Highlights
-
•
The severity of SARS-CoV-2 patients is difficult to quickly assess in the ED.
-
•
The ABG test is a quick and easy tool that can help identify more severe patients.
-
•
CT cannot be used on all suspected SARS-CoV-2 infected patients admitted in ED.
-
•
The CT volumetry correlates well with the values of severity reported by the ABG test.
Keywords: Arterail blood gas, COVID-19, SARS-CoV-2, CT volumetry, Emergency department, Emergency medicine, COVID-19 pneumonia
The extent of pulmonary inflammation caused by SARS-CoV-2 infection seems to correlate well with the patient's prognosis, but not with the severity of clinical manifestations presented at first evaluation in the emergency department (ED) (Colombi et al., 2020, Grasselli et al., 2020). Clinically, a non-negligible percentage of patients with mild symptoms on ED arrival may develop acute respiratory distress syndrome over the next hours (Paules et al., 2020). Therefore, tools to rapidly identify the extent of the ongoing inflammatory processes are essential. Chest CT appears to be the most effective diagnostic tool for COVID-19 pneumonia, and the morphology of the lung lesions seems to correlate with the severity of the inflammatory process (Colombi et al., 2020, Zhang et al., 2020, Dai et al., 2020). However, extensive use of CT on patients leads to an increased risk of radiological exposure and, possibly, a high number of negative scans. Recently, Shang et al. suggested that arterial blood gas (ABG) values may correlate with the presence and morphological characteristics of CT lesions (Shang et al., 2020). If this early evidence were confirmed, ABG, a rapid, inexpensive, and widely used test might become a valuable tool for the preliminary prognostic assessment of patients with SARS-CoV-2 infection in the ED.
This preliminary study was designed to investigate whether an ABG performed on patient arrival in the ED correlates with the extent of the pulmonary inflammatory process and with the prognosis in patients with SARS-CoV-2 infection.
From March 20, 2020, to April 10, 2020, in the ED of the Merano Hospital (Italy), all patients consecutively evaluated for a suspected SARS-CoV-2 infection were subjected to an ABG test and chest CT. ABG was performed in all suspected patients immediately after arrival in the ED. Retrospectively, only patients who tested positive by polymerase chain reaction for SARS-CoV-2 were included in the present study.
ABG values at ED admission were compared both with the volume of lung parenchyma involved in the inflammatory process (calculated as a percentage of the total lung volume) using Pulmo3D® software (Siemens Healthineers, Erlangen, Germany) and with mortality at 28 days.
Seventy-nine consecutive SARS-CoV-2 patients underwent CT and ABG during the study period. The median age of the patients was 68 years (range 61–78), and the majority were male (69.6%). The median percent extension of the pulmonary inflammatory process was 14.3% (5.0%–25.2%). Nine patients (11.4%) died within 28 days of ED evaluation.
Among the ABG indices, PaO2:FiO2 had an inverse correlation with the percent extension of the pulmonary inflammatory process on CT (r = −0.451, p < 0.001), as did PCO2 (r = −0.294, p = 0.009) and SpO2 (r = −0.444, p < 0.001), while pH had a direct correlation (r = 0.228, p = 0.044).
Patients who had died at 28 days presented reduced values of PaO2:FiO2 (215 versus 314, p = 0.005), PCO2 (26.6 versus 31.5, p = 0.049), and SpO2 (82.7 versus 92.3, p = 0.003) on arrival in the ED (Table 1 ).
Table 1.
Arterial blood gas test values in patients enrolled in the study, divided according to the median percentage of the extension of the pulmonary inflammatory process (14.3%).
| Parenchymal involvement < 14.2% | Parenchymal involvement > 14.2% | p | |
|---|---|---|---|
| Patients, n (%) | 40 (50.6) | 39 (49.4) | |
| Age, years, median (IQR) | 64 (57–74) | 72 (65–82) | 0.010 |
| Male, n (%) | 24 (60.0) | 31 (79.5) | 0.087 |
| Onset of symptoms, days (IQR) | 5 (2–10) | 5 (3–10) | 0.715 |
| Polycomorbidities | 15 (37.5) | 28 (71.8) | 0.003 |
| Arterial blood gas test | |||
| pH | 7.44 (7.42–7.49) | 7.45 (7.43–7.48) | 0.520 |
| PaO2 (mmHg) | 71.8 (62.5–80.8) | 62.9 (53.6–73) | 0.013 |
| PaCO2 (mmHg) | 35.9 (32.1–38) | 32.3 (31–36.8) | 0.080 |
| HCO3 | 24 (23.1–26.4) | 23.9 (21.5–26.6) | 0.430 |
| PaO2:FiO2 (mmHg) | 335 (293–365) | 250 (198–314) | <0.001 |
| SpO2 | 95.3 (94.3–97) | 92.8 (89.1–95.4) | 0.002 |
| Deaths within 28 days | 2 (5.0) | 7 (17.9) | 0.087 |
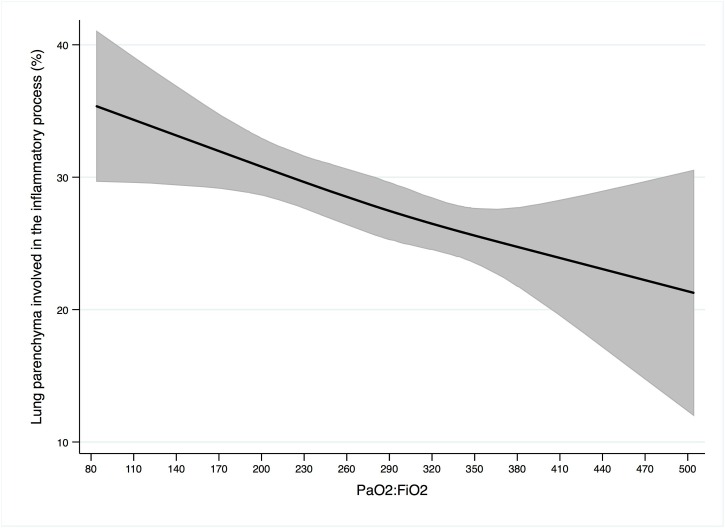
The regression cubic spline model revealed that reduced PaO2:FiO2 values are associated with a higher percentage of the lung being involved in the inflammatory process, as detected on CT (Figure 1 ).
Figure 1.
Restricted cubic spline model of the dose-response relationship between the PiO2:FiO2 values recorded on patient arrival in the ED and the percentage of the volume of lung parenchyma involved in the inflammatory process in patients with SARS-CoV-2 infection. The black line represents the pooled probability of the percentage of lung parenchyma involved in the inflammatory process linked to PiO2:FiO2 values and the grey lines indicate the 95% confidence interval.
Preliminary data from this study suggest that values from an ABG test performed upon arrival of a patient with SARS-CoV-2 in the ED may correlate with the extent of the pulmonary inflammatory process and provide indications of the patient's prognosis.
The correlation between ABG indices and CT morphological evaluation of patients with COVID-19 pneumonia has recently been reported. Shang et al. demonstrated a moderate correlation between the presence of ground-glass opacities (GGO) and pulmonary fibrosis on the chest CT with the oxygen index and PO2 and a weak correlation with PCO2 (Shang et al., 2020). These results are in line with the correlations observed in the data from this study, in which a higher percentage of the lung being involved in the inflammatory process, as reconstructed on the CT scan, appears to correlate with decreased oxygenation capacity. The presence of diffuse bilateral GGO, causing exclusion of pulmonary parenchyma (consolidations) and air trapping, has been previously identified in clinically severe patients (Dai et al., 2020). This could explain the difficulty of oxygenating the blood, even with high FiO2 values, and for this reason, an initially low PaO2:FiO2 index appears to underline the severity of the patient.
Colombi et al. suggested that software-based reconstruction of the quantity of well-ventilated lung at CT (and thus indirectly the severity of the extension of the pulmonary inflammatory process) can improve the estimation of the patient's severity compared to the morphological evaluation alone (Colombi et al., 2020).
Reduced ABG values on ED arrival may suggest a greater underlying extension of the inflammatory process and thus identify a patient who may present an increased prognostic risk even if not clinically compromised.
Further confirmatory data are required, but the results of this study suggest that in patients with SARS-CoV-2, the ABG test will be an important tool in the ED due to its rapidity and applicability.
Ethical approval
This study was approved by the local ethics committee (Protocollo nr. 57-2020).
Conflict of interest
None.
Funding source
None.
References
- Colombi D., Bodini F.C., Petrini M., Maffi G., Morelli N., Milanese G. Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology. 2020;(April) doi: 10.1148/radiol.2020201433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H., Zhang X., Xia J., Zhang T., Shang Y., Huang R. High-resolution chest CT features and clinical characteristics of patients infected with COVID-19 in Jiangsu, China. Int J Infect Dis. 2020;95(April):106–112. doi: 10.1016/j.ijid.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections-more than just the common cold. JAMA. 2020;323(8):707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- Shang Y., Xu C., Jiang F., Huang R., Li Y., Zhou Y. Clinical characteristics and changes of chest CT Features in 307 patients with common COVID-19 pneumonia infected SARS-CoV-2: a multicenter study in Jiangsu, China. Int J Infect Dis. 2020;96(May):157–162. doi: 10.1016/j.ijid.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N., Xu X., Zhou L.Y., Chen G., Li Y., Yin H. Clinical characteristics and chest CT imaging features of critically Ill COVID-19 Patients. Eur Radiol. 2020;30:1–10. doi: 10.1007/s00330-020-06955-x. [DOI] [PMC free article] [PubMed] [Google Scholar]