Abstract
The Cambie proposition is the American individualistic one: If I can afford to pay for quick access to care, then that should be my right. It denies any concept of universalism, of the common good or that your rights might adversely impact my rights and my healthcare experience. Some private care proponents offer the magical prospect that this quicker access for the wealthy few has no impact on access for the many. It is even sometimes perversely argued that if the wealthy pay for access outside the public health system, that reduces demand for public care, freeing up space for others and, hey presto, magically everyone benefits from the increase in inequality. The Australian experience is that this magic does not work.
Abstract
Le point de vue de Cambie correspond à l'approche individualiste des États-Unis: si j'ai les moyens de payer pour un accès plus rapide aux soins de santé, je devrais en avoir le droit. Ce point de vue fait fi de tout concept d'universalité, du bien commun et du fait que les droits de l'un peuvent affecter négativement les droits et services pour autrui. Certains défenseurs des services privés affirment magiquement que l'accès accéléré des mieux nantis n'a aucun impact pour les autres. On affirme même parfois que si les mieux nantis paient pour un accès en dehors du système public de santé, cela réduit la demande, libérant ainsi des places pour les autres et, comme par magie, tout le monde profite de cet accroissement des inégalités. L'expérience australienne montre que la magie ne fonctionne pas.
The Australian System in Brief
Hospital care in Australia involves a mix of public and private funding and public and private provision. About 45% of the population has private insurance for some level of hospital care, with private insurance subsidized by the government for people with lower to middle incomes (Duckett and Cowgill 2019). In parallel, all Australians have access to public hospital care under the public universal scheme, Medicare.
Private health insurance is a major funding source for private hospitals, accounting for about 50% of private hospital revenue. The Commonwealth government subsidies for private health insurance, paid through insurers, account for a further 18% of private hospital income (Figure 1).
Figure 1.
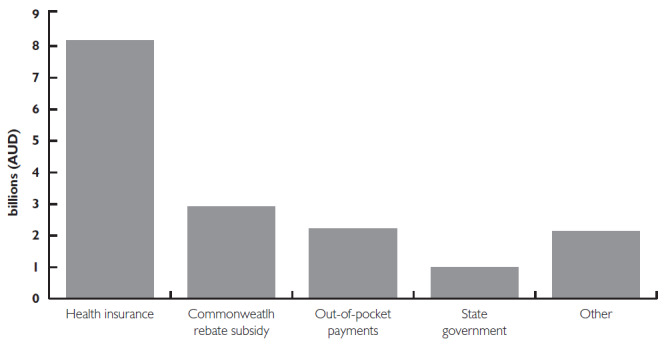
Private health insurance funds about half of private hospital expenditure
Note: Data show private hospital expenditure from 2017 to 2018 (billion AUD)
About 40% of all hospital admissions are to private hospitals, as are about 60% of all surgical admissions (Duckett and Nemet 2019). Private hospitals mainly focus on elective procedures – less than 1% of emergency admissions are to private hospitals, and these admissions account for only around 0.5% of all admissions to private hospitals. Most elective procedures are undertaken in private hospitals.
Public hospitals are more evenly distributed across Australia. There are a few private hospitals in rural and remote areas, and private hospitals are more common in wealthier suburbs where private insurance is more prevalent. Academic medicine is mostly concentrated in public hospitals, and most complex care (such as major trauma, advanced cancer care and organ transplantation) is only undertaken in public hospitals.
The relationship between public and private funding and care is complex. Private hospitals engage in cream skimming, focusing on patients with lower complexity on average (Cheng et al. 2015). Public hospitals may welcome this: Overburdened public hospitals willingly transfer insured patients with less complex needs or those who are in their recuperative phase to private hospitals. Public hospitals receive patient transfers from private hospitals where something has gone wrong (Brameld et al. 2006; Cheng et al. 2015), a hidden cross-subsidy from public hospitals to private hospitals.
There has been no coherence or consistency in the rhetoric about the roles of the two systems or the basis for public subsidies for private insurance (Duckett and Nemet 2019). Policy makers at various times have suggested that private care substitutes for public care, that it complements public care, that Medicare is a universal scheme or that Medicare is a residual scheme. The lack of clarity means that the policy on both public and private health insurance and private healthcare is an incoherent mess.
Creation of a large private sector weakens planning and system integration. Private hospitals operate autonomously and do not have to cooperate with the public sector.
The Australian experience is that a large private sector changes the dynamics of public policy. Rather than pursuing policies to ensure that the public system can meet demand, alternative policies to subsidize the private sector come to the fore and become entrenched and difficult to unwind. With almost half the population having private health insurance, the political dynamic is that the Labor Party, who might otherwise be more skeptical of the value of health insurance, cannot afford to alienate such a large proportion of the population. Labor knows that if it were to signal a policy of withdrawing subsidies, it would be vehemently opposed by insurers who would attempt to mobilize their contributors against such a policy.
The overwhelming academic evidence is that Australia's A$6 billion annual subsidy to private health insurance subsidies is not value for money (Cheng 2013, 2014; Colombo and Tapay 2004; Doiron and Kettlewell 2018; Frech and Hopkins 2004; Lu and Savage 2006; Vaithianathan 2002). If this annual subsidy is abolished, the cost of additional demand in the public sector would be less than the current subsidies. Despite this, no major political party will challenge the industry.
Private Care, Public Waiting
The evidence suggests that, contrary to what is often argued, relatively more private provision in Australia is associated with prolonged, not shortened, waiting (Duckett 2005, 2018). Waiting times in Australia's mixed public–private system are longer than in Canada's all-public system (McDonald and Duckett 2020).
The direction of causation could be hypothesized to go in either direction: Longer waits in the public sector create a demand for private care (the Cambie argument) or private care thrives by stifling public provision, thus creating longer waits, and this is enabled by “dual practice,” surgeons working in both the public and private sectors.
The former hypothesis assumes that public and private care are substitutes – that increases in private admissions reduce demand in the public sector. This is not always the case, partly because thresholds for admission to private hospitals are lower than those for public hospitals, and there is more low-value care in private hospitals (Badgery-Parker et al. 2019; Chalmers et al. 2019).
The latter hypothesis has two foci: The first, ascribing nefarious motives to surgeons – that they personally inflate waiting times in the public sector to encourage patients to shift to private care (Ferrinho et al. 2004).
The second, a more benign reason why undersupply of public care occurs alongside additional private care, is medical workforce limitations. Many surgeons practice in both the public and private hospitals. Surgeons generally receive high levels of remuneration in private hospitals (where they are paid on a fee-for-service basis) compared to public hospitals (where they are often paid on a salaried or a part-time salary basis). Fee-for-service remuneration yields greater payment per hour than salary payments.
Given the limitations on the supply of surgeons, expansion of demand for private care will often result in a reduction in availability of surgical time in the public sector (Cheng et al. 2013a; Cheng et al. 2013b; Cheng et al. 2015). This dynamic aspect of the public–private interface is often ignored by advocates of expanding private care, who implicitly assume that surgical time is infinitely elastic.
Conclusion
The evidence from Australia suggests that the community will not benefit from an expansion of private funding. The mixed public–private funding and provision has had a deleterious effect on the Australian hospital system.
In contrast to the claims by proponents (Flood et al. 2020), increased private provision does not lead to improved access to public care to any significant extent, nor does it reduce waiting times. It does, however, allow higher incomes for doctors and provides business opportunities for investors in private hospitals.
References
- Australian Institute of Health and Welfare. 2019, September 25 Health Expenditure Australia 2017–18 (Cat no. HWE 77, Canberra: AIHW). Retrieved May 2, 2020. <https://www.aihw.gov.au/reports/health-welfare-expenditure/health-expenditure-australia-2017-18/contents/summary>.
- Badgery-Parker T., Pearson S.-A., Chalmers K., Brett J., Scott I.A., Dunn S. et al. 2019. Low-Value Care in Australian Public Hospitals: Prevalence and Trends over Time. BMJ Quality and Safety 28(3): 205–14. 10.1136/bmjqs-2018-008338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brameld K., Holman D., Moorin R. 2006. Possession of Health Insurance in Australia – How Does It Affect Hospital Use and Outcomes? Journal of Health Services and Research Policy 11(2): 94–100. 10.1258/135581906776318901. [DOI] [PubMed] [Google Scholar]
- Chalmers K., Badgery-Parker T., Scott I.A., Pearson S.-A., Brett J., Elshaug A.G. 2019. Measuring 21 Low-Value Hospital Procedures: Claims Analysis of Australian Private Health Insurance Data (2010–2014). BMJ Open 9(3): e024142. 10.1136/bmjopen-2018-024142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng T.C. 2013, July Does Reducing Rebates for Private Health Insurance Generate Cost Savings? Melbourne Institute Policy Briefs Series – Policy Brief No. 3/13. Retrieved May 2, 2020. <https://melbourneinstitute.unimelb.edu.au/__data/assets/pdf_file/0010/2168182/pb2013n03.pdf>.
- Cheng T.C. 2014. Measuring the Effects of Reducing Subsidies for Private Insurance on Public Expenditure for Health Care. Journal of Health Economics 33: 159–79. 10.1016/j.jhealeco.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Cheng T.C., Joyce C.M., Scott A. 2013a. An Empirical Analysis of Public and Private Medical Practice in Australia. Health Policy 111(1): 43–51. 10.1016/j.healthpol.2013.03.011. [DOI] [PubMed] [Google Scholar]
- Cheng T.C., Kalb G.R.J., Scott A. 2013b. Public, Private or Both? Analysing Factors Influencing the Labour Supply of Medical Specialists Working Paper 40/13. Melbourne Institute. 10.2139/ssrn.2364168. [Google Scholar]
- Cheng T.C., Haisken-DeNew J.P., Yong J. 2015. Cream Skimming and Hospital Transfers in a Mixed Public–Private System. Social Science and Medicine 132: 156–64. 10.1016/j.socscimed.2015.03.035. [DOI] [PubMed] [Google Scholar]
- Colombo F., Tapay N. 2004. Private Health Insurance in OECD Countries: Benefits and Costs for Individuals and Health Systems. OECD Health Working Papers 15. OECD; Retrieved May 2, 2020. <https://www.oecd.org/els/health-systems/33698043.pdf>. [Google Scholar]
- Doiron D., Kettlewell N. 2018. The Effect of Health Insurance on the Substitution between Public and Private Hospital Care. Economic Record 94(305): 135–54. 10.1111/1475-4932.12394. [Google Scholar]
- Duckett S. 2005. Private Care and Public Waiting. Australian Health Review 29(1): 87–93. 10.1071/AH050366. [DOI] [PubMed] [Google Scholar]
- Duckett S. 2018. Coercing, Subsidising and Encouraging: Two Decades of Support for Private Health Insurance. In Cahill D., Toner P., eds., Wrong Way: How Privatisation and Economic Reform Backfired (pp. 40–58). La Trobe University Press. [Google Scholar]
- Duckett S., Cowgill M. 2019, December 3 Saving Private Health 2: Making Private Health Insurance Viable. Grattan Institute; Retrieved May 2, 2020. <https://grattan.edu.au/report/saving-private-health-2/>. [Google Scholar]
- Duckett S., Nemet K. 2019, July 15 The History and Purposes of Private Health Insurance. Grattan Institute; Retrieved May 2, 2020. <https://grattan.edu.au/report/the-history-of-private-health-insurance/>. [Google Scholar]
- Ferrinho P., Lerberghe W.V., Fronteira I., Hipólito F., Biscaia A. 2004. Dual Practice in the Health Sector: Review of the Evidence. Human Resources for Health 2(14). 10.1186/1478-4491-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flood C.M., Thomas B., White K. 2020. The Courts and Two-Tier Medicare. Healthcare Policy 15(4): 13–20. 10.12927/hcpol.2020.26229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frech H.E., Hopkins S. 2004. Why Subsidise Private Health Insurance. Australian Economic Review 37(3): 243–56. 10.1111/j.1467-8462.2004.00327.x. [Google Scholar]
- Lu M., Savage E. 2006. Do Financial Incentives for Supplementary Private Health Insurance Reduce Pressure on the Public System? Evidence from Australia. Working Papers 2006/11. CHERE, University of Technology. [Google Scholar]
- McDonald F., Duckett S. 2020. Embracing Private Finance and Private Provision: The Australian System. In Flood C.M., Thomas B., eds., Is Two-Tier Health Care the Future? (pp. 267–92). University of Ottawa Press. [Google Scholar]
- Vaithianathan R. 2002. Will Subsidising Private Health Insurance Help the Public Health System? The Economic Record 78(242): 277–83. 10.1111/1475-4932.00057. [Google Scholar]


