Abstract
Background and aims
COVID-19 is a contagious disease caused by a new coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Till now there are no vaccines and explicit medicines available for the treatment of COVID-19 disease, therefore the initiatives like public health and social measures are helpful in limiting the quantity of contaminations and saving lives. Keeping this in view, an attempt has been made in the present work to identify the barriers which hinder the implementation of these public health and social measures
Methods
The barriers to implement public health and social measures for preventing transmission of COVID-19 are identified using systematic literature review and these barriers are then categorized using Decision-making trial and evaluation laboratory (DEMATEL) method.
Results
Results reveal that among ten identified barriers, Lack of resources for implementing public health and social measures is found to be the most influential barrier to implement public health and social measures for preventing transmission of COVID-19.
Conclusions
The successful implementation of public health and social measures depends on the adequate availability of resources which include medical equipment, personnel and financial dealings. The outcome of this research work will benefit and motivate the higher authorities to consider and overcome various challenges to prevent the transmission of COVID-19.
Keywords: COVID-19, Public health and social (PHS) measures, Barriers, DEMATEL
Highlights
-
•
This paper identifies important barriers related to the prevention of COVID-19 and categorizes them using DEMATEL method.
-
•
Lack of resources is found to be the most influential barrier.
-
•
Some future research directions are given to prevent transmission of COVID-19.
1. Introduction
According to World Health Organization (WHO) (2020), COVID-19 is a contagious disease caused by a new coronavirus known as SARS-CoV-2 (2019-nCoV). The outbreak of this disease started in Wuhan, China in December 2019 [1]. It is rapidly spreading across the world [[2], [3], [4]]. Breathing difficulty, fever, tiredness, dry cough, nasal congestion etc. are some of the symptoms of COVID-19, which start appearing within two to fourteen days after getting infected. The respiratory droplets of infected individuals are the main reason of its transmission. This infection is diagnosed by using an RT-PCR test [5,6]. Polymerase chain reaction (PCR) testing uses the process of amplification [6]. There is no available evidence to indicate any particular treatment for suspected or confirmed COVID-19 patients. COVID-19 has been declared a pandemic by the WHO [7].
As there is no proper medical treatment reported for curing COVID-19, appropriate alternatives are required for preventing the transmission of COVID-19 in the form of public health and social (PHS) initiatives. Various steps that could limit COVID-19 transmission such as case isolation, contact tracing and quarantine, social distancing, foreign travel measures, and vaccinations and treatments [8].
Proper implementation of PHS measures will possible only after overcoming various challenges. These challenges act as barriers which hamper the implementation of the prevention programs [9]. There should be a proper understanding of obstacles/challenges faced during implementation of PHS measures with management techniques. Thus, it is essential to recognize the barriers that hamper the successful adoption of the PHS measures to prevent the transmission of contagious COVID-19. Further, it is also imperative to analyze these barriers using an appropriate decision making technique to enable management in taking decision regarding effective and efficient implementation of various measures for preventing COVID-19. For analyzing the barriers, an appropriate multi criteria decision making (MCDM) technique can be utilized to determine their relative importance, severity or priority [10]. In this study, the DEMATEL MCDM method is employed for analyzing the barriers.
To prevent the transmission of this contagious disease, an attempt has been made in this study to first recognize the barriers of COVID-19 prevention program through systematic literature survey and expert advice and then with the application of DEMATEL, this work identifies the position of each barrier alongside their level of viability on the prevention system and on the other barriers.
2. Literature review
2.1. Public health and social measures
Public safety and social initiatives must be enforced with the complete involvement of all citizens of community to limit or curb the propagation of COVID-19 [8]. PHS measures include detection and isolation of the infected individuals, contact-tracing and quarantine, social distancing, national and international travel measures, and treatments [8]. As there are no vaccines and treatment available for COVID-19 disease, it is necessary to look for other alternatives which could be helpful in lessening the quantity of contaminations and saving lives. Measures reported by WHO include physical distancing, teleworking, distance learning, restriction on the use of non-essential facilities and services, national and international travel restrictions, home staying etc. Such actions are taken in combination with individual protective measures which is frequent hand washing and etiquette during coughing against contagious COVID-19. To be effective in containing the community transmission of this disease, PHS initiatives must be adopted by the society.
2.2. Barriers for implementing public health and social measures to prevent COVID-19
The challenges which hinder the implementation of PHS measures to prevent COVID-19 are:
2.2.1. Lack of Safety commitment from public (Br-1)
Commitment is a force that binds an individual to a course of action of relevance to one or more targets [11]. Safety commitment from public refers to the fervor in the adoption of PHS measures as per the guidelines issued by the WHO to prevent the transmission of COVID-19. Proper knowledge of novel coronavirus among public and awareness of WHO regulations boost the safety commitment from public. Lack of Commitment from public or public resilience would result in increase in transmission rates [8].
2.2.2. Poor safety culture (Br-2)
A safety culture is a culture of government that puts a strong degree of emphasis on protection principles, values and attitudes - and these are shared by most of the citizens in the region [12].
Safety culture is defined as the set of beliefs, social and technical practices that are concerned with minimizing the exposure of people to conditions considered dangerous [13]. Poor safety culture would result in giving less preference to the prevention and safety measures shared by the WHO in containing the spread of COVID 19.
2.2.3. Lack of administrative commitment and support at community level (Br-3)
The prevention strategies profoundly depend on administrative support, which is necessary for the maintenance, participation, motivation in implementing the COVID-19 prevention process. The commitment from local administration by creating opportunities to facilitate the lock downs, ensuring the basic necessities to be provided to common people to restrict their movement [14,15]. As per WHO guidelines, lock downs are necessary in preventing the transmission rate of COVID-19 outbreak [8] and local administrations need to impose restriction on accessing the public places.
2.2.4. Lack of strict enforcement of WHO regulations (Br-4)
The strict enforcement of WHO regulations would only be possible by informing peoples, officials, leaders about WHO regulations.
Some of the regulations and recommendations provided by WHO [16] to minimize the risk of transmission of COVID-19 disease are
-
•
Evading close interactions with people infected with COVID-19.
-
•
Ensuring frequent hand-washing, exclusively after direct contact with infected people.
-
•
Maintaining cough etiquettes by the people suffering from respiratory infection.
If the regulations provided by WHO are not followed properly, the COVID-19 pandemic will contribute more to public hazard thereby more transmissions and loss of lives will follow [17,18]. Enforcement of strict social distancing measures may assist in limiting the spread of COVID-19 disease. The quarantine of individuals diagnosed with the SARS-CoV-2 virus along with their family members will be effective in reducing cases [18].
2.2.5. Lack of resources for implementing public health and social measures (Br-5)
Insufficient funds, improper resource allocation, short-ranged mentality, lack of interest etc. constitute the lack of resources [19]. Lack of resources complicates setting up isolation wards or treatment centers for coronavirus and providing critical care to those suffering from the most severe cases of COVID-19. Increase in the number of COVID-19 infected cases might put significant pressure on hospitals related to critical care facilities, some of which may not have proper resources or manpower to cope with this situation [20]. This barrier includes resources like equipment, personnel, financial dealings etc. which are considered to be critical barriers while implementing COVID-19 preventive measures.
2.2.6. Lack of medical facilities at community level (Br-6)
The pandemic novel coronavirus disease (COVID-19) has raised demand for medications, vaccinations, testing facilities, diagnostics and reagents. Procurement, use and management of medical products must be carefully done. Shortage of medical facilities like personal protective equipment, medical resources (i.e., oxygen supply, ventilators), have aggravated the rise of infections in China’s Wuhan [21].
2.2.7. Lack of door to door services during quarantine period (Br-7)
Around the globe major portion of public is under self-quarantine to prevent spreading of the novel COVID-19 facing several trails like shortage of basic groceries. The door to door services can prove a better plan in order to avoid large gatherings at distribution centers, medical shops [22].
2.2.8. Lack of proper communication between health advisors and public (Br-8)
Communication is a vital element in all phases of the health care procedure. Communication is playing important role in patient’s care as it involves different people (group of doctors, nurses, specialists, and other staff at a hospital at different stages to share patient information and discussing the treatment [23]. The aspects of healthcare include team work, leadership and workplace culture are all affected due to poor communication. Institutions with strong communication strategies can enrich the health of their patients, while those without effective procedures can adversely affect the well-being of patients. Health care experts and organizations need to understand the significance of communication in health care sector in order to stop the COVID-19 transmission. Also, proper communication between health advisors and public will motivate people to be aware of COVID-19 and take adequate measures to prevent its transmission.
2.2.9. Lack of government policies (Br-9)
It is obligatory for governments to formulate effective policies for the prevention, treatment and control of harmful diseases [15]. Governments must ensure that the details they share to the public about COVID-19 is accurate, timely, and consistent with human rights principles. Also, government should frame policies that could be easily implemented to prevent COVID-19 disease.
2.2.10. Public stigmatization (Br-10)
Stigma arises when people adversely link a particular group with an infectious disorder, such as COVID-19. Stigma can drive people to hide their illness which prevent patient from seeking immediate health care, discourage them from following health measures. Stigmatization may progressively contribute to more severe health issues, continuous transmission and difficulty in managing infectious diseases during an outbreak [24].
3. Methodology
Analyzing the Barriers for implementing PHS measures to prevent COVID-19 using DEMATEL is a Multiple-Comparison Decision Making (MCDM) method. In this work, the objective is the successful adoption of PHS measures to prevent COVID-19. Thus, to fulfill this goal, the barriers which hinder the successful implementation of the COVID-19 prevention measures need to be identified and evaluated. In order to do so, initially, 15 barriers are acknowledged through the systematic review of literature related to COVID-19 and PHS measures. The list of barriers reduced to 10 after validating the relevance of barriers in accordance with PHS measures to prevent COVID-19 by the designated Indian Experts.
Battelle Geneva Institute established the DEMATEL method in order to examine the complicated world problems, with the emphasis on interactive man-model methods and to examine the qualitative and factor-linked dimensions of societal problems [25]. This method assists with better understanding for distinguishing of pragmatic measures for particular problems or the cluster of intertwined issues. This technique is better than ordinary methods due to revelation of the interactions between factors, ranking the factors relating with the kind of associations and highlighting the influential strength of one factor over another factor [10].
The steps involved in the DEMATEL method are explained below:
-
(i)
Generate the individual direct influence matrix (P).
The non-negative matrix attained from the respondents after assessing the relationships between n criteria . Suppose m respondents are asked to indicate the direct influence of criteria “” on criteria “” by an integer score of 0, 1, 2, 3 and 4 that represents no effect, very low effect, small effect, moderate effect, and very strong effect respectively, then the direct influence provided by kth respondent is denoted by Where k is the number of respondents.
-
(ii)
Computation of group direct influence matrix.
The group direct influence matrix is computed by aggregating the opinions from m respondents can be computed from equation (1)
| (1) |
| (2) |
where,
| (3) |
-
(iv)
Computation of Total Relation matrix “T”
The total relation matrix is determined by summing the direct effects and indirect effects using equation (4)
| (4) |
where I is the identity matrix
-
(v)
Calculation of the Prominence and Relation values
| (5) |
| (6) |
The row summation of ith row elements of matrix T is symbolized by presented in equation (5) indicates the effect of ith criterion on the other criteria, likewise the column summation of jth column elements of matrix T is symbolized by presented in equation (6) indicates effect on jth criterion by other criteria. The values of (R − C) represent the net effect contributed by that criterion to the system. Furthermore, if (R − C) is positive, criterion i is a net cause, whereas criterion i is a net receiver if (R − C) is negative and the values R + C is called as Prominence which shows the degree of central role played by that criteria in the system.
4. Results
The present paper identifies and evaluates the barriers for the successful adoption of various measures to prevent COVID-19 disease. After reviewing prior research work and obtaining expert’s advice, ten barriers were identified and presented in section 2.3. The identified barriers were then evaluated by DEMATEL as discussed in section 3. The Prominence (R + C) and net effect (R–C) is calculated from the total relation matrix using Eq. (5) and Eq. (6) respectively. The overall direct relation matrix is computed using equation (1) as shown in Table 1 .
Table 1.
Overall direct relation matrix (Please refer to text (section 2.2) for Br-1 to Br-10).
| Barrier | Br-1 | Br-2 | Br-3 | Br-4 | Br-5 | Br-6 | Br-7 | Br-8 | Br-9 | Br-10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Br-1 | 0 | 4.4 | 3 | 3.6 | 2.8 | 4 | 4.2 | 3.4 | 3.4 | 4 |
| Br-2 | 2.2 | 0 | 2.4 | 2 | 2.4 | 2.6 | 2.6 | 2.4 | 2.4 | 2.4 |
| Br-3 | 3.2 | 3.4 | 0 | 3.6 | 2.6 | 2.8 | 3.6 | 3 | 4 | 4 |
| Br-4 | 2.2 | 2.4 | 2.4 | 0 | 2 | 3 | 3.6 | 2.4 | 2.4 | 3.2 |
| Br-5 | 3.8 | 4.4 | 3.8 | 4.4 | 0 | 4.6 | 4.2 | 3.8 | 3.6 | 4 |
| Br-6 | 2 | 2.4 | 2.6 | 2.6 | 2 | 0 | 2 | 2.4 | 2.2 | 2.6 |
| Br-7 | 2 | 2.4 | 2.2 | 2.4 | 1.6 | 3.6 | 0 | 2.4 | 2.2 | 3.6 |
| Br-8 | 3.2 | 4.4 | 3.8 | 4.4 | 3.2 | 3.8 | 3.6 | 0 | 3 | 3.6 |
| Br-9 | 2.8 | 4.4 | 3 | 4.2 | 2.4 | 2.8 | 3 | 2 | 0 | 2.6 |
| Br-10 | 2.2 | 2.6 | 2.6 | 3 | 1.8 | 3 | 2.8 | 2.4 | 2.2 | 0 |
The normalized direct-relation matrix (B) is computed from equations (2), (3) as presented in Table 2 .
Table 2.
Normalized direct-relation matrix (B) (Please refer to text (section 2.2) for Br-1 to Br-10).
| Barrier | Br-1 | Br-2 | Br-3 | Br-4 | Br-5 | Br-6 | Br-7 | Br-8 | Br-9 | Br-10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Br-1 | 0.000 | 0.120 | 0.082 | 0.098 | 0.077 | 0.109 | 0.115 | 0.093 | 0.093 | 0.109 |
| Br-2 | 0.060 | 0.000 | 0.066 | 0.055 | 0.066 | 0.071 | 0.071 | 0.066 | 0.066 | 0.066 |
| Br-3 | 0.087 | 0.093 | 0.000 | 0.098 | 0.071 | 0.077 | 0.098 | 0.082 | 0.109 | 0.109 |
| Br-4 | 0.060 | 0.066 | 0.066 | 0.000 | 0.055 | 0.082 | 0.098 | 0.066 | 0.066 | 0.087 |
| Br-5 | 0.104 | 0.120 | 0.104 | 0.120 | 0.000 | 0.126 | 0.115 | 0.104 | 0.098 | 0.109 |
| Br-6 | 0.055 | 0.066 | 0.071 | 0.071 | 0.055 | 0.000 | 0.055 | 0.066 | 0.060 | 0.071 |
| Br-7 | 0.055 | 0.066 | 0.060 | 0.066 | 0.044 | 0.098 | 0.000 | 0.066 | 0.060 | 0.098 |
| Br-8 | 0.087 | 0.120 | 0.104 | 0.120 | 0.087 | 0.104 | 0.098 | 0.000 | 0.082 | 0.098 |
| Br-9 | 0.077 | 0.120 | 0.082 | 0.115 | 0.066 | 0.077 | 0.082 | 0.055 | 0.000 | 0.071 |
| Br-10 | 0.060 | 0.071 | 0.071 | 0.082 | 0.049 | 0.082 | 0.077 | 0.066 | 0.060 | 0.000 |
The normalized direct-relation matrix (B) changed into Total-Relation Matrix (T) using equation (4) and the same is presented in Table 3 .
Table 3.
Total-Relation Matrix (T) (Please refer to text (section 2.2) for Br-1 to Br-10).
| Barrier | Br-1 | Br-2 | Br-3 | Br-4 | Br-5 | Br-6 | Br-7 | Br-8 | Br-9 | Br-10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Br-1 | 0.207 | 0.373 | 0.302 | 0.350 | 0.257 | 0.362 | 0.361 | 0.299 | 0.308 | 0.361 |
| Br-2 | 0.199 | 0.182 | 0.217 | 0.231 | 0.189 | 0.247 | 0.243 | 0.208 | 0.214 | 0.241 |
| Br-3 | 0.275 | 0.333 | 0.212 | 0.334 | 0.240 | 0.317 | 0.331 | 0.275 | 0.307 | 0.344 |
| Br-4 | 0.209 | 0.256 | 0.228 | 0.192 | 0.188 | 0.270 | 0.279 | 0.219 | 0.225 | 0.274 |
| Br-5 | 0.326 | 0.404 | 0.347 | 0.399 | 0.208 | 0.406 | 0.391 | 0.333 | 0.338 | 0.391 |
| Br-6 | 0.190 | 0.238 | 0.217 | 0.240 | 0.176 | 0.175 | 0.223 | 0.204 | 0.205 | 0.240 |
| Br-7 | 0.196 | 0.245 | 0.215 | 0.243 | 0.172 | 0.273 | 0.178 | 0.210 | 0.211 | 0.272 |
| Br-8 | 0.291 | 0.376 | 0.324 | 0.372 | 0.269 | 0.361 | 0.351 | 0.217 | 0.302 | 0.355 |
| Br-9 | 0.245 | 0.331 | 0.266 | 0.322 | 0.218 | 0.291 | 0.292 | 0.232 | 0.187 | 0.286 |
| Br-10 | 0.204 | 0.254 | 0.227 | 0.260 | 0.179 | 0.262 | 0.254 | 0.213 | 0.215 | 0.186 |
Finally using equations (5), (6), the prominence (Pi) and net effect (Ei) is computed and presented in Table 4 .
Table 4.
Prominence (Pi) and net effect (Ei) (Please refer to text (section 2.2) for Br-1 to Br-10).
| Barrier | R | C | R + C | R–C |
|---|---|---|---|---|
| Br-1 | 3.179 | 2.343 | 5.523 | 0.836 |
| Br-2 | 2.172 | 2.991 | 5.163 | −0.820 |
| Br-3 | 2.968 | 2.554 | 5.522 | 0.413 |
| Br-4 | 2.340 | 2.943 | 5.283 | −0.603 |
| Br-5 | 3.543 | 2.095 | 5.638 | 1.447 |
| Br-6 | 2.108 | 2.963 | 5.071 | −0.856 |
| Br-7 | 2.215 | 2.902 | 5.117 | −0.687 |
| Br-8 | 3.217 | 2.410 | 5.627 | 0.807 |
| Br-9 | 2.670 | 2.513 | 5.184 | 0.157 |
| Br-10 | 2.253 | 2.949 | 5.202 | −0.696 |
R: Row summation of ith row elements of total relation matrix (T).
C: Column summation of “jth” column elements of total relation matrix (T).
Mid-line in ‘R–C’ shows the ‘minus’ sign.
5. Discussion on results
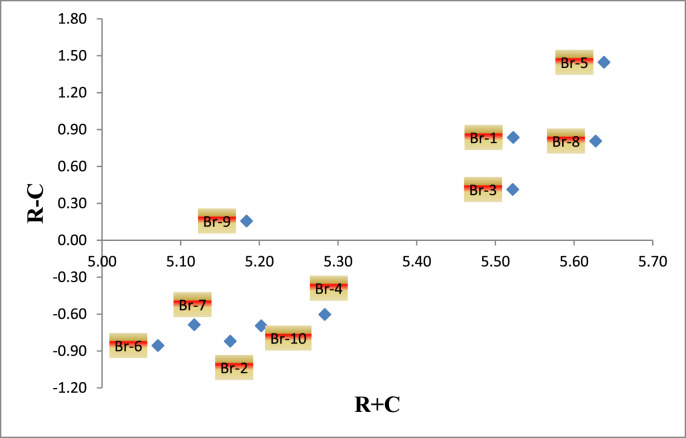
In this study, the relation among various criteria were evaluated by using DEMATEL method and unlike traditional models, this technique is not limited to considering only direct effects or single directions of criteria. The results shown in Table 4 indicate that Lack of resources for implementing PHS measures (Br-5) is the most influential factor (barrier) against the successful adoption PHS initiatives to prevent COVID-19. The successful implementation of PHS measures depends on the adequate availability of resources which include medical equipment, personnel, financial dealings. Results reported by the previous researchers supports the outcomes of current study as they have also concluded that lack of resources among the most severe barriers in the prevention of COVID-19 disease [19,26]. Lack of Resources (Br-5) followed by Lack of proper communication between health advisors and public (Br-8) and Lack of Safety commitment from Public (Br-1) are found to be the severe factors in hindering the successful implementation of PHS measures in order to prevent the transmission of COVID-19 disease. Based on the R + C values presented in Table 4, the severity order of the barriers is Br-5>Br-8>Br-1>Br-3>Br-9> Br-4> Br-10> Br-2> Br-7> Br-6. Thus, from the R–C values, the barriers are divided into two groups as cause and effect groups. The barriers ‘Lack of resources for implementing PHS measures (Br-5)’, ‘Lack of Safety commitment from Public (Br-1)’, ‘Lack of proper communication between health advisors and public (Br-8)’, ‘Lack of administrative commitment and support at community level (Br-3)’ and ‘Lack of government polices (Br-9)’ having the positive values of R–C. These barriers are categorized under cause group. The barriers ‘Lack of strict enforcement of WHO regulations (Br-4)’, ‘environmental protection laws (Br-10)’, ‘Poor safety culture (Br-2)’, ‘Lack of door to door services during quarantine period (Br-7) and ‘Lack of medical facilities at community level (Br-6)’ having the negative values of R–C are categorized under effect group.
Furthermore the “net cause/effect” of each barrier are determined through the values of (R–C). If the value of difference (R–C) is positive, then the barrier is assumed to produce the “net cause” and if the difference (R–C) if found to be negative then the barrier is the “net effect”. Fig. 1 displays the R + C and R–C plots, thereby representing the causal relation between the barriers of the successful implementation of PHS measures. For more perspectives, these findings were discussed with the experts.
Fig. 1.
Cause and effect diagram.
6. Research implications
The outcome of the present work will benefit and motivate the higher authorities to consider and overcome various challenges related to the prevention of COVID-19 disease transmission by understanding the severity of each barrier. Also, this study classifies the barriers into two categories viz. influential and influenced. On the basis of this classification, the administration will devise an appropriate plan to put more focus on dealing with the barriers as per their severity. The severity order provided in this study will enable the administration to concentrate only on the influential barriers while the severity of influenced barriers will be subsequently reduced. The findings of this research would also assist researchers in spreading awareness and the importance of PHS measures in controlling the virus transmission. As per the available literature accessed by the authors, it is found that more work is still need to be carried out on implementation of PHS measures in the infected areas.
7. Conclusions and future research directions
The initiatives like PHS measures are helpful in limiting the COVID-19 transmission. Different measures are being implemented in affected regions to control the spread of this disease. However, there are certain barriers that prevent implementation of PHS measures. Among ten identified barriers in the present study, lack of resources for implementing PHS measures is the most influential factor (barrier) against the successful adoption of PHS initiatives to prevent COVID-19. On the other hand, Lack of medical facilities at community level is the least influential factor (barrier).
This study depends on literature survey and feedback from experts. There is a chance to ignore certain barriers during literature survey and obtaining expert advice. Also, categorization of barriers is based on the expert feedback and could be skewed against their degree of research. Also, the study depends on the information provided by the Indian experts and the outcome of this work may not be generalized globally. These impediments open the door for future research. In future, more barriers may be found through focused studies and similar work may be carried out by including them in different countries to establish their priority and also relationship between them by using other MCDM methods.
Funding
None.
Author contribution
Annayath Maqbool: contributed in the original draft preparation of the paper, barrier identification and analysis. Noor Zaman Khan: contributed in reviewing and revising the language and the technical content of the paper.
Ethical approval
Not required (The current study does not involve any patient or volunteer which require any ethical approval).
Declaration of competing interest
None declared
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gorbalenya A.E. Severe acute respiratory syndrome-related coronavirus — the species and its viruses, a statement of the Coronavirus Study Group. 2020. https://www.biorxiv.org/content/10.1101/2020.02.07.937862v1 Preprint at.
- 4.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter M., Shieh J. Molecular cloning and recombinant DNA technology. In: Carter Matt., editor. Jennifer shieh, guide to research techniques in neuroscience. second ed. Academic Press; 2015. pp. 219–237. [DOI] [Google Scholar]
- 6.Hadaya J., Schumm M., Livingston E.H. Testing individuals for coronavirus disease 2019 (COVID-19) J Am Med Assoc. 2020 doi: 10.1001/jama.2020.5388. [DOI] [PubMed] [Google Scholar]
- 7.WHO WHO director-general’s statement on IHR emergency committee on novel coronavirus (2019-nCoV) 2020, January 30. https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-mergency-committee-on-novel-coronavirus-(2019-ncov Retrieved April 10, 2020, from.
- 8.WHO Coronavirus disease 2019 (COVID-19) situation report – 72. 2020, April 1. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?sfvrsn=3dd8971b_2 Retrieved April 5, 2020, from.
- 9.Koppelaar E., Knibbe J.J., Miedema H.S., Burdorf A. Determinants of implementation of primary preventive interventions on patient handling in healthcare: a systematic review. Occup Environ Med. 2009;66(6):353–360. doi: 10.1136/oem.2008.042481. [DOI] [PubMed] [Google Scholar]
- 10.Maqbool A., Khan S., Haleem A., Khan M.I. Investigation of drivers towards adoption of circular economy: a DEMATEL approach. In: Kumar H., Jain P., editors. Recent advances in mechanical engineering. Lecture notes in mechanical engineering. Springer; Singapore: 2020. [Google Scholar]
- 11.Cohen A. Organizational commitment and turnover: a meta-analysis. Acad Manag J. 1993;36:1140–1157. [Google Scholar]
- 12.Guldenmund F.W. The nature of safety culture: a review of theory and research. Safety Sci. 2000;34:215–257. [Google Scholar]
- 13.Turner B.A., Pidgeon N., Blockley D., Toft B. Position paper for the second world bank workshop on safety control and risk management, karlstad, Sweden. 1989. Safety culture: its importance in future risk management. [Google Scholar]
- 14.Dassin L.L., Kim J.H. Law enforcement priorities and practicalities during the COVID-19Pandemic. 2020. https://www.clearyenforcementwatch.com/2020/03/law-enforcement-priorities-and-practicalities-during-the-covid-19-pandemic/ Retrieved April 4, 2020, from.
- 15.Human Rights Watch March 19). Human rights dimensions of COVID-19 response. 2020. https://www.hrw.org/news/2020/03/19/human-rights-dimensions-covid-19-response Retrieved April 16, 2020, from.
- 16.WHO Coronavirus disease 2019 (COVID-19) situation report – 23. 2020, February 12. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200212-sitrep-23-ncov.pdf Retrieved April 16, 2020, from.
- 17.Wilder-Smith A. Can we contain the COVID-19 outbreak with the same measures as for SARS? LANCET Infec. Dis. 2020 doi: 10.1016/S1473-3099(20)-830129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kohli K.K. Enforcing strict social distancing measures may prevent covid 19 outbreak: lancet. Retrieved april 5, 2020, from enforcing strict social distancing measures may prevent covid 19 outbreak: lancet. 2020. https://medicaldialogues.in/medicine/news/enforcing-strict-social-distancing-measures-may-prevent-covid-19-outbreak-lancet-64205
- 19.Yazdani A., Wells R. Barriers for implementation of successful change to prevent musculoskeletal disorders and how to systematically address them. Appl Ergon. 2018;73:122–140. doi: 10.1016/j.apergo.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan W.J., Chen R.C., Zhong N.S. Strategies for the prevention and management of coronavirus disease 2019. Eur Respir J. 2019 doi: 10.1183/13993003.00597-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okyere M.A., Forson R., Essel-Gaisey F. Positive externalities of an epidemic: the case of the coronavirus (COVID-19) in China. J Med Virol. 2020:1–4. doi: 10.1002/jmv.25830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coiera E. Communication systems in healthcare. The Clinical biochemist. Review. 2006;27(2):89–98. [PMC free article] [PubMed] [Google Scholar]
- 24.WHO Coronavirus disease 2019 (COVID-19) situation report – 35. 2020, February 24. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200224-sitrep-35-covid-19.pdf?sfvrsn=1ac4218d_2 Retrieved April 17, 2020, from.
- 25.Gabus A., Fontela E. Battelle Geneva Research Centre; Switzerland, Geneva: 1972. World problems an invitation to further thought within the framework of DEMATEL. [Google Scholar]
- 26.Xie J., Tong Z., Guan X. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05979-7. [DOI] [PMC free article] [PubMed] [Google Scholar]