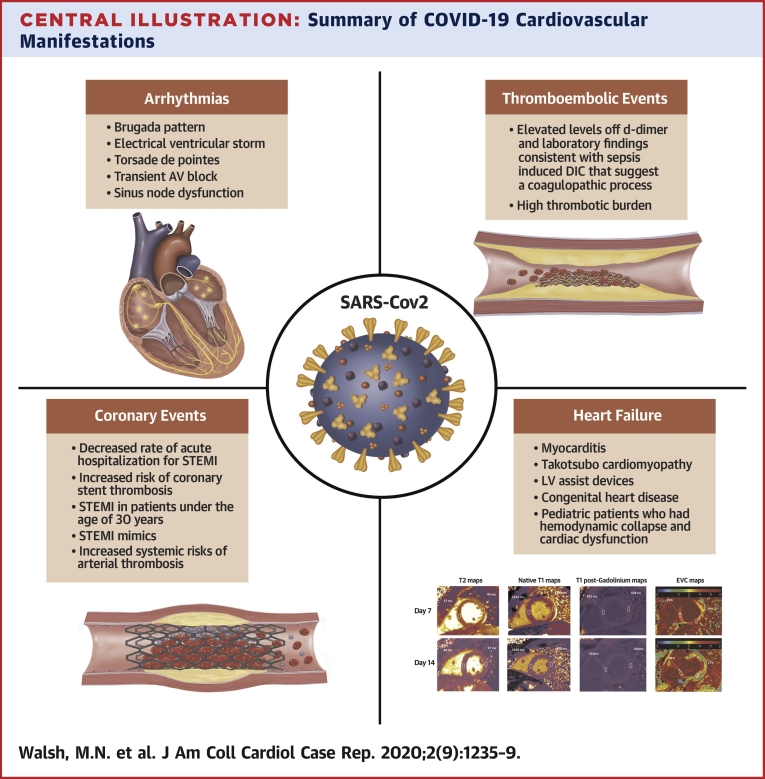
Central Illustration
The coronavirus disease-2019 (COVID-19) pandemic has revolutionized clinical practice in recent months unlike any other health emergency in recent years. JACC: Case Reports has taken this challenge very seriously, dedicating to it an entire issue. We have received excellent case reports from across the world. Our goal is to provide a comprehensive report of representative cardiovascular involvement in COVID-19 (Central Illustration).
Central Illustration.
Summary of COVID-19 Cardiovascular Manifestations
LV = left ventricular; STEMI = ST-segment elevation myocardial infarction.
Arrhythmias
Besides the concern regarding QT interval prolongation with hydroxychloroquine and azithromycin treatment, COVID-19 is strongly associated with the occurrence of sudden unexpected arrhythmias. Given the general ignorance of the pathophysiological mechanisms of the virus at the time of submission of these case reports, it is hard to state with certainty that COVID-19 has been the cause of these arrhythmias, but they surely offer an interesting direction for future research in the field. Included are cases of Brugada type I pattern positivization (1) in the context of fever, one of the most common presenting symptoms of the disease (2); electrical ventricular storm (3); transient atrioventricular block in the absence of myocarditis (4); sinus node dysfunction requiring pacemaker implantation (5); and finally a provocative report on the use of amiodarone as a possible treatment for COVID-19 (6). Overall, the cytokine storm has proved to have a strong impact on the conduction system.
Thromboembolic Events
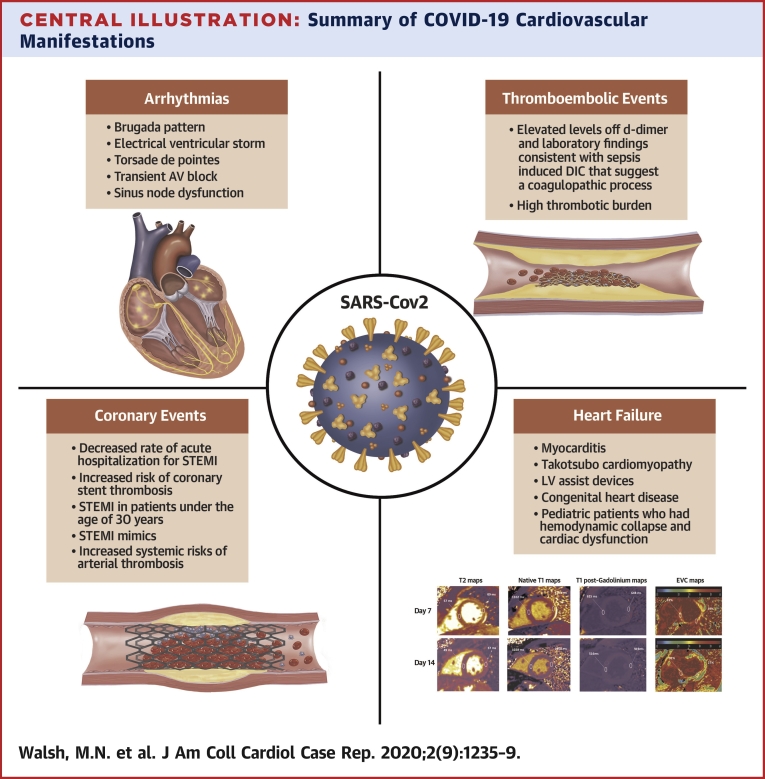
The clinical presentation of patients with COVID-19 has ranged from asymptomatic to acute respiratory distress syndrome requiring mechanical ventilation. One cause of sudden respiratory deterioration is the increased risk for venous thromboembolic disease in these patients (7) (Figure 1). These events have been noted both early and in the recovery phase of COVID-19. Furthermore, thromboembolic events have occurred despite the use of prophylactic anticoagulation or even full anticoagulation (8). A majority of patients have elevated levels of d-dimer and laboratory findings consistent with sepsis-induced diffuse intravascular coagulation, suggesting a coagulopathic process, yet no prospective studies have demonstrated the predictive nature of these markers for the occurrence of a thromboembolic event, only a higher risk for mortality (9). The early recognition and treatment of venous thromboembolic disease has therefore been a dilemma. We therefore provide commentary and suggest treatment algorithms (10).
Figure 1.
Thromboembolic Events: Pulmonary Embolism in a Patient With COVID-2019
Coronary Interventions
We received case reports in 4 general categories detailing an increased risk or arterial thrombosis during the COVID-19 pandemic.
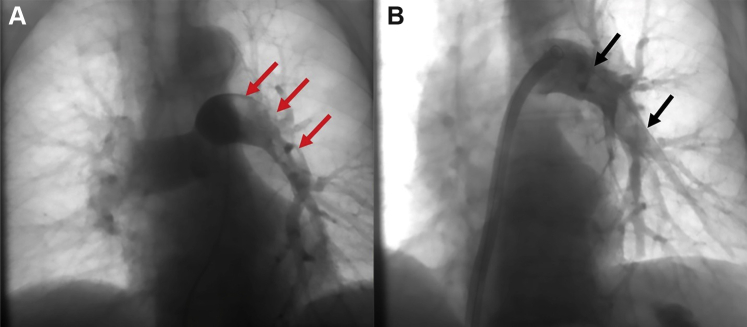
First, the decreased rate of acute hospitalization for ST-segment elevation myocardial infarction (STEMI) has paralleled an increased incidence of patients presenting late after STEMI onset. The result has been to remind us in several submissions of the natural history of STEMI before the reperfusion therapy era, when transmural infarction was associated with severe complications. These include complete atrioventricular heart block, left ventricular aneurysm formation, left ventricular apical thrombosis with risk for systemic embolization, severe ischemic cardiomyopathy, rupture of the left ventricular free wall or intraventricular septum, papillary muscle ischemia or rupture, and left or right ventricular shock. Another report suggests an increased risk for coronary stent thrombosis (Figure 2) causing STEMI in infected patients (11,12).
Figure 2.
Acute Stent Thrombosis in Patients With COVID-2019: Fluoroscopic and Optical Coherence Tomographic Study
Second, there were a number of cases of STEMI in patients younger than 30 years without risk factors for atherosclerosis (13). This phenomenon occasionally occurred before COVID-19, but the increased incidence reminds us to always include myocardial infarction in the differential diagnosis of a younger patient with chest pain and to always consider performing screening electrocardiography.
Third, a number of cases of STEMI mimics were submitted, including patients with ST-segment elevation due to myopericarditis, Brugada pattern, takotsubo cardiomyopathy, or endothelial dysfunction due to infection or cytokine storm. As many as 40% of patients with COVID-19 and ST-segment elevation may have normal coronary arteries on angiography, complicating the decision whether to administer fibrinolytic therapy to patients without early access to primary percutaneous coronary intervention.
Finally, there were reports of spontaneous thrombosis (14) involving the ascending and descending aorta, the cerebrovascular arteries, the mesenteric and renal arteries, and the peripheral arteries, underscoring an increased systemic risk for arterial thrombosis in patients with COVID-19.
Heart Failure and Cardiomyopathies
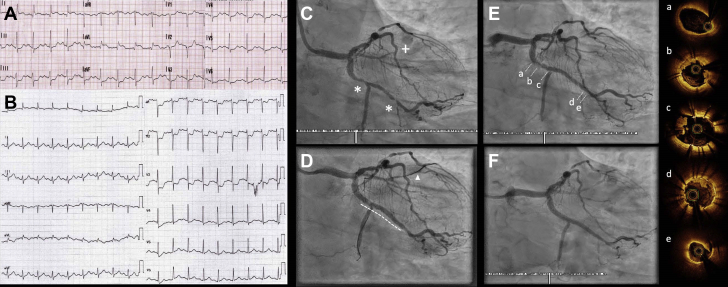
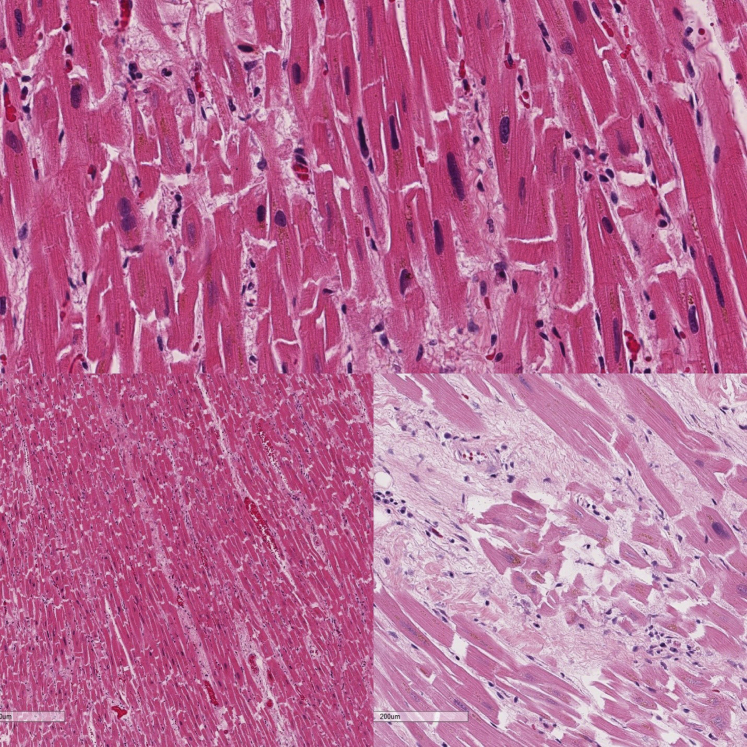
The development of heart failure in patients infected with severe acute respiratory syndrome coronavirus-2 has been described to involve 2 different, and overlapping, mechanisms. One is cytokine release resulting in myocardial inflammation (Figure 3), and the other is purported to be direct viral infection causing myocarditis (15). Endomyocardial biopsy of affected patients has demonstrated both inflammatory infiltrates and viral particles. The heart failure cases presented in this special issue, however, describe more varied presentations of patients, some with pre-existing heart failure and others with no known cardiac disease prior to becoming ill with infection.
Figure 3.
Endomyocardial Biopsy of a Patient With COVID-2019
In addition to cases of direct myocardial injury, some with pathological evidence, we also present 2 cases of takotsubo cardiomyopathy (16,17) without evidence of STEMI or coronary artery disease. Both patients had ventricular recovery after supportive treatment, 1 of whom had recently undergone cardiac transplantation. The investigators of this latter case elegantly describe the complex investigation of possible allograft rejection and the delicate balance of immunosuppression in the setting of severe acute respiratory syndrome coronavirus-2 infection. Two cases highlight the special circumstances faced by patients with left ventricular assist devices (18,19), which include the inability to tolerate prone positioning to augment respiratory support because of the mechanical equipment and the hypothesis that mechanical circulatory support may provide a type of protection against the most serious hemodynamic consequences of severe acute respiratory syndrome coronavirus-2 infection. Included also is a case series of pediatric patients who had hemodynamic collapse and cardiac dysfunction (20), a presentation that has been rare in this younger age group.
The now well-recognized thromboembolic disorders encountered with this disease include a case in this issue of massive pulmonary embolism and resultant severe right heart failure (8). And 2 separate reports describe patients with concomitant noncardiac disease, 1 with human immunodeficiency virus infection (18) and 1 with influenza (21). All the cases of heart failure represent the investigators’ best attempts at providing supportive and emerging therapies at a time when they had no established guidelines and no best practices to follow.
From the beginning of the pandemic, we believed that it was very important to publish the “voices” of our frontline colleagues across the world, to help cardiologists to get acquainted with mechanical ventilation (22), to describe the first evidence of sex differences in COVID-19 (23), and to discuss the significant changes in health care with telemedicine and virtual clinics. The impact of COVID-19 on African Americans has also recently been described in JACC (24). Our aim was to provide a complete and comprehensive issue, in parallel with the sister JACC journals and the American College of Cardiology’s COVID Hub.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Vidovich M.I. Transient Brugada-like electrocardiographic pattern in a patient with COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1245–1249. doi: 10.1016/j.jaccas.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorgente A., Capulzini L., Brugada P. The known into the unknown: Brugada syndrome and COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1250–1251. doi: 10.1016/j.jaccas.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Brien C., Ning N., McAvoy J. Electrical storm in COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1256–1260. doi: 10.1016/j.jaccas.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kir D., Mohan C., Sancassani R. Heart brake: an unusual cardiac manifestation of coronavirus disease 2019 (COVID-19) J Am Coll Cardiol Case Rep. 2020;2:1252–1255. doi: 10.1016/j.jaccas.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cimino G., Pascariello G., Bernardi N. Sinus node dysfunction in a young patient with COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1240–1244. doi: 10.1016/j.jaccas.2020.05.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castaldo N., Aimo A., Castiglione V., Padalino C., Emdin M., Tascini C. Safety and efficacy of amiodarone in a patient with COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1307–1310. doi: 10.1016/j.jaccas.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marginean A., Masic D., Brailovsky Y., Fareed J., Darki A. Difficulties of managing submassive and massive pulmonary embolism in the era of COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1383–1387. doi: 10.1016/j.jaccas.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ullah W., Saeed R., Sarwar U., Patel R., Fischman D.L. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. J Am Coll Cardiol Case Rep. 2020;2:1379–1382. doi: 10.1016/j.jaccas.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Konstantinides S.V. Thrombosis and thromboembolism related to COVID-19: increase the level of awareness, lower the threshold of suspicion, and keep following the guidelines. J Am Coll Cardiol Case Rep. 2020;2:1388–1390. doi: 10.1016/j.jaccas.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sethi S.S., Zilinyi R., Green P. Right ventricular clot in transit in COVID-19: implications for the pulmonary embolism response team. J Am Coll Cardiol Case Rep. 2020;2:1391–1396. doi: 10.1016/j.jaccas.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prieto-Lobato A., Ramos-Martínez R., Vallejo-Calcerrada N., Corbí-Pascual M., Córdoba-Soriano J.G. A case series of stent thrombosis during the COVID-19 pandemic. J Am Coll Cardiol Case Rep. 2020;2:1291–1296. doi: 10.1016/j.jaccas.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vidovich M.I., Fischman D.L., Bates E.R. COVID-19 STEMI 2020: it’s not what you know, it’s how you think. J Am Coll Cardiol Case Rep. 2020;2:1289–1290. doi: 10.1016/j.jaccas.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zendjebil S., Zeitouni M., Batonga M. Acute multi-vessel coronary occlusion revealing COVID-19 in a young adult. J Am Coll Cardiol Case Rep. 2020;2:1297–1301. doi: 10.1016/j.jaccas.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woehl B. Four cases of aortic thrombosis in patients with COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1397–1401. doi: 10.1016/j.jaccas.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garot J. SARS-CoV-2 fulminant myocarditis. J Am Coll Cardiol Case Rep. 2020;2:1342–1346. doi: 10.1016/j.jaccas.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Minhas A.S., Scheel P., Garibaldi B. Takotsubo syndrome in the setting of COVID-19 infection. J Am Coll Cardiol Case Rep. 2020;2:1321–1325. doi: 10.1016/j.jaccas.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernardi N., Emiliano C., Giuliana C. Covid-19 pneumonia, takotsubo syndrome and left ventricle thrombi. J Am Coll Cardiol Case Rep. 2020;2:1359–1364. doi: 10.1016/j.jaccas.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahmood K., Rashed E.R., Oliveros E. Predisposition or protection? COVID-19 in a patient on LVAD support with HIV/AIDS. J Am Coll Cardiol Case Rep. 2020;2:1337–1341. doi: 10.1016/j.jaccas.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chau V.Q., Oliveros E., Mahmood K. The imperfect cytokine storm: severe COVID-19 with ARDS in patient on durable LVAD support. J Am Coll Cardiol Case Rep. 2020;2:1315–1320. doi: 10.1016/j.jaccas.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joshi K., Kaplan D., Bakar A. Cardiac dysfunction and shock in pediatric patients with COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1267–1270. doi: 10.1016/j.jaccas.2020.05.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sang C.J., III, Heindl B., Von Mering G. Stress induced cardiomyopathy precipitated by COVID-19 and influenza a co-infection. J Am Coll Cardiol Case Rep. 2020;2:1356–1358. doi: 10.1016/j.jaccas.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gage A., Higgins A., Lee R., Panhwar M.S., Kalra A. Reacquainting cardiology with mechanical ventilation in response to the COVID-19 pandemic. J Am Coll Cardiol Case Rep. 2020;2:1402–1406. doi: 10.1016/j.jaccas.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma G., Volgman A.S., Michos E.D. Sex differences in mortality from COVID-19 pandemic: are men vulnerable and women protected? J Am Coll Cardiol Case Rep. 2020;2:1407–1410. doi: 10.1016/j.jaccas.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferdinand K.C., Nasser S.A. African-American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020;75:2746–2748. doi: 10.1016/j.jacc.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]