Highlights
-
•
A relationship between infecting dose and risk of disease severity has not been demonstrated for COVID-19.
-
•
We report three clusters of COVID-19 in Madrid, in which infected persons experienced different disease severity according to distinct sizes of viral inoculum.
-
•
Smaller viral inoculi as a result of wide social distancing would contribute to the lower pathogenicity of recent SARS-CoV-2 infections.
Keywords: coronavirus, COVID-19, inoculum, outbreak, transmission, epidemiology, disease severity
Abstract
A relationship between the infecting dose and the risk of disease severity has not been demonstrated for SARS-CoV-2 infection. Here, we report three clusters of individuals that were potentially exposed to distinct inoculum in Madrid. Overall each group developed divergent clinical forms of COVID-19. Our data support that a greater viral inoculum at the time of SARS-CoV-2 exposure might determine a higher risk of severe COVID-19.
A relationship between the infecting dose and the risk of disease severity has been demonstrated for several viral infections, including influenza and SARS (Hijano et al., 2019, Chu et al., 2004). For COVID-19, high viral loads either in saliva, respiratory secretions, or blood have been associated with more severe illness (Xu et al., 2020, To et al., 2020). However, it remains unclear whether exposure to a greater viral inoculum could determine a higher risk for developing severe COVID-19. Although intuitive, it has been challenging to obtain such dose-response data.
Herein we report three clusters of SARS-CoV-2 infection in Madrid, in which infected persons experienced divergent clinical outcomes, namely severe, mild, or asymptomatic. We hypothesize that distinct sizes of viral inoculum at the time of exposure could explain their different illness course.
The first cluster was represented by 25 women (age range, 34 to 86 years-old) that lived in a community located on the outskirts of Madrid. The house was large (2000 m2), with three floors, spacious typical ballrooms and halls, high ceilings, large rooms, and a big garden (1500 m2). Lockdown with strict stay home confinement was declared in Madrid on March 14. The day before, the index case, a 47-year-old woman was shopping and visiting relatives. On March 16, she developed fever, cough, anosmia, and dysgeusia. Despite isolation at her room, two household members developed mild symptoms 2-3 days later and another 15 during the following two weeks. Antibody tests performed on April 28 to all 25 residents identified three additional infected asymptomatic persons, whereas four remained seronegative (Fig. 1 ). In this cluster, low viral exposures and social distancing would account for more benign clinical forms of COVID-19, along with asymptomatic and uninfected cases.
Fig. 1.
The timeframe of SARS-CoV-2 infections and COVID-19 disease severity in persons belonging to groups with different viral exposure.
A second cluster of COVID-19 was identified in a group of 12 women (age range, 53 to 85 years-old) that lived together in an apartment flat (650 m2) in downtown Madrid. Several of them admitted going outside their home multiple times despite lockdown implementation. Furthermore, many acknowledged poor compliance with social distancing measures. Therefore, more than one index case could be expected in this site. From March 21th to 23rd, six of them developed mild to severe COVID-19 symptoms and asked for medical assessment at home or nearby clinics. Three developed bilateral pneumonia, one being hospitalized and requiring intensive care support. From March 25 to April 3, another four developed mild to severe symptoms, with one being hospitalized with bilateral pneumonia. Antibody tests on April 28 confirmed infection in all 12 residents, including two that had remained asymptomatic. In this cluster, indoor continuous viral exposure could account for a broader presentation of clinical forms of COVID-19, given that all residents were infected.
The third cluster consisted of a group of ten adults (seven male; age range, 56 to 76 years-old) that met in a small conference room (60 m2) for three hours on March 4, ten days before the nationwide lockdown was implemented. The event was held at a health institution in downtown Madrid. Three attendees had just arrived from Rome (two) and Milan (one), where they had been for a few days. All attendees were asymptomatic on the meeting day and did not take any preventive measures, including sitting next to each other and not wearing face masks. Two days later, two developed COVID-19 symptoms and the rest also did within the next week. COVID-19 was severe in at least four individuals, one being hospitalized at the intensive care unit for nearly one month. Fortunately, he recovered. This cluster reminds one of many features of a large outbreak reported among members of a choir in Washington, USA (Hamner et al., 2020). In this cluster, an extensive indoor viral exposure seemed to account for all attendees' infection and the development of severe clinical forms in half of them.
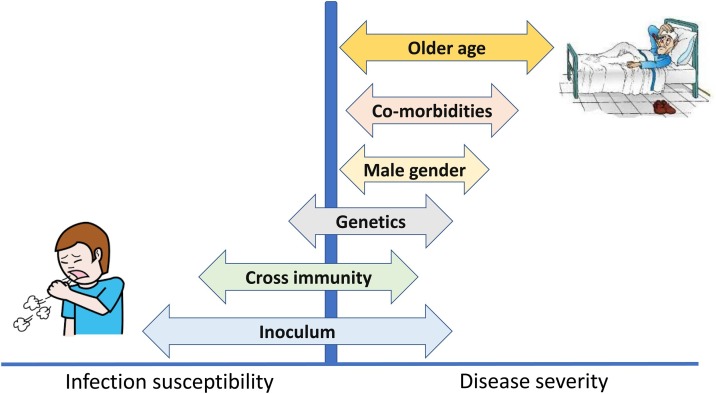
It is worth noting that of the six major determinants of SARS-CoV-2 susceptibility to infection and risk for disease severity (Fig. 2 ), the first two clusters only included women, whereas seven out of ten in the last cluster were male. The mean ages (63.4, 66.3, 62.7 years old, respectively) and the rate of chronic co-morbidities (roughly two-thirds of each group, with hypertension the most common) did not differ significantly in comparing the three clusters. Information on potential cross-immunity with other endemic coronaviruses or genetic variants that could influence the SARS-CoV-2 disease course, was not available, but all individuals were living in Madrid and were Caucasian. Therefore, we hypothesize that a different inoculum at the time of SARS-CoV-2 exposure could explain the different course of infection in these three clusters.
Fig. 2.
Major determinants of SARS-CoV-2 susceptibility to infection and risk for disease severity.
Intriguingly, most recent SARS-CoV-2 infections seem to be less virulent than those that occurred earlier in the COVID-19 outbreak (Pan et al., 2020, Little et al., 2020). Several factors might contribute to this observation, including more frequent late presentations at the beginning of the pandemic. Alternatively, the new coronavirus could steadily become less pathogenic, as result of co-adaptation to human hosts (Martinez, 2020). However, our findings suggest that it most likely reflects the overall lower size of the inoculum in recent infections due to extensive social distancing interventions compared to contagions that occurred earlier in the pandemic.
The recognition that exposure to low viral loads is associated with mild or asymptomatic infections would favor a sensible gradual re-opening of activities. For instance, restricting indoor gatherings where superspreading events are more likely to occur will have a significant impact on transmission, whereas other restrictions —on outdoor activity, for example— might be eased. Promoting activities in open spaces, coupled with rapid isolation of symptomatic persons (self-confinement) and quarantine of contacts would act synergistically to halt COVID-19 spread and severity (Cowling et al., 2020).
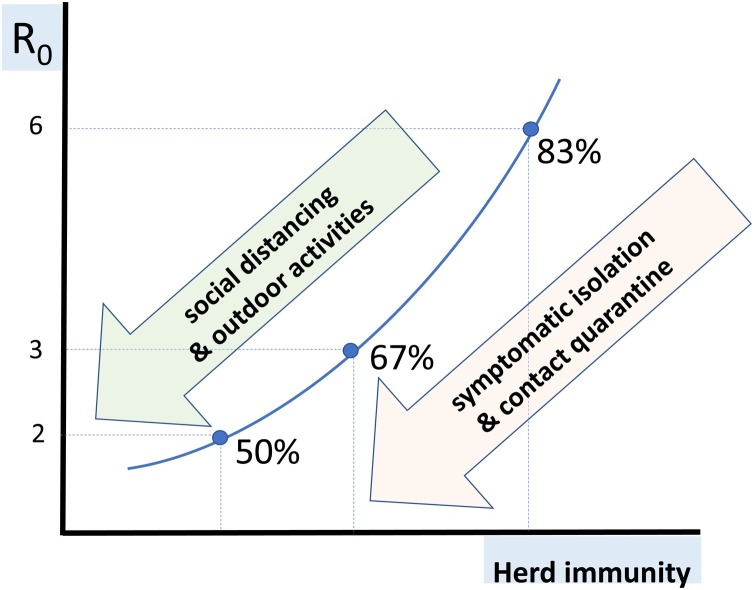
Since overall 80% of the contagions seem to have derived from only 10% of infected individuals (Jarvis et al., 2020), shifting the SARS-CoV-2 community transmission rate (R0) to less than 2 would require that less than half of the population would need to be infected to produce herd immunity (Fig. 3 ). In this scenario, COVID-19 spreading would be expected to be controlled, even in the absence of antivirals or vaccines. Our data support the proposal that keeping social distancing would be effective in reducing contagions as well as driving COVID-19 to less severe forms. This information is crucial when re-opening strategies are urgently needed to alleviate the harmful economic impact of prolonged lockdowns.
Fig. 3.
Herd immunity needed to halt the COVID-19 pandemic as a function of the average community transmission rate (R0).
Conflict of Interests
None.
Funding
We would like to thank the UNIR Foundation for funding diagnostic tests for SARS-CoV-2 antibody detection.
Ethical approval
The study received approval as a descriptive and retrospective observational analysis.
References
- Hamner L., Dubbel P., Capron I. High SARS-CoV-2 attack rate following exposure at a choir practice – Skagit County, Washington, March 2020. MMWR. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- Hijano D., Brazelton de Cardenas J., Maron G. Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR. PLoS One. 2019;14 doi: 10.1371/journal.pone.0220908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C., Poon L., Cheng V. Initial viral load and the outcomes of SARS. CMAJ. 2004;171:1349–1352. doi: 10.1503/cmaj.1040398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T., Chen C., Zhu Z. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. 2020;94:68–71. doi: 10.1016/j.ijid.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To K.K.-W., Tsang O.T.-Y., Leung W.-S.-S. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Wang C., Guo H. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323:1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little P., Read R., Amlot R. Reducing risks from coronavirus transmission in the home – the role of viral load. BMJ. 2020 doi: 10.1136/bmj.m1728. (in press) [DOI] [PubMed] [Google Scholar]
- Martinez M.A. Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob Agents Chemother. 2020;64:e00399–e00420. doi: 10.1128/AAC.00399-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B., Ali S., Ng T. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong-Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvis C., Van Zandvoort K., Gimma A. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020;18:124. doi: 10.1186/s12916-020-01597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]