Abstract
Ensuring that older adults in long-term care settings can effectively communicate is important. The goal of this study was to characterize key modifiable factors that could affect verbal communication in an adult day care setting, namely prevalence of audiometric hearing loss and the acoustic characteristics in the activity hall. The prevalence of age-related hearing loss among participants (n=51) was 71%, although only 15% of enrollees at the group care setting (n=21 of 140) used amplification. The noise and reverberation characteristics of the activity hall revealed signal-to-noise ratios of −3.1 decibels (dB) and −2.4 dB during morning activity and lunch, respectively, which are poorer than the recommended levels for understanding speech in background noise. Older adults attending adult day services are likely to spend the day in a room with acoustics that are too challenging to understand speech clearly. Opportunities to improve listening environments in group care settings for older adults are discussed.
Keywords: age-related hearing loss, adult day services
Effective communication is a key aspect of healthy aging. The ability to hear and communicate well can affect one’s social life and wellbeing. It can also affect one’s ability to perform everyday activities, such as grocery shopping and going to the post office, as well as more critical interactions such as medical appointments. While most older adults use compensatory skills to make up for age-related hearing loss that can impact communication, even mild hearing loss leads to increased cognitive load, stress, and fatigue as older adults navigate their daily interactions.1 Recent research on the impact of age-related hearing loss on healthy aging has emphasized the potential cascading pathways stemming from age-related hearing loss that lead to accelerated physical and cognitive declines.2 One critical step to treating age-related hearing loss as a public health priority is to recognize the needs and benefits of identifying hearing loss and creating good communication environments in places where older adults meet to engage socially with their peers.
Older adults have more difficulty understanding speech in noisy backgrounds than younger adults.3–6 Speech understanding difficulties are further exacerbated by the fact that a majority of adults older than 70 years have age-related hearing loss.7 Especially for adults with age-related hearing loss, the challenge of understanding speech in a noisy environment for extended periods contributes to increased cognitive demands that result in stress and fatigue.1,8 Moreover, many adults with age-related hearing loss experience more social isolation than their counterparts who do not have hearing loss.9–11 Social isolation and increased cognitive load have been hypothesized to contribute to accelerated rates of cognitive and physical declines observed in older adults with age-related hearing loss.2 One approach to reduce social isolation is participation in adult day services, which allows for older adults to engage in meals and activities during the day. However, for many older adults with untreated hearing loss, engagement in a noisy environment may prove difficult and even detrimental if the increased cognitive load lends itself to increased stress and fatigue.
The Program of All-Inclusive Care for the Elderly (PACE) is a unique, comprehensive care management program for adults older than 55 years who are nursing-home eligible but living in the community at time of enrollment.12 The interdisciplinary PACE team manages all medical and rehabilitation needs of each individual within a capitated financing structure. A key component of the PACE program is that most participants attend a day health center for meals, activities, and social engagement opportunities. Our research team wanted to evaluate the hearing loss burden and communication needs of participants at the day health center in order to improve program planning and management of hearing loss.
By evaluating the acoustic environment, we can estimate how well someone would be expected to understand speech in that environment. The measurements of background noise and speech output from the loudspeaker can be used to calculate the signal-to-noise ratio, which characterizes the level of the target signal (eg, speech) compared to the background noise level. By quantifying the signal-to-noise ratio available to listeners in the room when someone is making an announcement or leading an activity, we can make predictions as to how well participants can hear relevant speech in the activity hall. For example, in classroom environments, it is recommended that the signal-to-noise ratio for the teacher’s voice compared to the ambient noise levels be +15 decibels (dB) to ensure the ability of students to listen and learn.13 There are no specific recommendations for adult day services or long-term care (LTC) facilities, but we expect a similar need for an advantageous signal-to-noise ratio due to the difficulties many older adults have with understanding speech amid noisy backgrounds.
To characterize the burden of hearing loss in an exemplar PACE population, we wanted to know how many participants had difficulty hearing due to hearing loss as well as how the physical listening environment made understanding speech difficult. First, we determined the prevalence of hearing loss among participants who attend the day health center through voluntary on-site hearing tests. Next, we measured three acoustic features of the day health center: (1) the background noise level; (2) the average level of speech from the loudspeaker; and (3) reverberation characteristics of the activity hall. Background noise is made up of a combination of ambient sounds, such as heating/cooling systems or the hum of lights and other electronics, as well as the noises generated by people in the environment, such as talking and chairs being pushed across the floor. Reverberation is a measure of the amount of sound that reflects off hard surfaces in the environment. Rooms that have high reverberation have perceptible echos, which add to the background noise and may distort speech sounds.
Understanding the prevalence of hearing loss in an exemplar PACE population, as well as the acoustic characteristics of the activity hall, can directly inform strategies for addressing hearing loss and enhancing interpersonal communication. The goal of this study was to lay the groundwork for a communication intervention that addresses the group needs—both due to individual hearing loss and challenges from the physical environment.
Methods
Setting and Participants
The Hopkins ElderPlus PACE program is located at the Johns Hopkins Bayview Medical Center, in Baltimore, MD, and includes a hospital and specialty outpatient clinics. Total enrollment at the Hopkins ElderPlus PACE at the time of the study was 140 individuals; 80% of those are women. The racial demographics are approximately 62% black, 32% white, 4% Hispanic, and 3% other. Eligibility begins at age 55 years; two-thirds of PACE participants are between age 65 and 85 years. An average of 72 people are scheduled to attend the day health center each day, and the actual average attendance is 58 people. Each PACE participant has an individualized care plan, which determines how many days per week they are scheduled to attend the day health center for meals, activities, and/ or services from the interdisciplinary team, which could include social work, clinical nutrition, nursing, medical, acupuncture, podiatry, optometry, and physical and/or occupational rehabilitation services.
Hearing Testing
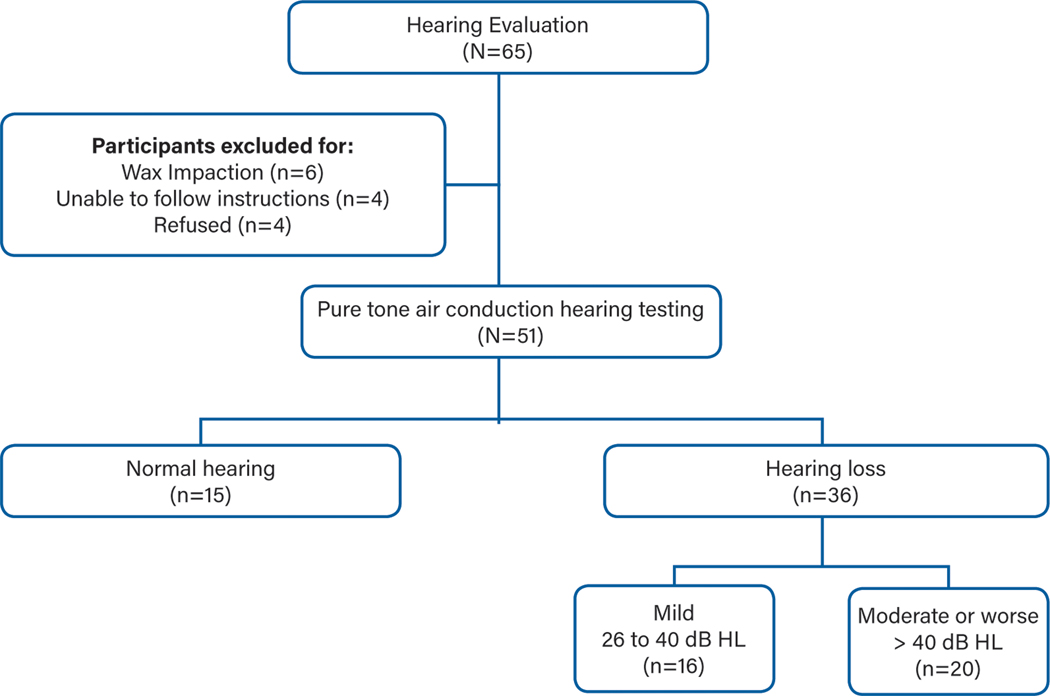
Over the course of several months, hearing tests were offered on-site to all attendees at the day health center. Participation was voluntary and included as a component of the comprehensive primary care provided at the day health center. Results were stored in each participant’s medical record to assist the interdisciplinary team with care planning for that individual. An explanation of the on-site test and results were sent home with the participant. Hearing tests were offered to 65 people, and 51 completed the testing. Of the 140 enrolled PACE participants, 134 were scheduled to attend the day health center at least once per week. Our convenience sample of 65 people was based on an attempt to offer testing several times each day of the week to test as many attendees as possible. Given the daily schedule of meals, activities, and other interdisciplinary team services (for some participants), not all attendees could be offered hearing tests during our period of data collection. For the 14 individuals who were offered but did not complete the hearing testing, reasons for not completing the test included being unable to follow instructions (n=4), impacted cerumen (n=6), and refusal (n=4). Approval to perform retrospective chart review for hearing test results was obtained by the Johns Hopkins School of Medicine Institutional Review Board.
Test Procedures
Testing was completed in a quiet office with insert or overthe-ear headphones using one of two portable audiometers (Interacoustics AS608 Screening Audiometer, Denmark; Clearwater Medical Shoebox Audiometry, Canada). Tests were performed by an audiologist, a trained research technician, or a trained post-doctoral fellow in geriatrics. Prior to selecting test sites, ambient noise levels were measured in all test sites to confirm appropriate test conditions per American National Standards Institute (ANSI) standards.14 Otoscopy was undertaken first to confirm the ear was not occluded with wax. If wax occlusion prevented the placement of the insert ear phones, the person was referred to the medical team for ear cleaning. Next, air conduction thresholds were obtained for octave frequencies from 500 to 8000 hertz (Hz) using a manual testing routine and a behavioral response to presented tones (ie, hand raise). To verify the reliability of the threshold responses, the response to 1000 Hz was tested twice in each ear. If the responses were not within ±5 decibels hearing level (dB HL), the test was considered unreliable. For determining the prevalence of hearing loss, a speech-frequency pure-tone average was calculated for each ear for the octave thresholds of 500, 1000, 2000, and 4000 Hz. Hearing loss was defined by the pure-tone average in the better hearing ear and categorized as normal hearing (≤ 25 dB HL), mild loss (26–40 dB HL), and moderate or worse loss (> 40 dB HL).
Acoustic Measurements
Ambient noise measurements were collected using a calibrated sound level meter after hours, when the room was unoccupied. Ambient noise reflects the sounds present when no person is creating the sound, such as air handlers, electrical systems, etc. A continuous recording was collected for 1 hour in accordance with the ANSI guidelines for ambient noise assessments in classrooms.13 Noise levels were reported in dBA, which represents a weighted average decibel level over the the length of the recording. Long-term average noise was also measured when the room was occupied in multiple locations throughout the activity hall for 1-hour intervals that covered activities and meal times. In addition, a sample of the level of speech output from the loudspeaker was collected at a distance of 1 meter from the speaker, and a sound dampening equation was used to calculate the estimated signal at the midway point (reference point) in the room. Using the speech output and background noise measures, a signal-to-noise ratio was derived, which reflects what the target signal (ie, speech) level is compared to the noise present in the environment.
Reverberation time (RT), a measurement of the length of time required for a sound to decay 60 dB from its initial sound level, was calculated in accordance with guidelines from the Acoustical Society of America (ASA).15 To calculate the RT, the volume of the room and area of all major surfaces (eg, cabinets) and objects (eg, tables, chairs) were measured. Using absorption coefficients from ASA, the RT was calculated using the Sabine formula to generate a noise reduction coefficient, which is a value that indicates how much of the sound in the room is absorbed when it hits that surface.16 Overall, the acoustic environment at the Hopkins ElderPlus Day Health Center was analyzed in terms of ambient noise when unoccupied, background noise when occupied during morning activity and lunch, reverberation coefficient, and signal from the loudspeaker.
Results
Hearing Testing
Using a 4-frequency pure tone average from the betterhearing ear, the average hearing threshold was 33.9 dB HL (standard deviation=14.3), which is consistent with mild hearing loss. Figure 1 shows the number of participants per hearing loss category. In this convenience sample (N=51), 71% (n=36) of those tested had at least a mild hearing loss in their better-hearing ear. Nearly 40% (n=20) of those tested had a moderate or worse degree of hearing loss, which is considered a disabling hearing loss by the World Health Organization.17 Of the 36 participants with hearing loss, only two were active hearing-aid users (one binaural, one monaural), and one person reported having tried hearing aids in the past. All three of these participants had moderate or worse hearing loss in the better-hearing ear. While only 35% (n=18) of participants indicated per self-report that they had a hearing loss, 71% had a hearing loss per objective test results.
Figure 1.
Prevalence of hearing loss among attendees at the Hopkins ElderPlus Program of All-Inclusive Care for the Elderly (PACE) Day Health Center.
Abbreviations: db, decibels; HL, hearing level.
Acoustic Measurements
The ambient noise measurement in the unoccupied room was 56.4 dBA over a 1-hour period in an unoccupied room. It should be noted that, while the room was unoccupied, there were still employees in the hallway and traffic outside the windows, which could potentially inflate this ambient noise measure. The average noise level was 73.9 dBA during morning activity and 73.2 dBA during lunch. The target signal (ie, speech from the loudspeaker) was 80.3 dBA, which was estimated by measuring the weighted signal from the main sound source (loudspeaker) at a distance of 1 meter. By using the equation for sound dampening across distance, the signal estimate at the midway point in the room was 70.8 dBA (ie, the level of speech was softer at a distance farther than 1 meter). Given the average background noise measured during activities, the signal-tonoise ratio for announcements made over the loudspeaker during morning activity and lunch was −3.1 dB and −2.4 dB, respectively. When the signal-to-noise ratio is a negative value, that means the target signal (eg, speech) is not as loud as the background noise, which results in a very difficult listening situation.
Finally, the RT of the room is 0.37 seconds. This RT value is within the recommended limits for classroom acoustics; as such, it will not be discussed further.13
Discussion
Results from the hearing testing revealed that the prevalence of hearing loss among this convenience sample of older adults attending a PACE day health center is consistent with national estimates, with more than two-thirds of older adults experiencing age-related hearing loss.7 Importantly, the acoustics in the large activity hall where the PACE activities and meals take place also create a challenging listening environment, especially for those with age-related hearing loss. Furthermore, it is likely that adults who have hearing loss and cognitive impairment experience increased difficulty in challenging listening environments due to reduced cognitive resources to manage the difficult cognitive load of speech perception in background noise.1,18
This study provides data to support what has likely long been assumed by people working in LTC settings: a majority of the participants have at least a mild hearing loss, and noisy environments for group activities and meals make communication difficult. It is particularly important to consider these facts in the context of the need for maintaining social engagement to promote healthy aging. A major benefit of adult day services and other group care activities is that individuals are not socially isolated. However, if hearing loss is not addressed and steps are not taken to optimize the listening environment, some individuals may experience increased stress and fatigue.
By simply quantifying the number of participants who could benefit from hearing loss treatment, the PACE team was able to begin to consider changes in group program planning that would benefit the group as a whole, such as making a change to the activity hall sound system—a useful adaptation given that a majority of the participants would benefit. Other potential interventions might include reducing the level of the background music commonly played during lunch at group care settings. In addition, simple headset amplification systems (eg, Pocketalker®) can be used as needed to improve one-on-one communication for individuals with untreated hearing loss. Finally, inviting a local audiologist to provide an in-service training on communication strategies to use with adults with hearing loss may help the staff be cognizant of their own communication behaviors.
There are no guidelines for acoustic environments in LTC settings. Well-established standards for ambient noise in classrooms state that unoccupied room ambient noise should not exceed 35 dBA.13 By comparison, the ambient noise measured in this study was too high at 56.4 dBA. While classroom acoustics recommendations are based on the need for children to learn new information, similarly enhanced listening environments are necessary for successful communication for older adults. The recommended target signal for classroom learning is +15 dB signal-to-noise ratio.13,19 Due to the high noise levels in the activity hall, the signal-to-noise ratio we estimated in this study was negative—meaning, the average noise was more intense than the target speaker throughout much of the room. There is extensive literature focused on the need for an enhanced signal-to-noise ratio for older adults to understand speech in noisy backgrounds as compared to young adults.20–22 For example, one study demonstrated that older adults with a mild degree of hearing loss needed a +10 dB signal-to-noise ratio to get 50% correct speech understanding of sentences in the presence of complex background noise.23 Importantly, older adults with hearing loss in that study needed an improvement of +20 dB signal-to-noise ratio compared to younger adults with normal hearing. This experimental evidence lends support to the argument that older adults in a noisy group care environment need an enhanced signalto-noise ratio (ie, improved access to the speech signal) to communicate well and engage in activities.
When faced with a negative signal-to-noise ratio, most listeners use compensatory strategies, such as context and visual cues. Using such compensatory strategies is known as effortful listening, which requires additional cognitive resources and can lead to fatigue and lack of motivation to expend the energy and attention necessary to communicate.18 When the listening becomes too difficult, many people use maladaptive behaviors such as bluffing or withdrawal. By improving the listening environment and the communication practices used in group settings, we can minimize maladaptive behaviors and support positive communication experiences.
There is a substantial body of evidence for the need to enhance social engagement to support healthy aging for older adults.24 However, if communication is too difficult in the space meant to support social engagement, it may be detrimental. To support communication opportunities for older adults, there need to be standards in place that create good environmental conditions for group care settings. Fortunately, environmental modifications can reduce high reverberation times (ie, echos) and absorb background noise in order to enhance speech intelligibility (Box 1).25 In addition, we have been working with our PACE partners to understand staff perception of communication difficulties and create experiential in-service trainings to learn good communication strategies.26
Box 1. Potential low-cost acoustic modifications.
Absorption fabric on walls and cabinets
Sound dampening carpet
Tablecloths
Moveable partitions or drapes to block off areas of excessive noise (eg, food prep)
A diffuse sound field system (ie, mounted speakers in multiple locations)
This study had several limitations. For hearing loss prevalence, we only offered hearing tests to approximately half of the total Hopkins ElderPlus PACE enrollment at the time. We were limited by not having results on individuals who could not follow instructions and complete the test (n=6). These individuals had severe cognitive impairment and represent a particularly vulnerable population. It is important to note that individuals who were unable to complete a simple behavioral hearing test on-site may benefit from a diagnostic evaluation with an audiologist to determine their hearing sensitivity in order to develop each person’s individualized health care plan. Nevertheless, combining the quantifiable burden of hearing loss with the acoustic characteristics of the environment during daily activities yields a useful context from which to consider the extent of the burden of hearing loss in group care settings.
Conclusion
Future research on the acoustic environments of group care settings for older adults should use a personal noise monitor on specific individuals to investigate comprehensive analyses of the sound environment throughout the day and inform targeted solutions to maximize signal-to-noise ratio during the most important times of the day, such as during guided activities and mealtimes. This in-depth approach to evaluating the communication environment could lead to group-level solutions that enhance engagement opportunities for many individuals rather than addressing communication needs one person at a time.
Acknowledgements:
The research support of Olivia Nirmalasari, Dona Occhipinto, and Alexandra Pletnikova to collect hearing status data and Jon Suen for collecting background noise samples is gratefully acknowledged.
Footnotes
Disclosures:
Dr Lin reports being a consultant to Cochlear and Amplifon. The remaining authors report no relevant financial relationships. This work was supported by the American Academy of Audiology (SKM), the National Institutes of Health (K23AG043504 (ESO)), the Roberts Fund (ESO), and the Eleanor Schwartz Charitable Foundation (FRL).
References
- 1.Lemke U, Besser J. Cognitive load and listening effort: Concepts and age-related considerations. Ear Hear. 2016;37(suppl 1):77S–84S. [DOI] [PubMed] [Google Scholar]
- 2.Lin FR, Albert M. Hearing loss and dementia-who is listening? Aging Ment Health. 2014;18(6):671–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pichora-Fuller MK, Schneider BA, Daneman M. How young and old adults listen to and remember speech in noise. J Acoust Soc Am. 1995;97(1):593–608. [DOI] [PubMed] [Google Scholar]
- 4.Humes LE, Dubno JR. Factors affecting speech understanding in older adults. In: GordonSalant S, Frisina RD, Popper AN, Fay RR, eds. The Aging Auditory System. New York, NY: Springer-Verlag; 2010. [Google Scholar]
- 5.Humes LE, Dubno JR, Gordon-Salant S, et al. Central presbycusis: a review and evaluation of the evidence. J Am Acad Audiol. 2012;23(8):635–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helfer KS, Freyman RL. Stimulus and listener factors affecting age-related changes in competing speech perception. J Acoust Soc Am. 2014;136(2):748–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med. 2011;171(20):1851–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pichora-Fuller MK. How social psychological factors may modulate auditory and cognitive functioning during listening. Ear Hear. 2016; 37(suppl 1):92S–100S. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein BE, Ventry IM. Hearing impairment and social isolation in the elderly. J Speech Hear Res. 1982;25(4):593–599. [DOI] [PubMed] [Google Scholar]
- 10.Mick P, Kawachi I, Lin FR. The association between hearing loss and social isolation in older adults. Otolaryngol Head Neck Surg. 2014;150(3):378–384. [DOI] [PubMed] [Google Scholar]
- 11.Mick P, Parfyonov M, Wittich W, Phillips N, Guthrie D, Pichora-Fuller MK. Associations between sensory loss and social networks, participation, support, and loneliness: analysis of the Canadian Longitudinal Study on Aging. Can Fam Physician. 2018;64(1):e33–e41. [PMC free article] [PubMed] [Google Scholar]
- 12.Mui AC. The Program of All-Inclusive Care for the Elderly (PACE): an innovative long-term care model in the United States. J Aging Soc Policy. 2001;13(2–3):53–67. [DOI] [PubMed] [Google Scholar]
- 13.American National Standards Institute Inc. American National Standard Acoustical Performance Criteria, Design Requirements, and Guidelines for Schools. Accredited Standards Committee S12, Noise. Melville, NY: Acoustical Society of America; 2002. [Google Scholar]
- 14.Frank T. ANSI update: maximum permissible ambient noise levels for audiometric test rooms. Am J Audiol. 2000;9(1):3–8. [DOI] [PubMed] [Google Scholar]
- 15.Acoustical Society of America (ASA). Classroom acoustics: a resource for creating learning environments with desirable listening conditions. ASA website. https://acousticalsociety.org/wp-content/uploads/2018/02/classroom_acoutics_1.pdf Published 2000. Accessed Augusr 15, 2019.
- 16.Acoustical Society of America (ASA). Classroom acoustics for architects: a companion booklet for ANSI/ASA S12.60 Parts 1 and 2. ASA website. https://acousticalsociety.org/wp-content/uploads/2018/02/Classroom_Acoustics_for_Architects_4_18_15.pdf. Accessed Augusr 15, 2019.
- 17.World Health Organization (WHO). WHO: report of the first informal consultation on future programme developments for the prevention of deafness and hearing impairment. Published 1997. [Google Scholar]
- 18.Pichora-Fuller MK, Kramer SE, Eckert MA, et al. Hearing impairment and cognitive energy: the framework for understanding effortful listening (FUEL). Ear Hear. 2016;37(suppl 1):5s–27s. [DOI] [PubMed] [Google Scholar]
- 19.American Speech-Language-Hearing Association (ASHA) Working Group on Classroom Acoustics. Guidelines for addressing acoustics in educational settings. ASHA website. http://www.asha.org/uploadedFiles/elearning/jss/6173/6173Article4.pdf. Published 2005. Accessed Augusr 15, 2019.
- 20.Plomp R, Mimpen AM. Speech-reception threshold for sentences as a function of age and noise level. J Acoust Soc Am. 1979;66(5):1333–1342. [DOI] [PubMed] [Google Scholar]
- 21.Helfer KS, Wilber LA. Hearing loss, aging, and speech perception in reverberation and noise. J Speech Hear Res. 1990;33(1):149–155. [DOI] [PubMed] [Google Scholar]
- 22.Humes LE. Understanding the speech-understanding problems of older adults. Am J Audiol. 2013;22(2):303–305. [DOI] [PubMed] [Google Scholar]
- 23.Goossens T, Vercammen C, Wouters J, van Wieringen A. Masked speech perception across the adult lifespan: impact of age and hearing impairment. Hear Res. 2017;344:109–124. [DOI] [PubMed] [Google Scholar]
- 24.Johnson KJ, Mutchler JE. The emergence of a positive gerontology: from disengagement to social involvement. Gerontologist. 2014;54(1):93–100. [DOI] [PubMed] [Google Scholar]
- 25.Hull RH. Environmental design--an expanding role in hearing rehabilitation for older adults. J Rehabil Res Dev. 2011;48(5):xv–xviii. [DOI] [PubMed] [Google Scholar]
- 26.Mamo SK, Mayhew SJ, Nirmalasari O, et al. Age-related hearing loss and communication at a PACE Day Health Center. J Am Med Dir Assoc. 2018;19(5):458–459. doi: 10.1016/j.jamda.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]