The coronavirus disease 2019 (COVID-19) pandemic has led to radical curtailing and reconfiguring of health services across the world to slow the spread of the disease. Planning for acute COVID-19 services has inevitably resulted in a precipitous reduction in endoscopy activity, but in the deceleration phase of the pandemic, endoscopy units will aim to restart. The primary concern will understandably be to protect patients and staff, while providing enough capacity to meet demand and manage postponed appointments.
However, it is crucial that we also use this time to analyse current practice in the context of another sustained and serious threat: climate change. The climate crisis has major consequences for global health, including food insecurity, respiratory and vector-borne diseases, and excess heat-related deaths, even in the UK.1 The National Health Service (NHS) accounts for 5·4% of UK carbon dioxide emissions,2 which, in 2015, amounted to 26·6 million tonnes of carbon dioxide equivalent—equating to 39% of all public sector emissions in England.3 Even during the brief period of lockdown around the world, the reduction in global activity has led to a decrease in greenhouse gas emissions by as much as 5·5%,4 and potentially thousands of lives saved through cleaner air.5 This drop might seem substantial but emissions will rebound rapidly once lockdowns end. If there is to be any chance of limiting global heating to less than 1·5°C above pre-industrial temperatures, year-on-year reductions of more than 7·6% are required for the next decade.6 Radical change is necessary across every part of society, and health care must be included in the process, both because of the health service's role as a major contributor to the problem but also because of the serious public health risks posed by climate change.1
Endoscopy appears to be a major contributor to the environmental footprint of health care, generating about 3·09 kg of waste per bed per day (the third highest emitting hospital department).7 High throughput caseloads, multiple non-renewable waste streams, numerous hospital visits for patients and relatives, and resource-heavy decontamination processes all contribute. Although some processes are necessary, others are ripe for change. Endoscope decontamination, for example, requires high volumes of water per decontamination cycle and multiple disinfectants, and has a major environmental impact as a result. There are no robust data on transport for patients and relatives, departmental energy use, and reusable versus disposable equipment.
The call for evidence to inform the NHS Net Zero8 plan is an important development, seeking practical ideas to achieve net carbon zero by 2050. The National Institute for Health and Care Excellence (NICE) has placed sustainability at the centre of their strategy,3 and numerous other organisations are springing up among concerned health-care professionals to make a difference on a regional, national, and international level. The gastroenterology community should be a part of this movement. Practitioners ought to review procedures against the principles of sustainable health care—prevention, patient empowerment and self-care, lean systems, and low-carbon alternatives—and identify areas amenable to transformation.
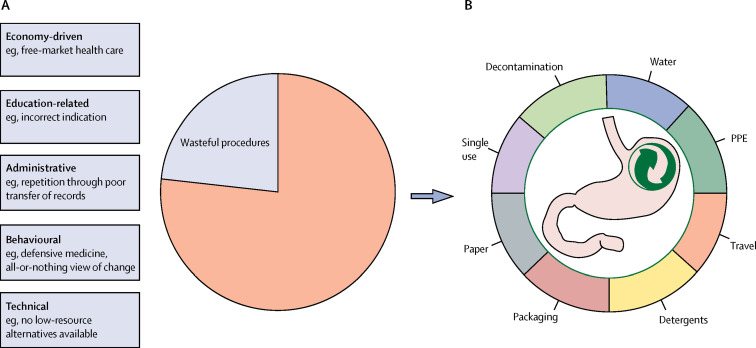
We can begin by looking at the total number of procedures done, the reasons leading to potentially unnecessary processes, and the waste products involved (figure ). Small but successive steps to analyse and change practice can have a substantial cumulative benefit. The magnitude of the problem as a whole should not engender inertia or act as a barrier to change.
Figure 1.
Potential targets for greener endoscopy
(A) Reducing unnecessary procedures by analysing the drivers behind them. (B) Reducing the environmental impact of each procedure through identifying areas of excess waste. PPE=personal protective equipment.
Undoubtedly, the approach likely to have the greatest impact will be to do fewer procedures, while recognising that endoscopy is a key component in the management of digestive diseases. Robust management of demand is axiomatic but will require an honest appraisal of our current values—for many, the natural inclination is to do more procedures, yet a reduction in endoscopic burden could be beneficial for patients. There are many drivers of increased endoscopy activity (figure, A), many of which result in unnecessary endoscopies. Identifying these unnecessary procedures and their primary drivers is an important first step. Potential solutions include rigorously checking the appropriateness of referrals, using low-waste alternatives (eg, faecal immunochemical tests, faecal calprotectin, video capsules, or CT where appropriate), or home testing to reduce travel (where technology allows and after effectiveness and safety have been established).
Such a strategy could pose a challenge for health-care systems that rely on the income generated by low-risk, high-throughput endoscopy. A considerable change in outlook from society as a whole is required but we argue that, although eschewing value-based health care for financial gain remains very much part of the problem, sustainable health care is not necessarily associated with financial losses in most settings.
A clear indication of the environmental impact of each procedure is required (figure). This insight could generate targeted interventions such as improved waste segregation, increased recycling, or the avoidance of single-use items where possible. Detailed analyses of the sustainability of each step in endoscopy activities would allow the identification of small but cumulative beneficial changes that could decrease our environmental impact.
There is an urgent unmet need for research on sustainable practice in endoscopy: from optimal service delivery models to greener technology and the effects of climate change on the health of patients with gastrointestinal disease. As our knowledge base develops, there needs to be a renewed drive to disseminate this information. Sustainable health care should be a central theme in undergraduate and postgraduate curricula, and a major consideration for patient groups who educate patients about developments in practice and technology.
Finally, physicians and researchers need to re-invent what endoscopy will look like in the long term. Practitioners should commit to importing the principles of sustainable health care into a new system for doing endoscopy. National bodies could also assist by evaluating endoscopy units, which could involve so-called green accreditation through meeting certain standards of sustainable practice. Action can, and must, also be taken at an individual level: an all-or-nothing approach risks inertia and prevents adoption of small changes that together could have a large effect.
This vision for disruptive innovation seemed challenging just a few months ago, but the COVID-19 pandemic has shown how rapidly processes can change when faced with a crisis. Although the recent pause has given us time to reflect on current practice, the climate crisis is still accelerating. Endoscopy and its associated specialities remain part of the problem. As we consider restarting endoscopy services, we should use this opportunity to rapidly embed sustainability principles into everyday practice and trigger action in a timely and strategic manner. We can and must act quickly and radically with our colleagues across health care, the public, and government. We must reinvent endoscopy and how we live our professional lives with a view to protecting the planet on which we rely.
For organisations engaging health-care workers in action on climate change see http://noharm.org/, https://www.medact.org/, and http://www.ukhealthalliance.org/
Acknowledgments
JBM reports non-financial support from Norgine and personal fees and non-financial support from Intercept Pharma, outside the submitted work. SS reports research grants from Takeda, Pfizer, Tillotts Pharma, and Amgen; speaker fees or advisory board honoraria fees, or both, from Pfizer, Takeda, Tillotts Pharma, Pharmacosmos, Janssen, Amgen, and AbbVie, outside the submitted work. BH reports grants from Olympus Medical UK and Fujifilm Europe; personal fees from Takeda and AbbVie; and board membership and shares in Ampersand Health and Surgease Medical; none of these relationships represent interests that relate to the work presented in this manuscript. All other authors declare no competing interests.
References
- 1.Royal College of Physicians Breaking the fever: sustainability and climate change in the NHS. March 15, 2017. https://www.rcplondon.ac.uk/projects/outputs/breaking-fever-sustainability-and-climate-change-nhs
- 2.Pichler P-P, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Lett. 2019;14 [Google Scholar]
- 3.National Institute for health and Care Sustainability. https://www.nice.org.uk/about/who-we-are/sustainability
- 4.UN News Fall in COVID-linked carbon emissions won't halt climate change—UN weather agency chief. April 22, 2020. https://news.un.org/en/story/2020/04/1062332
- 5.The Guardian Clean air in Europe during lockdown ‘leads to 11,000 fewer deaths’. April 30, 2020. https://www.theguardian.com/environment/2020/apr/30/clean-air-in-europe-during-lockdown-leads-to-11000-fewer-deaths
- 6.UN Environment Programme Cut global emissions by 7.6 percent every year for next decade to meet 1.5°C Paris target—UN report. Nov 26, 2019. https://www.unenvironment.org/news-and-stories/press-release/cut-global-emissions-76-percent-every-year-next-decade-meet-15degc
- 7.Vaccari M, Tudor T, Perteghella A. Costs associated with the management of waste from healthcare facilities: an analysis at national and site level. Waste Manag Res. 2018;36:39–47. doi: 10.1177/0734242X17739968. [DOI] [PubMed] [Google Scholar]
- 8.NHS England NHS Net Zero—Call for evidence. Jan 25–March 22, 2020. https://www.engage.england.nhs.uk/survey/nhs-net-zero/