Abstract
We surveyed Canadian healthcare experts to identify policies to address antimicrobial resistance (AMR) in Canada between 2008 and 2018. Respondents identified AMR policy interventions implemented in Canada during the previous 10 years. Additional policies were identified through systematic searches of seven electronic databases and a review of government documents. Fifty-two unique policies were identified, with at least one policy in most provinces and territories. This environmental scan suggests that Canadian AMR efforts are disjointed and inadequate, given the urgency of this public health threat. Governments have mostly refrained from using more powerful policy tools, including regulation, legislation and fiscal measures.
Abstract
Nous avons mené une enquête auprès d'experts canadiens des services de santé afin d'identifier les politiques de lutte contre la résistance aux antimicrobiens (RAM) au Canada entre 2008 et 2018. Les répondants ont identifié des politiques d'intervention contre la RAM mises en place au cours des 10 années précédentes. Des politiques supplémentaires ont par ailleurs été décelées au moyen d'une recherche systématique dans sept banques de données et par un examen des documents gouvernementaux. Cinquante-deux politiques ont été dénombrées et la plupart des provinces et territoires comptaient sur au moins une d'entre elles. Cette analyse du contexte porte à croire que les efforts canadiens contre la RAM sont incohérents et inadéquats face au caractère urgent de cette menace en matière de santé publique. Les gouvernements se sont généralement abstenus d'employer des outils politiques plus puissants comme, notamment, la réglementation, la législation ou des mesures fiscales.
Introduction
Addressing rising rates of antimicrobial resistance (AMR) is a top challenge for the Canadian health system. Drug resistance is a naturally occurring phenomenon, whereby microbes evolve to become resistant to the antimicrobial drugs that we depend on to treat infections. Human actions – particularly the overuse, misuse and abuse of antimicrobials in humans, animals and agriculture – have accelerated this process (Holmes et al. 2016).
AMR will have severe health and economic consequences; rising AMR jeopardizes future health system capabilities in Canada. Effective antimicrobials are needed for a range of routine medical procedures, including surgeries and chemotherapy treatments. As resistance becomes widespread, our ability to carry out these procedures is threatened. Health system costs will also increase because patients with resistant infections are more expensive to treat. The Council of Canadian Academies (CCA 2019) estimates that AMR was responsible for 5,400 deaths and 880,000 days in hospital in 2018. Meanwhile, the Organisation for Economic Cooperation and Development (OECD 2018) estimates that the effects of AMR cost the health systems of developed countries US$3.5 billion per year, and the CCA (2019) calculated that AMR reduced Canada's GDP by CA$2 billion in 2018.
Although antimicrobials are life-saving drugs, a large proportion of global antimicrobial use is inappropriate. Antibiotics, which treat bacterial infections, are commonly used in Canada and the US to treat conditions caused by microbes for which these are totally ineffective (Chua et al. 2019). Close to half of Ontario seniors are given antibiotics for respiratory tract infections that are not caused by bacteria (Silverman et al. 2017). The leading strategy for tackling AMR is education with the goal of reducing the inappropriate use of antimicrobials through increased provider and patient knowledge (Van Katwyk et al. 2018, 2019). However, drug resistance in Canada is part of a larger global problem, and investments, coordination and political support for policy interventions are needed to collectively address AMR at all levels of the health system.
To date, it has been difficult to take stock of organized efforts to address AMR in Canada, or to identify policies and programs perceived to be successful in the Canadian context. The first Canadian action plan on AMR was released in 1997 with the goal of reducing overall antimicrobial prescriptions by 25% within three years (Government of Canada 1997). Unfortunately, the lack of complete antimicrobial use data from 1995 to 1999 impeded efforts to estimate the full impact of this plan (Finley et al. 2013). Although early estimates suggested that the 1997 action plan was beginning to have an impact (Conly 2002), it is unclear to what extent the government's call to action was implemented or sustained. A study of national programs undertaken from 1995 to 2010 described four major AMR programs in Canada during that time (Conly 2012), and other ad hoc programs have been launched since 2010. The Canadian Committee on Antibiotic Resistance, which was established during this period to perform a collating and coordinating role for stakeholder groups across Canada, published a series of reports and action plans highlighting AMR challenges in Canada but was disbanded in 2009 following funding cuts (Conly 2002; NCCID 2014; Nicolle 2012). We now lack a current description of Canadian policy interventions addressing AMR. We undertook this environmental scan to identify and catalogue recent Canadian policy interventions on AMR, with the aim of better understanding existing AMR efforts across the country and critically evaluating whether Canada has taken sufficient action to mitigate this important threat.
Methods
Policy interventions
We defined policy intervention as any public- or community-focused intervention to reduce AMR or inappropriate antimicrobial use in humans through education, restriction, incentivization, coercion, training, persuasion, changing of the physical or social context, modelling of appropriate behaviour or reduction of barriers to action, in accordance with the Behaviour Change Wheel (Michie et al. 2011; Van Katwyk et al. 2019). National, provincial/territorial and local interventions were included; however, clinical interventions and interventions focused on individual hospitals, pharmacies and other healthcare facilities were not included.
Data collection
Survey
We circulated a short e-mail questionnaire to identify AMR policy interventions between 2008 and 2018. This e-mail questionnaire asked respondents (1) if they were aware of any policy interventions related to AMR or antimicrobial use in Canada during the specified period, (2) when and where these interventions were undertaken, (3) what their goals were and (4) whom we could contact to obtain more details about the policies. We used purposive sampling to ensure a range of responses from federal, provincial, territorial and municipal levels and across human health sectors; e-mails were sent to a judgment sample of 253 experts who, in our view, were likely to be aware of AMR programs operating in Canada as a result of their professional roles. We anticipated that experts would potentially identify the same policies, and given our multistream approach to data collection, our sampling strategy prioritized geographic representation and professional representation above response rate. This sample included members of Canada's AMR Steering Committee, Council of Chief Medical Officers, academic researchers and representatives from health professional associations (medical, dental, pharmacy and nursing), regulatory colleges, hospitals and federal, provincial, territorial and municipal governments. Experts were encouraged to forward our e-mail to anyone who they thought might be able to provide relevant insights. E-mails in English and French were sent in February 2018, and follow-ups were sent two weeks after the initial e-mails. Where additional information was needed, we followed up with the respondent and conducted targeted Web searches.
Systematic Literature Search
We conducted a systematic search for published literature on interventions to change antimicrobial use in Canada. In consultation with three research librarians from health science, social science and the government, we developed a structured search query to capture published evaluations of interventions that aimed to reduce antimicrobial use. Seven electronic databases from medicine and the social sciences (MEDLINE, CINAHL, Embase, PAIS Index, Cochrane Central Register of Controlled Trials, Web of Science and PubMed articles not indexed in MEDLINE) were searched from inception to January 28, 2019, without language or date limits. The full search strategy has been published elsewhere (Van Katwyk et al. 2017). We limited the search strategy to records that included the term “Canada” or named a province or territory in the abstract, author affiliations or keywords, and which were published after 2008. One author (Susan Rogers Van Katwyk) reviewed the abstracts and full texts of these studies to identify the ones that described a Canadian policy intervention between 2008 and 2018.
Review of Government and Policy Literature
Finally, we conducted a grey literature search for policy and government documents on AMR. We conducted targeted Web searches of the Government of Canada website and targeted Google searches for “antimicrobial resistance” combined with the names of the provinces and territories. Additional grey literature sources were identified by key informants. We reviewed the reference lists of identified documents to identify other grey literature sources. We also requested a list of all funding announcements related to AMR between 2008 and 2018 from the Canadian Institutes of Health Research (CIHR).
Analysis
For each identified policy intervention, we attempted to identify the intervention region, setting, time frame, goals and affiliated organizations. Regions were coded by province/territory, or as a national effort if the policy had a broader reach. We coded interventions as communication, legislation, service provision, regulation, fiscal, guideline and environmental and social planning interventions in accordance with the policy categories of the Behaviour Change Wheel (Michie et al. 2011) and our recent systematic review (Van Katwyk et al. 2019). The communications category was subdivided into educational programs and campaigns, events, action plans and communication tools.
We did not collect demographic data about survey respondents, as they were not the focus of this research project. Respondents' geographic location and professional affiliation were known from the development of our judgment sample, and we report on the distribution of these characteristics. Respondents who were affiliated with multiple types of bodies (e.g., government officials who held academic appointments) were coded according to their primary affiliation. The University of Ottawa Office of Research Ethics and Integrity determined that ethics approval was not required for this project.
Results
Thirty-seven experts responded to the survey, including at least one respondent from every province and territory, except Newfoundland and Labrador. Experts represented federal (n = 3), provincial (n = 8) and regional (n = 4) governments, as well as academia (n = 4), medicine (n = 5), nursing (n = 4), pharmacy (n = 4), dentistry (n = 2), veterinary medicine (n = 2) and civil society (n = 3). CIHR launched 14 funding calls on AMR from 2008 to 2018. Our structured literature review identified 235 studies that included the term “Canada” or named a province or territory. Ultimately, we identified six studies that reported evaluations of Canadian policy interventions between 2008 and 2018 (Dickson et al. 2017; Fuertes et al. 2010; McKay et al. 2011; Announcement: Get Smart About Antibiotics Week 2016; Patrick et al. 2009; Zoutman and Ford 2012). Our grey literature search identified an additional 63 government and policy documents that were screened to identify policy interventions in Canada between 2008 and 2018; a full list of these sources is provided in Appendix 1 (available here). Figure 1 summarizes our three streams of data collection, and Box 1 shows a timeline of key actions, statements and policy papers in Canada between 2008 and 2018.
Figure 1.

Flowchart describing our three-stream approach to identifying policy interventions in Canada between 2008 and 2018
Box 1. Timeline of key AMR events and reports, 2008–2018.
| Date | Event |
|---|---|
| Jan 2011 | The Public Health Agency of Canada identifies antimicrobial resistance as one of the most significant public health risks facing Canadians. |
| Mar 2013 | Ontario Medical Association release policy paper: When Antibiotics Stop Working |
| May 2014 | Canadian Paediatric Society release position statement: Antimicrobial Stewardship in Daily Practice |
| Jun 2014 | Canadian Public Health Association release a Statement of Concern on Antimicrobial Resistance |
| Oct 2014 | Antimicrobial Resistance and Use in Canada: A Federal Framework for Action released |
| Oct 2014 | Expert Advisory Group on Antimicrobial Resistance established |
| Jan 2015 | Global Health Security Agenda identifies AMR as a priority; Canada a leading country |
| Mar 2015 | Federal Action Plan on Resistance and Use in Canada: Building on the Federal Framework for Action |
| Apr 2015 | Auditor General Report on AMR — “Significant work remains to be done” |
| Apr 2015 | Canadian Federation of Medical Students and Students for Antimicrobial Stewardship Society release policy paper |
| Oct 2015 | Canada and G7 Health Ministers commit to strengthening antibiotic stewardship programs for professionals in medical and vet fields |
| Oct 2015 | Canada joins Transatlantic Task Force on AMR |
| Jan 2016 | AMR endorsed as a priority at the “Canadian Health Ministers' Meeting” |
| Apr 2016 | HealthcareCAN report: Building Canada's Antimicrobial Stewardship Action Plan |
| Apr 2016 | Pan-Canadian Public Health Network release report: Antimicrobial Stewardship Report |
| Jul 2016 | COA, CDA and AMMI release consensus statement: Dental Patients with Total Joint Replacements |
| Nov 2016 | Canada announces $9 million to WHO to support implementation of the GAP |
| Nov 2016 | Canadian Institutes of Health Research hosts Multi-Stakeholder Antimicrobial Stewardship Expert Forum |
| Jan 2017 | Canadian Paediatric Society re-affirm position statement: Antimicrobial Stewardship in Daily Practice |
| Aug 2017 | Tackling Antimicrobial Resistance and Antimicrobial Use: A Pan-Canadian Framework for Action |
| Oct 2017 | Canada becomes Chair of the Global Health Security Agenda AMR Action Package |
| May 2018 | HESA presents: A Study on the Status of Antimicrobial Resistance in Canada and Related Recommendations to the House of Commons |
| Jul 2018 | Government Response to HESA Study: A Study on the Status of Antimicrobial Resistance in Canada and Related Recommendations |
| Jul 2018 | Progress Report on the 2015 Federal Action Plan on Antimicrobial Resistance and Use |
Note: COA: Canadian Orthopaedic Association; CDA: Canadian Dental Association; AMMI: Association of Medical Microbiology and Infectious Disease; GAP: Global Action Plan; HESA: House of Commons Standing Committee on Health
Altogether, we identified 52 programs active in Canada at some point between 2008 and 2018. The distribution of programs by region is shown in Figure 2; at least one program was identified in all provinces and territories, except Nova Scotia, New Brunswick and Newfoundland and Labrador; however, more than half of the identified interventions were organized at the national level (n = 33). Programs varied considerably in size and reach, from a one-page leaflet, to a series of tweets, to a fully integrated regional-level stewardship program. As such, a higher number of implemented interventions does not necessarily indicate increased action or focus on AMR.
Figure 2.
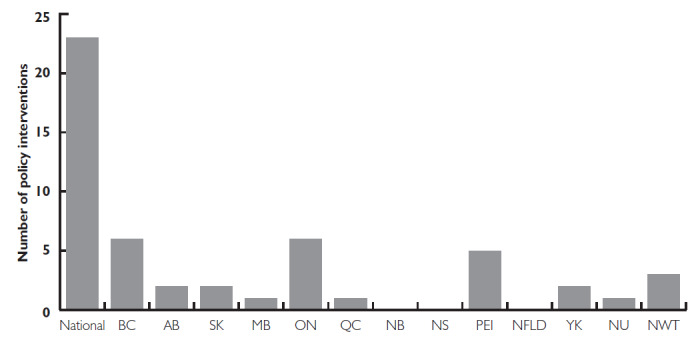
Distribution of identified policy interventions and programs across Canada
Between 2008 and 2018, CIHR announced 14 grant calls related to AMR and awarded $32.5 million to 77 teams (Box 1). These awards were to promote research in strategic areas, ranging from clinical and biological aspects of resistance to social science and global governance efforts. Many of these funding efforts have been in partnership with foreign governments: directly with the UK in 2008–2010, and, more recently, through the Joint Programming Initiative on AMR (JPIAMR). (Box 2 is available here.)
The most commonly identified interventions (n = 29) were communication interventions. Other identified interventions were guidelines (n = 9), regulations (n = 7), service provision (n = 5) and fiscal measures (n = 2). We did not identify any AMR-focused legislation or environmental and social planning programs. Among the included interventions, we are aware of five that have been quantitatively evaluated (Dickson et al. 2017; Fuertes et al. 2010; McKay et al. 2011; Patrick et al. 2009; Zoutman and Ford 2012).
Communication interventions
Among the communication interventions, we identified 16 educational programs, largely public awareness campaigns targeting health professionals and the public Table 1, available here). Many of the identified programs were provincial or regional variations on well-known programs such as “Do Bugs Need Drugs?” “Bugs and Drugs” or the annual Antibiotic Awareness Week. The Do Bugs Need Drugs? program has been linked to improvement in clinical knowledge of appropriate antibiotic treatment (McKay et al. 2011), and an ecological study has linked the program to declines in antimicrobial prescribing (Fuertes et al. 2010). Other smaller programs included radio broadcasts from the Northern Antibiotic Resistance Partnership, Twitter campaigns co-led by the Association of Medical Microbiology and Infectious Disease and the National Collaborating Centre for Infectious Disease and events organized by the Students for Antimicrobial Stewardship Society, a program organized by health professional students.
We identified three national frameworks and action plans released by the Public Health Agency of Canada (PHAC) in 2014, 2015 and 2017 (Government of Canada 2017). We also identified a provincial action plan that was in development in Quebec at the time of our survey, but no details were available. Three short educational events (1 to 2 days) were identified, two of which were hosted by CIHR and one by Health PEI. The remaining communication interventions included leaflets, posters and other tools to engage patients in discussions about antimicrobial use and to provide physicians with up-to-date information on antimicrobial prescribing.
Fiscal measures
We identified two fiscal policies (Table 2, available here), but neither provided funding for AMR action within Canada. The federal government provided $250,000 to support the World Bank in writing a report on AMR (World Bank 2017) and committed $9 million to the World Health Organization to support the development of national action plans in low- and middle-income countries.
Guidelines
We identified nine guideline interventions, seven of which were released by the federal or provincial governments, and two of which were collaborations among health professional associations (Table 3, available online at available here). Guidelines were released in response to the development of resistance in particular pathogens of concern, including methicillin-resistant Staphylococcus aureus and extensively drug-resistant Neisseria gonorrhoeae. A rigorous quasi-experimental evaluation of the effectiveness of introducing these new gonorrhea guidelines in Ontario found that uptake of the revised treatment guidelines was very slow. Following the release of new guidelines, the proportion of physicians prescribing according to treatment guidelines dropped by over 60% and never returned to pre-intervention levels (Dickson et al. 2017).
Regulations
We identified seven regulation interventions from 2008 to 2018 in Canada (Table 4, available here). The largest among these interventions was a regulation by Accreditation Canada requiring hospitals and long-term care facilities to have an antimicrobial stewardship program to receive accreditation. Only two regulations were identified at the level of the federal government: Health Canada implemented a regulation requiring a standard statement about AMR to be included on the drug monographs of all antibiotics, and Correctional Services Canada is in the process of developing a stewardship program for implementation in all their facilities.
Service provision
We identified five service provision interventions (Table 5, available here), two from Ontario and three from British Columbia. All five interventions provided education and training sessions on antimicrobial stewardship within the health system, often including audit and feedback on antimicrobial use rates. Three programs were delivered by, or in partnership with, provincial governments. Two programs were delivered in partnership with regional health units.
Discussion
Principal findings
AMR is among the top global threats facing humanity. Yet, the efforts identified in this environmental scan are too few, too small and too uncoordinated to meaningfully address this global threat. Our scan suggests that 10 years of AMR efforts in Canada have mostly consisted of a disjointed series of small projects that are inadequate to meet the Government of Canada's own AMR goals. Governments at all levels have prioritized small, education-based programs, rather than making use of the more powerful regulatory, fiscal and legislative policy levers at their disposal. Furthermore, the programs identified are not all based on scientific evidence or evaluated using rigorous scientific methods. There is only limited evidence that public awareness campaigns are effective at reducing antimicrobial use in the long term (Cross et al. 2016; Price et al. 2018), and there is no evidence that shows what program elements make an effective public awareness campaign (Van Katwyk et al. 2019). Indeed, at least one study showed that passively providing patients with information through posters and leaflets is ineffective (Hallsworth et al. 2016).
We believe Accreditation Canada's regulatory approach requiring all hospitals and long-term care facilities to implement antimicrobial stewardship programs is potentially more effective at reducing antimicrobial use. Although evidence that accreditation leads to improved care is weak (Brubakk et al. 2015), there is strong evidence that antimicrobial stewardship is effective (Davey et al. 2017). A rigorous evaluation of Accreditation Canada's program would be useful, particularly if it could identify the most effective components of a stewardship program. Other evidence-informed actions are the service provision efforts by the British Columbia Ministry of Health and Health Quality Ontario to provide audit and feedback on antimicrobial use to health professionals and long-term care facilities (Ivers et al. 2012).
We found relatively few references to clinical practice guidelines in this scan. Although we recognize that our search strategy may have missed examples of clinical practice guidelines, we note that guidelines are an important component of an AMR response. To respond to growing AMR, guidelines need to be regularly updated, widely disseminated and rapidly adopted by health professionals, although the simple production of guidelines without corresponding dissemination and implementation efforts is insufficient to address AMR (Dickson et al. 2017; Grol and Grimshaw 2003).
We identified few published or planned evaluations of policy effectiveness, and it was often unclear why an intervention was expected to work. For example, to the best of our knowledge, there is no evidence to suggest that placing warning labels about AMR on product monographs will change patient or professional behaviour. Although experimenting with new policies and strategies is essential for responding to AMR, policies planned without clear theories of change are unlikely to be effective.
Our findings suggest a surprising lack of engagement with AMR from key actors, including health professional associations and regulatory colleges. The Association of Medical Microbiology and Infectious Disease Canada is involved in many AMR efforts across Canada, and the College of Family Physicians of Canada has partnered with Choosing Wisely Canada on the Antibiotics Wisely campaign. Beyond these examples, we found only a few statements of concern released by the medical associations, and a guideline statement from the Canadian Dental Association. An effective, coordinated AMR response will require substantially more effort to integrate professional associations and bodies from medicine, dentistry, nursing and pharmacy.
The federated nature of the Canadian health system makes the provinces and territories responsible for regulating health professionals and antimicrobial use. The Office of the Auditor General of Canada (OAG 2015) found that the PHAC had not yet succeeded in mobilizing all federal, provincial and territorial partners and stakeholders toward a Pan-Canadian Strategy on AMR. We saw limited evidence that Canadian provinces were independently pursuing regulatory approaches to addressing AMR. Provincial government responses have largely focused on educational campaigns and prescribing guidelines, and, as far as we are aware, only Quebec is developing a provincial AMR action plan. The lack of action or action plans from other provinces and territories emphasizes the need for increased commitment, coordination and collaboration among government actors. The forthcoming Pan-Canadian Action Plan on AMR should provide a platform for increasing collaboration across levels of government; however, fulfilling the obligations of this action plan will require more action from provinces and territories than has been seen to date.
Policy implications
Despite the activities catalogued in this environmental scan, the rates of community antimicrobial use in Canada have been stable since 2013 (PHAC 2018). Increasing resistance highlights the extent to which the resources committed to AMR are incommensurate with the scale of the collective action problem. AMR represents a major threat to the sustainability of the Canadian healthcare system and requires substantially more focused investment and attention. Although Canada has taken on AMR leadership roles abroad, the level of political engagement, funding and regulatory and legislative action on AMR in Canada appears to be limited. Although PHAC provides routine funding for AMR surveillance and awareness campaigns, our scan did not identify any announcements of new domestic funding beyond CIHR research grants.
Framing AMR as a problem of individual patient and prescriber behaviour has unsurprisingly led to a series of AMR responses focused on education. This strategy recognizes that providers are more likely to prescribe antibiotics when patients request them (Coenen et al. 2006, 2013; Llor et al. 2013). However, antibiotic prescribing is also shaped by a series of health systems factors and social determinants of health, such as healthcare access, clinic volume, socio-economic status and patient–provider trust (Cole 2014; Gjelstad et al. 2011; Tangcharoensathien et al. 2018).
There are many policy approaches that have not been tried in Canada (Van Katwyk et al. 2019), including several legal, regulatory and fiscal strategies. To address AMR effectively, we need to make full use of these more powerful strategies and build a coordinated, evidence-based suite of policies to address AMR at multiple levels. Recent calls from CIHR and JPIAMR to fund social science and behaviour change research on AMR may lead to useful new strategies, and all policy interventions should be paired with appropriately rigorous evaluation plans to better inform resource allocation and shared learning across provinces and territories. As a starting point, provinces and territories should focus on improving and harmonizing the collection of data on AMR and antimicrobial use across the country, which will facilitate future evaluation efforts. The forthcoming Pan-Canadian Action Plan on AMR may provide the necessary platform for the federal and provincial governments to pursue a much ambitious AMR strategy. Future AMR action must move beyond simply integrating existing public communications campaigns and tools and toward effective, integrated, regulatory, legislative and fiscal measures.
Strengths and limitations
This report adds to the growing literature on AMR inaction in Canada. By surveying experts across Canada, we have captured data on AMR policy efforts at the national, provincial and territorial levels and those organized by academics and civil society. Although we aimed to be comprehensive through our combination of questionnaire, grey literature and published literature searching, some policies and programs may not have been captured if these were not identified by experts and if their Web resources were no longer available. We received responses from only 37 of our 235 experts and are more likely to have missed policies in regions or professions where we received fewer responses. This purposive sampling strategy focused on experts who currently hold positions where they would be aware of AMR programs in Canada; however, it is possible that we missed earlier programs because of staff turnover. We did not attempt to contact people who had moved on from their expert positions in the public health community. Similarly, online grey literature searching privileges recent sources over older documentation, particularly for defunct organizations such as the Canadian Committee on Antibiotic Resistance, whose Web resources have been removed. We have attempted to overcome these limitations by combining research strategies and, to the best of our ability, verifying our information through other sources. Finally, we chose to limit the scope of this study to policy interventions to reduce human antimicrobial use. We recognize that the Health Canada's Veterinary Drugs Directorate has made policy changes on antimicrobial use in animals that were not included in this report.
Conclusions
AMR is a major threat to public health and healthcare in Canada. Our review suggests that the AMR interventions in Canada over the past 10 years have been too few, too small and too uncoordinated to adequately address the threat posed by AMR. Increased commitment to AMR, including multisectoral inter-agency cooperation and funding, is needed to ensure that future interventions are effective, evidence-informed and sufficient for Canada to overcome this looming threat.
Acknowledgements
The authors would like to thank librarians Michael Boutet, Catherine McGoveran and Lindsey Sikora at the University of Ottawa, Ottawa, ON, who provided advice, support and peer review for the development of this search strategy.
Contributor Information
Susan Rogers Van Katwyk, Investigator, Global Strategy Lab, Dahdaleh Institute for Global Health Research, York University, Toronto, ON.
Jeremy M. Grimshaw, Senior Scientist, Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON.
Steven J. Hoffman, Dahdaleh Distinguished Chair, Global Governance and Legal Epidemiology, Global Strategy Lab, Professor of Global Health, Law, and Political Science, York University, Toronto, ON.
Funding
This work was completed as part of the International Collaboration for Capitalizing on Cost-Effective and Life-Saving Commodities (i4C) that is funded through the Research Council of Norway's Global Health and Vaccination Programme (GLOBVAC Project #234608). Susan Rogers Van Katwyk is supported by an Ontario Graduate Scholarship and Steven J. Hoffman is additionally supported by the Canadian Institutes of Health Research. Jeremy M. Grimshaw holds a Canada Research Chair in Health Knowledge Transfer and Uptake. None of the funders had a role in the design of the study, the preparation of this manuscript or the decision to publish it.
Conflict of interest
Steven J. Hoffman is Scientific Director of CIHR's Institute of Population and Public Health. The views expressed in this article are those of the authors and do not necessarily reflect those of CIHR or the Government of Canada.
References
- Announcement: Get Smart About Antibiotics Week – November 14–20, 2016. Morbidity & Mortality Weekly Report 65(44): 1240. 10.15585/mmwr.mm6544a9. [DOI] [PubMed] [Google Scholar]
- Brubakk K., Vist G.E., Bukholm G., Barach P., Tjomsland O. 2015. A Systematic Review of Hospital Accreditation: The Challenges of Measuring Complex Intervention Effects. BMC Health Services Research 15(1): 280. 10.1186/s12913-015-0933-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council of Canadian Academies (CCA). 2019. When Antibiotics Fail: The Expert Panel on the Potential Socio-Economic Impacts of Antimicrobial Resistance in Canada. Retrieved May 25, 2020. <https://cca-reports.ca/wp-content/uploads/2018/10/When-Antibiotics-Fail-1.pdf>.
- Chua K.P., Fischer M.A., Linder J.A. 2019. Appropriateness of Outpatient Antibiotic Prescribing Among Privately Insured US Patients: ICD-10-CM Based Cross Sectional Study. BMJ 364: k5092. 10.1136/bmj.k5092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coenen S., Michiels B., Renard D., Denekens J., Van Royen P. 2006. Antibiotic Prescribing for Acute Cough: The Effect of Perceived Patient Demand. British Journal of General Practice 56(524): 183–90. [PMC free article] [PubMed] [Google Scholar]
- Coenen S., Francis N., Kelly M., Hood K., Nuttall J., Little P. et al. 2013. Are Patient Views about Antibiotics Related to Clinician Perceptions, Management and Outcome? A Multi-Country Study in Outpatients with Acute Cough. PLoS One 8(10): e76691. 10.1371/journal.pone.0076691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole A. 2014. GPs Feel Pressurised to Prescribe Unnecessary Antibiotics, Survey Finds. BMJ 349: g5238. 10.1136/bmj.g5238. [DOI] [PubMed] [Google Scholar]
- Conly J.M. 2002. Antimicrobial Resistance in Canada. CMAJ. 167(8): 885–91. [PMC free article] [PubMed] [Google Scholar]
- Conly J.M. 2012. Antimicrobial Resistance Programs in Canada 1995–2010: A Critical Evaluation. Antimicrobial Resist Infect Control 1(1): 10. 10.1186/2047-2994-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross E.L., Tolfree R., Kipping R. 2016. Systematic Review of Public-Targeted Communication Interventions to Improve Antibiotic Use. Journal of Antimicrobial Chemotherapy 72(4): 975–87. 10.1093/jac/dkw520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey P., Marwick C.A., Scott C.L., Charani E., McNeil K., Brown E. et al. 2017. Interventions to Improve Antibiotic Prescribing Practices for Hospital Inpatients. Cochrane Database of Systematic Reviews 9(2): CD003543. 10.1002/14651858.CD003543.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson C., Taljaard M., Friedman D.S., Metz G., Wong T., Grimshaw J.M. 2017. The Antibiotic Management of Gonorrhoea in Ontario, Canada following Multiple Changes in Guidelines: An Interrupted Time-Series Analysis. Sexually Transmitted Infections 93(8): 561–65. 10.1136/sextrans-2017-053224. [DOI] [PubMed] [Google Scholar]
- Finley R., Glass-Kaastra S.K., Hutchinson J., Patrick D.M., Weiss K., Conly J. 2013. Declines in Outpatient Antimicrobial Use in Canada (1995–2010). PLoS One 8(10): e76398. 10.1371/journal.pone.0076398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuertes E.I., Henry B., Marra F., Wong H., Patrick D.M. 2010. Trends in Antibiotic Utilization in Vancouver Associated with a Community Education Program on Antibiotic Use. Canadian Journal of Public Health 101(4): 304–08. 10.1007/BF03405291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjelstad S., Straand J., Dalen I., Fetveit A., Strøm H., Lindbæk M. 2011. Do General Practitioners' Consultation Rates Influence Their Prescribing Patterns of Antibiotics for Acute Respiratory Tract Infections? Journal of Antimicrobial Chemotherapy 66(10): 2425–33. 10.1093/jac/dkr295. [DOI] [PubMed] [Google Scholar]
- Government of Canada. 1997. Controlling Antimicrobial Resistance. An Integrated Action Plan for Canadians. Canada Communicable Disease Report 23(Suppl 7): i–iv, 1–32. [PubMed] [Google Scholar]
- Government of Canada. 2017. Tackling Antimicrobial Resistance and Antimicrobial Use: A Pan-Canadian Framework for Action. Retrieved March 20, 2018. <https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/tackling-antimicrobial-resistance-use-pan-canadian-framework-action.html>.
- Grol R., Grimshaw J. 2003. From Best Evidence to Best Practice: Effective Implementation of Change in Patients' Care. The Lancet 362(9391): 1225–30. 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- Hallsworth M., Chadborn T., Sallis A., Sanders M., Berry D., Greaves F. et al. 2016. Provision of Social Norm Feedback to High Prescribers of Antibiotics in General Practice: A Pragmatic National Randomised Controlled Trial. The Lancet 387(10029): 1743–52. 10.1016/S0140-6736(16)00215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes A.H., Moore L.S.P., Sundsfjord A., Steinbakk M., Regmi S., Karkey A. et al. 2016. Understanding the Mechanisms and Drivers of Antimicrobial Resistance. The Lancet 387(10014): 176–87. 10.1016/S0140-6736(15)00473-0. [DOI] [PubMed] [Google Scholar]
- Ivers N., Jamtvedt G., Flottorp S., Young J.M., Odgaard-Jensen J., French S.D. et al. 2012. Audit and Feedback: Effects on Professional Practice and Healthcare Outcomes. Cochrane Database of Systematic Reviews 13(6): CD000259. 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llor C., Bjerrum L., Strandberg E.L., Radzeviciene R., Reutskiy A., Caballero L. 2013. Low Request of Antibiotics from Patients with Respiratory Tract Infections in Six Countries: Results from the Happy Audit Study. Antibiotics 2(4): 477–84. 10.3390/antibiotics2040477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay R.M., Vrbova L., Fuertes E., Chong M., David S., Dreher K. et al. 2011. Evaluation of the Do Bugs Need Drugs? Program in British Columbia: Can We Curb Antibiotic Prescribing? Canadian Journal of Infectious Diseases and Medical Microbiology 22(1): 19–24. 10.1155/2011/745090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., van Stralen M.M., West R. 2011. The Behaviour Change Wheel: A New Method for Characterising and Designing Behaviour Change Interventions. Implementation Science 6(1): 42. 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Collaborating Centre for Infectious Diseases (NCCID). 2014. Surveillance of Antimicrobial Resistance and Antimicrobial Utilization in Canada. Retrieved December 10, 2018. <https://nccid.ca/publications/surveillance-of-antimicrobial-resistance-and-antimicrobial-utilization-in-canada/#subMenuSection2>.
- Nicolle L.E. 2012. Control of Antimicrobial Resistance in Canada: Any Lessons to Learn? Antimicrobial Resistance and Infection Control 1: 6. 10.1186/2047-2994-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Auditor General of Canada (OAG). 2015. Report 1 – Antimicrobial Resistance. Retrieved May 16, 2019. <https://www.oag-bvg.gc.ca/internet/English/parl_oag_201504_01_e_40347.html>.
- Organisation for Economic Cooperation and Development (OECD). 2018. Stemming the Superbug Tide: Just a Few Dollars More. OECD Publishing; Retrieved January 15, 2019. <https://www.oecd.org/health/stemming-the-superbug-tide-9789264307599-en.htm>. [Google Scholar]
- Patrick D., Blondel-Hill E., Vrbova L., Fuertes E., Marra F., Henry B. et al. 2009. Evaluation of a Population-Based Program for the Wise Use of Antibiotics. International Journal of Antimicrobial Agents 34: S52–53. 10.1016/S0924-8579(09)70299-7. 19931820 [Google Scholar]
- Price L., Gozdzielewska L., Young M., Smith F., MacDonald J., McParland J. et al. 2018. Effectiveness of Interventions to Improve the Public's Antimicrobial Resistance Awareness and Behaviours Associated with Prudent Use of Antimicrobials: A Systematic Review. Journal of Antimicrobial Chemotherapy 73(6): 1464–78. 10.1093/jac/dky076. [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada (PHAC). 2014. Antimicrobial Resistance and Use in Canada: A Federal Framework for Action. Public Health Agency of Canada; Retrieved January 28, 2019. <https://www.canada.ca/en/public-health/services/antibiotic-antimicrobial-resistance/antimicrobial-resistance-use-canada-federal-framework-action.html>. [Google Scholar]
- Public Health Agency of Canada (PHAC). 2015. Federal Action Plan on Antimicrobial Resistance and Use in Canada: Building on the Federal Framework for Action. Public Health Agency of Canada; Retrieved January 28, 2019. <https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/federal-action-plan-antimicrobial-resistance-canada.html>. [Google Scholar]
- Public Health Agency of Canada (PHAC). 2018. Canadian Antimicrobial Resistance Surveillance System – Update 2018: Executive Summary: Public Health Agency of Canada. Retrieved April 7, 2019. <https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2018-report-executive-summary.html>.
- Silverman M., Povitz M., Sontrop J.M., Li L., Richard L., Cejic S. et al. 2017. Antibiotic Prescribing for Nonbacterial Acute Upper Respiratory Infections in Elderly Persons. Annals of Internal Medicine 166(11): 765–74. 10.7326/M16-1131. [DOI] [PubMed] [Google Scholar]
- Tangcharoensathien V., Chanvatik S., Sommanustweechai A. 2018. Complex Determinants of Inappropriate Use of Antibiotics. Bulletin of the World Health Organization 96(2): 141–44. 10.2471/BLT.17.199687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Katwyk S.R., Grimshaw J.M., Mendelson M., Taljaard M., Hoffman S.J. 2017. Government Policy Interventions to Reduce Human Antimicrobial Use: Protocol for a Systematic Review and Meta-analysis. Systematic Reviews 6(1): 256. 10.1186/s13643-017-0640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Katwyk S.R., Grimshaw J.M., Nkangu M., Mendelson M., Taljaard M., Hoffman S.J. 2019. Government Policy Interventions to Reduce Human Antimicrobial Use: A Systematic Review and Evidence Map. PLoS Medicine 16(6): e1002819. 10.1371/journal.pmed.1002819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Katwyk S.R., Jones S.L., Hoffman S.J. 2018. Mapping Educational Opportunities for Healthcare Workers on Antimicrobial Resistance and Stewardship Around the World. Human Resources for Health 16(1): 9. 10.1186/s12960-018-0270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. 2017. Drug Resistant Infections: A Threat to Our Economic Future. Retrieved August 11, 2018. <https://www.worldbank.org/en/topic/health/publication/drug-resistant-infections-a-threat-to-our-economic-future>.
- Zoutman D.E., Ford B.D. 2012. The Impact of Feedback on the Antibiotic Prescribing of Family Physicians for Respiratory Tract Infections. The Canadian Journal of Infection Control 27(4): 221–24. [Google Scholar]


