Abstract
Introduction
This study aims to quantify out-of-pocket spending associated with respiratory hospitalizations for conditions similar to those caused by coronavirus disease 2019 and to compare out-of-pocket spending differences among those enrolled in consumer-directed health plans and in traditional, low-deductible plans.
Methods
This study used deidentified administrative claims from the OptumLabs Data Warehouse (January 1, 2016–August 31, 2019) to identify patients with a respiratory hospitalization. It compared unadjusted out-of-pocket spending among consumer-directed health plan enrollees with that among traditional plan enrollees using difference of mean significance tests and repeated the analysis separately by age category and calendar year quarter. These data were collected on a rolling basis by OptumLabs and were analyzed in March 2020.
Results
Commercially insured consumer-directed health plan enrollees had significantly higher out-of-pocket spending than traditional plan enrollees, and these differences were largest among younger populations. The largest difference in out-of-pocket spending occurred during the first half of the year.
Conclusions
Consumer-directed health plan enrollees may experience differential financial burden from a hospitalization related to coronavirus disease 2019. Although some insurers are waiving cost-sharing payments for coronavirus disease 2019 treatment, self-insured employers remain exempt. As of now, policy responses may be insufficient to reduce the financial burden on consumer-directed health plans enrollees with respiratory hospitalizations related to coronavirus disease 2019.
INTRODUCTION
The U.S. is in the midst of a global health pandemic with high mortality and morbidity owing to respiratory illness.1 Coronavirus disease 2019 (COVID-19) can result in severe respiratory disease, including hospitalization. Hospitalizations and related treatments for COVID-19 are costly, complex, and could have a substantial impact on out-of-pocket (OOP) cost burden. Researchers at the University of Minnesota, Minneapolis, have aggregated data on hospitalizations and found that as of early May 2020, there have been 55,000 COVID-19 hospitalizations in the U.S. and the expectation is that hospitalization rates will continue to climb.2
Many individuals aged <65 years are enrolled in consumer-directed health plans (CDHPs),3 and an analysis of early COVID-19 hospitalizations found that 55% occurred among this age group.4 CDHPs generally feature high deductibles, requiring enrollees to pay for their healthcare OOP until they reach the deductible threshold. Congress has mandated that all cost sharing associated with the testing of COVID-19 be waived, and many insurers have agreed to waive cost sharing associated with the treatment.5 However, self-insured employers, representing nearly 60% of Americans with employer-sponsored insurance,6 are exempt from insurer-level commitments and allowed to opt out from waiving cost sharing on an employer-by-employer basis.5 Given the high cost of respiratory-related hospitalizations,7 , 8 COVID-19 may come with a significant financial burden among enrollees in CDHPs relative to those in traditional, low-deductible health plans.
METHODS
Using deidentified administrative claims from the OptumLabs Data Warehouse, patients enrolled in CDHPs and traditional plans from January 1, 2016 to August 31, 2019 were identified. These data were collected on a rolling basis by OptumLabs and analyzed in March 2020. CDHPs were defined as plans that were coupled with a tax-advantaged Health Savings Account or Health Reimbursement Account. Plans coupled with Health Savings Accounts were required by statue to have a high deductible (minimum of $1,300 during the study period). Plans coupled with Health Reimbursement Accounts generally featured high deductibles but were not required to do so. Traditional plans were not coupled with an account and had lower deductibles.
The unit of analysis was a unique respiratory hospitalization for conditions similar to those caused by COVID-19. Following the Centers for Disease Control and Prevention coding guidance,9 hospitalizations included pneumonia, acute bronchitis, lower respiratory infections, and acute respiratory distress syndrome. The sample was restricted to those aged <65 years in a commercial insurance plan and continuously enrolled in the same plan for 1 month before and 1 month after hospitalization.
The hospitalization-related spending measure summed all OOP spending (i.e., deductible payments, copayments, coinsurance payments) across all claims associated with the respiratory hospitalization. All spending was normalized to August 2019 dollars, and measures were trimmed at the 99th percentile separately for each plan group (CDHP versus traditional plan).
Unadjusted OOP spending for CDHP enrollees was compared with that of traditional plan enrollees using difference of mean significance tests, clustering SEs at the patient level to account for patients with multiple hospitalizations. This analysis was repeated separately by age category (0–21, 22–39, 40–55, 56–64 years) and by calendar year quarter. This research was determined to be exempt by the Johns Hopkins Bloomberg School of Public Health IRB.
Several sensitivity analyses were performed. Median spending was calculated, and Kolmogorov–Smirnov tests comparing median expenditures were performed. Next, spending was examined with different top-coding rules (no top coding, top coding at the 99th percentile across the whole sample). Finally, spending was examined for 3 potential comparator conditions (bone fractures, kidney stones, and poisoning).
RESULTS
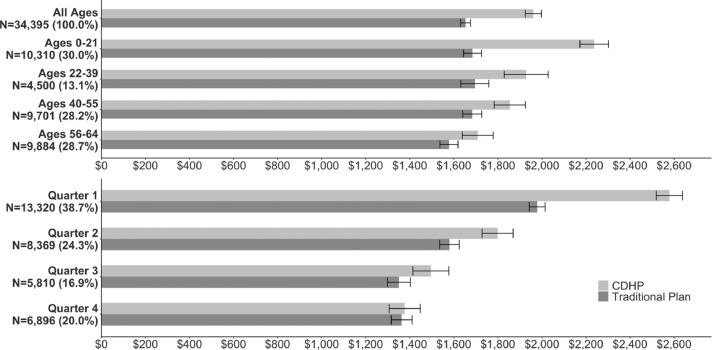
Average OOP spending for respiratory infection hospitalizations was $1,961 (95% CI=$1,924, $1,997) among enrollees in CDHPs and $1,653 (95% CI=$1,631, $1,676) among enrollees in traditional plans (Figure 1 ). This difference was largest for those aged 0–21 years, with CDHP enrollees spending $2,237 (95% CI=$2,172, $2,302) OOP and traditional plan enrollees spending $1,685 (95% CI=$1,644, $1,725) OOP. The difference in OOP spending between CDHP and traditional plan enrollees decreased as age increased, and those aged 56–64 years had the smallest difference, with CDHP enrollees spending $1,708 (95% CI=$1,639, $1,778) and traditional plan enrollees spending $1,578 (95% CI=$1,537, $1,619) OOP. Median differences across groups were slightly smaller, but statistical significance remained (Appendix Table 1, available online).
Figure 1.
Average OOP spending comparing CDHP and traditional plan enrollees with a respiratory-related hospitalization by age group and quarter of year.
Note: Analytic sample includes hospitalizations from January 1, 2016, through August 31, 2019, for individuals continuously enrolled for at least 1 month before and 1 month after the hospitalization. Costs are normalized to August 2019 dollars. Hospitalizations were for pneumonia, acute bronchitis, lower respiratory infections, and ARDS. CDHPs were defined as plans coupled with a Health Savings Account or Health Reimbursement Account. Traditional plans were defined as plans that were not coupled with an account. Note that some individuals may have had multiple hospitalizations.
ARDS, acute respiratory distress syndrome; CDHP, consumer-directed health plan; OOP, out-of-pocket.
Figure 1 also reports differences across the calendar year. The largest difference in OOP spending occurred during the first quarter of the year (January–March), with CDHP enrollees spending $2,578 (95% CI=$2,519, $2,638) and traditional plan enrollees spending $1,978 (95% CI=$1,943, $2,014) OOP. This difference persisted in the second quarter (April–June), with CDHP enrollees spending $1,798 (95% CI=$1,728, $1,869) and traditional plan enrollees spending $1,580 (95% CI=$1,536, $1,624) OOP. This difference continued to decrease in the third quarter (July–September) and was not significantly different by the fourth quarter of the year (October–December), with CDHP enrollees spending $1,377 (95% CI=$1,306, $1,447) and traditional plan enrollees spending $1,363 (95% CI=$1,316, $1,411) OOP.
Appendix Figure 1 (available online) reports several sensitivity analyses. The differences in OOP were similar for those who required the intensive care unit or a ventilator. In addition, the results did not qualitatively change with alternate top-coding rules. Hospitalizations for different conditions showed different baselines of OOP spending compared with respiratory hospitalizations but similar percentage differences between CDHP and traditional plans (respiratory: 19%, bone fracture: 21%, kidney stone: 13%, poisoning: 16%).
DISCUSSION
Overall, the findings suggest that financial strain associated with respiratory-related hospitalizations due to COVID-19 may fall disproportionately on CDHP enrollees. Commercially insured CDHP enrollees experiencing a respiratory hospitalization had substantially higher OOP spending than traditional plan enrollees, and these differences were largest among younger populations. The age-related differences are likely driven by the fact that younger individuals are, on average, healthier than older ones, meaning that younger individuals are less likely to exceed their deductible before a hospitalization.
There were larger differences between CDHP and traditional plan enrollees for those hospitalized during the first and second quarters of the year (January–June). Given the timing of the pandemic, hospitalizations related to COVID-19 are occurring early in the year when enrollees with CDHPs have likely not yet exceeded their deductibles. Given that many enrollees meet or exceed their deductible in the second half of the year, differences in OOP spending for CDHP enrollees may not be as large if the pandemic continues into or resurfaces in the fall. However, with many individuals currently delaying non-COVID–related care, many patients may not exceed their deductible by the fall.
Limitations
This study had several limitations. First, the analysis was observational and did not examine selection into CDHPs. Future research should examine these underlying mechanisms to understand the causes of the observed relationships. Second, the analysis measured past spending for all respiratory illnesses that mimic the symptoms of COVID-19. Given the severity of COVID-19‒related illness, the true OOP spending for patients with COVID-19 may be different.
CONCLUSIONS
Although many insurers have waived cost-sharing payments for COVID-19 treatment, self-insured employers remain exempt.5 Self-insured employers that have not waived cost-sharing payments for hospitalizations related to COVID-19 should consider doing so; for those that do not, federal policymakers should consider waiving cost sharing for those in self-insured plans, as some in Congress are debating.10 Though the findings highlight the importance of cost sharing for those enrolled in CDHPs, those in traditional plans were also exposed to potentially large OOP bills, suggesting that new policies should include all insurance products.
ACKNOWLEDGMENTS
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2020.05.008.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Branswell H, Joseph A. WHO declares the coronavirus outbreak a pandemic. Stat News. March 11, 2020.http://www.statnews.com/2020/03/11/who-declares-the-coronavirus-outbreak-a-pandemic/. Accessed March 20, 2020.
- 2.Carlson School of Management, University of Minnesota. COVID-19 hospitalization tracking project. Minneapolis, MN: Carlson School of Management, University of Minnesota.https://carlsonschool.umn.edu/mili-misrc-covid19-tracking-project. Published April 6, 2020. Accessed May 5, 2020.
- 3.Kaiser Family Foundation . Covered workers enrolled in an HDHP/HRA or HSA-Qualified HDHP. Kaiser Family Foundation; San Francisco, CA: 2018. Employer Health Benefits Survey: section 8: high-deductible health plans with saving option.http://www.kff.org/report-section/2018-employer-health-benefits-survey-section-8-high-deductible-health-plans-with-savings-option/ Published October 3, 2018Accessed March 20, 2020. [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albrecht L. Most major health insurers aren't charging patients for coronavirus treatment – but there's one big catch. Market Watch. May 11, 2020.http://www.marketwatch.com/story/most-major-health-insurers-arent-charging-patients-for-coronavirus-treatment-but-theres-one-big-catch-2020-05-01. Accessed May 11, 2020.
- 6.Fronstin P. Self-insured health plans: recent trends by firm size, 1996‒2018. Washington, DC: EBRI.http://www.ebri.org/publications/research-publications/issue-briefs/content/self-insured-health-plans-recent-trends-by-firm-size-1996-2018. Published August 1. 2019. Accessed May 4, 2020.
- 7.Thomas CP, Ryan M, Chapman JD. Incidence and cost of pneumonia in Medicare beneficiaries. Chest. 2012;142(4):973–981. doi: 10.1378/chest.11-1160. [DOI] [PubMed] [Google Scholar]
- 8.Rae M, Claxton G, Kurani N, McDermott D, Cox C. Pearson-KFF Health System Tracker; San Francisco, CA: 2020. Potential costs of COVID-19 treatment for people with employer sponsored coverage.http://www.healthsystemtracker.org/brief/potential-costs-of-coronavirus-treatment-for-people-with-employer-coverage/ Published March 13Accessed March 20, 2020. [Google Scholar]
- 9.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta, GA: 2020. ICD-10-CM official coding guidelines – supplement. Coding encounters related to COVID-19 coronavirus outbreak.http://www.cdc.gov/nchs/data/icd/ICD-10-CM-Official-Coding-Gudance-Interim-Advice-coronavirus-feb-20-2020.pdf Published February 20Accessed March 20, 2020. [Google Scholar]
- 10.American Medical Association . American Medical Association; Chicago, IL: 2020. Bill Requires ERISA plans to cover telehealth during COVID-19.http://www.ama-assn.org/practice-management/digital/bill-requires-erisa-plans-cover-telehealth-during-covid-19 Published April 30Accessed May 6, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.