Abstract
Background.
Despite the risk of developing posttraumatic stress disorder (PTSD) and associated comorbidities after physical injury, few Emergency Departments (ED) in the United States screen for the presence of psychological symptoms and conditions. Barriers to systematic screening could be overcome by using a tool that is both comprehensive yet brief. This study aimed to determine 1) the feasibility of screening for posttraumatic sequelae among adults with minor injury in the ED, and 2) the relationship between ED screening and later psychological symptoms and poor quality of life (QOL) at 6 weeks post-injury.
Methods.
In the EDs of two Level 1 trauma centers, we enrolled injured patients (n = 149) who reported serious injury and/or life threat in the past 24 hours. Subjects completed the Posttraumatic Adjustment Scale (PAS) to screen for PTSD and depression in the ED, and 6 weeks later they completed assessments for symptoms of PTSD, depression, and Trauma-Specific QOL (T-QoL).
Results.
Our retained sample at 6 weeks was 84 adults (51.2% male; M age = 33); 38% screened positive (+) for PTSD, and 76% screened positive for depression in the ED. Controlling for age, hospital admission, and ED pain score, regression analyses revealed that a (+) ED screen for both PTSD and depression was significantly associated with 6 weeks PTSD (p = 0.027, 95% confidence interval [CI] = 0.92–15.14) and depressive symptoms (p = 0.001, 95% CI = 2.20–7.74), respectively. Further, a (+) ED screen for depression (p = 0.043, 95% CI= −16.66 to −0.27) and PTSD (p = 0.015, 95% CI = −20.35 to −2.24) was significantly associated with lower T-QoL.
Conclusions.
These results suggest that it is feasible to identify patients at risk for post-injury sequelae in the ED; screening for mental health risk may identify patients in need of early intervention and further monitoring.
Keywords: Posttraumatic stress disorder, depression, quality of life, screening, emergency department
INTRODUCTION
Traumatic injury is a leading cause of mortality and morbidity in the United States1,2, and approximately 29% of annual Emergency Department (ED) visits are attributable to physical injury3. The majority of these injures are mild, with only 7% requiring hospital admission4. However, the stress of injury can lead to alterations in the psychological processing of the event and in the perception of pain, independent of tissue damage5. Psychological sequalae including depression and anxiety are common after trauma exposure6–8. Research conducted among hospitalized injury populations suggests that up to 31% report a psychiatric disorder one year post-injury, with 22% of these being new diagnoses9. Posttraumatic Stress Disorder (PTSD) and depression are particularly common, with rates of PTSD at 12-months post-injury ranging from 6% - 29%, and rates of depression at 12-month post-injury ranging from 9% - 28%9–11. Further contributing to a complicated recovery process, early psychiatric symptoms after trauma are associated with lower health-related quality of life (QOL) and long-term disability12,13. Notably, post-injury psychiatric symptoms (including anxiety, depressive and posttraumatic stress symptoms) are a major contributor to disability over time, above and beyond physical factors and pain severity14.
Regarding recovery after minor injury, Pacella and colleagues previously found that psychological symptoms are associated with physical symptoms among ED patients discharged home immediately from the ED; specifically, hyperarousal symptoms of PTSD are associated with daily pain during the first 14 days after injury15. Similarly, patients with mild-moderate motor vehicle crash (MVC)-related injuries report reduced health-related QOL at 2-years post-MVC12, and at least one psychiatric diagnosis (50%) at 6-, 12-, and 24-months post-MVC16. Despite these associations, patients with minor physical injuries that do not require hospitalization receive little or no psychological support services, and few studies have enrolled and monitored ED subjects to determine their health risk after minor injury. Thus, there may be an underused opportunity for interventions to prevent chronic pain and PTSD after trauma, but instruments are needed to identify patients most at risk.
Few studies examine risk factors for developing post-injury PTSD and/or depression in ED patients. Although multiple validated ED screening tools are available for assessing PTSD and depression in pediatrics17,18, no tools exist to identify adults at risk for posttraumatic symptoms during the initial hours after trauma. Barriers to systematic screening could be overcome by using a tool that is both comprehensive yet brief. In hospitalized adults, the Posttraumatic Adjustment Scale (PAS) is a brief (10-item) screening instrument that predicts subsequent PTSD and depression, with sensitivities of 0.82 and 0.72 for PTSD and depression, respectively19. An advantage of the PAS is that it assesses three general categories of risk: 1) pre-trauma items reflecting psychiatric and trauma history, and social support; 2) peri-trauma items reflecting the response to and severity of the event; and 3) post-trauma items reflecting acute pain, cognitive response, coping self-efficacy, and social support.
Current Study. Consistent with prior research determining feasibility and effectiveness for ED-based screening programs20, our study objectives are two-fold: we aim to determine 1) the feasibility of screening for posttraumatic sequelae among adults with minor injury in the ED, and 2) the relationship between psychosocial risk screening in the ED and symptoms of PTSD, depression and quality of life at 6 weeks post injury. We included patients who perceived their trauma to be serious irrespective of the actual physical injuries identified. Our primary outcomes were PTSD symptoms (PTSS) and depressive symptoms at 6 weeks post-injury. Given the association between posttraumatic symptoms and QOL, we included the secondary outcome of trauma-specific Quality of Life (T-QoL), assessed using an instrument specifically designed to evaluate QOL in patients with physical injury21. We hypothesized that ≥ 75% of patients approached in the ED will agree to psychological screening; and 2) a positive ED screening will be associated with elevated symptoms of PTSD and depression, and with reduced QOL at 6 weeks post-injury.
METHODS
Participants
We conducted an observational, prospective, cohort study of adults admitted within 24 hours of injury to the EDs of two Level 1 trauma centers between January 2016 and May 2017. Eligible patients met the following criteria: 1) suffered a physical injury (e.g. MVC, general trauma, fall, assault, etc.) within the past 24 hours; 2) were between the ages of 18 and 60; 3) were medically and emotionally stable to understand and provide medical consent; 4) were not being treated primarily for a mental health or substance use issue directly related to the injury (e.g., MVC related to alcohol abuse); 5) did not present with self-inflicted injury or suicidal thoughts; 6) did not have a neurological disease (e.g., seizure disorder, stroke, multiple sclerosis); and 7) met criterion A of the PTSD diagnosis (self-report of exposure to either actual or threatened death or serious injury) per the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5)22. We excluded patients who had a physical injury that was caused by a medical condition (e.g. MVC caused by syncope). Further, given our focus on ED patients with minor injury for this analysis, we excluded patients who were hospitalized for >1 day.
Procedures
The Human Research Protection Office of the University of XX approved all procedures. Recruitment occurred primarily during weekdays from afternoon to early evening based on research assistant (RA) availability and highest ED volume. The RA identified potential participants through the ED tracking board based on chief complaint (e.g. fall, crush, MVC, trauma), age and time in the ED. After this initial screen, the patient care team (physician, nurse, physician assistant, resident) provided a second screen for eligibility of the patient (e.g., confirming the patient was alert and stable), and obtained patient permission for the RA to introduce the study. The RA approached potential subjects in their treatment rooms to confirm eligibility (e.g., event happened within 24 hours and the patient endorsed perceived or actual serious injury or threat of death), obtain informed written consent, and complete baseline instruments.
Participants completed demographic information and baseline instruments on an iPad using REDCap23. Baseline instruments included the PAS, and instruments completed at 6 weeks post-injury included the PTSD Symptom Checklist (PCL), the 8-item Patient Health Questionnaire depression scale (PHQ-8), and the Trauma-specific quality of life (T-QoL) questionnaire. We emailed participants a link to complete the 6 weeks follow up assessment; for those who did not have access to a computer, the RA completed assessments with the participants over the phone. We paid participants $10 for the completion of the baseline assessment and $10 for completion of the 6 weeks follow-up assessment.
Measures
ED assessment
Demographic Information.
Participants completed demographic questions at baseline: age, sex, race (coded as White, African American, and Other), and educational background (coded as High school/GED or less, some college/technical or vocational school, college degree or higher education, and declined to answer).
Psychological History.
Participants self-reported their psychological history at baseline by answering yes/no to the question “Has there ever been a point in your life when you received help for emotional or mental health problems?”
Medical Record Review.
We abstracted the chief complaint/mechanism of injury (later recoded as MVC-related, fall, work, or general accident [e.g., sports, minor trips, interpersonal physical assault, etc.]), type of injury (later coded into 6 categories reflecting contusions, sprains and strains, fractures and dislocations, open wounds, crushing injury, and burns), injury location (e.g., head and neck, extremities, spine and back, and torso), and the initial ED pain severity score (ranging from 0–10) from the medical chart. The ED pain score was not available for 13 participants for varied reasons (e.g., no pain assessment conducted or only after medication administration). We used the discharge pain score (n = 6) and the admission pain score (n = 2) when available for 8 of these participants, resulting in 79 participants with complete ED pain score data and 5 participants with incomplete/missing data for ED pain score.
Baseline Assessment in ED: Predictors
PTSD and Depression.
Participants completed the PAS, a 10-item survey including pre-trauma, peri-trauma, and post-trauma risk factors used to screen for the risk of developing PTSD and depression after acute trauma19 (Figure 1). Each of the 10-items are scored on a Likert scale ranging from 0 (“Not at all”) to 4 (“Totally”). The PAS-PTSD score is calculated by summing all 10 items and applying a cutoff score of 16. The PAS- depression score is calculated by summing 5 of the 10 items and applying a cutoff score of 4 (see O’Donnell19 for detailed scoring procedures). Cronbach’s alpha in our sample was acceptable for the PAS-depression (a = 0.70) and PAS-PTSD subscales (a = 0.82).
Figure 1.
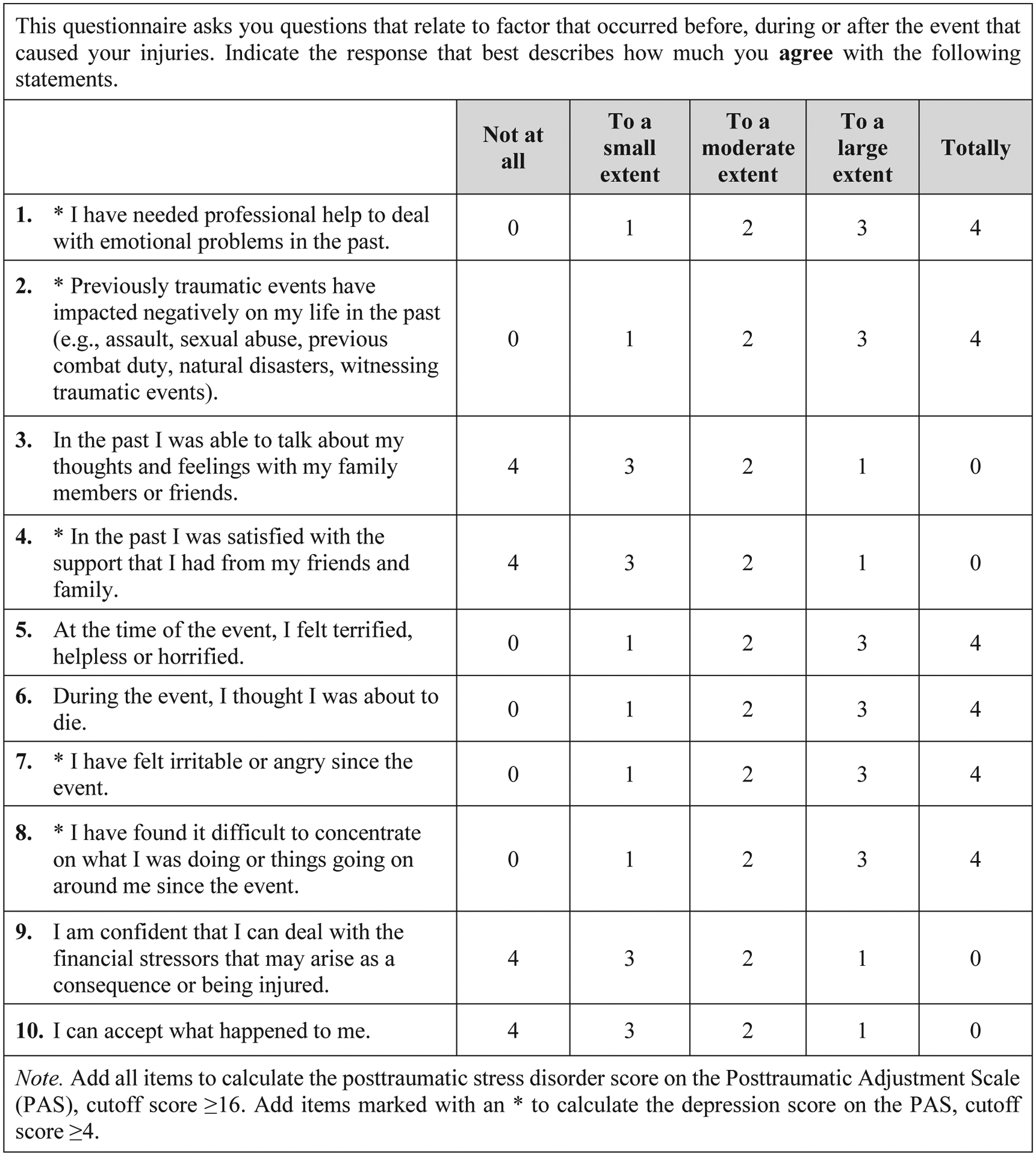
The Posttraumatic Adjustment Scale (Reproduced Figure+)
+Used with permission from O’Donnell, M. L., Creamer, M. C., Parslow, R., Elliott, P., Holmes, A. C., Ellen, S., … & Bryant, R. A. (2008). A predictive screening index for posttraumatic stress disorder and depression following traumatic injury. Journal of Consulting and Clinical Psychology, 76(6), 923.
Six-weeks post-injury assessment: Outcomes
Psychiatric Symptoms.
Participants completed the DSM-5 PCL and PHQ-8 to assess the symptoms and presence of possible PTSD and major depressive disorder, respectively. The PCL is a 20-item self-report measure that assesses DSM-5 PTSS24. The items are summed together to provide a continuous measure of PTSS severity with a total score ranging from 0 to 80, and a cut-point of ≥30 (internal consistency was high in our sample, α=0.96). The PHQ-8 is a valid severity scale for depressive symptoms composed of 8-items that are summed to obtain a total score from 0 to 24, with a cutoff value ≥10 (internal consistency was high in our sample, α=0.91)25.
QOL.
Participants completed the 43-item T-QoL survey21, specifically created for a traumatized population. The T-QoL has a 5-component structure with subscales that assess emotional well-being (16 items), functional engagement (8 items), recovery/resilience (6 items), peri-traumatic experience (5 items), and physical well-being (8 items). Response options for each item of the T-QoL are presented as a 4-choices (for 41 questions) and 5-choices (for 2 questions in the peritraumatic experiences subscale) Likert scale; however, to maintain consistency and allow for ease of administration to participants, we used a modified version that excluded the fifth response option for both items of the peritraumatic scale; this resulted in removing the “neutral” response option in the scale ranging from 0 (strongly disagree) to 4 (strongly agree); in this way, the 4 choices reflected the same response options for the remaining items in the entire scale. We summed the responses to create a single numerical measurement of total QOL, with a higher score indicating better T-QoL (internal consistency was high, α=0.91). Example items include: “I currently have physical limitations”; “I have trouble sleeping at night”; and “I felt fear when I was injured.”
Statistical Analysis
We used SPSS version 24.026 for statistical analyses; significance was defined using an alpha level of 0.05. We described the frequency of positive PTSD and depression screenings in the ED and probable rates of PTSD and depression at 6 weeks post-injury. We used analysis of variance (ANOVA) to determine whether there were any group differences based on sex in the outcomes of PTSS, depression symptoms and QOL at 6 weeks. We also measured the strength and direction of linear relationships between continuous variables (e.g., ED pain score, age, PCL, PHQ-8 and T-QoL) using Pearson correlations.
We used Pearson chi-square to test for associations between participant retention at 6 weeks and categorical variables of sex, race, hospital admission, and positive ED screen. ANOVA tested whether retention was associated with age and ED pain score.
For our primary analyses, we created separate hierarchical linear regression models to examine the PAS-PTSD score as a predictor of 1) 6-week PTSS and 2) T-QoL. Similarly, two additional models were conducted to examine the PAS-depression score as a predictor of 1) 6-week depression symptoms and 2) T-QoL. Variables with a significant association with the predictors or outcomes were used as covariates.
The basic assumptions were tested before conducting each of the ANOVA, chi-square and hierarchical regression analyses27–29. With one exception for regression analyses (see results section), all assumptions were satisfied.
Sample Size and Power.
Using GPower version 3.130, we calculated the sample size required for a linear multiple regression test of the increase in variance explained in the outcome due to the inclusion of the predictor variable (PAS screen), above and beyond the effects of 3 covariates, given α = 0.05 and a medium effect size (f2 = 0.15). for a power of 0.90, total sample size required for this test is N = 73; given that our retained sample size (N = 84) is higher than the target value, power was adequate for these models.
RESULTS
We approached 534 patients in the ED, of whom 148 refused to be screened (28%). Of those who refused, 38 (26%) did not agree to talk to the RA or wish to hear about the study, 61 (41%) were not interested in participating after a brief description by the RA, 32 (22%) stated that they were in too much pain to participate, 7 (5%) had no time to commit to the study, 8 (5%) were not willing to complete the surveys, and 2 (1%) stated that the compensation was too low. A total of 386 patients (72%) agreed to be screened for the study, and of those screened, 213(55%) were not eligible. Of those ineligible, 201 (94%) did not report exposure to threatened death or actual or serious injury (Criterion A of the PTSD diagnosis), and 12 (6%) subjects were injured ≥ 24 hours prior to ED admission. Of the 173 eligible patients, 154 completed baseline data prior to discharge, and 91 (59%) completed the follow-up survey at 6 weeks post-injury. Of the latter subjects, five patients were excluded for the following reasons: physical injury secondary to a medical condition (n = 4), illiteracy (n = 1), and hospital admission >1 day (n = 4).
Our final retained sample (N = 84) included nearly equal proportions of males and females of predominantly white race (Table 1). Participants reported a high ED pain score and the most common mechanism of injury was general accident. Eight patients (9%) were admitted to the hospital for their injuries for one day only (primarily for observation or minor procedures). Half of the sample (n = 42) reported receiving help for emotional or mental health problems in the past. Contusion was the most common type of injury (32%) and it was frequently located on head and neck (55.5%) and extremities (37%). Sprains and strains (29.8%), and fractures and dislocations (23.8%) were also common; other type of injuries were open wounds, crushing injuries, and burns. All participants reported threat of serious injury (eligibility criterion) and approximately one-third reported threat of death. Males (52% retained) were less likely than females (71% retained) to complete the 6-week assessment (χ2 (1) = 5.05; p = 0.025). Subjects who screened positive for depression in the ED were more likely to complete the 6-week assessment (66% compared to 46%) (χ2 (1) = 5.29; p = 0.021). Retention rates did not differ by race, hospital admission, or positive PTSD ED screening.
Table 1.
Descriptive statistics of the final sample (N = 84)
| Demographics | N (%) Mean (SD) |
|---|---|
| Age | 33 (11.88); Range 18–60 |
| Sex | |
| Male | 43 (51%) |
| Female | 41 (49%) |
| Race | |
| Caucasian | 46 (55%) |
| African American | 27 (32%) |
| Other | 11 (13%) |
| Education | |
| High school/GED or less | 35 (42%) |
| Some college/technical or vocational school | 33 (39%) |
| College degree or higher education | 13 (15%) |
| Declined to answer | 3 (4%) |
| ED Pain Score | 6.90 (2.64); Range 1–10 |
| Hospital Admission | |
| Admitted to hospital | 8 (9%) |
| Discharged from ED | 76 (91%) |
| Mechanism of Injury/Chief Complaint variables | 20 (24%) |
| Motor-vehicle crash | 20 (24%) |
| Falls | 14 (17%) |
| Work-related accident | 30 (35%) |
| General Accidents | |
| Type of injury | |
| Contusion | 27 (32.1%) |
| Sprain/Strain | 25 (29.8%) |
| Fracture/Dislocation | 20 (23.8%) |
| Open wound | 9 (10.7%) |
| Crushing injury | 2 (2.4%) |
| Burn | 1 (1.2%) |
| Received pre-injury help for emotional or mental health problems | 42 (50%) |
Note. Continuous variables are presented as Mean (SD), dichotomous variables are presented as n (%). SD = Standard deviation; ED= Emergency Department; GED= General Education Diploma; PTSD= Posttraumatic Stress Disorder.
ED Screening.
We screened a total of 155 patients in the ED, of whom 37% (n = 58) screened positive for PTSD and 67.7% (n = 105) for depression. Of the final sample retained at 6 weeks post-injury, 38% (n = 32) screened positive for PTSD and 76% (n = 64) for depression (Figure 2).
Figure 2.
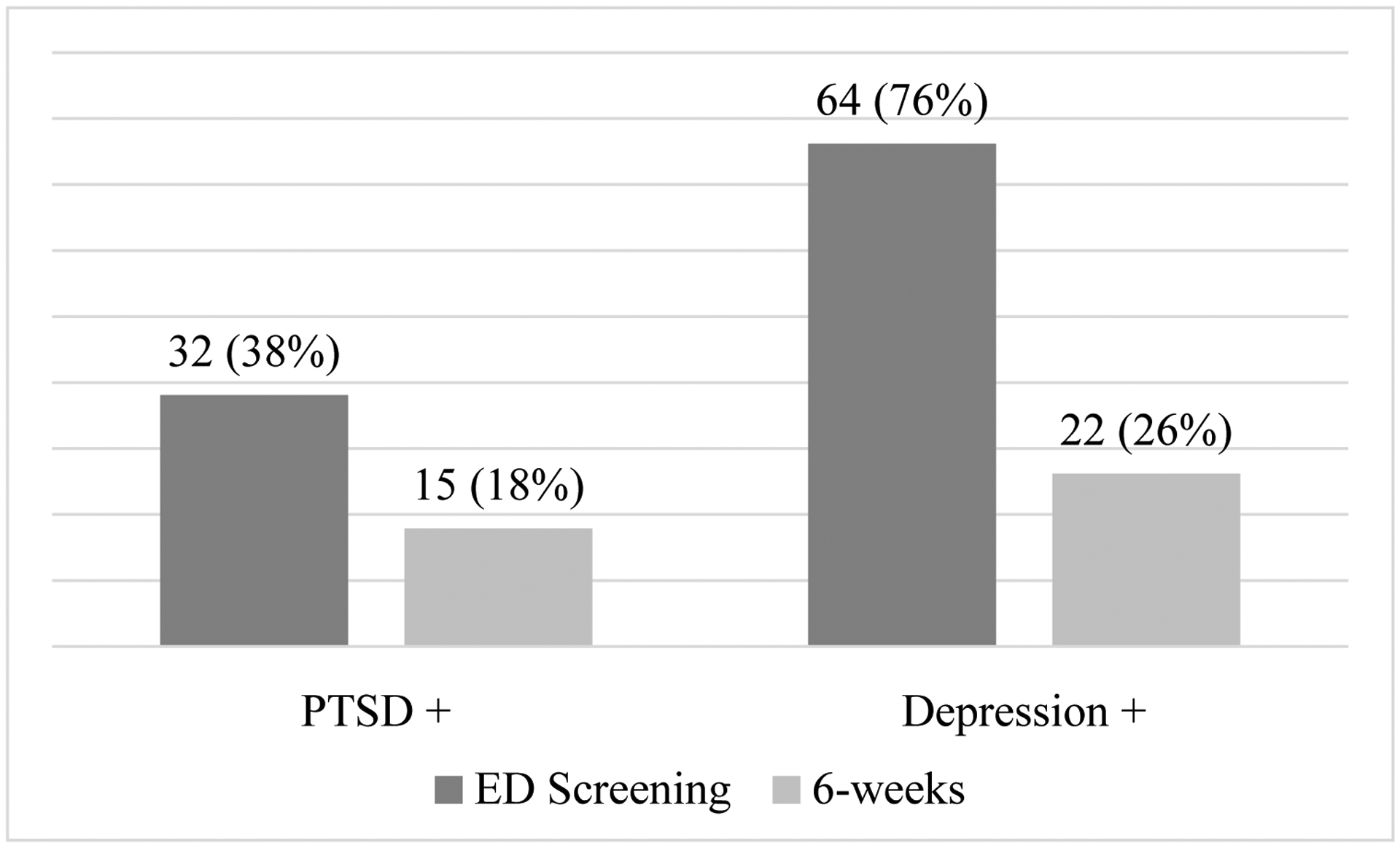
Rates of PTSD and Depression in the ED and at 6 weeks post-injury (N = 84).
PTSD= Posttraumatic Stress Disorder; ED= Emergency Department; PTSD + = PTSD Positive; Depression + = Depression Positive.
Outcomes.
At 6 weeks, 18% (n = 15) of participants scored above the cutoff for probable PTSD via the PCL, and 26% (n = 22) for probable depression via the PHQ-8. Hospital admission (n = 8) was associated with T-QoL, such that patients admitted to the hospital reported lower QOL (M = 115.37; SD = 21.22) than those not admitted to the hospital (M = 133.21; SD = 20.48); F = 5.45; p = 0.02).
ED pain score (Table 2) was positively correlated with poorer outcomes, older age was associated with greater depressive symptoms and poorer QOL There were no sex differences in T-QoL, PCL and PHQ-8 scores at 6 weeks post-injury (p’s ≥ 0.2), but hospital admission was significantly associated with poorer QOL.
Table 2.
Pearson correlations (N = 84).
| Variables | Age | Pain Score | Time since Injury | 6-week PTSS | 6-week Depressive Symptoms |
|---|---|---|---|---|---|
| Age | - | - | - | - | - |
| Pain score | 0.048 | - | - | - | - |
| 6-week PTSS | 0.197 | 0.250* | 0.178 | - | - |
| 6-week Depressive symptoms | 0.232* | 0.304** | 0.292** | 0.742** | - |
| 6-week QOL | −0.313** | −0.405** | −0.101 | −0.661** | −0.633** |
Note.
p <.05;
p <.01.
Note: 6-week PTSS assessed with the PCL; 6-week Depressive symptoms assessed with the PHQ-8. PTSS= Posttraumatic Stress Symptoms; QOL= Quality of Life.
Primary Regression Analyses (Table 3).
Table 3.
Summary of hierarchal regression analysis demonstrating the association of positive screening with development of PTSD symptoms at 6 weeks (N = 84).
| Variables | B | SE B | 95% CI | p-value | ΔR2 |
|---|---|---|---|---|---|
| Outcome: 6-week PTSD Symptoms | |||||
| Step 1: | 0.13 | ||||
| Age | 0.20 | 0.14 | [−0.02, 0.55] | 0.069 | |
| Hospital Admission | 0.17 | 6.05 | [−2.55, 21.53] | 0.121 | |
| ED Pain Score | 0.26 | 0.65 | [0.24, 2.84] | 0.021 | |
| Step 2: | 0.06 | ||||
| Age | 0.16 | 0.14 | [−0.70, 0.49] | 0.138 | |
| Hospital Admission | 0.13 | 5.96 | [−4.46, 19.29] | 0.217 | |
| ED Pain Score | 0.21 | 0.64 | [−0.02, 2.56] | 0.054 | |
| PTSD + Screen in ED | 0.24 | 3.56 | [0.92, 15.14] | 0.027 |
Note: B= standardized beta coefficient; SE B = standard error of B. PTSD= Posttraumatic Stress Disorder; ED= Emergency Department; PTSD + Screen= PTSD Positive screen.
Controlling for age, hospital admission, and ED pain score. A positive ED screening for PAS-PTSD was associated with PTSS at 6 weeks (B = 0.24, p = 0.027), and a positive ED screening for PAS-depression was associated with PHQ-8 score at 6 weeks (B = 0.36, p = 0.001). A positive ED screening for PAS-PTSD (B = −0.19; p = 0.043) and PAS-depression (B = −0.23, p = 0.015) was associated with lower T-QoL score at 6 weeks post-injury. The assumption of homoscedasticity was violated by the presence of 2 outliers with residual values >2 for the outcome of PTSS; however, upon excluding these subjects and repeating the analysis, the results remained unchanged. Therefore, we retained these individuals to maintain integrity of the data.
DISCUSSION
Consistent with our hypothesis, our data suggest that it is feasible to screen and identify ED patients at risk for post-injury psychological sequalae within 24 hours of minor physical injury. Specifically, >70% of patients approached about this research study agreed to be screened for eligibility, and 88% of eligible patients agreed to participate. The primary reason for ineligibility was no self-reported life threat or actual or threatened serious injury, consistent with the notion that we attempted to approach patients with minor injury who were likely to be discharged directly home from the ED. Further, high rates of positive ED screens for PTSD and depression emerged from the PAS: 38% of our sample screened positive for PTSD, and 76% screened positive for depression in the ED.
Similar findings regarding positive PTSD screens in ED patients have been reported by Downey and colleagues17 (35% of their sample of children and adults) and by Richmond and colleagues31 (36% of adults with minor injuries); higher rates (48.9%) were reported by Hunt and colleagues32 in hospitalized trauma patients. Characteristic symptoms of PTSS include intrusions (e.g., nightmares, flashbacks, etc.), avoidance of injury-related reminders, negative alterations in cognitions and emotions, and altered physiological arousal and reactivity22. The presence of these symptoms may negatively impact functioning and recovery, even in the absence of meeting criteria for full PTSD33,34. Two recent studies also highlight the critical impact of early post-injury PTSD on long-term psychological recovery. First, among an Australian cohort of patients injured in road traffic crashes, those with an early diagnosis of PTSD (rather than depression or anxiety) were significantly more likely to report a psychological diagnosis at 2-years post-injury35. Next, among hospitalized injury patients, those who reported at least subsyndromal PTSD at 3-months post-injury were significantly more likely to report poor QOL at 12-months compared to those who never developed PTSD, even after controlling for preinjury QOL, pain, and depression36.
Regarding depression risk, this sample screened positive for depression at a much higher rate (76%) than reported in previous studies conducted among ED patients with minor injuries31 and hospitalized trauma adults32 (37–44%). The presence of depressive symptoms after injury further complicates recovery and may contribute to poor QOL and long-term disability14,37. Our ED screening rates may be higher given the brief period of time that had passed between the injury and symptom assessment; symptoms are naturally high immediately post-injury and tend to diminish over time. A probable explanation also resides in the nature of the PAS screening tool; whereas all 10 items are used to create the PTSD risk score (with a cutoff of 16), five of these same items are used to calculate the depression risk score with a low cutoff of 4. Consequently, the PAS items may be more specific to PTSD than to depression risk. To this end, in the development of the PAS, O’Donnell and colleagues19 reported a low positive predictive value of 24% (i.e., the probability that a subject who screens positive for the disorder actually has the disorder), a limitation that likely contributes to our high positive screen rate. Further, the low cutoff score for depression compared to PTSD increases the sensitivity to screen positive for depression risk; namely, a patient must only endorse 1 item at the highest level (each item is scored 0–4) on the PAS to screen positive for depression. Given that half of the sample endorsed receiving help for mental health problems in the past (an item which overlaps with the first question on the PAS), it is likely that many patients met criteria for depression risk by endorsing this item alone. It is important to keep in mind that the PAS was designed to serve as a screener and identify those who may benefit from monitoring and reassessment; outcomes should be assessed via interview-administered gold-standard diagnostic tools to accurately estimate the utility of the screening instrument.
Our data also revealed that QOL is lower in individuals at risk for post-injury depression and PTSS, which is consistent with prior research that found a negative correlation between QOL scores and the presence of PTSS21. These findings along with previous data that displays the association between mental health and QOL with disability over time14, suggest that disability is not solely a consequence of physical insult but also of early psychological symptoms. This novel implementation of the T-QoL in ED patients showed utility in short-term assessments; further research is needed to examine its usefulness in long-term follow-ups.
We found that the covariate of hospitalization was related to QOL, but not with PTSS or depressive symptoms. Patients admitted to the hospital may have longer recovery periods and physical limitations that can lead to reduced functioning across both psychological and physical domains which are later reflected on lower QOL scores. This study also confirmed that ED pain score is an important factor to consider when assessing risk for mental health sequelae and QOL, even among patients with minor physical injury. Among hospitalized patients after a traumatic orthopedic injury, Archer et al.38 similarly found that increased pain at hospital discharge was associated with depression and PTSD.
Taken together, ED screening allows for the identification of those at risk for PTSD close to the point of injury, and provides an opportunity to monitor symptoms and administer interventions to prevent both psychological and physical health complications among a high-risk group. Although recent efforts on identifying risk factors for post-injury psychopathology has led to the development of predictive screeners to detect early psychological symptoms, research among acutely injured ED patients is limited. This lack of specificity among ED patients may be problematic given the many distinctions between hospitalized injured patients and those not requiring hospital admission, including the types of potentially traumatic events that contribute to hospitalization, the procedures likely involved in treatment for hospitalized patients, and the time between the event and assessment32.
Regarding screeners for hospitalized patients, Hunt et al.32 developed the Injured Trauma Survivor Screen, a nine-item binary (yes/no) response questionnaire ideal for a brief inpatient bedside evaluation of post-trauma PTSD and depression risk among hospitalized trauma patients. Although Richmond et al.31 developed and evaluated a screening tool for PTSD and depression designed for ED patients with minor injuries, the authors designed the scale to be administered to patients within two weeks post-trauma. It is not practical to administer this scale in the ED setting because some items would be difficult for ED patients to answer due to the proximal timing of the event to the assessment (e.g., “Has someone responded badly when you told them about what happened?” “Have you wanted to (or tried hard to) stay away from reminders of the event?” “Have you been staying away from people, even people you are usually close to?”). As such, the content of this survey limits its use in the acute setting given that the answers to these questions require additional processing time between the injury and the assessment of symptoms. Finally, although Mason et al.39 developed a brief screening tool for PTSD, depression and anxiety that is easy to administer in the acute setting, the high false positive rate led the authors to conclude that the tool was not cost effective or acceptable.
The majority of extant research in acute settings has tested established screeners for PTSD, as opposed to creating a new instrument for acute populations. Specifically, Walters and colleagues (2007) assessed the utility of the Trauma Screening Questionnaire (TSQ) in ED patients, but their sample was limited to assault-related injuries, and the TSQ should only be used three- to four-weeks post-trauma to allow for normal recovery processes to take place. Further, the TSQ only includes arousal and experiencing items; the avoidance cluster of DSM-IV is not represented40. Similarly, the brief 4-item Primary Care-Posttraumatic Stress Disorder screener has been used among patients hospitalized after acute injury41,42; however, this screener is anchored solely to post-trauma symptoms, provides a binary screen (yes/no) rather than assessing the severity of symptoms, and requires additional time for processing of the event (e.g., there is an item that asks about nightmares from the event).
Although ED patients not requiring hospitalization represent a significant proportion of injured patients and may benefit from further monitoring and follow-up care, these patients are often overlooked for psychological screening8. Consistent with prior research suggesting a weak and inconsistent relationship between the severity of injury and psychological consequences, a recent study among 460 patients admitted to a Level I trauma center revealed that no significant relationships emerged between injury severity score and symptoms of PTSD, depression, pain, and physical and mental health throughout 6-months post-injury43. These results support screening for PTSD in those treated in the ED, but whose injuries may not be sufficient to warrant hospitalization. However, the results of a 2014 trauma center survey conducted in Level I and II trauma centers throughout the United States (N = 391) revealed that early psychological screening procedures are lacking in general, as only 7% of trauma centers routinely screen for PTSD44. Moreover, psychological screening is often limited to: 1) the inclusion of hospitalized patients with severe trauma8 and 2) a focus on long-term outcomes (rather than acute outcomes) with follow-ups that occur months and years post-injury45,46.
In summary, existing screening tools do not assess pre- and peri-trauma risk factors and would not be practical to administer in ED patients to assess symptoms from the index injury. Our study built upon prior research by testing the utility of using the PAS among injured ED patients; the advantages of the PAS include its assessment of symptom severity to calculate risk and its inclusion of pre-, peri-, and post-trauma factors that can be used in close proximity to the index injury. The PAS also includes an item that reflects a history of psychological problems (factored into the risk score for both PTSD and depression), an important predictor variable of recovery after subsequent injury47–49. Further, our study extended prior research by including an assessment of risk for PTSD and depression within 24 hours post-injury among adults with any trauma-related chief complaint; we also reevaluated the presence of psychological symptoms at a short follow-up time frame after discharge (6 weeks), allowing for the early identification of individuals at risk who may benefit from acute intervention. Although the PAS was sufficient for identifying at-risk patients, future research is warranted to develop a screen specifically to meet the needs of ED patients.
Limitations.
Several limitations should be considered: As this was a feasibility study with limited personnel and compensation resources, our retention rate was low (59%), and therefore introduces the possibility of bias. Additionally, females and subjects with (+) ED screening for depression were more likely to be retained, and this may weaken the external validity of our results. Low retention has also been reported in prior behavioral studies performed in acutely injured patients, with dropout rates ranging from 41–50% among acute injury survivors with follow-up 4 to 12-weeks post-injury32,50. Given the myriad challenges that ED subjects are faced with after acute injury, this population requires a higher level of resources devoted specifically to retention51. In the context of low retention rate, small sample size, and wide confidence intervals, we caution that these results are preliminary, and must be replicated with larger samples with resources available to increase retention.
In addition, the PAS was designed to reflect the DSM-IV criteria and does not include the negative cognition and mood symptom cluster in DSM-5; an updated screener may be beneficial for more accurate assessments. Another important limitation is the short follow-up period to assess QOL. The construct of QOL may take longer than six weeks to evolve and its relationship with depression and PTSD may change over time; longer follow-up assessments would allow recognition of a better relationship between PTSS and QOL. Further, our primary outcomes of PCL and PHQ-8 are self-report and reflect the potential presence and severity of psychological symptoms; they cannot indicate a diagnosis. Finally, injury severity scores are not available for these patients; although the scores are likely low, future research among injured ED patients should consider adjusting for injury severity in models.
Despite these limitations, this is the first study to assess risk for depression and PTSD using the PAS in the acute setting of the ED after general injury, and to include mostly minor injuries which may be a good representation of the patients commonly seen in the EDs throughout the country. For example, 90% of MVC patients are not admitted to the hospital for their injuries52–54. Given the high rates of risk and posttraumatic psychological symptoms found in this study, it is worth further investigating the utility of routine screening during ED trauma care.
Early cognitive behavioral interventions such as education, exposure, cognitive restructuring, anxiety management, and even internet-virtual reality interventions show promise in the management of post-injury psychological symptoms55–59; further research is needed to determine efficacy, particularly among injured ED patients.
CONCLUSION
It is feasible to identify ED patients with minor injury at risk for future psychological effects of trauma using brief screens like the PAS in the ED. The early identification of individuals at risk may allow further monitoring of psychological symptoms and/or intervention, both of which may promote a better recovery and QOL. These results add to a growing literature demonstrating the importance of understanding the psychological and emotional responses that contribute to the processing of stress and pain after minor physical injury; our findings support and highlight the need for future research among larger samples of ED patients.
Table 4.
Summary of hierarchal regression analysis demonstrating the association of positive screening with development of depression symptoms at 6 weeks (N = 84).
| Variables | B | SE B | 95% CI | p-value | ΔR2 |
|---|---|---|---|---|---|
| Outcome: 6-week Depression Symptoms | |||||
| Step 1: | 0.17 | ||||
| Age | 0.23 | 0.53 | [0.01, 0.22] | 0.034 | |
| Hospital Admission | 0.18 | 2.20 | [−0.58, 8.21] | 0.088 | |
| ED Pain Score | 0.31 | 0.24 | [0.22, 1.17] | 0.005 | |
| Step 2: | 0.12 | ||||
| Age | 0.21 | 0.04 | [0.01, 0.20] | 0.035 | |
| Hospital Admission | 0.18 | 2.04 | [−0.19, 7.96] | 0.062 | |
| ED Pain Score | 0.23 | 0.22 | [0.07, 0.97] | 0.023 | |
| Depression + Screen in ED | 0.36 | 1.38 | [2.20, 7.74] | 0.001 |
Note: B= standardized beta coefficient; SE B = standard error of B. ED= Emergency Department; Depression + Screen= Depression Positive Screen.
Table 5.
Summary of hierarchal regression analyses demonstrating the association of positive PTSD and depression screening with quality of life at 6 weeks (N = 84).
| Variables | B | SE B | 95% CI | p-value | ΔR2 |
|---|---|---|---|---|---|
| Outcome: 6-week Quality of Life | |||||
| Step 1: Model #1 | 0.35 | ||||
| Age | −0.30 | 0.16 | [−0.85, −0.19] | 0.002 | |
| Hospital Admission | −0.33 | 6.93 | [−38.38, −10.76] | 0.001 | |
| ED Pain Score | −0.42 | 0.75 | [−4.86, −1.88] | 0.000 | |
| Step 2: | 0.03 | ||||
| Age | −0.26 | 0.16 | [−0.79, −0.14] | 0.006 | |
| Hospital Admission | −0.30 | 6.87 | [−36.07, −8.70] | 0.002 | |
| ED Pain Score | −0.38 | 0.74 | [−4.57, −1.59] | 0.000 | |
| PTSD + Screen in ED | −0.19 | 4.11 | [−16.66, −0.27] | 0.043 | |
| Step 2: Model #2 | 0.50 | ||||
| Age | −0.28 | 0.15 | [−0.81, −0.18] | 0.002 | |
| Hospital Admission | −0.33 | 6.70 | [−38.10, −11.38] | 0.000 | |
| ED Pain Score | −0.37 | 0.74 | [−4.45, −1.50] | 0.000 | |
| Depression + Screen in ED | −0.23 | 4.54 | [−20.35, −2.24] | 0.015 |
Note: Model #1 tests a positive PTSD screen as a predictor of QOL; Model #2 tests a positive depression screen as a predictor of QOL. Step 1 including the covariates is the same in both models. B= standardized beta coefficient; SE B = standard error of B. PTSD= Posttraumatic Stress Disorder; ED= Emergency Department; PTSD + Screen= PTSD Positive Screen; Depression + Screen= Depression Positive Screen.
Acknowledgments.
S.J. contributed to literature search, data interpretation, and writing. M.P-L. contributed to study design, literature search, data collection, analysis, data interpretation, writing, and revision. B.S. contributed to study design, writing, and revision. C.C. contributed to study design, writing, and revision. The authors acknowledge R. Kurtz, J. T. Kristen, J. M. Rupp, A. Keller, S. Diulus, D. Wang, and M. Kelly recruited and interviewed subjects for this study. R Kurtz also prepared the data for analysis.
Funding Sources. This project was supported by the Pittsburgh Emergency Medicine Foundation; and the use of REDCap was supported by the National Institutes of Health through Grant Number UL1TR001857.
Footnotes
Prior Presentations. This data was presented in 2018 at the 34th Annual Meeting of the International Society for Traumatic Stress Studies.
Disclosures. S.J., M.P-L., B.S., C.C. report no conflict of interest.
REFERENCES
- 1.Center for Disease Control and Prevention. WISQARS (Web-Based Injury Statistics Query and Reporting System). Choice Rev Online. 2011;48(08):48–4227-48–4227. doi: 10.5860/CHOICE.48-4227 [DOI] [Google Scholar]
- 2.National Trauma Institute. Trauma Statistics & Facts - National Trauma Institute. https://www.nattrauma.org/what-is-trauma/trauma-statistics-facts/. Published 2015. Accessed November 16, 2018.
- 3.Rui P, Kang K. National hospital ambulatory medical care survey: 2015 emergency department summary tables. Natl Cent Heal Stat. 2015. http://www.cdc.gov/nchs/ahcd/ahcd_survey_instruments.htm#nhamcs. [Google Scholar]
- 4.Villaveces A, Mutter R, Owens PL, Barrett ML. Causes of Injuries Treated in the Emergency Department, 2010: Statistical Brief #156. Rockville (MD); 2006. http://www.ncbi.nlm.nih.gov/pubmed/24006548. [PubMed] [Google Scholar]
- 5.McLean SA. The potential contribution of stress systems to the transition to chronic whiplash-associated disorders. Spine (Phila Pa 1976). 2011;36(25 Suppl):S226–32. doi: 10.1097/BRS.0b013e3182387fb4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abraham CM, Obremskey WT, Song Y, Jackson JC, Ely EW, Archer KR. Hospital delirium and psychological distress at 1 year and health-related quality of life after moderate-to-severe traumatic injury without intracranial hemorrhage. Arch Phys Med Rehabil. 2014;95(12):2382–2389. doi: 10.1016/j.apmr.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 7.Richmond TS, Kauder D. Predictors of Psychological Distress Following Serious Injury. J Trauma Stress. 2000;13(4):681–692. doi: 10.1023/A:1007866318207 [DOI] [PubMed] [Google Scholar]
- 8.Au EHK, Holdgate A. Characteristics and outcomes of patients discharged home from the Emergency Department following trauma team activation. Injury. 2010;41(5):465–469. doi: 10.1016/j.injury.2009.11.011 [DOI] [PubMed] [Google Scholar]
- 9.Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The Psychiatric Sequelae of Traumatic Injury. Am J Psychiatry. 2010;167(3):312–320. doi: 10.1176/appi.ajp.2009.09050617 [DOI] [PubMed] [Google Scholar]
- 10.Shih RA, Schell TL, Hambarsoomian K, Belzberg H, Marshall GN. Prevalence of Posttraumatic Stress Disorder and Major Depression After Trauma Center Hospitalization. J Trauma Acute Care Surg. 2010;69(6). https://journals.lww.com/jtrauma/Fulltext/2010/12000/Prevalence_of_Posttraumatic_Stress_Disorder_and.37.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zatzick D, Jurkovich GJ, Rivara FP, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8 [DOI] [PubMed] [Google Scholar]
- 12.Kenardy J, Heron-Delaney M, Warren J, Brown EA. Effect of mental health on long-term disability after a road traffic crash: Results from the UQ SuPPORT study. Arch Phys Med Rehabil. 2015;96(3):410–417. doi: 10.1016/j.apmr.2014.10.007 [DOI] [PubMed] [Google Scholar]
- 13.Antje Haagsma J, Scholten A, Andriessen T, Vos P, Beeck E, Polinder S. Impact of Depression and Post-Traumatic Stress Disorder on Functional Outcome and Health- Related Quality of Life of Patients with Mild Traumatic Brain Injury. Vol 32; 2014. doi: 10.1089/neu.2013.3283 [DOI] [PubMed] [Google Scholar]
- 14.O’Donnell ML, Varker T, Holmes AC, et al. Disability After Injury. J Clin Psychiatry. 2013;74(02):e137–e143. doi: 10.4088/JCP.12m08011 [DOI] [PubMed] [Google Scholar]
- 15.Pacella ML, Girard JM, Wright AGC, Suffoletto B, Callaway CW. The Association Between Daily Posttraumatic Stress Symptoms and Pain Over the First 14 Days After Injury: An Experience Sampling Study. Acad Emerg Med. 2018;25(8):844–855. doi: 10.1111/acem.13406 [DOI] [PubMed] [Google Scholar]
- 16.Kendrick D, Baker R, Hill T, et al. Early risk factors for depression, anxiety and post-traumatic distress after hospital admission for unintentional injury: Multicentre cohort study. J Psychosom Res. 2018;112:15–24. doi: 10.1016/j.jpsychores.2018.06.008 [DOI] [PubMed] [Google Scholar]
- 17.Downey LVA, Zun LS, Dismukes P, Hong A. Comparison of Self-Administered Post Traumatic Stress Disorder Tool vs. Researcher Administered Tool in the Emergency Department. J Natl Med Assoc. 2017;110(1):18–22. doi: 10.1016/j.jnma.2017.06.018 [DOI] [PubMed] [Google Scholar]
- 18.Schandorph Løkkegaard S, Rønholt S, Karsberg S, Elklit A. Validation of the PTSD screening cartoon test “Darryl” in a Danish clinical sample of children and adolescents. Int J Methods Psychiatr Res. 2016;26(1):e1514. doi: 10.1002/mpr.1514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Donnell ML, Creamer MC, Parslow R, et al. A Predictive Screening Index for Posttraumatic Stress Disorder and Depression Following Traumatic Injury. J Consult Clin Psychol. 2008;76(6):923–932. doi: 10.1037/a0012918 [DOI] [PubMed] [Google Scholar]
- 20.Kelen GD, Hexter DA, Hansen KN, et al. Feasibility of an emergency department-based, risk-targeted voluntary HIV screening program. Ann Emerg Med. 1996;27(6):687–692. doi: 10.1016/S0196-0644(96)70184-1 [DOI] [PubMed] [Google Scholar]
- 21.Wanner JP, deRoon-Cassini T, Kodadek L, Brasel K. Development of a trauma-specific quality-of-life measurement. J Trauma Acute Care Surg. 2015;79(2). https://journals.lww.com/jtrauma/Fulltext/2015/08000/Development_of_a_trauma_specific_quality_of_life.15.aspx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The American Psychiatric Association; Diagnostic and Statistical Manual of Mental Disorders. 5th ed Arlington, VA; 2013. [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weathers FW, Litz B, Keane TM, Palmieri PA, Marx BP, Achunurr PP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. www.ptsd.va.gov. Published 2013.
- 25.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- 26.IBM. IBM SPSS Statistics for Windows. 2016.
- 27.Gravetter FJ, Wallnau LB. Statistics for The Behavioral Sciences. Blemont, CA: Cengage Learning; 2016. https://books.google.com/books?id=ZCNTCwAAQBAJ. [Google Scholar]
- 28.Field A Discovering Statistics Using SPSS. London: SAGE Publications; 2009. https://books.google.com/books?id=a6FLF1YOqtsC. [Google Scholar]
- 29.George D, Mallery P. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 Update. 10th ed Boston: Allyn & Bacon; 2010. https://books.google.com/books?id=KS1DPgAACAAJ. [Google Scholar]
- 30.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- 31.Richmond TS, Ruzek J, Ackerson T, Wiebe DJ, Winston F, Kassam-Adams N. Predicting the future development of depression or PTSD after injury. Gen Hosp Psychiatry. 2011;33(4):327–335. doi: 10.1016/j.genhosppsych.2011.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hunt JC, Sapp M, Walker C, Warren AM, Brasel K, deRoon-Cassini TA. Utility of the injured trauma survivor screen to predict PTSD and depression during hospital admission. J Trauma Acute Care Surg. 2017;82(1). https://journals.lww.com/jtrauma/Fulltext/2017/01000/Utility_of_the_injured_trauma_survivor_screen_to.12.aspx. [DOI] [PubMed] [Google Scholar]
- 33.Stein MB, Walker J, Hazen AL, Forde D. Full and Partial Posttraumatic Stress Disorder: Findings from a Community Survey. Vol 154; 1997. doi: 10.1176/ajp.154.8.1114 [DOI] [PubMed] [Google Scholar]
- 34.Zlotnick C, Franklin CL, Zimmerman M. Does “subthreshold” posttraumatic stress disorder have any clinical relevance? Compr Psychiatry. 2002;43(6):413–419. doi: 10.1053/comp.2002.35900 [DOI] [PubMed] [Google Scholar]
- 35.Kenardy J, Edmed SL, Shourie S, et al. Changing patterns in the prevalence of posttraumatic stress disorder, major depressive episode and generalized anxiety disorder over 24 months following a road traffic crash: Results from the UQ SuPPORT study. J Affect Disord. 2018;236:172–179. doi: 10.1016/j.jad.2018.04.090 [DOI] [PubMed] [Google Scholar]
- 36.Bryant RA, McFarlane AC, Silove D, O’Donnell ML, Forbes D, Creamer M. The Lingering Impact of Resolved PTSD on Subsequent Functioning. Clin Psychol Sci. 2015;4(3):493–498. doi: 10.1177/2167702615598756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Donnell ML, Holmes AC, Creamer MC, et al. The role of post-traumatic stress disorder and depression in predicting disability after injury. Med J Aust. 2009;190(7 Suppl):S71–4. [DOI] [PubMed] [Google Scholar]
- 38.Archer KR, Heins SE, Abraham CM, Obremskey WT, Wegener ST, Castillo RC. Clinical Significance of Pain at Hospital Discharge Following Traumatic Orthopedic Injury: General Health, Depression, and PTSD Outcomes at 1 Year. Clin J Pain. 2016;32(3):196–202. doi: 10.1097/AJP.0000000000000246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason S, Farrow TFD, Fawbert D, et al. The development of a clinically useful tool for predicting the development of psychological disorder following injury. Br J Clin Psychol. 2009;48(1):31–45. doi: 10.1348/014466508X344799 [DOI] [PubMed] [Google Scholar]
- 40.Walters J, Bisson J, Shepherd J. Predicting Post-Traumatic Stress Disorder: Validation of the Trauma Screening Questionnaire in Victims of Assault. Vol 37; 2007. doi: 10.1017/S0033291706008658 [DOI] [PubMed] [Google Scholar]
- 41.Frank CA, Schroeter K, Shaw C. Addressing Traumatic Stress in the Acute Traumatically Injured Patient. J Trauma Nurs. 2017;24(2). https://journals.lww.com/journaloftraumanursing/Fulltext/2017/03000/Addressing_Traumatic_Stress_in_the_Acute.5.aspx. [DOI] [PubMed] [Google Scholar]
- 42.Hanley J, deRoon-Cassini T, Brasel K. Efficiency of a Four-Item Posttraumatic Stress Disorder Screen in Trauma Patients. Vol 75; 2013. doi: 10.1097/TA.0b013e3182a53a5f [DOI] [PubMed] [Google Scholar]
- 43.Boals A, Trost Z, Rainey E, Foreman ML, Warren AM. Severity of traumatic injuries predicting psychological outcomes: A surprising lack of empirical evidence. J Anxiety Disord. 2017;50:1–6. doi: 10.1016/j.janxdis.2017.04.004 [DOI] [PubMed] [Google Scholar]
- 44.Love J, Zatzick D. Screening and Intervention for Comorbid Substance Disorders, PTSD, Depression, and Suicide: A Trauma Center Survey. Vol 65; 2014. doi: 10.1176/appi.ps.201300399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. Gen Hosp Psychiatry. 2013;35(5):485–491. doi: 10.1016/j.genhosppsych.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haarbauer-Krupa JA Taylor C, Yue J, et al. Screening for Post-Traumatic Stress Disorder in a Civilian Emergency Department Population with Traumatic Brain Injury. J Neurotrauma. 2016;34. doi: 10.1089/neu.2015.4158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. [DOI] [PubMed] [Google Scholar]
- 48.Iverson GL, Gardner AJ, Terry DP, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941 LP–948. doi: 10.1136/bjsports-2017-097729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heron-Delaney M, Kenardy J, Charlton E, Matsuoka Y. A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury. 2013;44(11):1413–1422. doi: 10.1016/j.injury.2013.07.011 [DOI] [PubMed] [Google Scholar]
- 50.Price M, Kearns M, Houry D, Rothbaum BO. Emergency department predictors of posttraumatic stress reduction for trauma-exposed individuals with and without an early intervention. J Consult Clin Psychol. 2014;82(2):336–341. doi: 10.1037/a0035537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cofield SS, Conwit R, Barsan W, Quinn J. Recruitment and Retention of Patients into Emergency Medicine Clinical Trials. Acad Emerg Med. 2010;17(10):1104–1112. doi: 10.1111/j.1553-2712.2010.00866.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Platts-Mills TF, Hunold KM, Esserman DA, Sloane PD, McLean SA. Motor vehicle collision-related emergency department visits by older adults in the United States. Acad Emerg Med. 2012;19(7):821–827. doi: 10.1111/j.1553-2712.2012.01383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lewis GC, Platts-Mills TF, Liberzon I, et al. Incidence and predictors of acute psychological distress and dissociation after motor vehicle collision: a cross-sectional study. J Trauma Dissociation. 2014;15(5):527–547. doi: 10.1080/15299732.2014.908805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Albert M, McCaig LF. Emergency department visits for motor vehicle traffic injuries: United States, 2010–2011. NCHS Data Brief. 2015;(185):1–8. [PubMed] [Google Scholar]
- 55.Bisson JI, Shepherd JP, Joy D, Probert R, Newcombe RG. Early cognitive-behavioural therapy for post-traumatic stress symptoms after physical injury: Randomised controlled trial. Br J Psychiatry. 2004;184(JAN.):63–69. doi: 10.1192/bjp.184.1.63 [DOI] [PubMed] [Google Scholar]
- 56.Bryant RA. Early intervention for post-traumatic stress disorder. Early Interv Psychiatry. 2007;1(1):19–26. doi: 10.1111/j.1751-7893.2007.00006.x [DOI] [PubMed] [Google Scholar]
- 57.Guest R, Tran Y, Gopinath B, Cameron ID, Craig A. Psychological distress following a motor vehicle crash: A systematic review of preventative interventions. Injury. 2016;47(11):2415–2423. doi: 10.1016/j.injury.2016.09.006 [DOI] [PubMed] [Google Scholar]
- 58.Rothbaum BO, Kearns MC, Price M, et al. Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biol Psychiatry. 2012;72(11):957–963. doi: 10.1016/j.biopsych.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freedman SA, Dayan E, Kimelman YB, Weissman H, Eitan R. Early intervention for preventing posttraumatic stress disorder: an Internet-based virtual reality treatment. Eur J Psychotraumatol. 2015;6(1):25608. doi: 10.3402/ejpt.v6.25608 [DOI] [PMC free article] [PubMed] [Google Scholar]


