Abstract
Beyond their immediate effects on mortality, disasters have widespread, indirect impacts on mental and physical well-being by exposing survivors to stress and potential trauma. Identifying the disaster-related stressors that predict health adversity will help officials prepare for the coronavirus disease 2019 (COVID-19) pandemic. Using data from a prospective study of young, low-income mothers who survived Hurricane Katrina, we find that bereavement, fearing for loved ones’ well-being, and lacking access to medical care and medications predict adverse mental and physical health 1 y postdisaster, and some effects persist 12 y later. Adjusting for preexisting health and socioeconomic conditions attenuates, but does not eliminate, these associations. The findings, while drawn from a demographically unique sample, suggest that, to mitigate the indirect effects of COVID-19, lapses in medical care and medication use must be minimized, and public health resources should be directed to those with preexisting medical conditions, their social networks, and the bereaved.
Keywords: disasters, COVID-19 pandemic, Hurricane Katrina, mental health, physical health
The coronavirus disease 2019 (COVID-19) pandemic is a disaster of unprecedented scale and scope. It is more geographically and temporally diffuse than natural and human-made disasters, and, instead of causing extensive physical destruction, its threat is characterized by persistent potential for illness and trauma. In many ways, however, experiences during the pandemic resemble those common in other disasters: People fear for their well-being and for their loved ones, from whom many are physically isolated; some lack regular access to necessary medications and medical care; and others mourn the unexpected loss of relatives or friends. As of May 5, 2020, the CDC reports over 68,000 deaths from COVID-19 in the United States (1), although this statistic is subject to testing and reporting biases and likely underestimates mortality. In addition to its direct impacts on disease and mortality, disaster research suggests the pandemic will have indirect effects on health due to heightened trauma and stress and disruptions to fulfilling basic needs. The limited research on prior pandemics, for example, shows that extended periods of quarantine lead to declines in psychological well-being that often persist over time (2, 3). This is consistent with a large body of literature documenting adverse effects of natural and human-made disasters on mental health (4, 5) as well as disability, somatic symptoms, and cognitive function (6, 7). Thus, as medical experts combat COVID-19 directly, it is imperative that officials also mitigate the pandemic’s indirect consequences for survivors’ mental and physical health.
Developing an effective public health response requires knowledge of which disaster-related stressors are most harmful to well-being. Given the overlap between the experiences characteristic of the COVID-19 pandemic and those common in other disasters, insights may be gleaned from research on the latter. However, extant studies are of limited utility because they typically rely on summed scores of stressors (8, 9), obscuring the effects of the specific stressors on which policy makers could intervene. They also have yet to assess the extent to which the stressor–health relationship is explained by preexisting health and socioeconomic vulnerabilities (10). Disentangling the consequences of disasters for health by adjusting for preexisting characteristics is needed if resources are to be allocated efficiently to combat the pandemic, while also recognizing and addressing longstanding structural factors that contribute to health disparities.
We identify the specific stressors associated with four measures of health after Hurricane Katrina, one of the worst disasters in U.S. history. We draw on a longitudinal, prospective study of young, low-income mothers who were surveyed 1 y before Katrina as well as 1, 4, and 12 y after. We find that, rather than the physical damage idiosyncratic to natural and human-made disasters, the reported experiences most consequential for health are those that transcend disaster types, namely, bereavement, fearing for the safety of family and friends, and lacking access to medical care and medications. Preexisting health and socioeconomic conditions attenuate effects, particularly those of medical stressors, but independent associations remain. If, as expected, COVID-19 weakens health through these mechanisms, the associated public health burden could be unparalleled in recent American history. Steps must be taken now to eliminate or mitigate the effects of highly impactful stressors.
Results
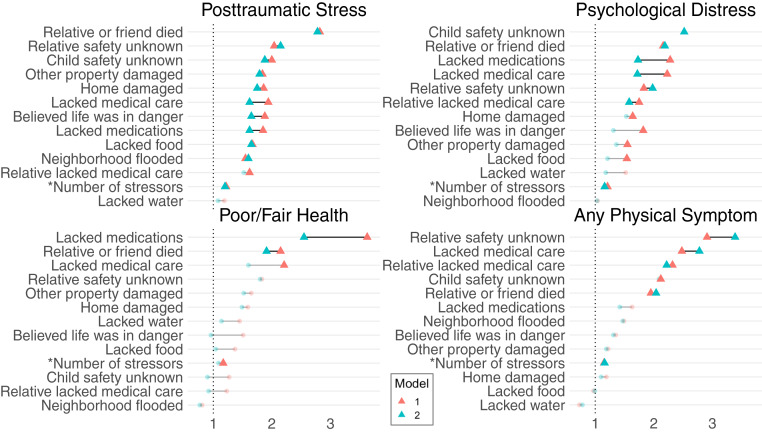
Which stressors are associated with health shortly after a disaster, and which associations are independent of preexisting health and socioeconomic vulnerabilities? Fig. 1 plots odds ratios (ORs) from logistic regression models predicting adverse health 1 y after Hurricane Katrina; separate models estimate associations between health and each of 12 stressors encountered during the hurricane and their count.
Fig. 1.
Associations between disaster-related stressors and odds of adverse health 1 y after Hurricane Katrina. ORs from logistic regression models unconditional (model 1, red) and conditional (model 2, blue) on preexisting health and socioeconomic vulnerability. Statistically significant effects (p 0.05) are denoted with bold triangles.
Strikingly, the stressors prevalent in the current pandemic are predictive of adverse health in the short-term aftermath of Hurricane Katrina. Their effects are more robust across health outcomes and models than those of home damage, property damage, and neighborhood flooding. In particular, those who were bereaved have significantly higher odds of experiencing adversity in all four health domains, and those who lacked knowledge of a loved one’s safety have higher odds of posttraumatic stress (PTS), psychological distress (PD), and physical symptoms. These results remain when controlling for preexisting risk, which was measured prospectively and is therefore not subject to retrospective reporting bias. Lacking medical care and medications following Hurricane Katrina is also associated with greater odds of mental and physical health adversity 1 y later. Although the attenuation observed when adjusting for preexisting vulnerability is greatest for medical stressors, one or both effects remain statistically significant in model 2 for all four outcomes, suggesting that lacking access to medical care and medications during a disaster has independent impacts on subsequent health.
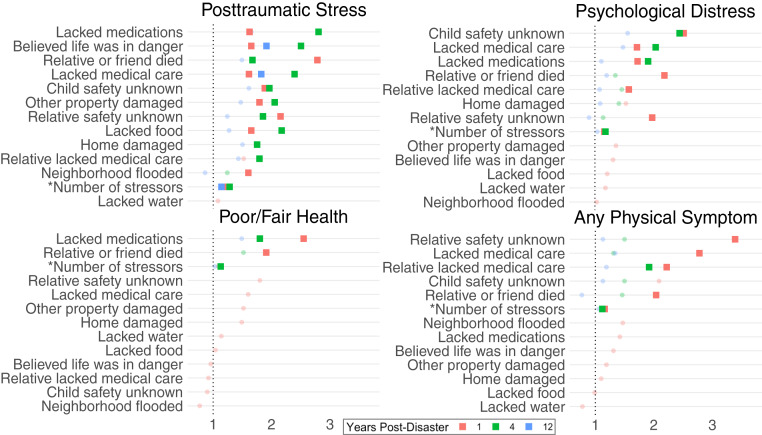
Do the effects of stressors on health persist over time? Fig. 2 presents ORs from fully adjusted logistic regression models predicting adverse health 1, 4, and 12 y after Hurricane Katrina. Whereas many of the stressors that are significantly associated with health 1 y post-Katrina no longer are significant at later follow-ups, several associations persist, and some are notably larger in magnitude. Bereavement, lacking knowledge of children’s and relative’s safety, and having a relative who lacked medical care continue to predict PTS, PD, and/or physical symptoms 4 y postdisaster, and believing one’s life was in danger is associated with significantly higher odds of PTS 12 y later (OR = 1.91, 95% CI = 1.09, 3.37). Lacking medications is associated with higher odds of PTS (OR = 2.80, CI = 1.75, 4.48), PD (OR = 1.91, CI = 1.18, 3.11), and poor or fair self-reported health (OR = 1.80, CI = 1.09, 2.98) 4 y postdisaster. Further, those who lacked medical care have over double the odds of PTS (OR = 2.39, CI = 1.48, 3.87) and PD (OR = 2.04, CI = 1.24, 3.34) 4 y postdisaster and higher odds of PTS 12 y later (OR = 1.82, CI = 1.02, 3.24).
Fig. 2.
Associations between disaster-related stressors and odds of adverse health 1 y (red), 4 y (green), and 12 y (blue) after Hurricane Katrina. ORs from logistic regression models conditional on preexisting health and socioeconomic vulnerability. Statistically significant effects (p .05) are denoted with bold squares. Stressors’ associations with health 4 and 12 y post-Katrina are presented only when the effect at 1 y post-Katrina is marginally significant (p 0.1).
In-depth interviews conducted 4 y after Hurricane Katrina illustrate how fear can induce health problems. A 30-y-old respondent recalled, “it was terrifying for me because I didn’t know if my sister made it [to the Superdome] safely ... so every morning I would get up and I’d have this like morning sickness like I was expecting or something but I wasn’t. It made my stomach very, very nervous.” Another interviewee recounted her experience: “I started having panic attacks ... I don’t know if it was being claustrophobic being stuck in that room, stuck in the house, not doing anything and letting the fear of death overwhelm me ... and I just remember holding on real tight to my mama saying, I hope she don’t die.”
Discussion
Understanding which specific stressors predict postdisaster mental and physical health may shed light on public health needs during the COVID-19 pandemic and potentially for many years afterward. We show that the most robust predictors of health 1, 4, and 12 y after Hurricane Katrina were not measures of home and property damage but rather the loss of loved ones, fear for one’s safety and for relatives and friends, and uncertain access to medical care and medications. Note that we used a particularly vulnerable sample of young, low-income mothers in New Orleans, so our results may not generalize on a national scale. Additionally, the particular disaster-related stressors we evaluated are just a subset of those that have emerged in the COVID-19 pandemic. In particular, job loss and financial stress due to the pandemic are likely to have disastrous effects on public health.
Our results are consistent with the broader disaster literature (4, 5), which suggests that the COVID-19 pandemic will have indirect consequences for human health, in addition to its direct effects on death and disease. This burden may be unprecedented in scale because, unlike other disasters, the pandemic is not geographically bounded, and millions of people will be impacted. In fact, recent work estimates that between 2.38 and 9.12 million Americans will experience at least one grandparental death due to COVID-19 (11). Officials need to prioritize minimizing lapses in medical care and medication access, which could be achieved by encouraging virtual counseling, telemedicine, and medication delivery. Public health messaging should attempt to assuage anxiety and provide tips for overcoming fear. Finally, policy makers should act swiftly to help researchers identify and then provide supplemental health services to those who are bereaved by or experiencing major fear and anxiety due to the pandemic.
Materials and Methods
Data and Sample.
Data are from the Resilience in Survivors of Katrina project. A study that began before the hurricane sampled 1,019 students from two community colleges in New Orleans. All were parents (92.4% mothers) ages 18 y to 34 y who earned less than 200% of the poverty line (12). Surveys occurred about 1 y before Hurricane Katrina and 1, 4, and 12 y after. Approximately 70% of the original sample was interviewed at each follow-up (with 94.0% participating at least once), and 49.7% of mothers responded to all three post-Katrina surveys (n = 468). Analyses of PTS, PD, and self-reported health include the n = 437 mothers with nonmissing information across outcomes at all post-Katrina surveys. Analyses of physical symptoms are conducted on the subset for which the timing of symptom onset could be ascertained (n = 304). At baseline, respondents were, on average, 25.2 y old (SD = 4.5), earned $954 per month (SD = $525), and had 1.0 child under age 5 y (SD = 0.8); 84.2% were non-Hispanic black, and 24.4% were married or cohabiting. The study was approved by Harvard Internal Review Board #13067, and informed consent was obtained at all survey waves.
Measures.
PTS uses the 22-item Impact of Event Scale–Revised, dichotomized using the threshold for PTS disorder (13, 14). PD uses the nonspecific Kessler-6 scale, dichotomized at the established threshold for probable mental illness (15). Self-reported health is dichotomized to poor or fair, or “1”, and good, very good, or excellent, or “0”. Physical symptoms include frequent migraines/headaches, back problems, or digestive problems. With the exception of neighborhood flooding, disaster-related stressors were self-reported 1 y or 4 y post-Katrina; on average, respondents experienced 4.4 of the 12 stressors (SD = 2.9).
Analysis.
Logistic regressions estimate the associations between disaster-related stressors and health. For health 1 y post-Katrina, model 1 adjusts for age and ethnoracial identification (non-Hispanic black versus any other race/ethnicity), and model 2 adds controls for predisaster health (self-rated health, PD, physical symptoms, and any of the following diagnoses: asthma, high cholesterol, high blood pressure, heart condition, depression, or anemia), and for predisaster monthly income (logged), number of children by age, marital/cohabitation status, and social support measured by the Social Provisions Scale (16). We predict health 4 and 12 y after Hurricane Katrina using model 2. Multiple imputation accounts for missing data on independent variables. For data and full table results, see https://osf.io/pt8a9/ (17).
Acknowledgments
We are grateful to Mariana Arcaya, Jean Rhodes, Mary Waters, and Tyler Woods for helpful comments. Support is from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Grants P01HD082032, R01HD057599, and R01HD046162; NSF Grant BCS-0555240; MacArthur Grant 04-80775-000-HCD; Robert Wood Johnson Grant 23029; the Princeton Center for Economic Policy Studies; the Harvard Center for Population and Development Studies; the Brown Population Studies and Training Center (Grant P2CHD041020); and a Malcolm H. Wiener PhD Scholarship.
Footnotes
The authors declare no competing interests.
Data deposition: Replication data, code, and supplementary materials are available on the Open Science Framework at https://osf.io/pt8a9/.
References
- 1. Center for Disease Control, Cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed 5 May 2020.
- 2.Brooks S. K., et al. , The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 395, 912–920 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonanno G. A., Galea S., Bucciarelli A., Vlahov D., What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J. Consult. Clin. Psychol. 75, 671–682 (2007). [DOI] [PubMed] [Google Scholar]
- 4.Goldmann E., Galea S., Mental health consequences of disasters. Annu. Rev. Publ. Health 35, 169–183 (2014). [DOI] [PubMed] [Google Scholar]
- 5.Norris F. H., et al. , 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatr. Interpers. Biol. Process. 65, 207–239 (2002). [DOI] [PubMed] [Google Scholar]
- 6.Isaranuwatchai W., Coyte P. C., McKenzie K., Noh S., Impact of the 2004 tsunami on self-reported physical health in Thailand for the subsequent 2 years. Am. J. Publ. Health 103, 2063–2070 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hikichi H., et al. , Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc. Natl. Acad. Sci. U.S.A. 113, E6911–E6918 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raker E. J., et al. , Twelve years later: The long-term mental health consequences of Hurricane Katrina. Soc. Sci. Med. 242, 112610 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson-Genderson M., Heid A. R., Pruchno R., Long-term effects of disaster on depressive symptoms: Type of exposure matters. Soc. Sci. Med. 217, 84–91 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lowe S. R., Rhodes J. E., Trajectories of psychological distress among low-income, female survivors of Hurricane Katrina. Am. J. Orthopsychiatry 83, 398–412 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verdery A. M., Smith-Greenway E., COVID-19 and family bereavement in the United States. Appl. Demogr 32, 1–2 (2020). [Google Scholar]
- 12.Waters M. C., Life after Hurricane Katrina: The resilience in survivors of Katrina (RISK) project. Socio. Forum 31, 750–769 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiss D., Marmar C., “The Impact of Event Scale–Revised” in Assessing Psychological Trauma and PTSD, Wilson J. P., Keane T. M., Eds. (Guilford, 1997), pp. 399–411. [Google Scholar]
- 14.Creamer M., Bell R., Failla S., Psychometric properties of the Impact of Event Scale–Revised. Behav. Res. Ther. 41, 1489–1496 (2003). [DOI] [PubMed] [Google Scholar]
- 15.Kessler R. C., et al. , Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 32, 959–976 (2002). [DOI] [PubMed] [Google Scholar]
- 16.Cutrona C., Russell D., “The provisions of social relationships and adaptation to stress” in Advances in Personal Relationships, Jones W. H., Perlman D., Eds. (JAI Press, 1987), vol. 1, pp. 37–67. [Google Scholar]
- 17.Raker E. J., Zacher M., Lowe S. R., Lessons from Hurricane Katrina for predicting the indirect health consequences of the COVID-19 pandemic. Open Science Framework. https://osf.io/pt8a9/. Deposited 29 April 2020. [DOI] [PMC free article] [PubMed]