Abstract
Cardiac rehabilitation programs across Canada have suspended in-person services as a result of large-scale physical distancing recommendations designed to flatten the COVID-19 pandemic curve. Virtual cardiac rehabilitation (VCR) offers an alternate mechanism of care delivery, capable of providing similar patient outcomes and safety profiles compared with centre-based programs. To minimize care gaps, all centres should consider developing and implementing a VCR program. The process of this rapid implementation, however, can be daunting. Centres should initially focus on the collation, utilization, and repurposing of existing resources, equipment, and technology. Once established, programs should then focus on ensuring that quality indicators are met and care processes are protocolized. This should be followed by the development of sustainable VCR solutions to account for care gaps that existed before COVID-19, and to improve cardiac rehabilitation delivery, moving forward. This article reviews the potential challenges and obstacles of this process and aims to provide pragmatic guidance to aid clinicians and administrators during this challenging time.
Résumé
En raison des recommandations concernant l’éloignement physique à grande échelle visant à aplatir la courbe pandémique de la COVID-19, tous les services offerts en personne dans le cadre de programmes de réadaptation cardiaque au Canada ont été suspendus. La réadaptation cardiaque virtuelle (RCV) constitue une solution de rechange pour la prestation des soins, dont les résultats pour les patients et les profils d’innocuité se comparent à ceux des programmes offerts en établissement. Afin de réduire le plus possible l’interruption ou le report des soins, tous les établissements devraient envisager de mettre au point et d’instaurer un programme de RCV. La mise en œuvre rapide d’un tel programme peut toutefois être intimidante. Il faut d’abord se concentrer sur la compilation, l’utilisation et le recyclage des ressources, des technologies et de l’équipement existants. Une fois les programmes en place, il faut veiller à ce que les critères de qualité soient satisfaits et à établir des protocoles pour la prestation des soins. Vient ensuite la mise au point de solutions de RCV durables comblant les lacunes qui existaient avant la COVID-19 et améliorant la prestation des soins de réadaptation cardiaque. Les auteurs passent en revue les défis et les obstacles potentiels d’une telle entreprise et tentent de formuler des conseils pragmatiques pour aider les cliniciens et les administrateurs en ces temps difficiles.
Cardiac rehabilitation (CR) programs across Canada have suspended in-person, centre-based cardiac rehabilitation (CBCR) services as a result of large-scale physical distancing recommendations designed to flatten the COVID-19 pandemic curve. CBCR has unequivocally demonstrated reductions in hospital readmissions, secondary events, and mortality in patients with cardiovascular disease.1 Significant consequences of CBCR suspension may include short- and longer-term adverse events including increased rates of cardiac-related ED visits and hospital admissions and exposure of this vulnerable cardiac population to infection. This all places additional burdens on an already strained health care system. Prolonged closure of—or reduced access to—CBCR is likely to result in a significant waitlist expansion for this service, perpetuating delay of in-person care delivery. In an effort to mitigate concerns related to the closure of CBCR programs during the pandemic, virtual CR (VCR) offers an alternate mechanism to CBCR, capable of delivering similar patient outcomes and safety profiles for low- to moderate-risk cardiac patients.1 , 2
VCR is home-based cardiac rehabilitation (HBCR) delivered by virtual mechanisms. Virtual care refers to any remotely occurring interaction between patients and their care providers that uses information and communication technologies to facilitate or maximize the quality and effectiveness of care. This includes telephone and videoconferencing communication, e-mail, mail, text or other messaging solutions, smartphone applications, online platforms, and wearable devices.
The process of rapidly implementing a VCR, however, can be daunting, particularly for centres without previously established virtual care programs. Conversely, for centres in which some home-based/virtual programs are already available, the conversion of all CR participation to VCR brings new challenges, largely around greater resource requirements, the risk-stratification process, and exercise delivery. A review of the challenges, limitations, and pragmatic guidance on the rapid transition to VCR is outlined in this article.
Current Status of Cardiac Rehabilitation During COVID-19
Before the COVID-19 pandemic, CR remained a significantly underused resource with up to 75% to 80% of eligible patients not participating.1 , 3 Although the the majority of Canadian CR care appears to have been delivered as CBCR, up to ∼80% of programs offered an alternative to CBCR delivery as well.3 This included home-based, community-based, or a hybrid model of initially supervised encounters transitioning to unsupervised settings. Smartphones, “apps,” or text messaging have been employed to some degree in approximately ∼30% of programs. The degree to which more extensive VCR programs exist in Canada has not been elicited.
Patient participation in VCR is determined by eligibility criteria based on risk stratification for cardiac events and patient factors such as access to required technology and self-motivation. The majority of VCR programs limit participation to low- to moderate-risk patients, with higher-risk patients enrolled in CBCR. Graded exercise testing (GXT) is used to inform the risk-stratification process.
During the COVID-19 pandemic, up to 50% of all Canadian CR programs have ceased providing any care (unpublished data, personal communication, Dr Paul Oh). Those that continued to provide care were adapted by labour-intensive telephone interviews in response to a lack of in-person intake assessments, a potential inability to perform routine GXT risk-stratification, and a lack of in-person exercise monitoring for those deemed to be at high risk of cardiac events. These programs have also innovated using a virtual model to deliver all other CR care components.
Care-Delivery Challenges and Obstacles
There are several specific areas of concern surrounding the transition to—and the delivery of—VCR. These include challenges faced owing to resource limitations, loss of in-person interactions, difficulties with risk stratification and supervision, and a lack of specific VCR delivery standards (Supplemental Table S1). The notion of VCR safety requires greater scrutiny, particularly in older and frail cardiovascular patients with comorbid illnesses.
During the initial implementation phases of VCR, centres face possible CR staff redeployment because of COVID-19–related issues; a potential lack of centre and patient experience with virtual care delivery; and uncertain access to affordable, effective technologies. Limited access to technology or a lack of technology literacy has the potential to exacerbate care-delivery gaps in vulnerable populations including the elderly, those of lower socioeconomic status, and those living in rural settings.
Furthermore, a lack of evidence exists for entirely virtual programs (ie, without any access to in-person intake assessments, the absence of risk stratification by GXT, and the inclusion of high-risk patients). This makes the identification and enrollment of high-risk patients particularly challenging, as intake GXT followed by clinical and electrographic monitoring to provide safe and effective exercise therapy are mainstays of CR delivery for this population. Without an intake GXT, exercise prescription must rely on estimates and subjective measures, although the use of wearables may provide reasonable estimates on target heart rate guidance for exercise.
Implementing Virtual Cardiac Rehabilitation
The protection of CR staff and patients from undue risk of nosocomial infection and the potential limited availability and use of personal protective equipment resources should remain primary considerations during all stages of the implementation process of VCR. Implementation should focus initially on the collation, use, and repurposing of existing resources, equipment, and technology over complex restructuring. This will allow for rapid delivery to mitigate the negative impact of a lack of CR in at-risk cardiovascular populations.
Program goals
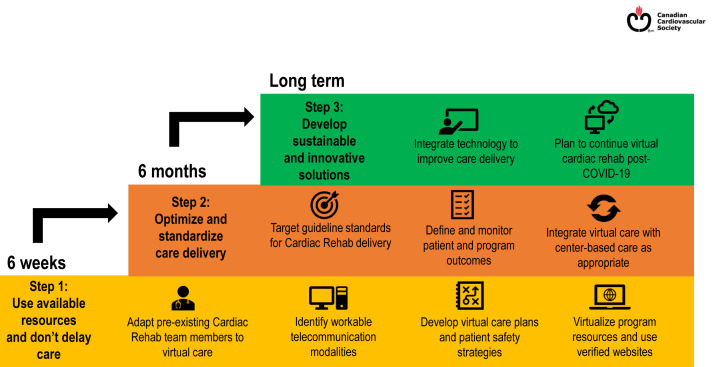
Centres should initially prioritize basic, safe, and timely care over complex and comprehensive care, particularly for those with no previously established virtual program (Fig. 1 , Step 1). Once a program is established, the focus should shift to ensuring that traditional CR care delivery standards are met, protocolized patient assessment and follow-up are defined, and workflow is optimized (Fig. 1, Step 2). Program evaluation should comprise, at a minimum, referral reason, CR intake and discharge dates, and data elements to assess adherence to Canadian Association of Cardiovascular Prevention and Rehabilitation (CACPR) Quality Indicators.4
Figure 1.
The steps of virtual cardiac rehabilitation delivery.
Once the preliminary establishment and quality assurance mechanisms are in place, centres should seek appropriate resources and supportive technologies to enhance care delivery and should aim to develop robust and sustainable VCR solutions not only to continue to provide high-quality care during the COVID-19 pandemic but also to address care gaps that may have existed before the pandemic (Fig. 1, Step 3).
Eligible patients
All patients eligible for conventional CBCR should be considered for participation in VCR in some capacity and ideally should include a component of exercise training. This includes patients previously excluded from VCR programs before the COVID-19 pandemic. Examples include patients at high risk of events (exercise-induced or otherwise), those with limited access to technology, vulnerable populations, the elderly, those of low socioeconomic status, and those in rural locations. Appropriate measures are required to ensure that the implementation of VCR does not widen gaps in care for these vulnerable populations. Programs with limited resources may require regular phone interactions and educational mailouts if the required technology is not available. Individual programs may also consider purchasing tablets, smart phones, or other electronic options for loan to participants to enhance a one-on one personalized experience. Enlisting family members to assist in effective communication for those who are technologically disadvantaged can be beneficial.
Risk stratification and exercise prescription
The risk of a severe exercise-related cardiovascular event is extremely rare during CR. Current evidence would suggest similar safety profiles exist for VCR compared with CBCR.1 However, the evidence for those deemed at higher risk is more limited and therefore requires a cautious approach.
Risk stratification for CR participation has traditionally relied heavily on symptom-limited GXT to assess for the presence of high-risk features such as abnormal hemodynamic responses, silent or residual ischemia, dysrhythmias, exercise-induced symptoms, and low functional capacity. The presence of these GXT findings, or other clinical parameters such as a reduced left ventricular ejection fraction (< 40%), would have previously precluded patients from at least initial participation in home or VCR programs (Supplemental Resources and References). With the alternative, however, being no CR during the current pandemic, the risk of excluding these high-risk patients compared with the accrued benefits of appropriately prescribed physical activity should be carefully balanced and a shared decision-making process undertaken.
Therefore, given the important role of GXT, it should be performed under safe conditions when at all possible and clinically indicated, including for new patient intakes. When not available, increased emphasis should be placed on clinical assessment and alternate methods of obtaining functional capacity (eg, Duke Activity Status Index and self-administered 6-minute walk test).5 This includes the potential use of smartphone applications and wearable technology (Supplemental Resources and References). Although these methods cannot replace GXT, they may provide a baseline metric of functional capacity and help to guide initial prescription for exercise.
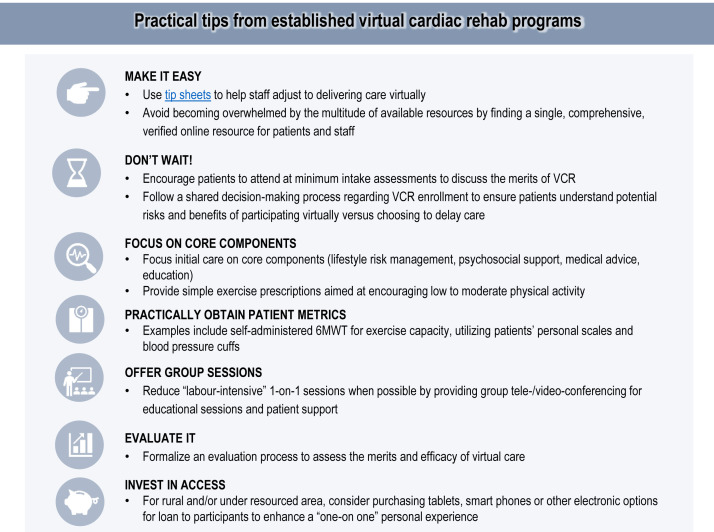
In the absence of standard risk-stratification methods and available in-person monitoring, exercise prescriptions for home-based exercise should be conservative and titrated slowly, particularly for high-risk patients. The target should be the minimal level of physical activity required to obtain the required health benefit, and exercise intensity should not exceed moderate levels of intensity. Patient education on symptom and intensity assessment is therefore paramount. Patient-driven intensity assessment can be achieved by heart-rate palpation, use of available wearable heart-rate monitors, and the talk test (Supplemental Resources and References). Figure 2 outlines further practical tips that may be of value in the establishment process.
Figure 2.
Practical tips for establishing a virtual cardiac rehabilitation program.
Planning for the Ebb and Flow of an Uncertain Future
The COVID-19 pandemic is likely to result in varying degrees of disruption of care for the foreseeable future. Once a VCR program has been established, centres should plan for an ebb and flow of care-delivery restrictions that are likely to follow the COVID-19 pandemic trajectory. Programs should also embrace the development of sustainable VCR solutions to account for care gaps that existed before the COVID-19 pandemic by planning to use the virtual care skills and infrastructure acquired to implement hybrid CR models when physical distancing recommendations eventually ease. Further guidance on planning for the different levels of restrictions on care is included in Supplemental Figure S1.
Funding Sources
The authors report no funding sources relevant to the contents of this paper.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1320 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at https://doi.org/10.1016/j.cjca.2020.06.006.
Supplementary Material
References
- 1.Thomas R.J., Beatty A.L., Beckie T.M. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol. 2019;74:133–153. doi: 10.1016/j.jacc.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babu A.S., Arena R., Ozemek C., Lavie C.J. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol. 2020;36:792–794. doi: 10.1016/j.cjca.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grace S.L., Turk-Adawi K., Santiago de Araujo Pio C., Alter D.A. Ensuring cardiac rehabilitation access for the majority of those in need: a call to action for Canada. Can J Cardiol. 2016;32:S358–S364. doi: 10.1016/j.cjca.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Grace S.L., Poirier P., Norris C.M. Pan-Canadian development of cardiac rehabilitation and secondary prevention quality indicators. Can J Cardiol. 2014;30:945–948. doi: 10.1016/j.cjca.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Arena R., Myers J., Williams M.A. Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation. 2007;116:329–343. doi: 10.1161/CIRCULATIONAHA.106.184461. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.