria | None | Multiple | Urticaria |
| Lichen striatus/blaschkitis | Unknown | Not established | Blaschkolinear dermatosis |
| Vasculitis | Hepatitis | Multiple | Vasculitis |
| Pityriasis lichenoides | Unknown | Multiple | Vasculitis (lymphocytic) |
| Drug reaction with eosinophilia and systemic clinical manifestations | HHV6 | EBV, CMV | Drug reaction |
CMV, cytomegalovirus; EBV, Epstein-Barr virus; HHV, human herpes virus.
Skin findings in patients with COVID-19
It is too early to provide an exhaustive classification of all the skin findings observed in patients with COVID-19. Never before in medicine and in our modern societies has a single topic, namely, COVID-19, been so present in the media, the politics, the minds, and the medical journals worldwide. This monothematic rush leads to considerable irrational behavior and precipitation. Even the most prestigious medical journals, such as The New England Journal of Medicine or The Lancet, rushed to publish contributions on COVID-19, only to retract the contributions shortly after their publication.3 , 4 Unfortunately, the mere publication has immediately led to discontinuation of major clinical trials.
I shall only focus on two skin findings that are related to COVID-19 and have a relative high degree of reliability. They have occurred in many patients during the pandemic, and they have been reported by different and independent investigators. For all of the numerous other reported skin findings, only time will let us know if they occurred by simple coincidence, or if they were causally related to COVID-19.
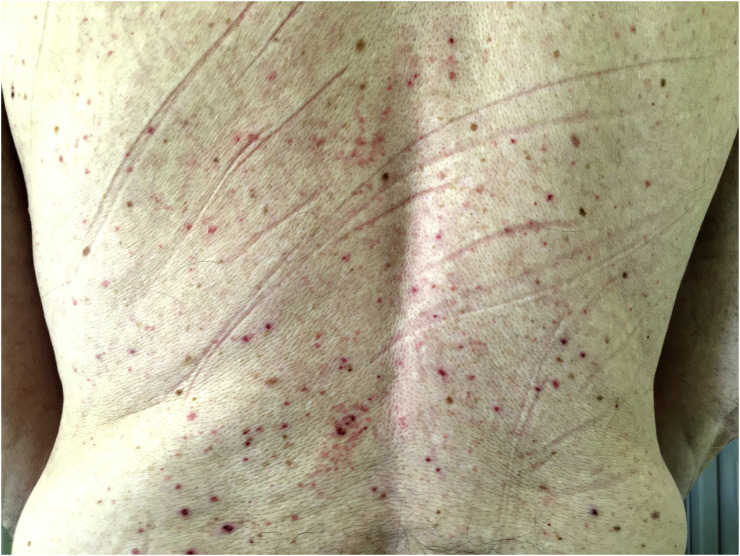
A classic viral eruption has been reported in patients with COVID-19.5 , 6 It is a localized or widespread nonpruritic or mildly pruritic vesicular eruption, involving mainly the trunk. Mucosal involvement has so far not been reported, though mucosal involvement can occur during COVID-19.7 Papules and pustules are often also present, and in some patients the eruption is monomorphic and reminiscent of Grover disease (Figure 1 ). A few patients were biopsied, and histopathologic evaluation revealed cytopathogenic changes typical of a viral eruption, with reticular degeneration of the epidermis, dyskeratotic, sometimes multinucleate keratinocytes, and foci of acantholysis.5 , 6 , 8 This eruption usually started a few days after the first signs of COVID-19, lasted about a week, and resolved without sequelae. In many patients, SARS-CoV-2 could be demonstrated by nasopharyngeal swabs. The severity of COVID-19 was variable. Ten of 24 (42%) Spanish patients with such an eruption developed pneumonia,6 whereas 3 of 22 Italian patients died.5
Fig. 1.
Monomorphic papulovesicular and excoriated mildly pruritic eruption in a 54-year-old man with positive severe acute respiratory syndrome coronavirus 2 nasopharyngeal swab. The eruption appeared 6 days after fever, chills, and myalgia, and the patient also developed dysgeusia.
For the second eruption, an epidemic of acral lesions highly suggestive of chilblains occurred during the COVID-19 pandemic,[9], [10], [11], [12] and this eruption can be considered as a paraviral manifestation of COVID-19. This condition was found mainly in children and young adults who did not have a history of chilblains. It occurred about 3 to 4 weeks either after contact with an infected person in asymptomatic individuals or after minor signs of COVID-19. Infection with COVID-19 could almost never be documented in those patients. None of the patients developed pneumonia. Lesions occurred mainly on the toes (Figure 2 ) and the fingers. Lesions persisted about 10 to 20 days. They manifested as papules, plaques, or swellings, sometimes accompanied by pain and/or itch. When the lesions were biopsied, they displayed the findings of chilblains, but no signs suggestive of a cytopathogenic viral effect.13 The majority of patients who developed chilblains were seronegative[13], [14], [15] (personal observation).
Fig. 2.
Erythematous papules on toes, which appeared 19 days after clinical manifestations of possible coronavirus disease 2019 (fever, headache, myalgia) in a 26-year-old woman. Nasopharyngeal swab and serology were negative.
Why is it important to distinguish between viral and paraviral skin manifestations of COVID-19?
A viral eruption means active disease with viremia, and thus the patient is at risk to develop the other manifestations of COVID-19. Such patients need surveillance, because they can contribute to spreading the disease. They need to be quarantined.
In the case of COVID-19, paraviral chilblains mean that the patient had had contact with the virus and was able to reject it. Those patients are not at risk for pneumonia, and they do not contribute to spreading the disease.
What is the significance of paraviral chilblain lesions in patients with COVID-19?
The facts include the following:
-
1.
Chilblains occurred exclusively in pauci- or asymptomatic patients about 1 to 4 weeks after minor findings of COVID-19 or contact with a patient.
-
2.
The majority of patients were not found to bear the virus by nasopharyngeal swabs.
Many of them did not develop specific anti-SARS-CoV-2 antibodies, which suggests that they might have a natural resistance to the virus, as I have hypothesized elsewhere.16 These findings suggest that their innate immune system rejects the virus and that the adaptive immune system does not need to intervene, explaining the lack of specific antibodies.
Interestingly, children with rare monogenic disorders leading to an enhanced antiviral innate immune response also develop chilblains, supporting this hypothesis. These disorders are called type 1 interferonopathies and include such entities as the different Aicardi-Goutières syndromes or STING (STimulator of INterferon Genes)-associated vasculopathy with onset in infancy.17 It is possible that the otherwise asymptomatic individuals who developed chilblains after COVID-19 do have variants of genes involved in this pathway that confer them a natural resistance to COVID-19.
I leave it up to other investigators to carefully analyze all the other numerous cutaneous manifestations that have been reported in patients with COVID-19 in the last few months. It will be up to them to determine the association with SARS-CoV-2 and the meaning of the findings in terms of viral versus paraviral.
Conclusions
The mechanisms discussed in this short review on the meaning of skin findings during COVID-19 probably apply to the disease process in general. Some signs are the direct consequence of the virus interacting with an organ, whereas others are the consequence of activation of the immune system. This is important because therapy and care of the patients will not be the same whether the target is the virus or the immune system.
Declaration of competing interest
The author declares that he has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Lipsker D., Saurat J.H. A new concept: paraviral eruptions. Dermatology. 2005;211:309–311. doi: 10.1159/000088498. [DOI] [PubMed] [Google Scholar]
- 2.Saurat J.H., Lipsker D. Le concept d’éruption paravirale: clarification terminologique. In: Saurat J.H., Lipsker D., Thomas L., Borradori L., Lachapelle J.M., editors. Dermatologie et Infections Sexuellement Transmissibles. 6th ed. Elsevier/Masson; Paris: 2017. Chapter 2.1 page 86–7. [Google Scholar]
- 3.Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Retraction: cardiovascular disease, drug therapy, and mortality in COVID-19 [published online ahead of print, 2020 May 1] [retracted in: N Engl J Med. 2020 Jun 4]. N Engl J Med 10.1056/NEJMoa2007621. [DOI]
- 4.Mehra MR, Desai SS, Ruschitzka F, Patel AN. Retracted: hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis [published online ahead of print, 2020 May 22] [retracted in: Lancet. 2020 Jun 5]. Lancet 10.1016/S0140-6736(20)31180-6. [DOI] [PMC free article] [PubMed] [Retracted]
- 5.Marzano A.V., Genovese G., Fabbrocini G. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83:280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandez-Nieto D, Ortega-Quijano D, Jimenez-Cauhe J, et al. Clinical and histological characterization of vesicular COVID-19 rashes: a prospective study in a tertiary care hospital [e-pub ahead of print]. Clin Exp Dermatol. doi:10.1111/ced.14277, accessed JUNE 8, 2020 [DOI] [PMC free article] [PubMed]
- 7.Martín Carreras-Presas C, Amaro Sánchez J, López-Sánchez AF, Jané-Salas E, Somacarrera Pérez ML. Oral vesiculobullous lesions associated with SARS-CoV-2 infection [e-pub ahead of print]. Oral Dis. doi:10.1111/odi.13382, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 8.Mahé A, Birckel E, Merklen C, et al. Histology of skin lesions establishes that the vesicular rash associated with COVID-19 is not “varicella-like” [e-pub ahead of print]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16706, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 9.de Masson A, Bouaziz JD, Sulimovic L, et al. Chilblains are a common cutaneous finding during the COVID-19 pandemic: a retrospective nationwide study from France [e-pub ahead of print]. J Am Acad Dermatol. doi:10.1016/j.jaad.2020.04.161, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 10.Colonna C, Monzani NA, Rocchi A, et al. Chilblain-like lesions in children following suspected COVID-19 infection [e-pub ahead of print]. Pediatr Dermatol. doi:10.1111/pde.14210, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 11.Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases [e-pub ahead of print]. Br J Dermatol. doi:10.1111/bjd.19163, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 12.Andina D, Noguera-Morel L, Bascuas-Arribas M, et al. Chilblains in children in the setting of COVID-19 pandemic [e-pub ahead of print]. Pediatr Dermatol. doi:10.1111/pde.14215, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 13.Kanitakis J, Lesort C, Danset M, Jullien D. Chilblain-like acral lesions during the COVID-19 pandemic (“COVID toes”): histologic, immunofluorescence and immunohistochemical study of 17 cases [e-pub ahead of print]. J Am Acad Dermatol. doi:10.1016/j.jaad.2020.05.145, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 14.Mahieu R, Tillard L, Le Guillou-Guillemette H, et al. No antibody response in acral cutaneous manifestations associated with COVID-19? [e-pub ahead of print]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16688, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 15.El Hachem M, Diociaiuti A, Concato C, et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain-like lesions: lights and shadows on the relationship with COVID-19 infection [e-pub ahead of print]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16682, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 16.Lipsker D. A chilblain epidemic during the COVID-19 pandemic: a sign of natural resistance to SARS-CoV-2? [e-pub ahead of print]. Med Hypotheses. doi:10.1016/j.mehy.2020.109959, accessed JUNE 8, 2020. [DOI] [PMC free article] [PubMed]
- 17.Volpi S., Picco P., Caorsi R. Type I interferonopathies in pediatric rheumatology. Pediatr Rheumatol Online J. 2016;14:35. doi: 10.1186/s12969-016-0094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]