This prospective multicenter cohort study investigated the predictive value of clinical and radiological findings for nonunion after osteoporotic compression fractures. A diffuse low type pattern on T1-weighted MRI and diffuse low and fluid type patterns on T2-weighted MRI were the independent risk factors for nonunion in the acute phase.
Keywords: kyphosis, low back pain, nonunion, osteoporotic vertebral fracture, patient-reported outcome measures, quality of life, radiographic assessments, risk factors
Abstract
Study Design.
Prospective cohort study.
Objective.
To characterize a patient population with nonunion after acute osteoporotic vertebral fractures (OVFs) and compare the union and nonunion groups to identify risk factors for nonunion.
Summary of Background Data.
While OVFs are the most common type of osteoporotic fracture, the predictive value of a clinical assessment for nonunion at 48 weeks after OVF has not been extensively studied.
Methods.
This prospective multicenter cohort study included female patients aged 65 to 85 years with acute one-level osteoporotic compression fractures. In the radiographic analysis, the anterior vertebral body compression percentage was measured at 0, 12, and 48 weeks. Magnetic resonance imaging (MRI) was performed at enrollment and at 48 weeks to confirm the diagnosis and union status. The patient-reported outcome measures included scores on the European Quality of Life-5 Dimensions (EQ-5D), a visual analogue scale for low back pain, and the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) at 0, 12, and 48 weeks.
Results.
In total, 166 patients completed the 12-month follow-up, 29 of whom had nonunion. Patients with nonunion at 48 weeks after OVF had lower EQ-5D and JOABPEQ walking ability, social life function, mental health, and lumbar function scores than those with union at 48 weeks after injury. The independent risk factors for nonunion after OVF in the acute phase were a diffuse low type pattern on T1-weighted MRI and diffuse low and fluid type patterns on T2-weighted MRI. The anterior vertebral body compression percentage and JOABPEQ social life function scores were independent risk factors at 12 weeks.
Conclusion.
A diffuse low type pattern on T1-weighted MRI and diffuse low and fluid type patterns on T2-weighted MRI were independent risk factors for nonunion in the acute phase. Patients who have acute OVFs with these risk factors should be carefully monitored for nonunion.
Level of Evidence: 2
Because vertebral fractures are the most common type of osteoporotic fracture, the number of osteoporotic vertebral fractures (OVFs) increases as the population ages. Indeed, the Rotterdam study showed that while the incidence of vertebral fractures was 7.8/1000 person-years at ages 55 to 65 years, the incidence increased to 19.6/1000 person-years at ages of 75 years or older for women.1 In the acute stage, OVFs cause severe back pain, disabilities in activities of daily living, and deterioration of the quality of life (QOL). For most patients with OVFs, pain levels and QOL gradually improve as bony union is achieved.2 However, if bony union fails, continuous lower back pain, deterioration of QOL, and even neurological deficits attributable to nerve compression can occur.3 Accordingly, operative interventions such as vertebroplasty, spinal decompression, and instrumentation surgery are performed for patients with such nonunions to reduce back pain and the risk of developing further spinal deformities. However, these procedures have disadvantages of procedural complications and may increase the risk of fracture in the adjacent vertebrae.4 Moreover, while some reports have shown the usefulness of radiological findings for predicting delayed union (3–6 mo after injury),3,5,6 there are few reports that have investigated the risk factors for nonunion (48 wks or longer after injury). Therefore, improved identification methods for patients at high risk of nonunion after OVF are needed so that preventive measures can be implemented to decrease the incidence of this complication.
The purpose of this prospective multicenter study was to characterize a patient population with nonunion after acute OVFs and to compare the union and nonunion groups to identify risk factors associated with nonunion, with a focus on patient-reported outcome measures and radiographic assessments to identify cut-off values for these risk factors.
MATERIALS AND METHODS
Seventy-one hospitals in Japan joined this prospective multicenter cohort study. From August 2014 to September 2016, female patients aged between 65 and 85 years with one acute OVF were recruited for this study. The diagnosis of OVF was based on the presence of acute low back pain, plain lateral radiographs, and magnetic resonance imaging (MRI) findings. The exclusion criteria included the following: more than two (>2) previous OVFs from T10 to L2; neurological deficits; spinal metastasis; spinal infections; inability to complete the questionnaires; and incomplete MRI evaluations at enrollment and 48 weeks, since a fresh fracture diagnosis was confirmed by MRI at enrollment and union status was determined by MRI at 48 weeks. A total of 284 patients were enrolled. Reasons for dropout during the 48-week follow-up period included the following: two patients due to changes in osteoporosis medication (bisphosphonate, 1; teriparatide, 1), six due to operations (for neurological deficits, 4; for severe pain, 1; for lumbar spinal stenosis, 1), five due to their own decision, two for dementia progression, three because they changed hospitals, three because of death, one for pneumoniae, 29 for missing MRI at enrollment, 33 for missing MRI at 48 weeks, 34 with no reason given. Finally, 166 patients with 48 weeks of follow-up were included in this study.
This study was approved by the Institutional Ethical Committee, and all patients provided written informed consent. The physicians explained the pathological condition to each patient, and after providing approval, each patient was invited to participate in this study. The patients wore premade braces until they were fitted with a thoracolumbar sacral rigid or soft brace. The braces were indicated to wear at all times for 12 weeks. In terms of antiosteoporosis treatment, the patients were allowed to use only the same medication they were taking before the injury or a newly prescribed active vitamin D drug in order to exclude any negative or positive impact of osteoporosis medication on fracture union. In terms of analgesic use, the patients were allowed to use aspirin, nonsteroidal anti-inflammatory drugs, and weak opiates. The participants did not receive financial support for the treatments, including the braces and pain medication.
Patient-reported Outcome Measures
For the patient-reported outcome measures, scores on the European Quality of Life-5 Dimensions (EQ-5D-3 L range: −0.111 to 1, with higher scores indicating a better QOL),7 a visual analogue scale (VAS) for low back pain (range: 0–100, with higher scores indicating more severe pain),8 and the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) for pain-related disorders, lumbar spine function, walking ability, social life function, and mental health (range from 0–100, with higher scores indicating better function)9 were used. These questionnaires were administered at a regular hospital visit (0, 12, and 48 wk after brace application). We allowed relatives and carers to help the patients to complete these questionnaires, but the questionnaires were completed without assistance from the surgeon or any other person involved in the trial.
Radiographic Assessment
Lateral radiography was performed at 0, 12, and 48 weeks. MRI was performed at enrolment and at 48 weeks after fracture to confirm union status. In the radiographic analysis, the anterior vertebral body compression percentage (AVBCP), the ratio between the vertical height of the compressed anterior section of the injured vertebral body and the posterior vertebral body height at the same level, was measured independently at 0, 12, and 48 weeks after brace application by two radiologists who were unaware of the treatment method. The mean value from the two evaluators was used. Nonunion was defined as a recognizable gas- or fluid-filled cleft separating the superior and inferior end plates on MRI and radiography at the 48-week follow-up. We slightly modified the MRI classification by Tsujio et al5 into confined low-intensity and diffuse low-intensity T1-weighted images and diffuse high-intensity, confined low-intensity, diffuse low-intensity, and fluid-intensity T2-weighted image patterns (Figure 1A–F).
Figure 1.
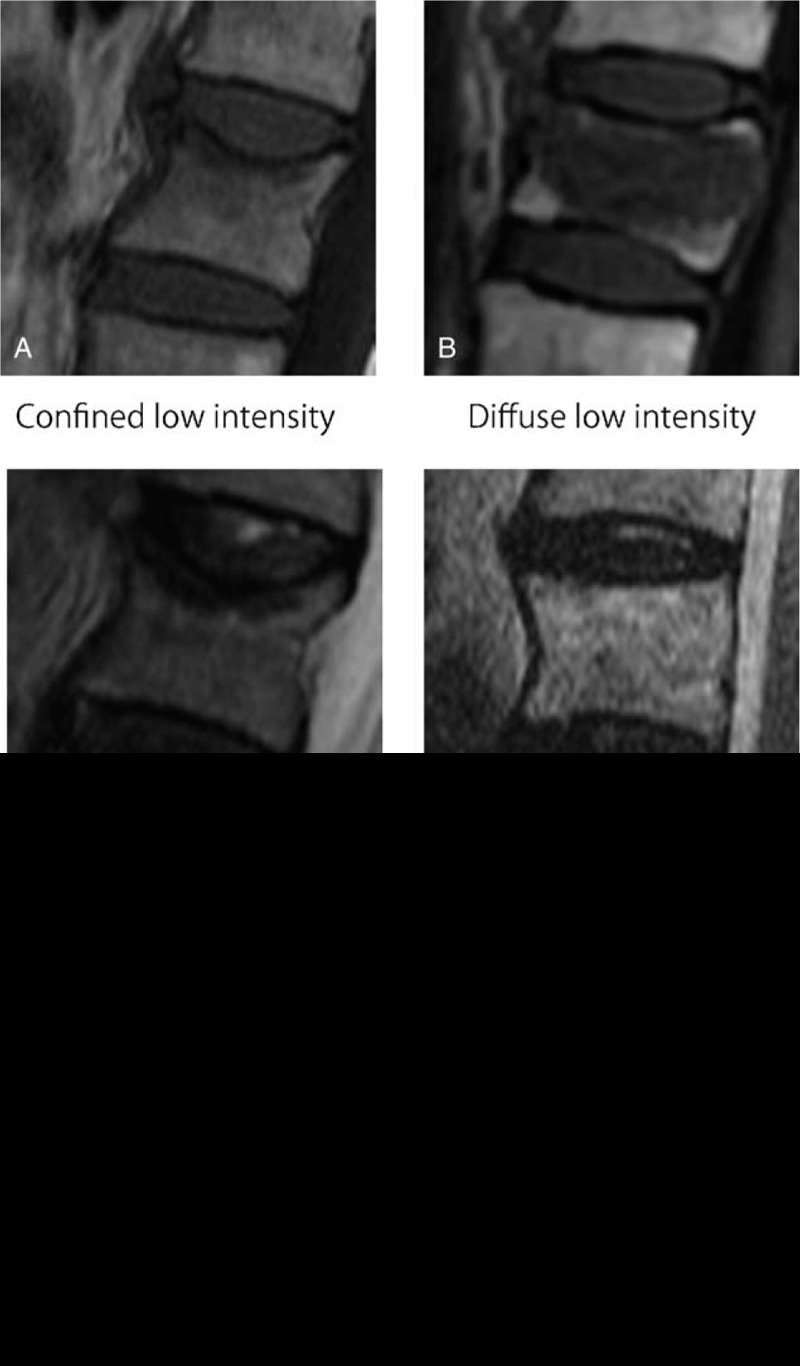
Classification of OVFs on T1-weighted images. A, Confined low-intensity image. B, Diffuse low-intensity image. Classification of OVFs on T2-weighted images. C, Confined low-intensity image. D, Diffuse high-intensity image. E, Diffuse low-intensity image. F, Fluid-intensity image. OVF indicates osteoporotic vertebral fractures.
DATA ANALYSIS
All data were collected by a blinded clinical research assistant. Outcome and risk factor analyses were performed by comparing the union and nonunion groups. We analyzed continuous variables using an unpaired two tailed t test for normally distributed data and continuous data with skewed distribution using the Mann–Whitney U test after assessing normality with the Shapiro–Wilk test. Fisher exact test was used for nominal variables. To identify the most significant risk factors for nonunion, risk factor analysis was performed by multivariate logistic regression analysis with a forward-backward stepwise procedure (P < 0.1 for entry). Then, odds ratios and their approximate 95% confidence intervals for nonunion were calculated. For continuous variables, the odds ratio reflects the incremental risk associated with a one-unit change in that variable. To assess the cut-off point, a receiver operating characteristic analysis was conducted. For all statistical analyses, JMP version 12 (SAS Institute, Cary, NC), EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), and a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria)10,11 were used. We imputed the missing data measurements with data obtained by the Multiple Imputation by Chained Equations package in R. We chose 20 iterations for multiple imputation. All tests were two-sided, and P values < 0.05 were considered significant.
RESULTS
A total of 166 patients with 48 weeks of follow-up were included in this study. The reasons for patient exclusion are shown in Figure 2. Of the 166 patients analyzed in the present study, 29 (17.5%) were diagnosed with nonunion. The baseline characteristics of the patients are shown in Table 1. There were no significant differences between the two groups in any of the background variables. In particular, regarding the effect of brace treatment on bony union, there were no significant differences in the distribution of braces between the union and nonunion groups.
Figure 2.
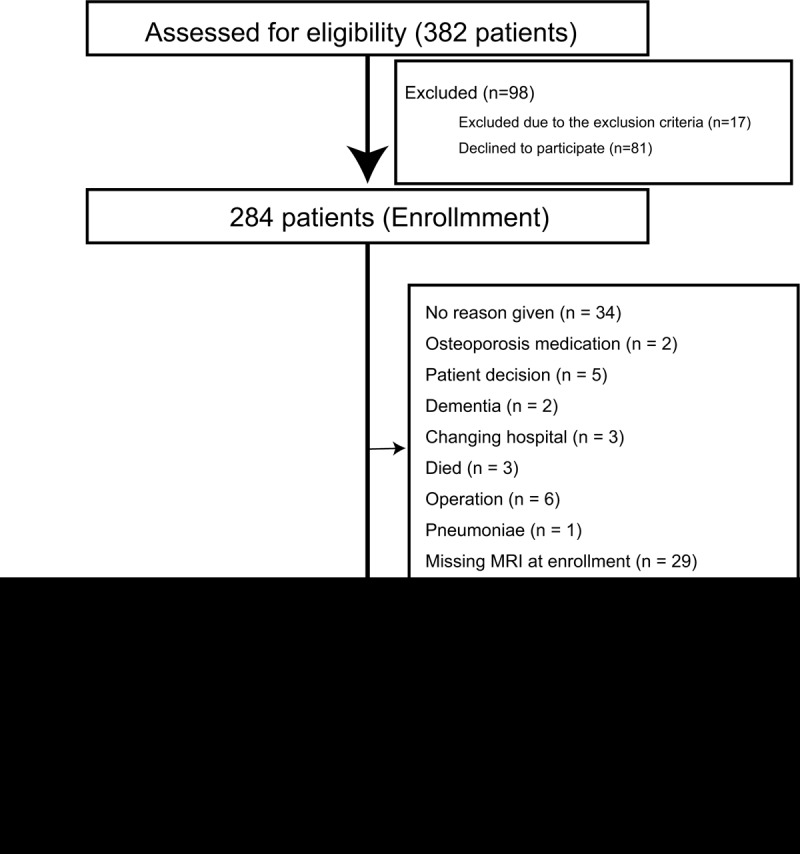
Participant flow through the study. During the study period, 382 patients were seen at hospitals due to OVFs. Eighty-one patients declined to participate in the study and 17 patients were excluded due to the exclusion criteria. Finally, 284 patients were enrolled in this prospective cohort study. An additional 118 patients were excluded during the follow-up period. OVF indicates osteoporotic vertebral fractures.
TABLE 1.
Baseline Characteristics of the Patients
| Characteristic | Union n = 137 | Nonunion = 29 | P |
| Mean age (SD), yrs | 75.3 (5.5) | 76.5 (5.1) | 0.28 |
| Mean time since fracture, wks | 1.4 (1.1) | 1.6 (0.9) | 0.14 |
| Patients under anti-osteoporotic treatment, n (%) | 33 (24) | 8 (28) | 0.81 |
| Previous vertebral fracture, n (%) | 25 (18) | 6 (21) | 0.79 |
| Ethnicity, n (%) | Asian 137 (100) | Asian 29 (100) | > 0.99 |
| Level, n (%) | 0.60 | ||
| T10 | 4 (3) | 0 (0) | |
| T11 | 9 (7) | 2 (7) | |
| T12 | 51 (37) | 15 (52) | |
| L1 | 46 (34) | 9 (31) | |
| L2 | 27 (20) | 3 (10) | |
| Type of brace | Rigid 69Soft 68 | Rigid 15Soft 14 | > 0.99 |
Table 2 shows the differences in the patient-reported outcome measures between the union and nonunion groups. At enrollment, there were no differences in any scores between the two groups. At 12 weeks, JOABPEQ social life function, mental health, and lumbar function scores were significantly lower in the nonunion group than in the union group (P = 0.03, 0.04, and 0.04, respectively). At 48 weeks, EQ-5D and JOABPEQ walking ability, social life function, mental health, and lumbar function scores were significantly lower in the nonunion group than in the union group (P = 0.01, 0.008, 0.049, 0.04, and 0.007, respectively).
TABLE 2.
Patient-reported Outcome Measures
| Measure | Union n = 137 | Nonunion n = 29 | P |
| EQ-5D | |||
| 0 | 0.26 (0.30) | 0.20 (0.25) | 0.38 |
| 12 wks | 0.72 (0.17) | 0.68 (0.21) | 0.20 |
| 48 wks | 0.77 (0.19) | 0.67 (0.18) | 0.01* |
| VAS low back pain | |||
| 0 | 74.1 (26.2) | 79.6 (23.7) | 0.32 |
| 12 wks | 26.1 (21.2) | 32.8 (28.8) | 0.37 |
| 48 wks | 25.0 (25.7) | 37.8 (30.5) | 0.06 |
| JOABPEQ | |||
| Pain-related disorder | |||
| 0 | 31.9 (31.3) | 26.2 (23.2) | 0.58 |
| 12 wks | 73.1 (29.6) | 67.3 (35.2) | 0.49 |
| 48 wks | 60.4 (29.4) | 48.9 (33.6) | 0.09 |
| Walking ability | |||
| 0 | 20.5 (28.4) | 9.9 (15.2) | 0.15 |
| 12 wks | 56.7 (33.1) | 44.5 (33.4) | 0.08 |
| 48 wks | 64.9 (33.0) | 47.3 (35.3) | 0.008* |
| Social life function | |||
| 0 | 21.9 (27.3) | 13.9 (20.4) | 0.26 |
| 12 wks | 55.0 (25.9) | 42.4 (29.5) | 0.03* |
| 48 wks | 63.3 (25.6) | 51.6 (29.4) | 0.049* |
| Mental health | |||
| 0 | 37.0 (22.5) | 38.6 (24.0) | 0.95 |
| 12 wks | 55.2 (18.8) | 47.2 (20.7) | 0.04* |
| 48 wks | 57.3 (19.0) | 48.3 (22.1) | 0.04* |
| Lumbar function | |||
| 0 | 19.4 (26.9) | 12.9 (21.8) | 0.44 |
| 12 wks | 60.4 (29.4) | 46.3 (34.4) | 0.04* |
| 48 wks | 69.5 (28.3) | 50.8 (35.2) | 0.007* |
*P < 0.05.
EQ-5D indicates European Quality of Life-5 Dimensions; JOABPEQ, Japanese Orthopaedic Association Back Pain Evaluation Questionnaire; VAS, visual analog scale.
Table 3 shows the differences in the radiographic data between the union and nonunion groups. The nonunion group had a significantly lower AVBCP than the union group at 0, 12, and 48 weeks (P = 0.02, <0.001, and <0.001, respectively). Regarding the MRI findings at enrollment, middle column injury, a diffuse low-intensity T1 image pattern, and fluid-intensity and diffuse low-intensity T2-weighted image patterns were frequently observed in the nonunion group (Table 3). Based on the possibility of nonunion occurrence in our study, we further classified the T2-weighted images into the following four ordinal categories: very low frequency (confined low), low frequency (diffuse high), intermediate frequency (diffuse low), and high frequency (fluid).
TABLE 3.
Radiographic Assessment
| Characteristic | Union (U) n = 137 | Nonunion (NU) n = 29 | P |
| AVBCP (SD) | |||
| 0 | 73.6 (12.7) | 67.5 (12.7) | 0.02* |
| 12 | 58.6 (14.8) | 47.0 (15.5) | <0.001* |
| 48 | 57.0 (15.4) | 43.2 (16.2) | <0.001* |
| MRI findings at enrollment (%) | |||
| Middle column injury | 54 (39) | 18 (62) | 0.04* |
| T1 | 0.01* | ||
| Confined low | 42 (31) | 2 (7) | |
| Diffuse low | 95 (69) | 27 (93) | |
| T2 | <0.001* | ||
| Confined low | 67 (49) | 5 (17) | |
| Diffuse high | 28 (20) | 4 (14) | |
| Diffuse low | 32 (23) | 10 (34) | |
| Fluid | 10 (7) | 10 (34) | |
*P < 0.05.
AVBCP indicates anterior vertebral body compression percentage.
As shown in Table 4, the risk factors for nonunion in the acute phase were evaluated using a stepwise multiple logistic regression analysis. Based on the univariate analysis, the dependent variable was defined as the presence of nonunion, and the independent variables were AVBCP, middle column injury, and MRI T1 and T2 findings at 0 weeks. As a result, the independent risk factors in the acute phase were identified as MRI T2 findings (compared with those with very low-frequency findings, patients with high-frequency findings had a higher incidence [odds ratio, 11.4, 95% confidence interval 3.3–44.7, P < 0.001]) and MRI T1 findings (compared with those with a confined low image pattern, patients with a diffuse low image pattern had a higher incidence [odds ratio, 4.42, 95% confidence interval 1.14–29.4, P = 0.03]). Next, based on the univariate analysis, the dependent variable was defined as the presence of nonunion, and the independent variables were the JOABPEQ walking ability score, JOABPEQ social life function score, JOABPEQ mental health score, JOABPEQ lumbar function score, and AVBCP at 12 weeks. As a result, the independent risk factors at 12 weeks were identified as the AVBCP (odds ratio = 0.95, 95% confidence interval 0.92–0.98, P < 0.001) and the JOABPEQ social life function score (odds ratio = 0.98, 95% confidence interval 0.96–0.998, P = 0.02).
TABLE 4.
Independent Risk Factors for Nonunion
| Independent Risk Factors for Nonunion | |||
| Variable | Odds Ratio | 95% Confidence Interval | P |
| 0 wks | |||
| MRI T1 finding | |||
| Confined low | 1.0 | Reference | |
| Diffuse low | 4.42 | 1.14–29.4 | 0.03* |
| MRI T2 finding | |||
| Very low frequency | 1.0 | Reference | |
| Low frequency | 1.81 | 0.41–7.46 | 0.41 |
| Intermediate frequency | 3.20 | 1.02–11.2 | 0.045* |
| High frequency | 11.4 | 3.3–44.7 | <0.001* |
| 12 wks | |||
| AVBCP | 0.95 | 0.92–0.98 | <0.001* |
| JOABPEQ social life function | 0.98 | 0.96–0.998 | 0.02* |
*P < 0.05.
AVBCP indicates anterior vertebral body compression percentage; JOABPEQ, Japanese Orthopaedic Association Back Pain Evaluation Questionnaire.
The cut-off values and their relevant sensitivity and specificity were predicted by receiver operating characteristic analysis. The area under the curve (AUC) indicated that the MRI T2 findings were the best indicators for nonunion. The cut-off value for the MRI T2 findings was the intermediate frequency. The AUC was 0.74 (P < 0.001). The sensitivity and specificity were 0.69 and 0.69, respectively. When a diffuse low-intensity image pattern on MRI T1 findings was used to predict nonunion, the AUC was 0.62 (P = 0.003), and the sensitivity and specificity were 0.93 and 0.31, respectively. The cut-off value for the AVBCP at 12 weeks was ≤ 46.7. The AUC was 0.71 (P < 0.001). The sensitivity and specificity were 0.59 and 0.77, respectively. The cut-off value for the JOABPEQ social life function score at 12 weeks was ≤ 27.0. The AUC was 0.63 (P = 0.02). The sensitivity and specificity were 0.38 and 0.86, respectively.
DISCUSSION
This study investigated the risk factors for nonunion at 48 weeks after acute OVFs. We found that middle column injury, a diffuse low-intensity T1-weighted image pattern on MRI, and fluid-intensity and diffuse low-intensity T2-weighted image patterns on MRI in the acute phase were frequently observed in the nonunion group. The nonunion group had a significantly lower AVBCP than the union group at 0, 12, and 48 weeks. At 12 weeks, the JOABPEQ social life function, mental health, and lumbar function scores were significantly lower in the nonunion group than in the union group. Furthermore, the nonunion group showed lower EQ-5D and JOABPEQ scores for walking ability, social life function, mental health, and lumbar function at 48 weeks than the union group. Finally, the stepwise multivariate logistic regression analysis showed that the independent risk factors for nonunion in the acute phase were a diffuse low-intensity T1-weighted MRI pattern and fluid-intensity and diffuse low-intensity T2-weighted MRI patterns. To the best of our knowledge, this study is the first to demonstrate that MRI findings could potentially be used to predict nonunion 48 weeks after OVFs.
Although previous studies reported that the incidence of delayed union at 6 months after OVF was in the range of 13.5% to 19.6%,5,6 there are, as far as we are aware, no reports that have investigated the incidence of nonunion (48 wk or longer after injury). Despite the fact that the results are not comparable due to differences in follow-up periods, our study showed that the nonunion incidence 48 weeks after OVF was 17.5%. To date, there is no universal criterion for the diagnosis of nonunion after OVF. The current study defined nonunion as a recognizable gas- or fluid-filled cleft separating the superior and inferior end plates on MRI and radiography at 48 weeks after injury. Although several studies investigated nonunion or delayed union via X-rays,3,5 basic research has shown that even dynamic X-rays are unable to accurately predict fusion outcomes for spinal fusion patients.12 Moreover, while bony union is usually assessed with computed tomography (CT), the use of CT causes a radiation dose effect for the patient.13 Because MRI correlates well with CT for identifying vertebral fracture union and nonunion,13 we used X-ray and MRI to assess the fracture union in this study. Indeed, the patients diagnosed with nonunion in this study showed significantly lower QOL, which is consistent with the symptoms of nonunion.14
Prospective cohort studies found that middle column injury and T2 high-signal changes showed a significant association with delayed union at 6 months after OVF.3,14 Our study also showed that the radiological risk factors for nonunion at 48 weeks after OVF in the acute stage were middle column injury, diffuse low-intensity T1-weighted MRI pattern, and fluid-intensity and diffuse low-intensity T2-weighted MRI patterns. Thus, our results are consistent with the results of previous studies in which the MRI findings in the acute phase can be predictive factors for deterioration in union status after OVFs.
Moreover, we identified that the AVBCP was an independent risk factor for nonunion at 12 weeks. Typically, vertebroplasty or kyphoplasty is considered for patients who have intractable, intense pain from OVF despite at least 6 weeks of conservative medical therapy.15 Thus, the impact of OVF on local spinal deformity formation has not been deeply considered as an indication of vertebroplasty or kyphoplasty instead of low back pain. In our study, while the AVBCP was significantly lower in the nonunion group, the VAS score for low back pain showed no significant differences between the two groups at the 12-week assessment. Expanding on our research, when considering the indications of vertebroplasty or kyphoplasty for patients at high risk of nonunion in the acute phase, physicians should take not only the VAS score for low back pain but also local spinal kyphosis into account.
Our study identified patient populations at high risk of nonunion. While a prospective study showed that initial conservative treatment did not affect patient outcomes,14 another study recently showed that teriparatide treatment more effectively prevented vertebral collapse and cleft formation after OVF than did risedronate treatment.16 Because bone anabolic agents such as parathyroid hormone and sclerostin antibodies have shown to improve fracture union in basic research,17,18 the application of these agents could be a potential alternative for patients with a high risk of nonunion. Further prospective research is necessary to investigate this treatment strategy. Moreover, a clinical study showed that a high tendency for bone resorption is a risk factor for nonunion after spinal fusion surgery;19 thus, comparing fluctuations in the levels of bone turnover markers between the union and nonunion groups may also be interesting.
This study has several limitations. First, a large number of patients (n = 118) were excluded after enrollment. Attrition bias might limit the internal validity of this study. However, attrition in cohort studies of older people does not inevitably indicate bias, as health and social difficulties develop with age.20 Second, because the patients in the present study were Japanese females of an advanced age, it might be difficult to apply these findings to males, other ethnicities, and a younger age group. As a result, more studies across genders, ethnicities, and age ranges are needed. These limitations should be validated in future prospective studies. On the other hand, we believe that our findings could be applied to elderly (65–85 yr old) Asian women. Third, we did not perform bone mineral density assessment. Although the severity of osteoporosis might affect fracture union, a lower bone mineral density does not necessarily reflect an impaired bone formation status. Indeed, a case control study showed that diminished bone quality does not influence the occurrence of nonunion.21
In conclusion, the present study demonstrated that a diffuse low-intensity T1-weighted MRI pattern and fluid-intensity and diffuse low-intensity T2-weighted MRI patterns in the acute phase were significant risk factors for nonunion at 48 weeks after OVF. Patients who have acute OVFs with these risk factors should be carefully monitored for nonunion.
Key Points
This prospective cohort study investigated the risk factors associated with nonunion at 48 weeks after OVFs.
Patients with nonunion after OVF had lower EQ-5D and JOABPEQ walking ability, social life function, mental health, and lumbar function scores than those with union at 48 weeks after injury.
The independent risk factors for nonunion were a diffuse low-intensity T1-weighted MRI pattern and fluid-intensity and diffuse low-intensity T2-weighted MRI patterns.
At 12 weeks after injury, the independent risk factors for nonunion after OVFs were a low anterior vertebral body compression percentage and a low JOABPEQ social life function score.
Acknowledgments
The authors thank Tomoko Nakajima for her help with data collection, Dr Makoto Tomita for his help with the statistical analysis, and Dr Ukihide Tateishi for his help with the radiological analysis. The authors also thank the doctors from Tokyo Medical and Dental University, Kyorin University, Nihon University, Osaka City University, Hamamatsu University of Medicine, Niigata University, University of Yamanashi, Kitasato University, Kurume University, St Marianna University, Hokkaido University, Fukushima Medical University School of Medicine, and their affiliated hospitals for enrolling patients in this prospective study.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
Grants-in-Aid from the Japan Agency for Medical Research and Development (grant number 16dk0110008h0003) funds were received in support of this work.
Relevant financial activities outside the submitted work: board membership.
References
- 1.van der Klift M, De Laet CE, McCloskey EV, et al. The incidence of vertebral fractures in men and women: the Rotterdam Study. J Bone Mineral Res 2002; 17:1051–1056. [DOI] [PubMed] [Google Scholar]
- 2.Kato T, Inose H, Ichimura S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med 2019; 8: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takahashi S, Hoshino M, Takayama K, et al. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: a multicenter cohort study. Osteoporos Int 2016; 27:3567–3575. [DOI] [PubMed] [Google Scholar]
- 4.Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 2010; 376:1085–1092. [DOI] [PubMed] [Google Scholar]
- 5.Tsujio T, Nakamura H, Terai H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976) 2011; 36:1229–1235. [DOI] [PubMed] [Google Scholar]
- 6.Kanchiku T, Imajo Y, Suzuki H, et al. Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech 2014; 27:E61–E65. [DOI] [PubMed] [Google Scholar]
- 7.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 1990; 16:199–208. [DOI] [PubMed] [Google Scholar]
- 8.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med 1988; 18:1007–1019. [DOI] [PubMed] [Google Scholar]
- 9.Fukui M, Chiba K, Kawakami M, et al. JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions. April 16, 2007. The Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orhop Sci 2009; 14:348–365. [DOI] [PubMed] [Google Scholar]
- 10.Ihaka R, Gentleman R. R: A Language for Data Analysis and Graphics. Journal of Computational and Graphical Statistics 1996; 5:299–314. [Google Scholar]
- 11.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013; 48:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sugiyama S, Wullschleger M, Wilson K, et al. Reliability of clinical measurement for assessing spinal fusion: an experimental sheep study. Spine (Phila Pa 1976) 2012; 37:763–768. [DOI] [PubMed] [Google Scholar]
- 13.Warwick R, Willatt JM, Singhal B, et al. Comparison of computed tomographic and magnetic resonance imaging in fracture healing after spinal injury. Spinal Cord 2009; 47:874–877. [DOI] [PubMed] [Google Scholar]
- 14.Hoshino M, Tsujio T, Terai H, et al. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2013; 38:E641–E648. [DOI] [PubMed] [Google Scholar]
- 15.Kendler DL, Bauer DC, Davison KS, et al. Vertebral fractures: clinical importance and management. Am J Med 2016; 129:221.e1–10. [DOI] [PubMed] [Google Scholar]
- 16.Tsuchie H, Miyakoshi N, Kasukawa Y, et al. The effect of teriparatide to alleviate pain and to prevent vertebral collapse after fresh osteoporotic vertebral fracture. J Bone Mineral Metabolism 2016; 34:86–91. [DOI] [PubMed] [Google Scholar]
- 17.Takahashi A, Mulati M, Saito M, et al. Loss of cyclin-dependent kinase 1 impairs bone formation, but does not affect the bone-anabolic effects of parathyroid hormone. J Biological Chem 2018; 293:19387–19399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Florio M, Gunasekaran K, Stolina M, et al. A bispecific antibody targeting sclerostin and DKK-1 promotes bone mass accrual and fracture repair. Nat Commun 2016; 7:11505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inose H, Yamada T, Mulati M, et al. Bone turnover markers as a new predicting factor for nonunion after spinal fusion surgery. Spine (Phila Pa 1976) 2018; 43:E29–E34. [DOI] [PubMed] [Google Scholar]
- 20.Lacey RJ, Jordan KP, Croft PR. Does attrition during follow-up of a population cohort study inevitably lead to biased estimates of health status? PLoS One 2014; 8:e83948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Wunnik BP, Weijers PH, van Helden SH, et al. Osteoporosis is not a risk factor for the development of nonunion: a cohort nested case-control study. Injury 2011; 42:1491–1494. [DOI] [PubMed] [Google Scholar]


