Abstract
Objective:
To compare the efficacy of Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST) with geriatric case management (CM) in a sample of older adults meeting DSM-5 diagnostic criteria for hoarding disorder (HD).
Methods:
Fifty-eight older adults with HD were enrolled in a randomized controlled trial between December 2011 and March 2014. Thirty-one participants received CREST, and 27 participants received CM. Both interventions consisted of 26 individual sessions over a period of 6 months and included several home visits by the study therapists (CREST) or nurses (CM).The Saving Inventory-Revised (SI-R) and the UCLA Hoarding Severity Scale (UHSS) were the main outcome measures.
Results:
Participants in the CREST condition had significantly greater improvement on the SI-R than participants in the CM group (group × time interaction: β = 3.95, SE = 1.81, P = .029), with participants who completed the CREST condition averaging a 38% decrease in symptoms and participants who completed the CM condition averaging a 25% decrease in symptoms. In contrast, there was not a significant group × time interaction effect on the UHSS (β = 1.23, SE = 0.84, P = .144), although participants did report greater improvement in symptoms in the CREST condition (35%) than in the CM condition (24%). Treatment gains were maintained at 6-month follow-up.
Conclusions:
CREST appears to be an efficacious treatment compared to CM for older adults, but CM also showed meaningful benefits.
Trial Registration:
ClinicalTrials.gov identifier: NCT01227057
Hoarding disorder (HD) is a chronic and progressive1,2 psychiatric condition that leads to far-reaching community consequences, particularly in later life.3,4 Hoarding is common among older adults. Community epidemiologic reports estimate the prevalence of clinically significant hoarding symptoms from 2%5 to 6%6 in the general population, and the prevalence of HD in older adults may be up to 3 times higher.7
Accumulation of clutter can put older individuals at risk due to fire danger, fall hazards, infestations, food contamination, medication mismanagement, social isolation, and nutritional deprivation.1,3,4,8 Medical problems, functional impairment, and decreased quality of life are commonly and directly associated with hoarding severity in geriatric HD patients. 3,9–12 For example, 64% of older adults with HD have difficulty with self-care and 81% have direct physical health risks due to fires, falls, and sanitation problems 4
Executive functioning problems (eg, difficulty with planning, cognitive flexibility, and problem-solving) are evident in older HD patients.13–16 Geriatric HD patients often have deficits in planning, problem-solving, cognitive flexibility, and prospective memory,14,16 which may negatively affect response to standard cognitive-behavioral therapy (CBT).14,17 Geriatric HD patients had limited treatment response in a pilot study (N = 12) of CBT for hoarding,18 and participants reported that behavioral exposure was the most helpful aspect of CBT.17 Neurocognitive impairment is associated with poorer response to CBT in other geriatric psychiatric populations,19 which may explain the poor outcomes seen with CBT for geriatric hoarding. Adding cognitive rehabilitation interventions to CBT for HD in older adults may enhance treatment response.
Taking advantage of emerging data regarding the importance of exposure therapy for hoarding, as well as executive dysfunction as a rate-limiting factor in treatment response in older adults, we developed Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST),20 which pairs compensatory cognitive training (CCT) to improve executive functioning with behavioral exposure to the distress of discarding/not acquiring. This novel treatment addresses neurocognitive weaknesses that may contribute to HD while targeting the core symptoms of urges to save and avoidance of discarding that lead to the accumulation of clutter. An open trial of CREST in older adults with HD20 showed significant improvement in hoarding severity from baseline to posttreatment, with large effect sizes (d = 1.02–1.51) on the primary outcome measures.20
The present study is the first randomized clinical trial of a treatment for geriatric HD. We compared 2 active treatments: CREST and case management (CM). Case management was chosen as this is the most widely available and utilized intervention for HD. We hypothesized that, compared to older adults with HD receiving CM, those treated with CREST would show (1) clinically significant and greater decreases in acquisition, difficulty discarding, and excessive clutter; (2) greater decreases in anxiety and depression; and (3) greater decreases in disability and functional impairment. We hypothesized that there would be more treatment responders with CREST than with CM and that these gains would be maintained over a 6-month follow-up period.
METHODS
The study was approved by the local ethics committee, written informed consent was obtained, and the study was registered at ClinicalTrials.gov (identifier: NCT01227057). Details of the recruitment methods and a discussion of the factors related to participant retention have been published elsewhere.21
Participants
Participants were recruited via posted flyers and electronic advertisements from December 2011 to March 2014 from the San Diego community. Participants were included if they were 60 years of age or older, could speak and read English, were able to participate in face-to-face individual psychotherapy, met the DSM-5 criteria for a primary diagnosis of HD as determined by clinical interview, and scored ≥20 on the UCLA Hoarding Severity Scale (UHSS)22 and ≥40 on the Saving Inventory-Revised (SI-R).23 Final HD diagnosis was determined by a consensus conference including at least 2 therapists with expertise in hoarding, supervised by a licensed clinical psychologist (C.R.A.).
Participants were excluded if they were enrolled in psychotherapy in the past 3 months; had psychotropic medication changes in the past 3 months; met diagnostic criteria for current substance abuse, history of mania or psychosis, and active suicidal ideation as determined by the Mini-International Neuropsychiatric Interview (MINI)24; and screened for dementia by scoring less than 21 on the Montreal Cognitive Assessment (MoCA)25 and if their hoarding symptoms were due to a secondary condition (eg, obsessive-compulsive disorder [OCD], traumatic brain injury), as per DSM-5 criteria.
Assessments
The assessment battery was administered in person at baseline and 6 months (posttreatment) and over the phone at 3 months (mid-treatment), 9 months, and 12 months. The primary outcome measures were the SI-R and the UHSS. The SI-R is a 23-item self report scale that measures excessive acquisition, difficulty discarding, and clutter. The UHSS is a 10-item clinician-administered assessment and includes items related to clutter, impairment caused by hoarding, and procrastination. Secondary outcome measures included the Clutter Image Rating (CIR),26,27 the Hospital Anxiety and Depression Scale (HADS),28 the Activities of Daily Living–Hoarding scale (ADL-H),29 and the Clinical Global Impressions (CGI)30 Severity and Improvement scales. The CGI Severity scale was included as a continuous measure of global improvement and rated on a scale of 1 (“normal”) to 7 (“extremely ill”). The CIR, HADS, and CGI were administered at baseline and posttreatment (6-month) assessments only.
Baseline and posttreatment assessments were conducted by master’s level clinical psychology graduate students who received 15 hours of training. All study assessments were videotaped for review by a licensed clinical psychologist (C.R.A.). Assessments conducted over the phone (at 3, 9, and 12 months) were conducted by graduate or undergraduate research assistants with at least 20 hours of assessment training.
Interventions
CREST included 26 weekly 60-minute individual sessions over 6 months. The manual was developed by the principal investigator and the coinvestigators of the study (E.W.T., S.S., and J.L.W.) based in part on the compensatory cognitive training31 and CogSMART interventions32,33 and did not include traditional cognitive therapy elements, such as cognitive restructuring. An overview of the treatment is provided in Table 1. The first 6 sessions of CREST involved teaching skills that target prospective memory, planning, cognitive flexibility, and problem solving. Sessions 7–9 prepared the participant for exposure therapy, and sessions 10–24 involved exposure sessions initially taking place in the clinic and, later, more advanced exposures in the participants’ homes. Sessions 25–26 involved relapse prevention and maintenance. Daily homework was emphasized and reviewed at the beginning of each session.
Table 1.
CREST Modules, Target Domains, and Manual Content
| Module | Session/Homework Content |
|---|---|
| CCT (target domain) | |
| Session 1. Introduction to CCT and psychoeducation about the link between brain functioning and HD | Discussion of patient’s experienced consequences of HD, barriers to treatment adherence and possible solutions, and treatment goals and expectations |
| Session 2. Calendar use (prospective memory) | Discussion of current/past calendar system; goal setting of where to keep calendar and when to use it; practicing use of calendar with “real-world” type scenario; using linking tasks and automatic places to help with daily activities |
| Session 3. Linking tasks, using a “to-do” list (prospective memory) | Review of calendar use and linking tasks; using “to-do” lists along with calendar; determination of to do categories and frequencies; short-term prospective memory strategies (eg, “can’t miss reminders”) |
| Sessions 4–5. Problem solving | Brainstorming practice exercises (therapist- and patient-provided examples); 6-step problem solving method; practice evaluating solutions for feasibility |
| Session 6. Thinking flexibly and planning (cognitive flexibility) | Self-talk and self-monitoring; brainstorming steps to meet a goal; practicing setting time lines for long-term goals. |
| Session 7. Home visit and organizational preparation (cognitive flexibility) | Creating a plan for organizing home (ie, where types of items should be stored); brainstorm “to-do” list for organization; rules of organizing; home maintenance system (current and proposed rules) |
| ET | |
| Session 8. Exposure preparation | Discussion of expectations, decision making, habituation, and avoidance; rules of discarding; motivational interviewing about willingness to change; acquisition hierarchy; fear of discarding hierarchy |
| Session 9. Introduction to exposure therapy | Review of organizational plan, rules of organizing, maintenance system, and rules of discarding; introduction to Subjective Units of Distress (SUDS) Ratings; discarding exposure |
| Sessions 10–22. Exposure to discarding and acquiring | Evaluation of progress; discarding exposure; discussion of reasons for saving and strategies for making discarding choices; introduction to advanced exposure (eg, discussion of rules, preparing for sorting for a longer time, and use of outside help); review of treatment goals |
| Sessions 23–24. Advanced exposure | Longer exposure time (2–4 hours) with outside help; evaluation of progress; discussion of reasons for saving and strategies for making discarding choices; review of treatment goals |
| Sessions 25–26. Relapse prevention and maintenance | Review of progress in therapy; discussion of everyday uses for cognitive strategies (eg, calendar use, “to do” lists, problem solving); exposure review; planning for the future |
Abbreviations: CCT = compensatory cognitive training, ET = exposure therapy, HD = hoarding disorder.
Case management involved 26 weekly 45- to 60-minute sessions over 6 months. Case management was conducted by registered nurses with specialization in geriatric populations, as this would be standard care in the community. They performed an initial assessment to evaluate participants’ home, health, safety, and welfare and provided case management for identified needs. For example, if a participant was not receiving medical care, the case manager would facilitate linkages with appropriate medical treatment. Case managers provided support and advocacy as well as appropriate resources for social services. Case managers did not assist with decluttering. If a participant’s items posed a safety problem (eg, papers on stove top), they would relocate the items but not assist with removal of the items. They were instructed not to provide cognitive-behavioral therapy, cognitive rehabilitation, or exposure therapy for hoarding.
Supervision and Fidelity Monitoring
CREST was administered by 2 doctoral-level therapists and 1 master’s level therapist with at least 3 years of experience with psychotherapy for anxiety and obsessive-compulsive spectrum disorders. Therapist training involved multiple in-person training sessions and completion of cases from the pilot trial. Therapists were supervised by a licensed clinical psychologist (C.R. A.) who reviewed tapes for clinical supervision. All treatment sessions were videotaped, and 20% of sessions were reviewed for competency and adherence. Therapist adherence was calculated as the degree to which the therapist implemented all required elements of each session. Therapist competency was judged on a scale from 1 (“low competency”) to 3 (“high competency”) for each session section, and then ratings were converted to an overall percentage for the session. Adequate fidelity scores were defined a priori as 80% adherence and competency. Fidelity ratings across all sessions suggested low adherence (78% [SD = 25.51%]; range, 24.24%–100%) but high competence (94.12% [SD = 10.39%]; range, 66.67%–100%). The low adherence ratings were due in part to therapist efforts to enhance motivation and insight.
Case management was provided by 2 nurses with experience in general geriatric care management. Case manager training involved a review of best practices of geriatric case management, trainings on HD and individual supervision with audio tape review to ensure that there was no exposure or other forms of psychotherapy being delivered. The case managers were not trained in CREST.
Randomization
Participants were randomized after inclusion status was confirmed based on baseline assessment. Condition assignment was determined using computer-generated randomization with a 1:1 ratio. Clinician assignment was based on therapist availability. Study assessors were blind to the randomization status of participants.
Data Analysis
All analyses were performed using Stata version 13.0.34 Baseline clinical characteristics and demographic data were compared between CREST and CM groups using χ2 analyses and t tests (see Table 1). Linear mixed models with random intercepts were used to evaluate the change in outcome variables over time, the effect of group, the effect of treatment, and the group × time interaction, both for the treatment phase (0–6 months) and follow-up phase (6–12 months). Baseline characteristics that differed between groups were included as covariates for all analyses.
All analyses (0–6 months) were conducted on an intent-to-treat (ITT) basis and then among completers only. The ITT analyses were conducted using the data from all randomized participants. The proportions of participants from each group classified as treatment responders were compared using χ2 analyses in the completer sample. Treatment response was defined as achieving subclinical levels of hoarding severity (<41 on the SI-R or <4 on the CIR) or a score of 2 (much improved) or 1 (very much improved) on the CGI Improvement scale. Participants without information at posttreatment were categorized as nonresponders. Between-group effect size was calculated as Cohen d using the mean difference in baseline and posttreatment scores for the completer sample for all outcome measures. Within-group effect size was calculated as Cohen d using the mean difference in baseline and posttreatment scores for the completer sample for the SI-R Total only.
Power Analysis
Power calculations were based on the SI-R using effect size estimates from a previous trial comparing individual CBT with a wait-list control.35 In this study, the effect size of CBT relative to wait list was d = 2.21 on the SI-R. Accounting for a smaller effect size due to having an active control condition, we expected to have 80% power to detect a large (d = 0.80) effect size with a completer sample size of N = 56. The number of participants enrolled (n = 58) exceeded this target, and the completer sample (n = 44) was 79% of the target N.
RESULTS
Baseline participant characteristics (N = 58) are presented in Table 2. The majority of participants were female (71%), white (84%), and retired (60%). The average participant was 67 years old and had 16 years of education. Participants randomized to the CREST condition were significantly older (69 vs 64 years, t56 = −3.28, P = .0009) and reported having significantly more years of education (16.55 vs 15.33, t54 = −2.20, P = .016). Groups did not differ on other demographic variables (see Table 2).
Table 2.
Baseline Participant Characteristicsa
| Characteristic | Overall (N = 58) | CREST (n = 31) | CM (n = 27) | P Valueb |
|---|---|---|---|---|
| Age, mean (SD), y | 66.95 (6.48) | 69.35 (6.49) | 64.19(5.35) | .0009 |
| Education, mean (SD), y | 15.96 (2.14) | 16.55 (2.10) | 15.33 (2.04) | .016 |
| Women | 41 (70.69) | 24 (77.42) | 17 (62.96) | .228 |
| Race | .225 | |||
| White | 49 (84.48) | 26 (83.87) | 23 (85.19) | |
| Black | 1 (1.72) | 1 (3.23) | 0 | |
| Asian | 2 (3.45) | 2 (6.45) | 0 | |
| Hispanic | 2 (3.45) | 1 (3.23) | 1 (3.70) | |
| Biracial | 3 (5.17) | 0 | 3 (11.11) | |
| Other | 1 (1.72) | 1 (3.23) | 0 | |
| Marital status | .179 | |||
| Never married | 16 (27.59) | 6 (19.35) | 10 (37.04) | |
| Married or living with someone | 16 (27.59) | 9 (29.03) | 7 (25.93) | |
| Separated/divorced | 22 (37.93) | 15 (48.39) | 7 (25.93) | |
| Widowed | 4 (6.90) | 1 (3.23) | 3 (11.11) | |
| Employment status | .052 | |||
| Retired | 35 (60.34) | 23 (74.19) | 12 (44.44) | |
| Employed full- or part-time | 18 (31.03) | 7 (22.58) | 11 (40.74) | |
| Unemployed | 5 (8.62) | 1 (3.23) | 4 (14.81) | |
| Assessment scores, mean (SD) | ||||
| SI-R | 58.34 (12.08) | 57.35 (10.23) | 59.48 (14.01) | .254 |
| CIR | 4.24 (1.89) | 4.15 (1.71) | 4.33 (2.11) | .358 |
| UHSS | 27.52 (5.65) | 26.35 (5.31) | 28.85 (5.82) | .047 |
| ADL-H | 31.31 (11.23) | 30.85 (9.30) | 31.90 (13.53) | .376 |
| HADS Anxiety | 9.56 (3.98) | 9.06 (4.39) | 10.15 (3.41) | .154 |
| HADS Depression | 7.79 (4.16) | 7.13 (3.23) | 8.56 (4.97) | .098 |
| CGI Severity | 3.81 (1.06) | 3.67 (.92) | 3.96 (1.19) | .148 |
| Presence of comorbid diagnosis | ||||
| OCD | 15 (26.32) | 4 (13.33) | 11 (40.74) | .019 |
| Any anxiety disorder (non-OCD) | 16 (28.07) | 6 (20.00) | 10 (37.04) | .153 |
| Any mood disorder | 22 (38.60) | 12 (40.00) | 10 (37.04) | .819 |
| Taking psychotropic medications | 23 (39.66) | 10 (32.26) | 13 (48.15) | .217 |
| No. of medical conditions, mean (SD) | 3.13 (2.28) | 3.52 (2.47) | 2.68 (1.99) | .091 |
Values are expressed as n (%) unless otherwise indicated.
For comparison of CREST and CM, using t tests or χ2 tests and a critical P value of ɑ = .05. Boldface indicates statistical significance.
Abbreviations: ADL-H = Activities of Daily Living–Hoarding scale, CGI = Clinical Global Impressions scale, CIR = Clutter Image Rating, CM = case management, CREST = Cognitive Rehabilitation and Exposure/Sorting Therapy, HADS = Hospital Anxiety and Depression Scale, OCD = obsessive-compulsive disorder, SI-R = Saving Inventory-Revised, UHSS = UCLA Hoarding Severity Scale.
Twenty-eight percent of all participants met DSM-IV-TR criteria for an anxiety disorder (excluding OCD), and 39% of all participants met DSM-IV-TR criteria for a mood disorder (see Table 2). Twenty-six percent of all participants met DSM-IV-TR criteria for OCD; a significantly higher percentage of CM participants (41%) than CREST participants (13%) met OCD criteria (χ21 = 5.50, P = .019). Participants randomized to the CM condition were rated to have significantly more severe HD symptoms on the UHSS (t56 = −1.71, P = .047), although there were no differences in baseline symptom severity on self-reported hoarding severity (SI-R, CIR, or CGI) or on functional (ADL-H) or psychiatric (HADS) symptom severity (all P values > .05). On the basis of the significant group differences found at baseline, age, years of education, and presence of comorbid OCD were used as covariates in the models described below.
Attrition
Study patient flow is depicted in Figure 1. A total of 67 (54%) of 125 individuals who called to express interest provided consent and were assessed for eligibility, of whom 58 (87%) were randomized. Over 80% of CREST participants and 70% of CM participants completed posttreatment assessment at 6 months. There was not a significant group difference in dropout rate at posttreatment (χ21 = 0.832, P = .362). More than 65% of all randomized patients were retained through the 12-month follow-up assessment.
Figure 1.
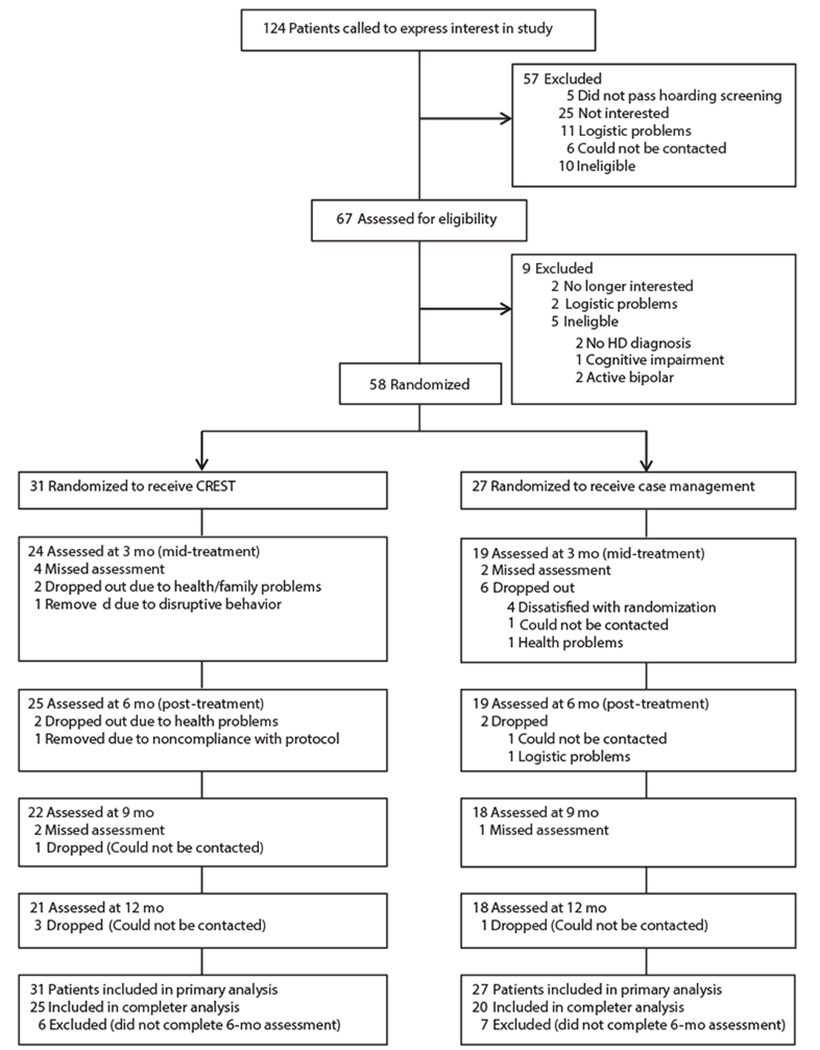
Flow of Participants Through Each Phase of the Study
Abbreviations: CREST = Cognitive Rehabilitation and Exposure/Sorting Therapy, HD=hoarding disorder.
Pretreatment to Posttreatment Outcomes (0–6 Months)
Mean observed scores at baseline, mid-treatment (3 months), and posttreatment (6 months) are presented in Table 3.The ITT sample did not differ statistically from observed values. Overall, participants reported significant decreases in symptom severity from baseline to posttreatment on all primary and secondary outcome measures (time effect; Table 3) using mixed-effects linear regression models with the ITT sample and controlling for baseline age, years of education, and OCD diagnosis. The change in observed symptom severity for each treatment group at each time point is presented in Table 3.
Table 3.
Observed Mean (SD) Scores on Outcomes Measures Across Time for 58 Older Adults Receiving Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST) or Geriatric Case Management (CM) for Hoarding Disorder
| Assessment Group | Active Treatment (0–6 mo) |
Follow-Up (6–12 mo) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Pointa |
Mean % Changeb | d (95% CI) | Time Effectc |
Group × Time Interaction |
Time Pointa |
Time Effect |
Group × Time Interaction |
||||||||
| Baseline (n = 58) | 3 mo (n = 43) | 6 mo (n = 44) | 9 mo (n = 40) | 12 mo (n = 38) | |||||||||||
| β (SE) | P | β (SE) | P | β (SE) | P | β (SE) | P | ||||||||
| SI-R | |||||||||||||||
| CREST | 57.35 (10.23) | 45.96 (15.38) | 35.44 (15.48) | 38.20% | 0.63 (0.02–1.24) | −10.82 (1.21) | <.001 | 3.95 (1.81) | .03 | 36.5 (13.76) | 41.29 (13.83) | 2.07 (1.11) | .06 | −1.86 (1.65) | .26 |
| CM | 59.48 (14.01) | 51.89 (14.15) | 44.68 (13.29) | 24.88% | 46.44 (17.12) | 45.17 (18.34) | |||||||||
| UHSS | |||||||||||||||
| CREST | 26.35 (5.31) | 21.96 (7.63) | 17.20 (6.50) | 34.72% | 0.50 (0.11–1.10) | −4.41 (0.57) | <.001 | 1.23 (0.84) | .14 | 17.14 (5.99) | 18.00 (5.96) | 0.005 (0.53) | .99 | −0.25 (0.79) | .75 |
| CM | 28.85 (5.82) | 23.95 (7.56) | 21.84 (7.82) | 24.30% | 20.78 (8.64) | 21.39 (8.59) | |||||||||
| CIR | |||||||||||||||
| CREST | 4.15 (1.71) | … | 2.47 (1.05) | 40.48% | 0.55 (0.07–1.16) | −0.67 (0.14) | <.001 | 0.38 (0.21) | .07 | … | |||||
| CM | 4.33 (2.11) | … | 3.65 (2.17) | 15.70% | |||||||||||
| ADL-H | |||||||||||||||
| CREST | 30.85 (9.30) | 24.20 (10.86) | 21.09 (6.67) | 31.64% | 0.67 (0.04–1.38) | −3.93 (0.73) | <.001 | 2.31 (1.09) | .04 | 21.63 (5.89) | 20.56 (4.50) | 0.04 (0.54) | .94 | −0.44 (0.79) | .57 |
| CM | 31.90 (13.53) | 25.35 (11.07) | 27.81 (14.29) | 12.82% | 23.71 (10.25) | 21.33 (5.26) | |||||||||
| HADS Anxiety | |||||||||||||||
| CREST | 9.06 (4.39) | … | 5.63 (4.05) | 37.86% | 0.60 (0.02–1.21) | −1.59 (0.37) | <.001 | 1.11 (0.54) | .04 | … | |||||
| CM | 10.15 (3.41) | … | 8.68 (4.51) | 14.48% | |||||||||||
| HADS Depression | |||||||||||||||
| CREST | 7.13 (3.23) | … | 4.33 (2.20) | 39.27% | 0.55 (0.07–1.16) | −1.41 (0.33) | <.001 | 0.79 (0.49) | .11 | … | |||||
| CM | 8.56 (4.97) | … | 6.84 (4.39) | 20.09% | |||||||||||
| CGI Severity | |||||||||||||||
| CREST | 3.67 (0.17) | … | 2.67 (1.01) | 27.25% | 0.65 (0.01–1.28) | −0.51 (0.09) | <.001 | 0.29 (0.14) | .04 | … | |||||
| CM | 3.96 (0.23) | … | 3.50 (1.54) | 11.62% | |||||||||||
Sample sizes by time point: baseline: CREST: n = 31, CM: n = 27;3 mo: CREST: n = 24, CM: n = 19; posttreatment (6 mo): CREST: n = 25, CM: n = 19; 9 mo: CREST: n = 22, CM: n = 18; 12 mo: CREST: n = 21, CM: n = 18.
Calculated using completer sample (n = 44) only.
Analyses were mixed-effects linear regression models using the intent-to-treat sample and controlling for baseline age, years of education, and OCD diagnosis.
Abbreviations: ADL-H = Activities of Daily Living–Hoarding scale, CGI = Clinical Global Impressions scale, CIR = Clutter Image Rating, HADS = Hospital Anxiety and Depression Scale, HD = hoarding disorder, OCD = obsessive-compulsive disorder, SI-R = Saving Inventory-Revised, UHSS = UCLA Hoarding Severity Scale. Symbol: … = not applicable.
Primary outcomes.
ITT analyses indicated that participants in the CREST condition had significantly greater improvement on the SI-R total than participants in the CM group (group × time interaction β = 3.95, SE = 1.81, P = .029), with participants who completed the CREST condition averaging a 38% decrease in symptoms and participants who completed the CM condition averaging a 25% decrease in symptoms (Table 3). Completer analyses resulted in a similar pattern of statistical findings. ITT analyses of the SI-R subscales indicated a significant group by time interaction for the SI-R clutter subscale only (clutter: β = 2.02, SE = 0.88, P = .022; difficulty discarding: β = 0.90, SE = 0.67, P = .18; acquisition: β = 1.12, SE = 0.60, P = .059). Paired t tests using the observed data indicated that participants had significant decreases on the SI-R total in both the CREST (t24 = 6.81, P < .0001) and the CM (t18 = 6.11, P < .0001) conditions from baseline to posttreatment. There was a medium to large between-group effect size for the nonadjusted completer sample change score between baseline and posttreatment assessment on the SI-R total (d = 0.63; 95% confidence interval [CI], 0.02–1.24). There was a large within-group effect size for the nonadjusted completer sample change score between baseline and posttreatment assessment on the SI-R total for both CREST (d = 1.71; 95% CI, 1.08–2.32) and CM (d = 1.08; 95% CI, 0.44–1.70).
In contrast, there was not a significant group × time interaction effect on the UHSS (β = 1.23, SE = 0.84, P = .144), although participants did report greater improvement in symptoms in the CREST condition (35%) than in the CM condition (24%). Completer analyses resulted in a similar pattern of statistical findings. Paired t tests using the observed data indicated that participants had significant decreases on the UHSS in both the CREST (t24 = 7.22, P < .0001) and the CM (t18 = 4.46, P < .001) conditions from baseline to posttreatment. There was a medium effect size for the nonadjusted completer sample change score between baseline and posttreatment assessment on the UHSS (d = 0.50; 95% CI, 0.11–1.10).
Secondary outcomes.
ITT analyses indicated that participants in the CREST condition had significantly greater improvement on the ADL-H relative to participants in the CM group (β = 2.31, SE = 1.09, P = .035), with participants who completed the CREST condition averaging a 32% improvement and participants who completed the CM condition averaging a 13% improvement (Table 3). Participants in the CREST condition had significantly greater improvement relative to participants in the CM group on the HADS Anxiety subscale (38% vs 14%; β = 1.11, SE = 0.54, P = .04) and on the CGI Severity scale (27% vs 12%; β = 0.29, SE = 0.14, P = .04). The difference in symptom improvement between the CREST and CM treatment conditions was not significant for the CIR (40% vs 16%; β = 0.38, SE = 0.21, P = .072) or for the HADS Depression subscale (39% vs 20%; β = 0.79, SE = 0.49, P = .107). Completer analyses resulted in a similar pattern of statistical findings. Between-group effect sizes for the nonadjusted completer sample change score between baseline and posttreatment assessment for all secondary measures are displayed in Table 3.
Long-Term Outcomes (6–12 Months)
Mean observed scores at 9 and 12 months are presented in Table 3.The long-term outcomes on the SI-R, UHSS, and ADL-H for both treatment groups are presented in Figure 2. Covariate-adjusted mixed-effects linear regression models with the ITT sample indicated no symptom change from posttreatment assessment through 12-month follow-up assessment on any of the primary or secondary outcome measures (time effect; Table 3), and this did not differ by group (group × time interaction; Table 3).
Figure 2.
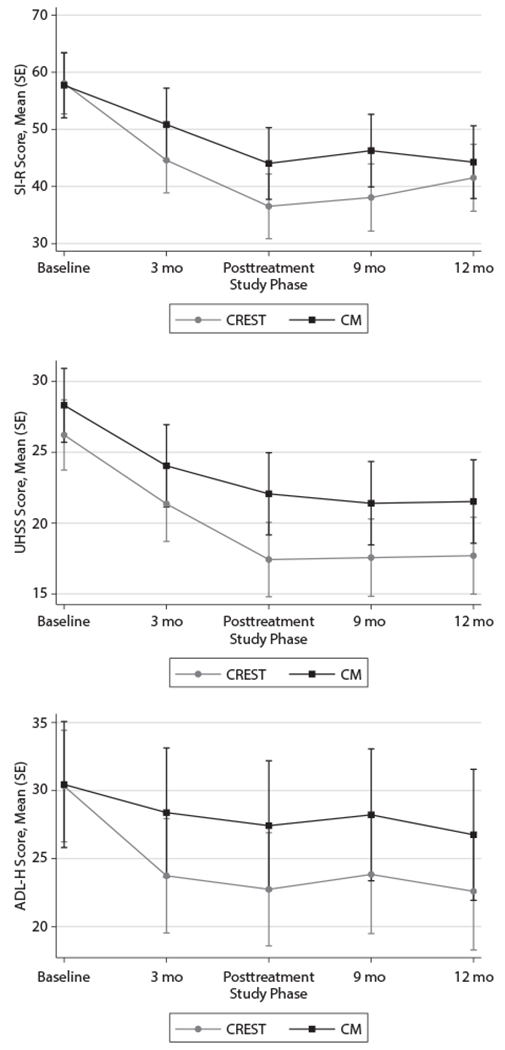
Hoarding Symptom Severity on Outcome Measures as a Function of Treatment Group for 58 Participants Receiving CREST or CM for Hoarding Disordera
aData are predicted values based on mixed models with standard error bars. Abbreviations: ADL-H = Activities of Daily Living–Hoarding scale, CM = case management, CREST=Cognitive Rehabilitation and Exposure/Sorting Therapy, SI-R = Saving Inventory-Revised, UHSS = UCLA Hoarding Severity Scale.
Treatment Response Rates
A significantly greater proportion of CREST participants were categorized as treatment responders when compared with CM participants on the CGI Improvement scale (78% vs 28%; χ21 = 10.45, P = .001, OR = 0.11). A significantly greater proportion of CREST participants were categorized as having subclinical posttreatment scores when compared with CM participants on the CIR (88% vs 50%; χ21 = 7.51, P = .006, OR = 7.33). Although more CREST participants were categorized as having subclinical posttreatment scores when compared with CM participants on the SI-R (64% vs 42%), this difference was not statistically significant (χ21 = 2.09, P = .149, OR = 2.44). The number needed to treat in order for 1 additional patient to achieve subclinical posttreatment scores was 2.6 on the CIR and 4.5 on the SI-R.
DISCUSSION
The primary goal of the present study was to test the efficacy of a novel treatment approach that combined CCT with behavioral exposure therapy in older adults with HD. Compared to participants randomized to CM, participants who received CREST had higher response rates to treatment and had greater improvement in hoarding severity, activities of daily living, and general anxiety from baseline to posttreatment. There was no reversal of treatment gains for either condition for the 6 months following posttreatment assessment. These results are consistent with our previous open trial of CREST in older adults.20 Contrary to our hypotheses, participants in the CREST condition did not demonstrate significantly greater decreases in depression or clutter volume when compared to participants in CM.
Despite the severe negative impact of HD on individuals and the community, available CBT treatments for hoarding do not consistently reduce hoarding symptoms to subclinical levels,36 especially for geriatric HD patients.18 Only 4 previous trials have utilized control groups,35,37–39 and none of those studied geriatric patients. Two of those trials utilized wait-list control groups,35,37 and the additional trials used unguided or guided bibliotherapy as the control group.38,39
The CM condition yielded results similar to that of CBT for geriatric hoarding (for CM: 25% change on the SI-R; d = 1.08). Ayers and colleagues18 observed a 20% reduction on the SI-R in older adults receiving individual CBT for hoarding, a change approximately half that observed in participants receiving CREST (38% change on the SI-R; d = 1.71). A second study of CBT for late life hoarding8 did not use the SI-R as an outcome measure but did report a 28% reduction in clutter level on the CIR. This change in clutter was larger than what the present study observed in the CM condition (16% reduction) but was 12 points lower than the change in clutter reported for the CREST participants (40%). The lack of significant group differences on the UHSS in the present study may indicate that the tested intervention does not affect the associated features of HD. In addition to core HD symptoms (clutter, excessive acquisition, and difficulty discarding), the UHSS includes items related to perfectionism, indecisiveness, and procrastination.22 These additional items may be less likely to change in response to exposure-based psychotherapy.
The superiority of CREST over CM on multiple outcome variables and percentage of treatment responders demonstrates the efficacy of CREST for older adults with HD. The superior efficacy of CREST may be due to inclusion of CCT and emphasis on exposure therapy (rather than cognitive therapy). The CCT modules may have assisted with ability to complete exposure therapy homework. While CM did not outperform CREST, it is believed that CM improved health, safety, and other areas of an individual’s life that may have enabled them to start addressing their hoarding problems. Thus, CM targeted many of the indirect consequences of hoarding. Given that CM is the most widely used intervention, these results are encouraging as CM has not been systematically tested. However, it should be noted that while CM was considered a treatment-as-usual condition, the frequency (weekly for 26 weeks) was much larger than typically seen in the community in order to control for face-to-face time.
The high retention rate of patients in both conditions throughout treatment and follow-up procedures demonstrates the motivation of HD patients in the community to engage in evidence-based treatment. The details of the techniques used to recruit and retain participants have been previously published21; in brief, study staff utilized motivational interviewing and problem solving when scheduling participants in order to minimize potential barriers to treatment engagement.
This study benefited from multiple strengths, including an active control condition, adherence to HD diagnostic criteria for enrollment, randomization, and strict supervision and fidelity to the manualized treatment protocol. With 58 enrolled participants, the current study represents the largest clinical trial to date of individual psychotherapy for HD.36 However, there are multiple factors that limit the generalizability of the findings. First, the outcome analyses were underpowered due to the unexpected strength of the CM treatment. Our sample size was selected based on a priori power calculations assuming a large (d = 0.80) effect size. Although the current study found consistent results in favor of CREST, none of the analyses had an associated effect size larger than 0.67. Furthermore, although the current study did not have assessor ratings of the participants’ clutter levels, previous studies conducted on this sample demonstrated that therapist ratings on the CIR were highly consistent with participants’ ratings.27 Additionally, although participants’ ages ranged from 60 to 85 years, the majority of participants were in their 60s (74% of our sample were aged 60–69 years). Participants were also mostly white, highly educated, and female. Finally, there was a significantly higher incidence of OCD in the CM group than in the CREST group. Although we controlled for OCD diagnosis in the outcome analyses, it is possible that this difference in psychiatric comorbidity could have biased the results.
Future studies of the efficacy of CREST in late-life hoarding may want to focus on recruiting participants in the old-old category (ie, aged 75 years or older) to establish CREST as a viable treatment option for this population. CREST should be examined in midlife HD populations given findings of neurocognitive deficits across multiple cognitive domains in midlife hoarding samples.40 The long-term outcomes of the current study are similar to those observed in research involving CBT for midlife hoarding at post-assessment.36 A head-to-head comparison of CBT and CREST, as well as studies looking at the mechanisms of each intervention, may help to determine which aspects of each treatment are most effective for maintaining reductions in hoarding symptoms.
Clinical points.
Traditional cognitive-behavioral therapy for hoarding disorder may not be as effective in older adults due to increased levels of neurocognitive impairment.
Individual psychotherapy combining compensatory cognitive training with exposure for sorting and discarding led to increased treatment gains in older adults with hoarding disorder when compared to geriatric case management.
Acknowledgments
Funding/support: This study was funded by a Career Development Award (CSRD-068-10S) from the Clinical Science Research and Development Program of the Veterans Health Administration awarded to Dr Ayers.
Role of the sponsor: The Veterans Health Administration had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Potential conflicts of interest: None.
Publisher's Disclaimer: Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs or the United States Government.
Previous presentation: Presented at the American Association for Geriatric Psychiatry Annual Conference, Washington, DC, March 18, 2016.
REFERENCES
- 1.Ayers CR, Saxena S, Golshan S, et al. Age at onset and clinical features of late life compulsive hoarding. Int J Geriatr Psychiatry. 2010;25(2):142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dozier ME, Porter B, Ayers CR. Age of onset and progression of hoarding symptoms in older adults with hoarding disorder. Aging Ment Health. 2016;20(7):736–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayers CR, Dozier ME. Predictors of hoarding severity in older adults with hoarding disorder. Int Psychogeriatr. 2015;27(7):1147–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HJ, Steketee G, Frost RO. Hoarding by elderly people. Health Soc Work 2001;26(3):176–184. [DOI] [PubMed] [Google Scholar]
- 5.Iervolino AC, Perroud N, Fullana MA, et al. Prevalence and heritability of compulsive hoarding: a twin study. Am J Psychiatry. 2009;166(10):1156–1161. [DOI] [PubMed] [Google Scholar]
- 6.Bulli F, Melli G, Carraresi C, et al. Hoarding behaviour in an Italian non-clinical sample. Behav Cogn Psychother. 2014;42(3):297–311. [DOI] [PubMed] [Google Scholar]
- 7.Samuels JF, Bienvenu OJ, Grados MA, et al. Prevalence and correlates of hoarding behavior in a community-based sample. Behav Res Ther. 2008;46(7):836–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turner K, Steketee G, Nauth L. Treating elders with compulsive hoarding: a pilot program. Cognit Behav Pract. 2010;17:449–457 [Google Scholar]
- 9.Ayers CR, Scheiuser D, Liu L, et al. Functional impairment in geriatric hoarding participants. J Obsessive Compuls Relat Disord. 2012;1:263–266. [Google Scholar]
- 10.Ayers CR, Iqbal Y, Strickland K. Medical conditions in geriatric hoarding disorder patients. Aging Ment Health. 2014;18(2):148–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diefenbach GJ, DiMauro J, Frost R, et al. Characteristics of hoarding in older adults. Am J Geriatr Psychiatry. 2013:21(10):1043–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steketee G, Schmalisch CS, Dierberger A, et al. Symptoms and history of hoarding in older adults. J Obsessive Compuls Relat Disord. 2012;1:1–7 [Google Scholar]
- 13.Ayers CR, Dozier ME, Wetherell JL, et al. Executive functioning in participants over age of 50 with hoarding disorder. Am J Geriatr Psychiatry. 2016;24(5):342–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayers CR, Wetherell JL, Schiehser D, et al. Executive functioning in older adults with hoarding disorder. Int J Geriatr Psychiatry. 2013;28(11):1175–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dozier ME, Wetherell JL, Twamley EW, et al. The relationship between age and neurocognitive and daily functioning in adults with hoarding disorder. Int J Geriatr Psychiatry. 2016;31 (12):1329–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackin RS, Areán PA, Delucchi KL, et al. Cognitive functioning in individuals with severe compulsive hoarding behaviors and late life depression. Int J Geriatr Psychiatry. 2011;26(3):314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayers CR, Bratiotis C, Saxena S, et al. Therapist and patient perspectives on cognitive-behavioral therapy for older adults with hoarding disorder: a collective case study. Aging Ment Health. 2012;16:915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayers CR, Wetherell JL, Golshan S, et al. Cognitive-behavioral therapy for geriatric compulsive hoarding. Behav Res Ther. 2011;49(10):689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohlman J, Gorman JM. The role of executive functioning in CBT: a pilot study with anxious older adults. Behav Res Ther. 2005;43(4):447–465. [DOI] [PubMed] [Google Scholar]
- 20.Ayers CR, Saxena S, Espejo E, et al. Novel treatment for geriatric hoarding disorder: an open trial of cognitive rehabilitation paired with behavior therapy. Am J Geriatr Psychiatry. 2014;22(3):248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayers CR, Dozier ME, Espejo E, et al. Treatment recruitment and retention of geriatric patients 2015;38:235–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saxena S, Ayers CR, Dozier ME, et al. The UCLA Hoarding Severity Scale: development and validation. J Affect Disord. 2015;175:488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frost RO, Steketee G, Grisham J. Measurement of compulsive hoarding: Saving Inventory-Revised. Behav Res Ther. 2004;42(10):1163–1182. [DOI] [PubMed] [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33, quiz 34–57. [PubMed] [Google Scholar]
- 25.Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. [DOI] [PubMed] [Google Scholar]
- 26.Frost RO, Steketee G, Tolin DF, et al. Development and validation of the Clutter Image Rating. J Psychopathol Behav Assess. 2008;30:193–203. [Google Scholar]
- 27.Dozier ME, Ayers CR. Validation of the Clutter Image Rating in older adults with hoarding disorder. Int Psychogeriatr. 2015;27(5):769–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 29.Frost RO, Hristova V, Steketee G, et al. Activities of daily living scale in hoarding disorder. J Obsessive Compuls Relat Disord. 2013;2(2):85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guy W ECDEU Assessment Manual for Psychopharmacology. Revised Edition Washington, DC: US Department of Health, Education, and Welfare; 1976. [Google Scholar]
- 31.Twamley EW, Vella L, Burton CZ, et al. Compesatory cognitive training for psychosis: effects in a randomized controlled trial. J Clin Psychiatry. 2012;73(9):1212–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Twamley EW, Jak AJ, Delis DC, et al. Cognitive Symptom Management and Rehabilitation Therapy (CogSMART) for veterans with traumatic brain injury: pilot randomized controlled trial. J Rehabil Res Dev. 2014;51 (1):59–70. [DOI] [PubMed] [Google Scholar]
- 33.Twamley EW, Thomas KR, Gregory AM, et al. CogSMART compensatory cognitive training for traumatic brain injury: effects over 1 year. J Head Trauma Rehabil. 2015;30(6):391–401. [DOI] [PubMed] [Google Scholar]
- 34.Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 35.Steketee G, Frost RO, Tolin DF, et al. Waitlist-controlled trial of cognitive behavior therapy for hoarding disorder. Depress Anxiety. 2010;27(5):476–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tolin DF, Frost RO, Steketee G, et al. Cognitive behavioral therapy for hoarding disorder: a meta-analysis. Depress Anxiety. 2015;32(3):158–166. [DOI] [PubMed] [Google Scholar]
- 37.Frost RO, Ruby D, Shuer LJ.The Buried in Treasures Workshop: waitlist control trial of facilitated support groups for hoarding. Behav Res Ther. 2012:50(11):661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mathews CA, Uhm S, Chan J, et al. Treating hoarding disorder in a real-world setting: results from the Mental Health Association of San Francisco. Psychiatry Res. 2016;237:331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muroff J, Steketee G, Rasmussen J, et al. Group cognitive and behavioral treatment for compulsive hoarding: a preliminary trial. Depress Anxiety. 2009;26(7):634–640. [DOI] [PubMed] [Google Scholar]
- 40.Woody SR, Kellman-McFarlane K, Welsted A. Review of cognitive performance in hoarding disorder. Clin Psychol Rev. 2014;34(4):324–336. [DOI] [PubMed] [Google Scholar]


