Abstract
Background
Determining whether members follow guidelines, including guidelines prepared to help direct practice management during the coronavirus disease 2019 (COVID-19) pandemic, is an important goal for medical associations.
Objective
To determine whether practice of urologists is in line with guidelines for the management of common urological conditions during the COVID-19 pandemic produced by leading (inter)national urological associations.
Design, setting, and participants
Self-selected urologists completed a voluntary survey available online from March 27 to April 11, 2020 and distributed globally by the Société Internationale d’Urologie.
Outcome measurements and statistical analysis
Responses to two survey questions on the (1) management of 14 common urological procedures and (2) priority scoring of 10 common urological procedures were evaluated by practice setting and geographical region using chi-square and one-way analysis of variance analyses, respectively.
Results and limitations
There were 2494 respondents from 76 countries. Oncological conditions were prioritised over benign conditions, and benign conditions were deferred when feasible and safe. Oncological conditions with the greatest malignant potential were prioritised over less aggressive cancers. Respondents from Europe were least likely to postpone and most likely to prioritise conditions identified by guidelines as being of the highest priority. Respondents’ priority scoring of urological procedures closely matched the priorities assigned by guidelines. The main limitation of this study is that respondents were self-selected, and access to the survey was limited by language and technology barriers.
Conclusions
Prioritisation and management of urological procedures during the COVID-19 pandemic are in line with current guidelines. The greatest agreement was reported in Europe. Observed differences may be related to limited resources in some settings.
Patient summary
When deciding how best to treat patients during the coronavirus disease 2019 (COVID-19) pandemic, urologists are taking into account both expert recommendations and the availability of important local resources.
Keywords: Coronavirus, COVID-19, Guidelines, Pandemic, Practice management, Severe acute respiratory syndrome coronavirus 2, Urology
Take Home Message
Urologists worldwide have a high level of knowledge of coronavirus disease 2019 (COVID-19) guidelines for the management of urological conditions during the pandemic but may need to adapt their practices based on regional resource availability.
1. Introduction
Guidelines are developed through evaluation and synthesis of the best available data, ideally including available randomised controlled trials and meta-analyses, and ranked by quality of evidence. On rare occasions, however, practice-changing events occur that necessitate the provision of guidance to health care systems in the absence of data.
Such an event is the coronavirus disease 2019 (COVID-19) pandemic in 2020, which necessitated rapid practice change in order to minimise the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus among patients and health care workers, and to ensure that adequate resources are available to treat an unprecedented influx of COVID-19 patients. To provide guidance to health care professionals globally, medical associations prepared and disseminated guidelines for patients’ care rapidly during the COVID-19 pandemic. In the absence of data to guide decision making, these guidelines were developed based largely on expert consensus. The European Association of Urology (EAU) Guidelines Office commissioned a Rapid Reaction Group to facilitate the development of adapted guidelines to assist urologists internationally. The American Urological Association took a different approach and adopted the more general American College of Surgeons (ACS) guidelines.
We hypothesised that urologists worldwide have changed their patients’ management due to COVID-19. Our aim was to assess whether current practice is in line with the COVID-19 guidelines. This will clarify whether the present guidelines have practical utility in the clinical setting, as the pandemic may influence medical practice for months and possibly years. Such information can provide insight into the development of useful and effective guidelines for future pandemics and global emergencies.
2. Patients and methods
This study is an analysis of a survey developed and conducted by the Société Internationale d’Urologie (SIU). It includes multiple-choice questions about respondent demographics and general practice change in response to COVID-19, as well as questions about educational needs and concern about contracting COVID-19. These are reported separately because they represent different domains. This analysis specifically addresses responses to questions about the approach to and prioritisation of specific procedures (ie, questions 11 and 12). The full survey has been published [1] and is available as Appendix 1 at http://www.mdpi.com/2077-0383/9/6/1730/s1.
The survey was opened on March 27, 2020 and closed on April 11, 2020. It was administered online using the Aventri platform. The survey was distributed via e-mail to 15 252 contacts (members and nonmembers of SIU) from the SIU eNews mailing distribution list. No compensation was offered for its completion. All responses were anonymous.
In order to facilitate the analysis of the impact of COVID-19 on health care settings as it spread from east to west, respondents were grouped into the following regions: East/Southeast Asia and nearby regions, West/Southwest Asia and nearby regions, Europe, Africa, North America, and South America. The list of countries included in each region has been presented in another publication [1] and is available as Appendix 2 at http://www.mdpi.com/2077-0383/9/6/1730/s1.
To determine whether responses to the survey reflect currently available guidelines for adaptation of practice during the COVID-19 pandemic, several leading guidelines in English language were evaluated and summarised by key recommendations (Table 1, Table 2 ) [2], [3], [4], [5], [6], [7], [8], [9], [10].
Table 1.
Summary of EAU [2], BAUS [5], [6], [7], [8], [9], [10], and USANZ [4] guideline recommendations for prioritisation of nononcological urological proceduresa, b.
| EAU guidelines Priority (1) |
BAUS guidelines Stages (2) |
USANZ guidelines Urgent intervention (3) |
|
|---|---|---|---|
| Urodynamics | Low | 1 | Defer |
| BPH surgery | Low | 1 | Defer |
| Other benign conditionsc | Low | 1 | Defer |
| Removal of a double-J stent | Low to Intermediate based on double-J–related symptoms | Delay if possible | Defer |
| Stone management (without infection) | From low to high based on symptoms | 1 (Elective URS and PCNL) 3 (URS with stent or ureteric stones) |
For symptomatic stones |
| Cystoscopy | Macroscopic haematuria: high F/U without haematuria: from Low to intermediate based on risk group |
1 | F/U for high-risk group Diagnostic when abnormal radiology or abnormal cytology |
ACS = American College of Surgeons; BAUS = British Association of Urological Surgeons; BPH = benign prostatic hyperplasia; EAU = European Association of Urology; F/U = follow-up; PCNL = percutaneous nephrolithotomy; TVT = tension-free vaginal tape; URS = ureteroscopy; USANZ = Urological Society of Australia and New Zealand.
ACS guidelines are not included because they did not refer to specific procedures.
1—EAU priorities: low, clinical harm very unlikely if postponed for 6 mo; intermediate, not recommended to postpone for >3 mo; high, the last to cancel, prevent delay of >6 wk; emergency, cannot be postponed for >24 h. 2—BAUS stages: 1, first cancellations; 2, secondary cancellations; 3, last to be cancelled; 4, emergency cases only. 3—USANZ priorities: conditions that may warrant urgent surgical intervention; conditions not proposed were considered deferrable.
Varicocele, hydrocele, circumcision, TVTs, etc.
Table 2.
Summary of EAU [2], BAUS [5], [6], [7], [8], [9], [10], and USANZ [4] guideline recommendations for prioritisation of oncological urological proceduresa, b.
| EAU guidelines priority (1) |
BAUS guidelines Stages (2) |
USANZ guidelines Urgent intervention (3) |
|
|---|---|---|---|
| TUR of bladder tumour | From low to high based on haematuria and risk group | 2 (low risk) 3 (high risk) |
High-risk group |
| Radical cystectomy | Intermediate | 2 (low risk) 3 (high risk) |
Urgent (ideally prior neoadjuvant chemotherapy and delay in surgery after discussion with medical oncologists) |
| Nephroureterectomy | High for high-risk patients | 2 (low risk) 3 (high risk) |
Urgent (consider neoadjuvant chemotherapy) |
| Prostatic biopsy | From low to high based on risk for PCa | 1 (GA transperineal) 2 (LA transperineal for high PSA) |
Only for suspicious prostate lesions or PIRADS 4/5 on prior MRI |
| Radical prostatectomy (localised PCa) | Intermediate but can be postponed until after pandemic | Defer new patients 2 (RARPs) |
Only for a proportion of high-risk PCa patients |
| Radical/partial nephrectomy | From low to high based on clinical stage | 1 (partial) 3 (time sensitive) |
For large RCCs >7 cm, or complicated with venous thrombus |
| Radical orchidectomy/penectomy | Emergency | 3 | Urgent |
| RPLND | High | Defer and offer chemotherapy | Urgent (deferral if suggestive of slowly growing mature teratoma) |
ACS = American College of Surgeons; BAUS = British Association of Urological Surgeons; EAU = European Association of Urology; GA = general anaesthetic; LA = local anaesthetic; MRI = magnetic resonance imaging; PCa = prostate cancer; PIRADS = Prostate Imaging Reporting and Data System; PSA = prostate-specific antigen; RARP = robot-assisted radical prostatectomy; RCC = renal cell carcinoma; RPLND = retroperitoneal lymph node dissection; TUR = transurethral resection; USANZ = Urological Society of Australia and New Zealand.
ACS guidelines are not included because they did not refer to specific procedures.
1—EAU priorities: low, clinical harm very unlikely if postponed for 6 mo; intermediate, not recommended to postpone for >3 mo; high, the last to cancel, prevent delay of >6 wk; emergency, cannot be postponed for >24 h. 2—BAUS stages: 1, first cancellations; 2, secondary cancellations; 3, last to be cancelled; 4, emergency cases only. 3—USANZ priorities: conditions that may warrant urgent surgical intervention; conditions not proposed were considered deferrable.
2.1. Statistical analysis
Participants indicated whether they manage each of 14 common urological procedures by postponing it, performing it as in the past, using an alternative technique (eg, minimally invasive procedure, chemotherapy, or radiotherapy), including it in the surgical priority list, or referring it to another centre. Omnibus chi-square tests were used to compare whether the management of these 14 procedures varied among geographical regions and practice settings. The statistical significance threshold for these analyses was Bonferroni corrected for multiple comparisons, yielding a critical alpha threshold of 0.004.
Statistically significant differences of clinical interest were further explored by calculating, for each cell in each contingency table, its adjusted standardised residual. Conceptually, these are the Z-transformed differences between the expected percentage for that cell under the null hypothesis and the observed percentage [11]. By examining the adjusted standardised residuals, we determined which observed cells showed a higher/lower percentage than expected. The statistical significance threshold for the adjusted standardised residuals within each contingency table was Bonferroni corrected for the number of residuals calculated within that table; this yielded a threshold of Z = 2.94 (corresponding to an alpha of 0.003) for each procedure crossed with the practice setting factor and a threshold of Z = 3.14 (corresponding to an alpha of 0.002) for each procedure crossed with the region factor.
Participants also rated the priority of 10 common urological procedures on a scale of 1 (lowest priority) to 10 (highest priority). Omnibus one-way analyses of variance (ANOVAs) and follow-up pairwise comparisons were used to compare the priority ratings of these 10 procedures among geographical regions and practice settings. The one-way ANOVAs were Bonferroni corrected for multiple comparisons, yielding an adjusted alpha level of 0.005. The pairwise comparisons within each one-way ANOVA were also Bonferroni corrected, yielding alpha thresholds of 0.017 for comparisons within the practice setting and 0.003 for comparisons within a region. Analysis was conducted using SPSS version 26.0 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Management of common urological conditions
A total of 2494 urologists from 76 countries completed the survey. The response rate was 16.35%. Although this was a self-selected, nonrepresentative, nonprobability sample, the large number of participants and their representation from around the world allows us to draw inferences about urologists broadly.
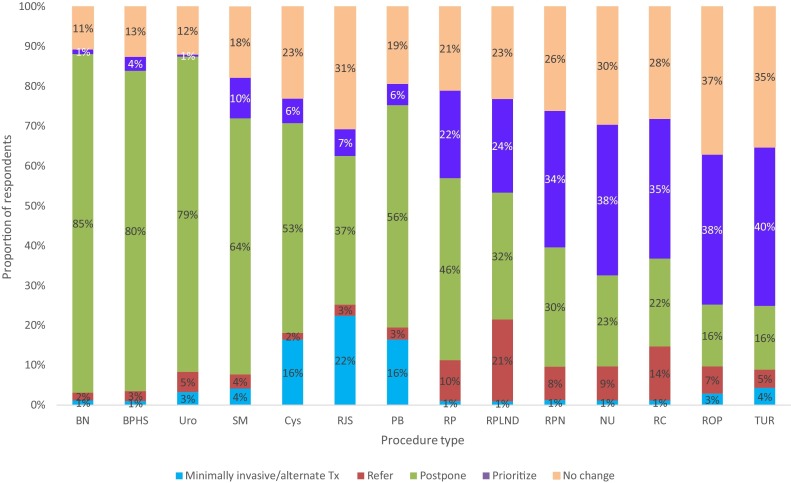
As seen in Figure 1 , nononcological procedures (ie, benign conditions, surgery for benign prostatic hyperplasia [BPH], urodynamics, stone management, and cystoscopy) were postponed or managed via alternative options more often than oncological procedures (ie, prostatic biopsy, radical prostatectomy, retroperitoneal lymph node dissection [RPLND], radical/partial nephrectomy, nephroureterectomy, radical cystectomy, radial orchidectomy/penectomy, and bladder tumour transurethral resection [TUR]). This approach is in line with the (inter)national guideline recommendations.
Fig. 1.
Approach to the management of common urological procedures in the time of COVID-19.
BN = benign conditions; BPHS = surgery for benign prostatic hyperplasia; COVID-19 = coronavirus disease 2019; Cys = cystoscopy; NU = nephroureterectomy; PB = prostatic biopsy; RC = radical cystectomy; RJS = removal of double-J stent; ROP = radial orchidectomy/penectomy; RP = radical prostatectomy; RPLND = retroperitoneal lymph node dissection; RPN = radical/partial nephrectomy; SM = stone management (no infection); TUR = transurethral resection for bladder tumour; Tx = treatment; Uro = urodynamics.
Chi-square analyses revealed significant variations in response for each procedure by geographic region at p < 0.001 (see Supplementary Table 1). Follow-up examinations of the adjusted standardised residuals revealed that respondents from East/Southeast Asia consistently reported higher than expected rates of no change for all procedures. In contrast, Europeans had low rates of no change for prostatic biopsy, cystoscopy, urodynamics, BPH surgery, and management of kidney stones and benign conditions.
Respondents from Europe reported higher than expected rates of postponement for procedures designated by guidelines to be of low priority (ie, all nononcological conditions except for removal of a double-J stent).
For seven of 14 procedures designated as higher priority by guidelines (ie, cystoscopy, bladder tumour TUR, nephrectomy, nephroureterectomy, cystectomy, radial orchidectomy/penectomy, and RPLND), Europeans reported lower than expected rates of postponement and higher than expected rates of inclusion on the priority list (data not shown).
For RPLND, referrals to dedicated centres were reported at higher than expected rates in Europe and at lower rates in North and South America.
Although there were a number of statistically significant differences by practice setting, these were deemed to be not of theoretical interest and are not discussed further.
3.2. Prioritisation of common urological conditions
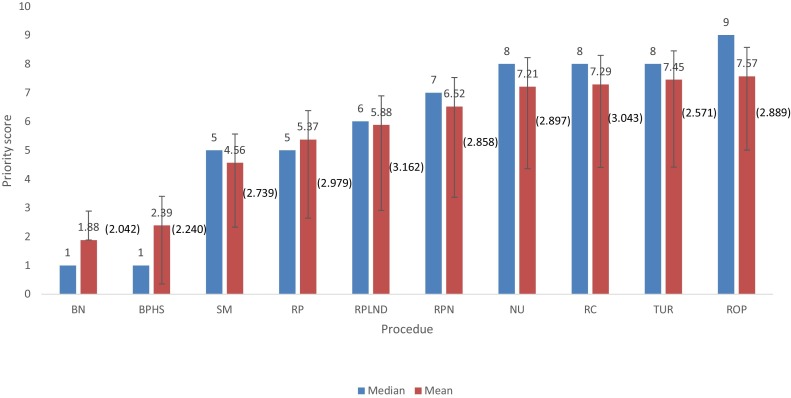
Figure 2 demonstrates the median and mean priority scores given to each of the 10 common urological procedures by respondents. Table 3 lists the rank order priority of each procedure, from 1 (most important) to 10 (least important), among respondents overall as well as by region and practice setting.
Fig. 2.
Median and mean (SD) priority scores of common urological procedures in the time of COVID-19. Rating scale: 1–10; 1 = lowest priority, 10 = highest priority.
BN = benign conditions; BPHS = surgery for benign prostatic hyperplasia; COVID-19 = coronavirus disease 2019; NU = nephroureterectomy; RC = radical cystectomy; ROP = radial orchidectomy/penectomy; RP = radical prostatectomy; RPLND = retroperitoneal lymph node dissection; RPN = radical/partial nephrectomy; SD = standard deviation; SM = stone management (no infection); TUR = transurethral resection for bladder tumour.
Table 3.
Rank order of priority for common urological procedures at the time of COVID-19 by regiona.
| Procedure | Total (N = 2494) |
Region |
Practice setting |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Africa (n = 209) |
E/SE Asia (n = 441) |
Europe (n = 1074) |
North America (n = 186) |
South America (n = 198) |
W/SW Asia (n = 386) |
Academic (n = 1161) |
Private (n = 719) |
Public (n = 614) |
||
| Other benign conditionsb | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| BPH surgery | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Stone management | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Radical prostatectomy (localised PCa) | 4 | 5 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| RPLND | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Radical/partial nephrectomy | 6 | 6 | 6 | 6 | 6 | 6 | 7 | 6 | 6 | 6 |
| Nephroureterectomy | 7 | 9 | 9 | 8 | 7 | 7 | 8 | 8 | 7 | 7 |
| Radical cystectomy | 8 | 8 | 8 | 9 | 8 | 8 | 6 | 9 | 8 | 8 |
| TUR of bladder tumour | 9 | 10 | 10 | 7 | 9 | 9 | 10 | 7 | 10 | 9 |
| Radical orchidectomy/penectomy | 10 | 7 | 7 | 10 | 10 | 10 | 9 | 10 | 9 | 10 |
BPH = benign prostatic hyperplasia; COVID-19 = coronavirus 2019; E/SE = East/Southeast; PCa = prostate cancer; RPLND = retroperitoneal lymph node dissection; TUR = transurethral resection; W/SW = West/Southwest.
Rank order from 1 to 10: 1 = lowest priority; 10 = highest priority.
varicocele, hydrocele, circumcision, TVTs, etc.
Surgeries for benign conditions were ranked lowest in priority, followed by BPH and management of stone conditions not associated with infection. These are in line with the guideline recommendations presented in Table 1, Table 2, which indicate that nononcology procedures should be deferred, with lithiasis considered to be of higher priority than BPH, depending on clinical circumstances.
Among the oncological procedures, radical prostatectomy was given the lowest priority. This is also in line with guidelines, which indicate that this surgery should be given priority only for high-risk patients.
Notable regional differences were observed for radical cystectomy (F 5,2192 = 39.766; p < 0.001), nephroureterectomy (F 5,2281 = 29.113; p < 0.001), TUR for bladder tumour (F 5,2348 = 11.009; p < 0.001), and radical orchidectomy/penectomy (F 5,2281 = 30.172; p < 0.001). There were no significant differences by practice setting.
When each procedure is placed in rank order of priority by region (Table 3), radical cystectomy was rated as lower priority in West/Southwest Asia than in other regions. In Europe, North America, and South America, orchidectomy was given the highest priority, which is in line with all the guidelines, but this was not the case in Asia or Africa. Nephroureterectomy was ranked higher in Africa and South/Southeast Asia than in other regions. TUR of bladder tumour received a lower priority rating in Europe as well as in the academic setting.
Follow-up pairwise statistical analyses revealed a significantly lower mean priority score for radical cystectomy in West/Southwest Asia than in all other regions (p ≤ 0.003 for all comparisons). Priority scores for orchidectomy were significantly higher in Europe and South America, than in Africa and both Asian regions (p < 0.001 for all comparisons). In North America, it was ranked significantly higher than East/Southeast Asia (p = 0.001).
Among the 10 procedures listed on the survey, respondents in each region ranked RPLND as moderate priority despite the fact that the EAU categorises this as high priority and Urological Society of Australia and New Zealand (USANZ) as urgent. Only British Association of Urological Surgeons (BAUS) guidelines recommend conducting chemotherapy and deferring the procedure.
4. Discussion
The provision of evidence-based care is the cornerstone of health care systems worldwide. Practice guidelines, prepared by recognised experts and published by leading professional associations, form the backbone of efforts to provide this.
The urological community became rapidly aware that available practice guidelines lacked relevance during the pandemic crisis. In response, many urology societies and associations developed COVID-19 guidelines, out of necessity, in the absence of objective evidence. These new guidelines aim to provide tools to facilitate decision making that minimise the risk for both health care professionals and patients. They also provide a blueprint for future development of robust guidelines that address the present and future crisis situations.
The most important finding from the present survey is the confirmation of global validity of the COVID-19 guidelines prepared by different (inter)national societies through consensus and supported by the best knowledge available.
The recommendations for prioritisation by different guideline bodies have certain subtle nuances but, in the vast majority of cases, offer the same recommendations (Table 1, Table 2). These differences may be related to resource limitations in local settings (eg, availability of blood products, intensive care unit [ICU] beds, alternative treatment methods, and operating room access) and infrastructure.
Overall, responses indicate that current practice matches with current COVID-19 guidelines, with aggressive malignancies prioritised, less aggressive cancers deferred or managed using alternative strategies (when possible), and benign procedures postponed (unless this is likely to cause harm) or treated by alternative means (Fig. 1). Notably, alternative options are more readily available for benign conditions (eg, double-J stent removal in operative setting can be deferred in the outpatient setting under local anaesthesia).
Among all the regions, Europe appears to be following the guidelines most closely. This region reported the highest rates of postponement of procedures categorised as low priority by guidelines and the lowest rate of postponement of procedures designated as high priority or urgent. For cystoscopy, bladder tumour TUR, nephrectomy, nephroureterectomy, cystectomy, radial orchidectomy/penectomy, and RPLND, all of which are designated as high priority by guidelines, Europeans were less likely to postpone and more likely to place these on the surgical priority list than respondents from other regions. Referral to dedicated centres for RPLND was also reported most often in Europe. On the contrary, in East/Southeast Asia where the pandemic is furthest along, participants were most likely to report that procedures are being conducted as before, suggesting that their health care systems are returning to pre–COVID-19 states.
The second survey question, in which respondents rated how common urological procedures should be prioritised, addresses their level of knowledge of current guidelines, since it reflects their view of how these conditions should be prioritised.
Our results indicate global unanimity that benign conditions are of the lowest priority (Fig. 2). In addition, nephroureterectomy, cystectomy, and bladder tumour TUR were scored as high priority by respondents in all regions. These are all treatments for transitional cell carcinomas, which are known to have a high malignant potential and may incur suboptimal outcomes if treatments are delayed. This is reflected in all guidelines that recognise these procedures as urgent/high priority, particularly for high-risk patients. In contrast, procedures for prostate cancer and renal cell carcinoma were rated as moderate priority, as good outcomes can still be achieved with management other than surgical resection (eg, active surveillance, medical therapy, radiation) in appropriately selected patients. Respondents’ prioritisation scores are in line with available COVID-19 guidelines.
It is striking that the Asian regions and Africa did not rank orchidectomy as the highest-priority procedure, despite the fact that this is what all guidelines recommend and the fact that this procedure can be performed without the need for blood transfusion, prolonged hospitalisation, or ICU stay.
In all regions, RPLND was rated as moderate priority despite being given high priority by all guidelines except those of BAUS (Table 2). The potential reasons for the need for transfusion or ICU stay can contribute to this finding, as both are resources that may be limited during a pandemic. EAU and ACS guidelines recommend that hospitals and surgical centres consider their logistic capability to meet patients’ needs when prioritising surgeries.
As for the benign conditions, stone treatment is prioritised over BPH management. This is in line with the new COVID-19 guidelines and underscores a higher potential threat from stone disease, than from voiding complaints, to the safety of patients.
Guidelines cannot address differences in practice between urologists working in academic, public, or private settings. It is reassuring that there is no difference by practice setting when prioritising for the different benign and malignant conditions (Table 3). The same is true for regional differences. Overall, there is a striking level of agreement in prioritising different surgical procedures, either benign or malignant.
The question remains “when or will ever practice normalise?” Once they do, an enormous backlog of patients deferred during the current triage must be addressed. Can these novel COVID-19 guidelines continue to be used until conditions normalise or will transition guidelines be made?
This study has several limitations. It included self-selected, nonrepresentative, and nonrandom participants from all around the world. At the time of survey, regions/countries were at varying phases of the pandemic that might result in differences in terms of speed of action of adopted measures and strategies. The strength of this survey is that it represents a global and timely snapshot of the current situation in line with the proposed COVID-19 guidelines. Upon normalisation of conditions, there will be no opportunity to confirm the validity of the guidelines in another format.
5. Conclusions
Urologists’ priority rankings for common urological procedures are in line with the most commonly used guidelines for the management of urological patients during the pandemic. Actual practice also seems to be in agreement with guideline recommendations. Deviations from the guidelines likely reflect regional differences in resources. EAU and ACS guidelines recommend prioritising surgeries based on local resource availability, so these practices can be interpreted not as a failure to implement guidelines but as a reflection of local adaptation to individual circumstances. Respondents from Europe reported the highest agreement with guideline recommendations.
Author contributions: Stavros Gravas had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Gravas, Bolton, Gomez, Klotz, Kulkarni, Tanguay, de la Rosette.
Acquisition of data: Gravas, Fournier, Oya, Summerton, Scarpa, Chlosta, Gkialas, Xie, Rasyid, Bolton, Gomez, Klotz, Kulkarni, Tanguay, de la Rosette.
Analysis and interpretation of data: Gravas, de la Rosette.
Drafting of the manuscript: Gravas, de la Rosette.
Critical revision of the manuscript for important intellectual content: Fournier, Oya, Summerton, Scarpa, Chlosta, Gkialas, Xie, Rasyid, Bolton, Gomez, Klotz, Kulkarni, Tanguay.
Statistical analysis: None.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: Gravas, de la Rosette.
Other: None.
Financial disclosures: Stavros Gravas certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: The SIU did not receive external funding for this study.
Acknowledgements: The authors would like to acknowledge support from SIU Central Office, including Merveille de Souza, Carrie Thompson, Melissa St-Onge, Susie Petrusa, Christine Albino, as well as the contributions of Alison Palkhivala for medical writing and editorial support, and Michael Barlev for statistical support.
Associate Editor: Malte Rieken
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euf.2020.06.006.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Gravas S., Bolton D., Gomez R. Impact of COVID-19 on urology practice: a global perspective and snapshot analysis. J Clin Med. 2020;9:1730. doi: 10.3390/jcm9061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ribal M.J., Conford P., Birganti A., the European Association of Urology Guidelines Office Rapid Reaction Group An organisation-wide collaborative effort to adapt the EAU guidelines recommendations to the COVID -19 era. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.04.056. Online ahead of print, S0302-2838(20)30324-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Surgeons. COVID-19 guidelines for triage of urology patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/urology.
- 4.Urological Society of Australia and New Zealand. Urological prioritisation during COVID-19. March 25, 2020. https://usanz.org.au/publicassets/3fdf1dd5-5d6e-ea11-90fb-0050568796d8/Pol-020-Guidelines-Urol-Prioritisation-During-COVID-19--25-3-2020.pdf.
- 5.British Association of Urological Surgeons. COVID-19 strategy for the interim management of prostate cancer prepared by the BAUS section of oncology. March 19, 2020. https://www.baus.org.uk/_userfiles/pages/files/professionals/sections/oncology/COVID-19%20BAUS%20Oncology%20Prostate%20final.pdf.
- 6.British Association of Urological Surgeons. COVID-19 strategy for the interim management of penile cancer Prepared by the BAUS sections of oncology & andrology. March 25, 2020. https://caunet.org/wp-content/uploads/2020/04/BAUS-Oncology-COVID-19-Penis.pdf.
- 7.British Association of Urological Surgeons. COVID-19 strategy for the interim management of testicular cancer prepared by the BAUS section of oncology. Updated April 14, 2020. https://www.bopa.org.uk/resources/covid-19-strategy-for-the-interim-management-of-testicular-cancer-prepared-by-the-baus-section-of-oncology/.
- 8.British Association of Urological Surgeons. COVID-19 bladder cancer contingency plan prepared by the BAUS section of oncology. March 19, 2020. https://www.baus.org.uk/_userfiles/pages/files/professionals/sections/oncology/COVID-19%20BAUS%20Oncology%20Bladder%20final.pdf.
- 9.British Association of Urological Surgeons. COVID-19 strategy for the interim management of kidney cancer prepared by the BAUS section of oncology. March 19, 2020. https://www.baus.org.uk/_userfiles/pages/files/professionals/sections/oncology/COVID-19%20BAUS%20Oncology%20Kidney%20final.pdf.
- 10.British Association of Urological Surgeons. BAUS guidance on urological laparoscopy and robotic-assisted laparoscopic surgery during the COVID-19 pandemic. March 30, 2020. https://caunet.org/wp-content/uploads/2020/04/BAUS-Guidance-on-Laparoscopy-v1.pdf.
- 11.Agresti A. ed. 3. Wiley-Interscience; Hoboken, NJ: 2013. Categorical Data Analysis. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.