Coronavirus disease 2019 (COVID-19) infection, caused by the severe acute respiratory syndrome coronavirus 2, poses a double threat to public health: The immediate threat is the morbidity and mortality related to the infection, and the more subtle threat is the shift of attention and resources away from the care of regular diseases.
Patient- and Healthcare Network–Related Factors
Multiple investigators across Europe have reported a reduction in patients admitted for ST-segment–elevation myocardial infarction (STEMI) since the COVID pandemic began.1 This may be the result of a decreased awareness/shift of attention of patients, the desire not to overload the emergency medical systems (EMS), and the fear of infection and not receiving proper treatment, as well. For similar reasons, clinicians and nurses visiting patients at home or nursing homes may have a higher threshold to refer patients with chest pain to the emergency departments (Figure). An EMS alert may be challenging because of jammed phone lines and a limited number of ambulances. Trained ambulance personnel may not be available to make STEMI diagnosis on site. In addition, shared experiences estimate an up to 60-minute increase in intrinsic delay from diagnosis to reperfusion with primary percutaneous coronary intervention (PCI) in regions deeply affected by the COVID-19 pandemic, because of suboptimal EMS availability and the implementation of personal protective equipment at any level of care (prehospital, emergency department, and cardiac catheterization laboratory). Moreover, uncertainty regarding diagnosis, given reports of myopericarditis presenting as a STEMI mimic, may add to delays. Spoke centers may have been converted to COVID hospitals, may be more restrictive in transferring patients who have STEMI for primary PCI, and may adopt fibrinolytic treatment without subsequent systematic referral for angiography. It is important to note that the safety and efficacy of fibrinolysis in patients with COVID-19 presenting with ST elevation who may have associated myopericarditis or coagulopathy, ranging from isolated d-dimer level elevation observed in up to 40% of patients to disseminated intravascular coagulation, remain unknown.2
Figure.
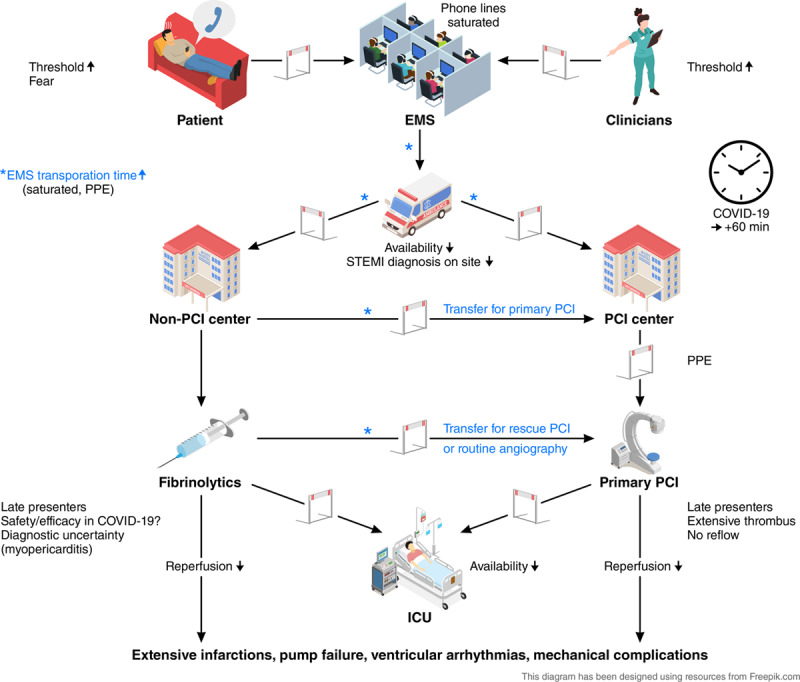
Obstacles affecting timely reperfusion in ST-segment–elevation myocardial infarction (STEMI) at the patient, emergency services (EMS), and institutional levels during the COVID-19 pandemic. Although patient and primary care workers may be reluctant to call EMS, it is estimated that the overload of the healthcare systems, the increase in transportation time, and the need for personal protection equipment (PPE) may increase the time to reperfusion up to 60 minutes. Late presentations are more common and decrease the efficacy of both primary percutaneous coronary intervention (PCI) and fibrinolytic therapy. An increase in complications of myocardial infarction, such as pump failure, ventricular arrhythmias, and mechanical complications, is expected. COVID-19 indicates coronavirus disease 2019; and ICU, intensive care unit.
Impact on Primary PCI
In patients with STEMI and multivessel coronary artery disease, guidelines recommend complete revascularization, which in many institutions is performed as a staged procedure. In the COVID-19 pandemic, 2 considerations based on the disease complexity may change this strategy. If the culprit lesion has been treated successfully with no complications, the additional coronary lesions are easily accessible, and the patient is hemodynamically stable, immediate complete revascularization may be an attractive guideline-conforming option to avoid a staged procedure, which would prolong the hospital stay or require a second admission and additional personnel exposure if the patient is COVID-19 positive.3 If revascularization of the culprit lesion has been challenging or associated with a complication (eg, no reflow), the patient is unstable, or a nonculprit disease would require complex PCI, the operator may opt for medical management of the nonculprit disease to avoid the risk of hemodynamic deterioration and the need for (prolonged) intensive care unit surveillance.
Bergamo’s Experience
At the end of February 2020, the city of Bergamo, Italy, became the place where COVID-19 hit Europe first and in the hardest way. The EMS, one of the most efficient local and regional networks for time-dependent disease transportation in Italy, was flooded by calls of patients in severe respiratory distress. During a 40-day period starting February 23, 2020, the emergency department of the Papa Giovanni Hospital (where one of the authors [Dr Guagliumi] practices) admitted 1407 patients with interstitial pneumonia, >400 and 150 of them requiring noninvasive ventilation and endotracheal intubation, respectively. A survey from administrative data, provided by 138 municipalities representing 70% of the total population in the province of Bergamo, showed that >5400 people died in March 2020, 6 times more than in the corresponding month of the previous year.4 Among them, 2060 were COVID-19 in-hospital deaths, whereas the remaining occurred at home or nursing homes without diagnosis. Therefore, they were not integrated in the COVID-19 statistics.
The regional STEMI network was quickly changed into a model of macrohubs to concentrate personnel and urgent activities, such as primary PCI for STEMI or interventional stroke management, while expanding health resources for patients with COVID-19 in all remaining hospitals. Protocols were implemented to allow and regulate separate patient admission of patients with STEMI, from triage through the catheterization laboratory, to reduce cross-infections and to train the personnel to the new personal protective equipment standards. Despite an increase in delays, primary PCI was offered to most patients with STEMI. The decision was made not to perform primary PCI, and instead administer fibrinolytic treatment, in patients with COVID-19 presenting with severe respiratory distress syndrome but not qualifying for endotracheal intubation based on age or comorbidities. All patients in severe respiratory distress undergoing primary PCI were intubated before arrival at the catheterization laboratory to minimize contamination. During the month of March 2020, a marked reduction in primary PCI for STEMI (–37%) and an increase in late presentations (+25%) were observed in the province, in comparison with the monthly average of the previous year. Extensive infarctions, heart failure, high coronary thrombus burden, and no reflow were more frequent.
Madrid’s Experience
Spain was among the countries that have been hit hard by the COVID-19 pandemic, with >166 000 infected people and >17 000 deaths (~350 per million inhabitants) as of April 12, 2020. Madrid (where one of the authors [Dr Ibanez] practices) was the region of Spain with the highest prevalence of the disease, with >47 000 confirmed cases and ≈6300 deaths (≈870 deaths per million inhabitants) on the same date. According to the Spanish Ministry of Health, the first patient with COVID-19 was admitted to intensive care in Madrid on March 8, whereas the peak of patients with COVID-19 in intensive care was achieved on April 5 with 1510 patients). The pandemic has disrupted the Codigo Infarto Madrid, a successful STEMI network treating ≈2500 patients with STEMI per year, >98% of them by primary PCI, in 11 catheterization laboratories 24/7. The main challenge in the Madrid area, and in other affected areas of Spain, as well, has been the saturation of the EMS. A survey conducted in Madrid showed that the number of primary PCIs has been reduced by half since the inception of the COVID-19 pandemic in comparison with the previous weeks. This has been accompanied by a slight increase in the use of fibrinolysis, mainly in patients presenting at non-PCI centers.5 After a massive reduction in patients seeking EMS for chest pain, the cardiology community in the region is performed a public awareness campaign in newspapers and social media. Primary PCI program remained the preferred reperfusion strategy in the region, provided it could be done in a timely manner. All patients were handled as potential COVID-19 positive.
Conclusion
The COVID-19 pandemic represents an unprecedented challenge for healthcare systems and negatively affects time-dependent care of acute cardiovascular conditions such as STEMI. Two European cities hit hard, Bergamo, Italy, and Madrid, Spain, are examples.
Disclosures
None.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Wood S. The mystery of the missing STEMIs during the COVID-19 pandemic. tctMD. Apr 2, 2020. https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19-pandemic. Accessed April 10, 2020.
- 2.Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection [published online March 3, 2020]. Clin Chem Lab Med. doi: 10.1515/cclm-2020-0198. doi: 10.1515/cclm-2020-0198 https://www.degruyter.com/view/journals/cclm/ahead-of-print/article-10.1515-cclm-2020-0198/article-10.1515-cclm-2020-0198.xml. Accessed April 9, 2020. [DOI] [PubMed] [Google Scholar]
- 3.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 4.Invernizzi I. Coronavirus, the real death toll: 4,500 victims in one month in the province of Bergamo. Newspaper Eco di Bergamo. 2020 Apr 1; https://www.ecodibergamo.it/stories/bergamo-citta/coronavirus-the-real-death-tool-4500-victims-in-one-month-in-the-province-of_1347414_11. Accessed April 8, 2020. [Google Scholar]
- 5.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Rumoroso JR, López-Palop R, Serrador A, Cequier A, Romaguera R, Cruz I, et al. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol. 2020;2:82–89. doi: 10.24875/RECIC.M20000120. [Google Scholar]


