Abstract
Background
The COVID-19 pandemic has generated a new era in the world while we still figure out the consequences in different aspects of our daily life. The food supply chain and the food industry do not comprise an exception.
Scope and approach
This review summarizes the possible transmission ways of COVID-19 through the foods, food supply chain, surfaces, and environment before exploring the development of corresponding detection tools of SARS-CoV-2. For the time being, the possibility of transmission through the food sector is considered negligible, and tracing of SARS-CoV-2 in working environments is not considered as a priority by public authorities. However, the adverse effects on the environment, food systems, and people along the food supply chain are already evident.
Key findings and conclusions
As long as we move from farm to fork, more safety measures are needed since more people (and subsequently more potential sources of infection) are involved in the process. The need for developing respective bioanalytical protocols for food and environmental safety applications to adapt in the post-lockdown period is also highlighted.
Keywords: Food safety, Supply chain, After lockdown, Swab tests, Virus detection, SARS-CoV-2
1. Introduction
The novel coronavirus SARS-CoV-2 is known to cause COVID-19, which is an easily transmissible disease spreading from person to person via cough, sneeze, respiratory droplets, or exhale (ECDC, 2020a). The symptoms of COVID-19, which appear approximately 5 days after infection, are relevant to flu (e.g., fever, and coughing), but also include other ones like sore throat, muscle aches (CDC, 2020a) and loss of taste or smell (Bienkov, 2020). The COVID-19 has similar clinical presentation and characteristics with two well-known diseases of the lower respiratory tract Severe Acute Respiratory Syndrome: “SARS-CoV” and Middle East Respiratory Syndrome: “MERS” (Das, 2020).
Coronaviruses circulate among animals, and in some cases, may infect humans. Indeed, MERS, SARS-CoV, and SARS-CoV-2 may be attributed to zoonotic transmission (Das, 2020; Rodriguez-Morales et al., 2020). However, SARS-CoV-2 is the only one with pandemic potential (Mackenzie & Smith, 2020). Consumption of exotic mammals like horseshoe bats, which comprise a vast reservoir of SARS-CoV-related viruses, enhances the possibility that novel viruses emerged from animals, or relevant environments (Cheng et al., 2007). The first infections of SARS-CoV2 were associated with Huanan Seafood Market (Li et al., 2020), where live and slaughtered bats, snakes, marmots, pheasants and organs of rabbits and deer are sold (Jalava, 2020). Zhou et al. (2020) suggested bats as a possible source of SARS-CoV2 since the latest has a similar gene sequence (up to 96.2%) with coronavirus that exist in bats. However, other animals may also be natural hosts for SARS-CoV2. For instance, MERS-CoV and SARS-CoV may be transmitted to humans from camels and civet cats, respectively (ECDC, 2020b).
SARS-CoV-2 was identified within December 2019, and approximately 3 months later, COVID-19 declared by WHO as a pandemic (WHO, 2020f). On May 30th, 2020, the COVID-19 pandemic had spread to over 5.9 million people in more than 188 countries, leading to over 365,000 deaths (Dong et al., 2020) and lockdown of one-third of the world's population (Kaplan et al., 2020). At the moment (May 30th, 2020), no universal treatment, cure, or vaccine has been developed for COVID-19 disease. The scientific community, authorities, food safety inspectors and professionals in the food industry are emergently seeking insights on how to manage the pandemic, e.g, understanding the transmission routes, and developing treatment and vaccines. It is also essential to develop innovative diagnostics for SARS-CoV-2 not only for infected people but also for food, surfaces, and surrounding environments. This article explores the possibility of COVID-19 transmission through the food supply chain before discussing the development of respective detection tools for food and environmental safety applications.
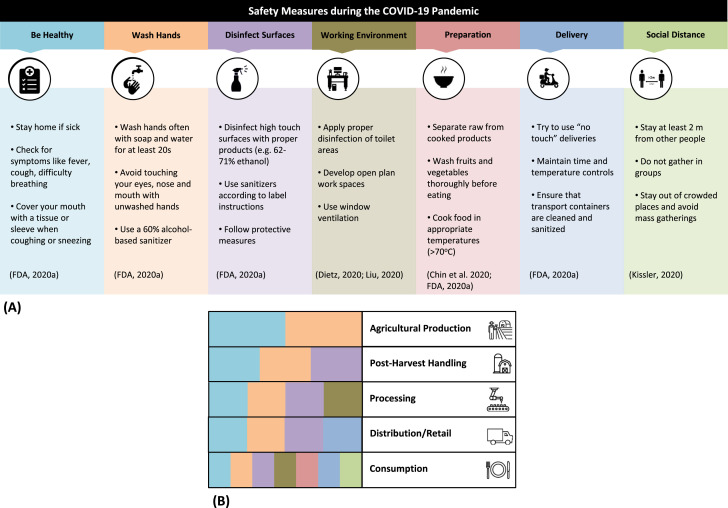
2. Safety of foods and measures in the food supply chain
Food safety is among the four pillars of the food systems affected in the era of the coronavirus (COVID-19) pandemic (Galanakis, 2020). Fig. 1 summarizes the proposed safety measures for the food sector during the pandemic (Fig. 1A), emphasizing the most critical precautions needed for each stage of the food supply chain from farm to fork (Fig. 1B). Actions are grouped in workers' medical condition (e.g., stay home if sick), personal hygiene (e.g., wash hands), disinfection of surfaces, keeping working environments clean, food preparation and delivery, and finally social distancing. Although these measures apply in all five stages of the food chain, most precautions are critically necessary at the last stages (e.g., consumption). This observation is generated by the fact that the more we move to the final stages of the food supply chain, the more people (potential sources of infection) are involved. Moreover, it is of the highest importance for the food sector to ensure that the food reaching consumers’ plate is safe and does not risk their health in any step of the process (e.g., even at the moment of delivery).
Fig. 1.
Safety measures for the food sector during the pandemic (Fig. 1A) and the most critical for each stage of the food supply chain from farm to fork (Fig. 1B).
Besides, there are precaution measures (e.g., during food preparation) that mostly apply to the consumption stage. For instance, at the beginning of the crisis, many restaurants, cafeterias, and health authorities in Central Europe stopped serving rare steaks and meats as a general precaution measure (Euractiv, 2020) against viruses and pathogens even though foodborne transmission of SARS-CoV-2 is unsupported by scientific evidence. Moreover, in the United States, some of the largest beef-packing and meat processing companies and announced plant closures (Reiley, 2020). Nonetheless, these plants closed when employees tested positive for COVID-19, not because of the virus transmission from raw meat; this is why FDA did not anticipate that food products need to be recalled from the market (FDA, 2020c).
A few weeks later, the majority of restaurants and cafeterias around the world lockdown and remain functional only for take-away or delivery services. To this line, the transmission of SARS-CoV-2 is monitored closely by the food safety authorities around the world, like the European Food Safety Authority (EFSA) and the United States Food and Drug Administration (FDA). Both organizations agree that up to now (the 30th of May 2020), there is no evidence that food is a likely route of transmission; however, they continue to gather information related to the potential persistence of the virus on foods.
Food was not a transmission route in previous outbreaks (MERS and SARS-CoV) (EFSA, 2020; FDA, 2020c), while it is known that the acidic conditions of the stomach (pH < 3.5) inactivate SARS-CoV coronavirus (Darnell et al., 2004). Both MERS and SARS-CoV, which possibly originated from bats, crossed the species barrier and infected humans through an intermediate host which could be a domestic animal, a wild animal, or a domesticated wild animal suggesting that transmission of SARS-CoV-2 could happen in a like manner (Lu et al., 2015, WHO, 2020d) Based on that, some eating and cooking habits may be a risk factor for the reemergence of the virus into the human population (Cheng et al., 2007).
Coronavirus may reach fresh food products (e.g., vegetables, fruits, or bakery) or food packaging through an infected person who is sneezing or coughing directly on them. Transmission appears to be possible if the virus is transferred shortly afterward via the hands or the food itself to the mucous membranes of the mouth, throat, or eyes (BfR, 2020). As a study showed, physical contact and shared food during a conference resulted in a cluster of COVID-19 patients in Singapore (Pung et al., 2020). Similarly to SARS-CoV and MERS coronaviruses, studies for SARS-CoV-2 showed that the virus is highly stable at 4 °C, and it is expected to have similar behavior to its predecessors at freezing temperatures, meaning it could remain infectious at −20 °C for up to 2 years (WHO, 2020b). However, as previous studies demonstrated, coronaviruses are thermolabile: SARS-CoV can be inactivated after incubation for 15 min at >75 °C, while MERS is inactivated after incubation for 1 min at 65 °C (Darnell et al., 2004; Leclercq et al., 2014). In a like manner, SARS-CoV-2 found to be inactive after 5 minutes incubation at 70 °C (Chin et al., 2020). These outcomes suggest that normal cooking temperatures (>70 °C) are sufficient for viral inactivation, but transmission from frozen food may still be possible; this is why thorough hand washing after handling raw food is imperative. Furthermore, the likelihood is even lower for foods (packaged or not) that are shipped over days at the room, frozen, or refrigerated temperatures (BfR, 2020). Additionally, according to Centers for Disease Control and Prevention (CDC) and Environmental Protection Agency (EPA), drinking water likewise food, is not considered as a way of the spread of SARS-CoV-2 and the typical water treatment methods are sufficient against the virus (CDC, 2020b; EPA, 2020).
To minimize the risk from touching food potentially exposed to coronavirus, handling of packages and goods should be followed by hand washing or using hand sanitizer (Seymour et al., 2020). FDA has also suggested that good hygiene practices, as well as cleaning and sanitization of kitchens' and restaurants' surfaces, are preferred precaution measures compared to the environmental monitoring of SARS-CoV-2 (FDA, 2020a). Taps, door handles, refrigerator handles, and other areas of “high touch” should be subject to frequent and effective cleaning. The personnel involved in the preparation of food should be encouraged to adopt standard hygiene practices used to control known foodborne viruses and bacteria. These include handling carefully raw animal products to avoid cross-contamination with other foods, washing vegetables and fruit before eating, cooking eggs or meat thoroughly, and covering nose and mouth when sneezing or coughing, among others (Safefood, 2020). Since current evidence shows that individuals who are symptomatic comprise the most significant risk of SARS-CoV-2 transmission, food businesses should be following employee health department recommendations and policies to keep those individuals at home (Seymour et al., 2020). The usage of gloves and masks in the food industry can also be useful in reducing the spread of COVID-19, but only if appropriately used (WHO, 2020b). Takeout, drive-thru, and delivery of food are also considered good risk management practices, especially for high-risk populations (e.g., older adults) as the number of touchpoints is reduced (University of Florida, 2020). Consumers and individuals should also wash their hands thoroughly before eating, as well as after changing a child's diaper, touching animals, or using the toilet (WHO, 2020e).
Would these measures be adequate in the post-lockdown period? As of the April 21, 2020, strict rules placed on people's movements are applied to limit the spread of COVID-19. These restrictions people's freedom and disruptions to food environments give even more reason to ensure that everyone has the right to adequate food and the right to health. On the other hand, while grocers and supermarkets have become a confronting barometer of pandemic's scale, shopping of food is one of the only practices with what people knew as normal life (UNSCN, 2020). After lockdown, food service businesses as the last actor of the food supply chain will have to operate again under pressure prioritizing the health of the workers in the sector and their outcomes (FAO, 2020). At the same time, they will have to face consumers' phobia for transmission. The safety and hygienic conditions of animal-based food sources during retailing and cooking in big local markets and especially “wet markets” are challenging to be monitored by authorities. Nevertheless, laws and regulations concerning safety in food markets should be re-evaluated as poor practices such as wildlife trade, continue to be practiced in inadequately regulated sites around the world (Galanakis, 2020; Yuan et al., 2020). Taking into account the status quo of food safety within the COVID-19 pandemic and the forthcoming post-lockdown period, the need for developing accurate and fast tools for the detection of SARS-CoV-2 in food and working environment is emerging.
3. Environmental safety
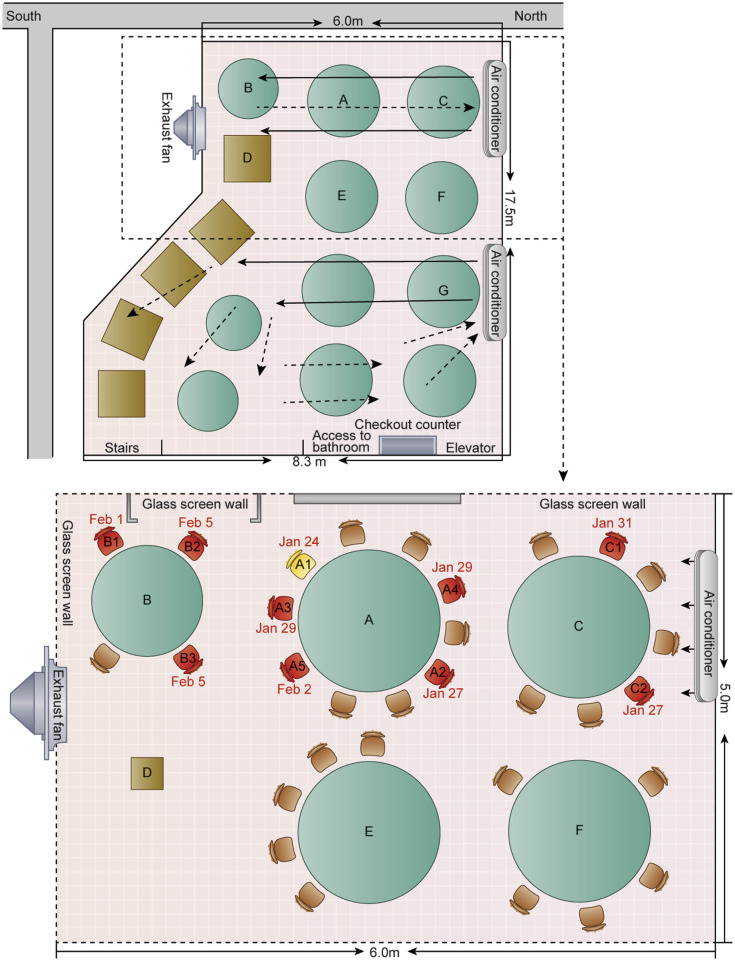
The role of the environment in the COVID-19 pandemic indicates the diverse needs of applied research that should be met to effectively control outbreaks of novel enveloped viruses (Wigginton & Boehm, 2020). Once spread in the air, virus particles are exposed to different environmental conditions (e.g., air temperature, and relative humidity) influencing their inactivation rates (Casanova, Jeon, Rutala, Weber, & Sobsey, 2010; Casanova, Rutala, Weber, & Sobsey, 2010; Kim et al., 2018). Other factors, such as the specific strain of the virus and the type of surface, play a crucial role (WHO, 2020c). However, especially for built environments, the proper disinfection of toilet areas, sanitization of surfaces, open space, and window ventilation can effectively limit the concentration of SARS-CoV-2 (Dietz et al., 2020; Liu et al., 2020). This practice is also supported by a study conducted in a restaurant inside a building without windows in China. In this study, 10 out of 83 customers became ill with COVID-19. At the same time, smear samples from the air-conditioning of the restaurant that tested with a quantitative real-time polymerase chain reaction for SARS-CoV-2 found to be negative. The airborne transmission was considered as the origin of the outbreak. However, as distances among the first documented patient (Patient A1) and other affected persons were longer than 1 m, it was underlined that the air circulation caused by the, air-conditioning might have aided the droplet transmission and the COVID-19 spread among the customers (Fig. 2 ) (Lu et al., 2020).
Fig. 2.
The arrangement of tables and air conditioning airflow at a site of COVID-19 outbreak in a restaurant placed in Guangzhou (China). Red chairs indicate seating of future case-patients, whereas the yellow chair indicates index case-patient. Remade from Lu et al. (2020). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Although not sure how long SARS-CoV-2 survives on air and surfaces, it seems possible to behave like other coronaviruses, e.g., that of SARS-CoV (van Doremalen et al., 2020). A recent review discussing the survival of human coronaviruses on surfaces noted large variability from 2 hours to 9 days (Kampf et al., 2020). Furthermore, according to a recent study conducted by van Doremalen et al. (2020), SARS-CoV-2 remains viable in aerosols for 3 hours, but still being detected on surfaces even after 72 hours. However, after a specific time, the load of the virus is importantly reduced, e.g., the viability of SARS-CoV-2 on stainless steel and plastic is ~5.6 and 6.8 hours, respectively. In contrast, no viable SARS-CoV-2 measured after 4 and 24 hours application on copper and cardboard, respectively. An effective inactivation of SARS-CoV-2 could be achieved using common disinfectants (e.g. 62–71% ethanol, 0.5% hydrogen peroxide or 0.1 sodium hypochlorite l) (Kampf et al., 2020).
The SARS-CoV-2 RNA shedding pattern suggests that the virus is replicating in the gastrointestinal tract (Woelfel et al., 2020) and thus may be found in stool samples similar to SARS-CoV (Leung et al., 2003). Besides, recent findings suggest that the SARS-CoV-2 is capable of infecting human and bat intestinal organoids (Zhou et al., 2020). Once aerosolized, sewage-contaminated with the virus could potentially expose a large number of people (NIVA, 2020). SARS-CoV-2 was recently detected in sewage samples of different cities in the Netherlands (Medema et al., 2020) in Spain (Randazzo et al., 2020) and Australia (Ahmed et al., 2020). In any case, more studies are needed to explore the survival of SARS-CoV-2 in water or sewage. The SARS-CoV-2 may be inactivated significantly faster than non-enveloped human enteric viruses (e.g., rotavirus, hepatitis A, norovirus, and adenoviruses) with a known waterborne transmission. High or low pH, sunlight, heat, and disinfectants (e.g., chlorine) facilitate die-off (WHO, 2020e).
At this moment, the most exposed environments in coronavirus are the healthcare settings. There is an increasing number of studies showing extensive environmental contamination in COVID-19 patients’ rooms (Guo et al., 2020; Ong et al., 2020; Santarpia et al., 2020; Yung et al., 2020). Given the environmental persistence of the virus (van Doremalen et al., 2020), social distancing measures and quarantine of exposed persons are considered imperative not only in hospitals but in nonhealthcare settings such as workplaces and schools. The importance of these measures has been studied regarding the influenza pandemic (Fong et al., 2020). Concerning COVID-19, a recent study demonstrated via mathematical models the transmission dynamics of SARS-CoV-2 in the post-pandemic period and suggested that prolonged or periodic social distancing may be necessary for the next few years (Kissler et al., 2020).
4. Detection of SARS-CoV-2 in food, on surfaces and the environment
As the global interest for coronavirus is focused on human health, the full impact of the pandemic on food supply chain and food industries is not yet known. However, the adverse effects on food systems and people along the food supply chain are already evident. For this reason, the development of detection tools for SARS-CoV-2 that can be applied to foods is essential to ensure food safety and prevent the disruption of food supply chains. The reliable detection of viruses in foods remains a challenge due to the heterogeneous distribution of viral particles, the low viral load, and the non-optimal tedious isolation (Bosch et al., 2018). For this purpose, different methodologies have been suggested, such as molecular detection assays based on RT-qPCR (Bosch et al., 2018), enzyme-free immunosorbent assay (Wu et al., 2016) and nano-ELISA (Wu et al., 2019).
Currently, the two predominant laboratory testing methods for SARS-CoV-2 detection are the molecular test, which is used to identify the presence of the virus and the serological tests, which detect either the antibodies against the virus or the viral antigens (Table 1 ). According to WHO, the recommended method for diagnosis of COVID-19 in patients is the detection of the virus’ RNA in respiratory tract samples by molecular testing such as quantitative real-time polymerase chain reaction (RT-qPCR) with confirmation with sequencing when necessary (WHO, 2020c). However, this method is only 66–80% sensitive and has a high rate of false-negative results. This result can be attributed to sampling errors or testing at the beginning of the disease, where the viral load is below the detection level (Kakodkar & Kaka, 2020).
Table 1.
Tests that are used for the diagnosis of SARS-CoV-2.
| SARS-CoV-2 testing method | Sample Type | Advantages | Disadvantages |
|---|---|---|---|
| RT-qPCRa | Nasopharyngeal swab | High sensitivity Robustness Can detect active infection |
False negative results Labor intensive Cannot detect past infection |
| Antibody tests | Whole blood, Serum, Plasma | Low cost Short time to diagnosis Can detect past infection |
Under validation Cannot diagnose active infection |
| Antigen tests | Whole blood, Serum, Plasma Nasopharyngeal swab |
Short time to diagnosis Can detect active infection |
Under validation Cannot detect past infection |
RT-qPCR stands for quantitative real-time polymerase chain reaction.
In addition to molecular diagnostic tests, serological tests performed in blood serum samples have been developed for SARS-CoV-2 identification through the detection of antibodies against the virus. The majority of studies suggest that the immune response to the virus initiates at least 7 days after the onset of symptoms (Chen & Li, 2020; Zhao et al., 2020). Although there are tests approved for diagnosis purposes (FDA, 2020b; JHCHS, 2020), the use of serological assays is not recommended for the diagnosis of COVID-19 by the WHO. However, it could be used for monitoring the population's immunity (WHO, 2020a).
Another type of diagnostic test for COVID-19 is the antigen test, which detects the viral proteins (ECDC, 2020a). Similarly to a polymerase chain reaction (PCR), antigen tests are usually carried out in respiratory tract samples and provide information about the presence of the virus; thus, they are appropriate for acute phase diagnosis. The efficiency of this type of test can be affected by the viral load during the infection (Udugama et al., 2020). Many rapid diagnostic tests currently developed for COVID-19 are based on antigen testing (JHCHS, 2020).
Considering the detection of SARS-CoV-2 in food, surfaces, and surrounding environments, the challenge could be even more significant. Currently, no studies have been performed, or tests have been developed for the detection of the virus in foods as there is no evidence that coronavirus is transmitted through food (EFSA, 2020). Nevertheless, as discussed above, the transmission may be possible from infected workers through surfaces and surrounding environment of the food industry and the food supply chain. Concerning the detection of SARS-CoV-2 in environmental samples, several studies have been carried out mainly in built environments. In these studies, the RT-qPCR method was used for the detection of the virus in all fomites sampled (Guo et al., 2020; Li et al., 2020; Yung et al., 2020). Although these are preliminary results, some companies have already developed commercially available kits for the detection of SARS-CoV-2 in environmental swabs (Chai, 2020; Eurofins, 2020) or offering sampling kits for surfaces (Hawk Environmental, 2020; Tentamus, 2020). However, especially the sampling kits are rather expensive, making difficult their broad application in large facilities of the food sector.
Another approach that seems to gain researchers’ interest is the wastewater-based epidemiology (WBE). In particular, monitoring of viruses has been proved efficient for early warning purposes, e.g., by detecting the presence of pathogens before the expression of symptoms in the population. The quantitative monitoring of viruses in municipal wastewater may enable the modeling of the pandemic in real-time (NIVA, 2020). As viable SARS-CoV-2 has been isolated from the faeces and urine of infected people (Holshue et al., 2020; Wang et al., 2020), it is believed that testing of the wastewater with paper-based kits can lead to the detection of potential disease carriers even if they are asymptomatic. This method can provide rapid screening of specific areas and help authorities take the appropriate measures (Mao et al., 2020). The development of detection methodologies for SARS-CoV-2 in sewage samples could be useful in the post-lockdown period.
5. Conclusion
The COVID-19 pandemic generated a new era in the food supply chain and the food industry. We still figure out the consequences of humanity, economy, and food safety (Galanakis, 2020). Researchers and professionals in the food sector have many challenges ahead, e.g., ensuring food safety, detecting SARS-CoV-2 in environments where food is produced, processed and delivered, sanitizing surfaces and working environments adequately, and others. As long as we move to the last stages of the supply chain, more measures are needed since more people are involved in the process. At this moment, the possibility of COVID-19 transmission through the food sector is considered negligible, whereas tracing of SARS-CoV-2 in the food sector and surrounding environments is not considered as a priority for public authorities. However, moving to a post-lockdown routine, public health surveillance will depend more and more on the development of relevant bioanalytical tools. This approach may not only concern screening of populations but also monitoring of foods, surfaces, and surrounding environments.
References
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O'Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. The Science of the Total Environment. 2020;728:138764. doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BfR Can the new type of coronavirus be transmitted via food and objects? - BfR. 2020. https://www.bfr.bund.de/en/can_the_new_type_of_coronavirus_be_transmitted_via_food_and_objects_-244090.html
- Bienkov A. Coronavirus: Loss of smell and taste may be hidden symptom of COVID-19 - Business Insider. 2020. https://www.businessinsider.com/coronavirus-symptoms-loss-of-smell-taste-covid-19-anosmia-hyposmia-2020-3
- Bosch A., Gkogka E., Le Guyader F.S., Loisy-Hamon F., Lee A., van Lieshout L., Marthi B., Myrmel M., Sansom A., Schultz A.C., Winkler A., Zuber S., Phister T. Foodborne viruses: Detection, risk assessment, and control options in food processing. International Journal of Food Microbiology. 2018;285:110–128. doi: 10.1016/j.ijfoodmicro.2018.06.001. Elsevier B.V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Applied and Environmental Microbiology. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L., Rutala W.A., Weber D.J., Sobsey M.D. Coronavirus survival on healthcare personal protective equipment. Infection Control and Hospital Epidemiology. 2010;31(5):560–561. doi: 10.1086/652452. [DOI] [PubMed] [Google Scholar]
- CDC How coronavirus spreads. National center for immunization and respiratory diseases (NCIRD), Division of viral diseases. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Ftransmission.html
- CDC Water transmission and COVID-19: Questions and answers. 2020. https://www.cdc.gov/coronavirus/2019-ncov/php/water.html
- Chai Coronavirus environmental test kit | Chai. 2020. https://www.chaibio.com/coronavirus-environmental-test-kit
- Cheng V.C.C., Lau S.K.P., Woo P.C.Y., Kwok Y.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clinical Microbiology Reviews. 2007;20(4):660–694. doi: 10.1128/CMR.00023-07. American Society for Microbiology (ASM) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Li L. SARS-CoV-2: Virus dynamics and host response. The Lancet Infectious Diseases. 2020 doi: 10.1016/s1473-3099(20)30235-8. 0(0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30003-3. 0(0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell M.E.R., Subbarao K., Feinstone S.M., Taylor D.R. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. Journal of Virological Methods. 2004;121(1):85–91. doi: 10.1016/j.jviromet.2004.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das U.N. Can bioactive lipids inactivate coronavirus (COVID-19)? Archives of Medical Research. 2020 doi: 10.1016/j.arcmed.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz L., Horve P.F., Coil D.A., Fretz M., Eisen J.A., Van Den Wymelenberg K. 2019 novel coronavirus (COVID-19) pandemic: Built environment considerations to reduce transmission. mSystems. 2020;5(2) doi: 10.1128/mSystems.00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30120-1. (Vol. 0, Issue 0). Lancet Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. 2020 doi: 10.1056/nejmc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC An overview of the rapid test situation for COVID-19 diagnosis in the EU/EEA. 2020. https://www.ecdc.europa.eu/en/publications-data/overview-rapid-test-situation-covid-19-diagnosis-eueea
- ECDC Q & A on COVID-19. 2020. https://www.ecdc.europa.eu/en/covid-19/questions-answers
- EFSA Coronavirus: No evidence that food is a source or transmission route. 2020. https://www.efsa.europa.eu/en/news/coronavirus-no-evidence-food-source-or-transmission-route
- EPA Coronavirus and drinking water and wastewater | coronavirus (COVID-19) | US EPA. 2020. https://www.epa.gov/coronavirus/coronavirus-and-drinking-water-and-wastewater
- Euractiv No evidence of COVID-19 transmission through food, says EFSA. 2020. https://www.euractiv.com/section/coronavirus/news/no-evidence-of-covid-19-transmission-through-food-says-efsa/
- Eurofins Detection of SARS-CoV-2 in swabs of environmental surfaces. 2020. https://www.eurofins-technologies.com/products/viruses.html
- FAO COVID-19 and the risk to food supply chains: How to respond? |Policy support and Governance| food and Agriculture Organization of the United Nations. 2020. http://www.fao.org/policy-support/resources/resources-details/en/c/1269383/
- FDA Best practices for retail food stores, restaurants, and food pick-up/delivery services during the COVID-19 pandemic | FDA. 2020. https://www.fda.gov/food/food-safety-during-emergencies/best-practices-retail-food-stores-restaurants-and-food-pick-updelivery-services-during-covid-19
- FDA Coronavirus (COVID-19) update: Serological tests | FDA. 2020. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-serological-tests
- FDA Food safety and the coronavirus disease 2019 (COVID-19) | FDA. 2020. https://www.fda.gov/food/food-safety-during-emergencies/food-safety-and-coronavirus-disease-2019-covid-19
- Fong M.W., Gao H., Wong J.Y., Xiao J., Shiu E.Y.C., Ryu S., Cowling B.J. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerging Infectious Diseases. 2020;26(5) doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanakis C.M. The food systems in the era of the coronavirus (CoVID-19) pandemic crisis. Foods. 2020;9(4) doi: 10.3390/foods9040523. MDPI Multidisciplinary Digital Publishing Institute. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z.-D., Wang Z.-Y., Zhang S.-F., Li X., Li L., Li C., Cui Y., Fu R.-B., Dong Y.-Z., Chi X.-Y., Zhang M.-Y., Liu K., Cao C., Liu B., Zhang K., Gao Y.-W., Lu B., Chen W. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerging Infectious Diseases. 2020;26(7) doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk Environmental Surrogate bacterial surface test kit for coronavirus (COVID-19) | Hawk environmental services. 2020. https://hawkenvironmental.com/surrogate-covid-19-test-kit/
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L., Patel A., Gerber S.I., Kim L., Tong S., Lu X., Lindstrom S.…Pillai S.K. First case of 2019 novel coronavirus in the United States. New England Journal of Medicine. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalava K. First respiratory transmitted food borne outbreak? International Journal of Hygiene and Environmental Health. 2020;226:113490. doi: 10.1016/j.ijheh.2020.113490. Elsevier GmbH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JHCHS . 2020. Serology-based tests for COVID-19.https://www.centerforhealthsecurity.org/resources/COVID-19/ [Google Scholar]
- Kakodkar P., Kaka N. A comprehensive literature review on the clinical presentation , and management of the pandemic coronavirus disease 2019 history of the outbreak. Cureus. 2020;12(4) doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. W.B. Saunders Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan J., Frias L., McFall-Johnsen M. 2020. 2020. Countries that are on lockdown because of coronavirus - Business Insider.https://www.businessinsider.com/countries-on-lockdown-coronavirus-italy-2020-3 [Google Scholar]
- Kim Y., Krishna V.D., Torremorell M., Goyal S.M., Cheeran M.C.J. Stability of porcine epidemic diarrhea virus on fomite materials at different temperatures. Veterinary Sciences. 2018;5(1) doi: 10.3390/vetsci5010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020 doi: 10.1126/science.abb5793. eabb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclercq I., Batéjat C., Burguière A.M., Manuguerra J.C. Heat inactivation of the Middle East respiratory syndrome coronavirus. Influenza and Other Respiratory Viruses. 2014;8(5):585–586. doi: 10.1111/irv.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung W.K., To K., Chan P.K.S., Chan H.L.Y., Wu A.K.L., Lee N., Yuen K.Y., Sung J.J.Y. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125(4):1011–1017. doi: 10.1016/s0016-5085(03)01215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. New England Journal of Medicine. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., Sun L., Duan Y., Cai J., Westerdahl D., Liu X., Xu K., Ho K.F., Kan H., Fu Q., Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;1–4 doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., Zhou D., Yu C., Xu B., Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerging Infectious Diseases. 2020;26(7) doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu G., Wang Q., Gao G.F. Bat-to-human: Spike features determining “host jump” of coronaviruses SARS-CoV, MERS-CoV, and beyond. Trends in Microbiology. 2015;23(8):468–478. doi: 10.1016/j.tim.2015.06.003. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie J.S., Smith D.W. COVID-19: A novel zoonotic disease caused by a coronavirus from China: What we know and what we don't. Microbiology Australia. 2020;41(1):45. doi: 10.1071/ma20013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao K., Zhang H., Yang Z. Can a paper-based device trace COVID-19 sources with wastewater-based epidemiology? Environmental Science & Technology. 2020 doi: 10.1021/acs.est.0c01174. [DOI] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-Coronavirus-2 in sewage. MedRxiv. 2020 doi: 10.1101/2020.03.29.20045880. 2020.03.29.20045880. [DOI] [PubMed] [Google Scholar]
- NIVA . Can the sewers disclose the scale of COVID-19? - NIVA. 2020. https://www.niva.no/en/news/can-the-sewers-disclose-the-scale-of-covid-19 [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA - Journal of the American Medical Association. 2020 doi: 10.1001/jama.2020.3227. American Medical Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.C., Clapham H.E., Cook A.R., Maurer-Stroh S., Toh M.P.H.S., Poh C., Low M., Lum J., Koh V.T.J., Mak T.M., Cui L., Lin R.V.T.P., Heng D., Leo Y.S., Lye D.C.…Ang L.W. Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. The Lancet. 2020;395(10229):1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randazzo W., Truchado P., Cuevas-Ferrando E., Simón P., Allende A., Sánchez G. SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Research. 2020 doi: 10.1016/j.watres.2020.115942. 115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiley L. Meat processing plants are closing due to covid-19 outbreaks. Beef shortfalls may follow. 2020. https://www.washingtonpost.com/business/2020/04/16/meat-processing-plants-are-closing-due-covid-19-outbreaks-beef-shortfalls-may-follow/
- Rodriguez-Morales A.J., Bonilla-Aldana D.K., Balbin-Ramon G.J., Rabaan A.A., Sah R., Paniz-Mondolfi A., Pagliano P., Esposito S. History is repeating itself: Probable zoonotic spillover as the cause of the 2019 novel Coronavirus Epidemic. Infezioni in Medicina, Le. 2020;28(1):3–5. http://www.ncbi.nlm.nih.gov/pubmed/32009128 [PubMed] [Google Scholar]
- Safefood . 2020. COVID-19 advice - safe food.https://www.safefood.qld.gov.au/covid-19-advice/ [Google Scholar]
- Santarpia J.L., Rivera D.N., Herrera V., Morwitzer M.J., Creager H., Santarpia G.W., Crown K.K., Brett-Major D., Schnaubelt E., Broadhurst M.J., Lawler J.V., Reid S.P., Lowe J.J. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska medical center. MedRxiv. 2020 doi: 10.1101/2020.03.23.20039446. 2020.03.23.20039446. [DOI] [Google Scholar]
- Seymour N., Yavelak M., Christian C., Chapman B. COVID-19 and food safety FAQ: Is coronavirus a concern with takeout? 2020. https://edis.ifas.ufl.edu/fs349
- Tentamus New sampling-kit to test your surfaces for coronavirus! | Tentamus. 2020. https://www.tentamus.com/new-test-kit-surfaces-coronavirus/?cn-reloaded=1&cn-reloaded=1
- Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y.C., Chen H., Mubareka S., Gubbay J., Chan W.C.W. Diagnosing COVID-19: The disease and tools for detection. ACS Nano. 2020 doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- University of Florida COVID-19 and food safety FAQ: Is coronavirus a concern with takeout? | EDIS. 2020. https://journals.flvc.org/edis/article/view/121236
- UNSCN Food environments in the COVID-19 pandemic. 2020. https://www.unscn.org/en/news-events/recent-news?idnews=2040
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. JAMA - Journal of the American medical association. American Medical Association; 2020. Detection of SARS-CoV-2 in different types of clinical specimens. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Advice on the use of point-of-care immunodiagnostic tests for COVID-19 Rapid diagnostic tests based on antigen detection. 2020. [DOI]
- WHO COVID-19 and food safety: Guidance for food businesses. 2020. https://www.who.int/publications-detail/covid-19-and-food-safety-guidance-for-food-businesses
- WHO Laboratory testing for coronavirus disease (COVID-19) in suspected human cases. 2020. https://apps.who.int/iris/bitstream/handle/10665/331501/WHO-COVID-19-laboratory-2020.5-eng.pdf?sequence=1&isAllowed=y
- WHO Virus origin/Reducing animal-human transmission of emerging pathogens. 2020. https://www.who.int/health-topics/coronavirus/who-recommendations-to-reduce-risk-of-transmission-of-emerging-pathogens-from-animals-to-humans-in-live-animal-markets
- WHO Water, sanitation, hygiene and waste management for COVID-19. 2020. https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-covid-19
- WHO WHO Director-General’s opening remarks at the media briefing on COVID-19 - 15 April 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---15-april-2020
- Wigginton K.R., Boehm A.B. Environmental engineers and scientists have important roles to play in stemming outbreaks and pandemics caused by enveloped viruses. Environmental Science and Technology. 2020 doi: 10.1021/acs.est.0c01476. American Chemical Society. [DOI] [PubMed] [Google Scholar]
- Woelfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Mueller M.A., Niemeyer D., Vollmar P., Rothe C., Hoelscher M., Bleicker T., Bruenink S., Schneider J., Ehmann R., Zwirglmaier K., Drosten C., Wendtner C. Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster. MedRxiv. 2020 doi: 10.1101/2020.03.05.20030502. 2020.03.05.20030502. [DOI] [Google Scholar]
- Wu L., Li G., Xu X., Zhu L., Huang R., Chen X. Application of nano-ELISA in food analysis: Recent advances and challenges. TrAC - Trends in Analytical Chemistry. 2019;113:140–156. doi: 10.1016/j.trac.2019.02.002. Elsevier B.V. [DOI] [Google Scholar]
- Wu L., Yin W., Tang K., Shao K., Li Q., Wang P., Zuo Y., Lei X., Lu Z., Han H. Highly sensitive enzyme-free immunosorbent assay for porcine circovirus type 2 antibody using Au-Pt/SiO2 nanocomposites as labels. Biosensors and Bioelectronics. 2016;82:177–184. doi: 10.1016/j.bios.2016.04.001. [DOI] [PubMed] [Google Scholar]
- Yuan J., Lu Y., Cao X., Cui H. Regulating wildlife conservation and food safety to prevent human exposure to novel virus. Ecosystem Health and Sustainability. 2020;6(1) doi: 10.1080/20964129.2020.1741325. [DOI] [Google Scholar]
- Yung C.F., Kam K.-Q., Wong M.S.Y., Maiwald M., Tan Y.K., Tan B.H., Thoon K.C. Environment and personal protective equipment tests for SARS-CoV-2 in the isolation room of an infant with infection. Annals of Internal Medicine. 2020 doi: 10.7326/M20-0942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Yuan Q., Wang H., Liu W., Liao X., Su Y., Wang X., Yuan J., Li T., Li J., Qian S., Hong C., Wang F., Liu Y., Wang Z., He Q., Li Z., He B., Zhang T.…Zhang Z. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clinical Infectious Diseases. 2020. [DOI] [PMC free article] [PubMed]
- Zhou P., Yang X., Lou, Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R., Di, Liu M.Q., Chen Y.……Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]