Abstract
Introduction:
Delirium is well studied in the acute care setting, but there is limited understanding of its impact in the post-acute care setting, particularly in the inpatient rehabilitation facility (IRF).
Objective:
To investigate the prevalence and related outcomes of delirium in the IRF setting, particularly patients’ transfers to acute care hospitals.
Design:
Retrospective cohort study
Setting:
A freestanding IRF
Participants:
Patients discharged from an IRF between January 2016 and December 2016 (12 months)
Interventions:
Not applicable
Main Outcome Measures:
Transfer to acute care hospitals, motor and cognitive Functional Independence Measures (FIM), length of stay, discharge disposition
Results:
A total of 1,567 patients (53.86% female, mean age 72.86 +/− 13.9) were included in the analysis. Positive scores were found among 142 (9.1%) patients on a 3-Minute Diagnostic Interview for Confusion Assessment Method (3D-CAM), indicating delirium on admission. Fifty-nine (3.8%) were un-scorable on 3D-CAM. Twice as many delirium patients were transferred to acute care hospitals compared to non-delirium patients (22.5% versus 10.8%, P<.001). Multi-variate logistic regression showed that, for patients with 3D-CAM positive scores, there was an increased risk of transfers to acute care hospitals at an odds ratio of 1.61 (1.03–2.53, P=.04) after adjusting for age, gender, neurological diagnosis, and motor FIM score. The delirium group also showed lower gains in motor function, increased lengths of stay, and reduced discharges to home when compared to the non-delirium group (P<.001).
Conclusions:
This study finds that delirium on admission to an IRF is associated with worsened outcomes related to function, length of stay, discharge status and transfer to acute care hospitals. Positive delirium screening is an independent predictor for transfer to acute care hospitals from an IRF. Early identification of delirium is recommended in order to mitigate preventable transfers.
Keywords: Delirium, Acute Care Transfer, Rehabilitation
INTRODUCTION
Delirium is an acute dysfunctional cognitive state characterized by inattention and a disturbance in awareness which fluctuates over a relatively short period of time. It is one of the most commonly acquired conditions among hospitalized older adults, with a prevalence as high as 80% in acute care hospitals and estimations of 10–40% in post-acute care settings [1–3]. Most significantly, up to 40% of these cases could have been prevented or even reversed in the acute care setting [4,5]. Clearly, early detection and intervention is needed for optimal care. Patients in Inpatient Rehabilitation Facilities (IRFs) may have multiple risk factors for delirium including: older age with multiple co-morbidities such as cognitive impairment, depression, and visual/hearing impairments [6]. Of the patients in IRFs, 62% are age 65 or older and a quarter of the patients are over age 85 [7,8]. Thus, many of the patients in IRFs are at risk for delirium. However, this clinical diagnosis is largely under-recognized by physicians and other disciplines in this setting. This is unfortunate because delirium potentially reflects underlying medical illnesses even before other clinical or laboratory signs for illness are evident and serves as a predictive role in patient outcomes, including transfers to the acute care hospitals. One study in a skilled nursing facility found that ‘altered mental status’ was the second most common reason for transfers to acute care hospitals [9]. These un-planned interruptions in patient care contribute to negative outcomes related to rehabilitative care and cause tremendous distress to patients and their families. The Centers for Medicare & Medicaid Services (CMS) recently implemented the National Quality Forum (NQF)-endorsed measures to report hospital readmission rates in 2016 [10]. Although the transfer to acute care hospitals is recognized as a health care quality indicator, there is still a limited understanding of the factors that influence patients being transferred back to acute care settings from IRFs. This gap in practice provides clinicians an opportunity to improve care at IRFs by systematically screening for delirium.
There are several non-modifiable factors, identified as possible predictors for transfers to acute care hospitals, including geographical location, financial structuring of the organization (i.e. whether the organization is for-profit or non-profit), and specific diagnoses such as brain injury [11,12]. Considering that delirium, a potentially modifiable condition, is often an early sign of medical illnesses and that altered mental status is one of the leading causes of transfers to acute care hospitals, it is plausible that the systematic screening of delirium at admission will help clinicians to recognize high-risk patients. Therefore, the primary objective of this study is to investigate whether the systematic screening of delirium at admission will independently predict transfers to acute care hospitals at IRFs. Screening for delirium on admission can result in three distinct groups: those positive for delirium, those negative for delirium and those unscorable due to unforeseen circumstances. The secondary objective is to characterize and compare demographics, diagnoses, and clinical and administrative outcomes between patients with delirium compared to the non-delirium, as well as patients with unscorable results compared to the non-delirium group. Positive delirium screening at admission to an IRF was hypothesized to independently predict transfer of patients to the acute care hospital. Patient outcomes were hypothesized to show increased lengths of stay, fewer discharges to home and decreased FIM scores on discharge in the delirium group compared to the non-delirium group, as well as the unscorable group compared to the non-delirium group.
METHODS
Study participants and setting
All patients who were discharged from the IRF from January 1st to December 31st, 2016, were included in the study. The first-time admission of a patient was included if that patient had multiple admissions; subsequent admissions for the same individual were excluded. The demographic, clinical, and administrative outcomes data for this study were extracted from eRehabData®, an inpatient rehabilitation outcomes system monitored by the American Medical Rehabilitation Providers Association that is available to inpatient rehabilitation providers for purposes of research and development. The details of this data are described in a later section.
Assessment of delirium
The 3-Minute Diagnostic Assessment for Delirium using the Confusion Assessment Method (3D-CAM) has been used as the screening tool for delirium at our IRF since January 2015. The algorithm includes 20 mandatory and two optional items, with a sensitivity of 95%, a specificity of 94%, and an interrater reliability of 95% [13]. This measurement tool consists of four categories for identifying delirium: (1) acute change and fluctuating course, (2) inattention, (3) disorganized thinking, and (4) altered level of consciousness. An analysis of each category occurs in a flow diagram type decision making where the results are typically binary – that is, patients were usually either positive or not positive for delirium. Of note, there were patients who were unable to be scored when the family was not present to determine whether the current condition was at the patient’s baseline or a change in the patient’s clinical state and the patient wasn’t able to communicate.
Implementation of the delirium screening is described in detail in a previous publication [14]. In brief, a Delirium Taskforce consisting of a geriatric physiatrist, clinician researcher, Chief Quality Officer, research occupational therapist, and nurse manager built a protocol using 3D- CAM. Members of the taskforce held educational sessions with clinicians and admission nurses. After the training, the taskforce randomly audited 424 cases and found that 99% of cases were in compliance with screening for delirium using 3D-CAM on admission. The results of 3D-CAM were recorded as positive, negative, or unscorable. Nurses were instructed to record the reasons for unscorable results.
Study design and sample size
A power analysis was done based on transfer proportions of delirium and non-delirium patients from small previously published studies. Marcantonio et al. showed 30% of the delirium patients readmitted to the acute care hospital compared to 13% of the non-delirium patients, whereas Guerini et al. showed 18.3% transfers for those with delirium [5,15]. Based on these studies, transfer to acute care hospitals was estimated to be 18% in the delirium group and 13% in the non-delirium group. This led to an estimation of 1,474 patients to provide the study with a power of 80% to detect a 5% difference in transfer proportions between the delirium and non-delirium group at an overall two-sided alpha level of 0.05. Due to the retrospective nature of the study, twelve months was chosen as the length of time to follow the cohort based on the expected number of admissions to the facility, with the final sample size of 1,567 patients more than adequately meeting the results of the power analysis. This is the data being used to retrospectively analyze the cohort of patients who were screened for delirium for the purpose of this study.
Primary outcome variable
The primary outcome variable is the transfer of patients back to the acute care hospitals. The status of transfer to acute care hospitals was determined by the final destination recorded in eRehabData® for each patient. The designation of transfer to acute care hospitals includes patients who were discharged from the IRF and returned to the same IRF within three consecutive calendar days as defined by the Center for Medicaid/Medicare Services (CMS) and termed, “interrupted stays”. These patients were included because their temporary absences from rehabilitative care reflected a loss of care similar to transfers which resulted in a longer stay at acute care hospitals. FIM scores on discharge were also recorded as measured by therapists and stored in the eRehabData® database.
Demographics and co-variates
Demographics, FIM scores at admission, length of stay, co-morbidities, Body Max Index (BMI), and admission diagnoses were obtained from eRehabData®.
Statistical analyses
All statistical analyses were performed using the statistical package Stata SE Version 14.0 (StataCorp, College Station, TX, USA). Characteristics of patients on admission were compared and the statistics reported accordingly, with the delirium group and unscorable groups compared separately to the non-delirium group. The Wilcoxon sum-rank test was used for non-parametric data, and proportions were compared with chi-square tests. Multi-variate logistic regression was used to evaluate whether a positive or unscorable result in 3D-CAM is an independent predictor for transfer to acute care hospitals, with adjustment of covariates identified by univariate analysis with clinical or statistical significance of P<.05. The covariates included age, gender, neurological diagnosis, and motor FIM scores. Due to the co-linearity between delirium and cognitive FIM scores, the cognitive FIM scores were not included in the multivariate analysis. The delirium group and the unscorable group were separated in the multivariate logistic regression using a dummy variable in order to determine an odds ratio for each group.
Bias
This study is prone to selection bias and misclassification bias due to the nature of a retrospective cohort study. However, the records collected during the delirium screening training were thoroughly monitored via periodic audits for validity.
This study was approved by the Institutional Review Board.
RESULTS
The prevalence of delirium and the characteristics of the study population
There were 1,567 patient discharges included in the analysis after excluding subsequent multiple admissions for the same individuals (n=159). The prevalence of delirium (as defined by a positive 3D-CAM score) at admission was 9.1% (n=142 out 1567) (Table 1). The proportion of unscorable results was 3.8% (n=59 out of 1567). As noted by nursing staff, the most common reason patients were unscorable was because of “aphasia” (n=31). The second most common reason was “severe disorders of consciousness” (n=13). This is followed by four patients each who were noted to be “deaf/hard of hearing”, “refused”, “tracheostomy present.” Lastly, one patient each was noted with “dysarthria”, “language barrier” and “baseline dementia.”
Table 1.
Characteristics of study population (total n=1567)
| Characteristics | Delirium (n=142, 9.1%) | Delirium v. Non-Delirium | Non-Delirium (n=1366, 87.2%) | Non-Delirium v. Unscorable | Unscorable (n=59, 3.8%) |
|---|---|---|---|---|---|
| Age at admission (years)† | 74.8±13.3 | .11 | 72.9±13.8 | .01 | 67.7±16.5 |
| Female (%)‡ | 70 (49.3) | .19 | 751 (55.0) | .02 | 23 (39.0) |
| Body Mass Index (BMI) (kg/m2)† | 28.8±7.0 | .29 | 28.3±7.5 | .23 | 27.1±5.9 |
| Primary Diagnosis Type(%)‡ | |||||
| Neurologic Injury | 71 (50.0) | <.001 | 348 (25.5) | <.001 | 53 (89.8) |
| Non-Neurologic Injury | 71 (50.0) | 1018 (74.5) | 6 (10.2) | ||
| Comorbidities(%)‡ | |||||
| Cardiac Disease | 106 (74.7) | .96 | 1017 (74.5) | .75 | 45 (76.2) |
| Depression | 18 (12.7) | .67 | 191 (14.0) | .23 | 5 (8.5) |
| Dementia | 10 (7.0) | .61 | 113 (8.3) | .06 | 9 (15.3) |
| Diabetes Mellitus | 36 (25.4) | .21 | 284 (20.1) | .93 | 12 (20.3) |
| Cancer | 15 (10.6) | .62 | 127 (9.3) | .05 | 10 (17.0) |
| Lung Disease | 24 (17.0) | .08 | 318 (23.3) | .41 | 11 (18.6) |
| DVT/PE | 10 (7.0) | .20 | 63 (4.6) | .66 | 2 (3.4) |
| Alcoholism | 15 (10.6) | .78 | 155 (11.4) | .60 | 8 (13.6) |
| Renal Disease | 29 (20.4) | .80 | 267 (19.6) | .27 | 15 (25.4) |
| Admission motor FIM score† | 24.3±9.6 | <.001 | 31.3±9.1 | <.001 | 17.4±9.1 |
| Admission cognition FIM score† | 15.2±5.8 | <.001 | 24.2±6.0 | <.001 | 10.2±5.9 |
Wilcoxon rank-sum test was used for comparison of values of age at admission, body mass index (BMI) and admission FIM scores which are described as mean±standard deviation (SD).
Chi-square test was used for comparison of proportions among the groups.
The demographic data is described in Table 1. The mean age of the delirium group was 74.8 years compared to 72.9 years in the non-delirium group without statistical significance (P=.11). There is, however, statistical significance (P=.01) when the mean age of the unscorable group (67.7 years) is compared to the mean age of the non-delirium group (72.9 years). A higher proportion of men were in the delirium group than the non-delirium group (50.7 %, 45.0%, P=.19) with a statistically significant higher proportion of men in the unscorable group compared to the non-delirium group (61.0%, 45.0%, P=.02). There was no difference when comparing the body mass index (BMI) of those with delirium to those without delirium (28.8, 28.3, P=.29) or when comparing the BMI of the unscorable group to the non-delirium group (27.1, 28.3, P=.23). There were more patients with neurologic conditions in the delirium group compared to those without delirium (P<.001); the highest percentage of neurologic conditions was in the unscorable group (89.8%), which is statistically significant (P<.001) compared to the non-delirium group. Of all the co-morbidities studied, the near-statistically significant results include a higher proportion of dementia in the unscorable group compared to the non-delirium group (15.3%, 8.3%, P=.06) and higher proportion of cancer in the unscorable group compared to the non-delirium group (17.0%, 9.3%, P=.05). The admission FIM scores were significantly lower in the delirium group compared to the non-delirium group (motor: 24.3, 31.3, P=.01, cognition: 15.2, 24.2, P=.01). The unscorable population had even lower admission motor and cognitive FIM scores compared to both the delirium and the non-delirium groups.
Transfers to acute care hospitals in delirium versus non-delirium group
The proportion of transfers to acute care hospitals was highest among the delirium group (22.5%, P<.001) followed by the unscorable group (22.4%, P=.01) compared to the non-delirium group (10.8%) (Table 2).
Table 2.
Outcomes of patients by delirium screening results using 3D-CAM
| Outcomes | Delirium (n=142, 9.1%) | Delirium v. Non-Delirium | Non-Delirium (n=1366, 87.2%) | Non-Delirium v. Unscorable | Unscorable (n=59, 3.8%) |
|---|---|---|---|---|---|
| Acute Care Transfer (%)† | 32 (22.5) | <.001 | 147 (10.8) | .01 | 13 (22.4) |
| Discharge motor FIM score ‡ | 41.8±18.4 | <.001 | 57.6±14.4 | <.001 | 34.5±19.3 |
| Discharge cognition FIM score‡ | 18.5± 6.5 | <.001 | 27.2±5.9 | <.001 | 14.3±7.1 |
| Gain in motor FIM score‡ | 20.5±13.1 | <.001 | 26.3±10.5 | <.001 | 17.1±15.3 |
| Gain in cognition FIM score‡ | 3.3±5.1 | <.001 | 3.0±4.2 | <.001 | 4.1±5.6 |
| Change in FIM score per day‡ | 1.7±1.2 | <.001 | 2.5±1.6 | <.001 | 1.3×1.6 |
| Length of Stay (days) | 15.1±7.1 | <.001 | 13.3±13.0 | <.001 | 23.1±12.7 |
| Discharge to home (%) | 72 (50.6) | <.001 | 978 (71.7) | <.001 | 21 (36.1) |
Chi-square test was used for comparison of proportions between the groups.
Wilcoxon rank sum test was used comparison of FIM scores and length of stay with mean±SD (median) values described.
Multivariate logistic regression analysis showed that the odds of transfers to acute care hospitals are 1.6 times greater in the positive delirium group than in the non-delirium group after adjusting for age, gender, neurological diagnosis, and motor FIM scores at admission [odds ratio (OR) 1.61 confidence interval (CI), 1.03–2.53, P=.04] (table 3). The unscorable group was analyzed separately using a dummy variable. The odds ratio of transfers to acute care hospitals for the unscorable group was 1.17 relative to the non-delirium group without reaching statistical significance [OR 1.17 CI, 0.58–2.31, P=.66](table 3).
Table 3.
Factors associated with acute care transfers between delirium and non-delirium group
| Variables | Odds Ratio (95% Confidence Interval) |
P value |
|---|---|---|
| Delirium v. Non-Delirium | 1.61 (1.03–2.53) | .04 |
| Unscorable v. Non-Delirium | 1.17 (0.58–2.31) | .66 |
| Neurological diagnosis | 1.00 (0.98–1.03) | .85 |
| Age at admission | 0.99 (0.98–1.01) | .39 |
| Female gender | 1.01 (0.73–1.39) | .96 |
| Motor FIM scores at admission | 0.56 (0.48–0.66) | <.001 |
Functional and administrative outcomes
The functional and administrative outcomes are summarized in Table 2. Delirium and unscorable groups consistently showed significantly lower motor and cognitive FIM scores at discharge compared to the non-delirium group. In addition, the gain in motor FIM (20.5, 26.3, P<.001) and change in FIM score per day (1.7, 2.5, P<.001) was lower in the delirium group compared to the non-delirium group. There was, however, a trend toward higher gain in cognition FIM scores in the delirium group compared to the non-delirium group with statistical significance (3.3, 3.0, P<.001), as well as higher gain in cognition FIM scores in the unscorable group compared to the non-delirium group (4.1, 3.0, P<.001).
The length of stay was the longest among the unscorable group (23.1 days, P<.001) followed by the delirium group (15.1 days, P<.001) compared to the non-delirium group (13.3 days). The home discharges showed a similar pattern: the lowest home discharges were in the unscorable group (36.1%, P<.001), followed by the delirium group (50.6%, P<.001) compared to the non-delirium group (71.7%).
DISCUSSION
The results of this study showed that positive delirium screening at admission independently predicts transfers of patients to acute care hospitals from an IRF, even after taking into account their initial functional status. These patients with delirium at admission also demonstrated lower functional gains and decreased likelihood of discharges to the community after rehabilitation in spite of longer lengths of stay at the IRF compared to those without delirium. Those with unscorable results on delirium screening at admission showed a similar trend similar to those with positive delirium; however, being screened unscorable at admission was not a statistically significant independent predictor for transfers to acute hospitals.
The diagnostic criteria of delirium defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) are as follows: 1) a disturbance in attention and awareness; 2) symptoms of disturbance occurring over a short period of time (hours to days) with fluctuation during this time; 3) disturbances in cognition; 4) disturbances in cognition that cannot be explained by preexisting, established or evolving neurocognitive disorders; 5) evidence of direct physiologic causes of the disturbance (general medical condition, intoxicating substances, medications or their side effects) [16]. Using these criteria to diagnose delirium may require the services of behavioral health clinicians who may not be readily available. However, this study supports the use of a screening test for delirium, 3D-CAM, which has been validated and found reliable and can be performed easily at the rehabilitation setting by trained medical personnel.
Additionally, there are three different types of delirium: hypoactive, hyperactive and mixed types. Hypoactive delirium is characterized by decreased activity, speech and awareness; it is an elusive condition that is diagnosed late in its course, has poorer outcomes than other types, and is often underdiagnosed [17]. Underlying dementia, older age, and impaired sensorium (e.g. hearing) are also identified as risk factors for under-recognition of delirium. A high index of suspicion and the use of reliable and validated diagnostic tools are essential for the early detection of delirium.
Delirium: prevalence
Currently, there is considerable medical literature regarding the presence of delirium and related negative health care outcomes in various health care settings. The prevalence of delirium has been highest in the intensive care units (ICUs) and postoperative acute care settings with reported proportions up to 80% in the critically ill [1]. Similarly, delirium is one of the most common hospital acquired complications in the geriatric population with prevalence rates ranging between 14% – 67%[18]. It is probable the true rate of delirium is higher than the observed rates due to frequent non-detection. Delirium has been associated with high rates of morbidity, mortality and eventual institutionalization [19–21].
Despite the abundance of related research as mentioned above, research regarding the prevalence and outcomes of delirium specifically in the rehabilitation population is relatively limited. Published data of prevalence in the post-acute care setting varies widely due to the different settings (skilled nursing facility, long term care unit, acute rehabilitation units, community) and the variability in the diagnostic tools used, resulting in prevalence of delirium ranging from below 1% to 89% [5,22–24]. More recent data from the acute rehabilitation care setting shows a prevalence of about 10–16.3% [2,3]. The prevalence also depends on the diagnosis prior to admission to rehabilitation, including 33% in stroke patients and 32–39% in those admitted after hip fractures [2,25]. Overall, despite this variability, all of the studies report poor morbidity, mortality, and length of stay outcomes in similar proportions.
The prevalence in this study of those positive for delirium (9.1%) reflects the data found in other long term care facilities [2,3]. While there are certain similarities between the populations of IRFs, nursing homes and other skilled nursing facilities, the intensive therapy schedules and the interdisciplinary team approach in IRFs make for a unique setting to study the presence and effects of delirium.
Delirium: a predictor of transfers to the acute care hospital
Several studies on transfers of patients to the acute care hospital from rehabilitation facilities demonstrate that these interruptions are detrimental to clinical progress. These studies showed that transfers to acute care hospitals were highest among patients with brain injuries (22 %), followed by cancer (17.3%), burns (12.8%), and spinal cord injuries (11.2%) [11,26–28]. While prior studies have identified risk factors such as geography and organizational structures, these remain nonmodifiable risk factors, limiting our ability to intervene. This study finds that the presence of delirium is predictive of transfers to acute care hospitals. Patients with positive 3D-CAM results are 1.6 times more likely to be transferred back to the acute care hospital after adjusting for demographic, motor function, and the presence of neurological diagnoses. Delirium is a potentially modifiable and remediable factor, which may reduce preventable transfers to acute care hospitals. These findings support the importance of delirium assessment and management within the setting of inpatient rehabilitation facilities, and suggest that implementation of such practices could potentially improve patient care and related outcomes.
Delirium: demographics
Compared to the non-delirium group, patients with delirium are older (74.8 years), slightly more often male (50.7%), and with lower functional status in both motor and cognitive realms at admission (FIM motor 24.3, FIM cognitive 15.2) (table 1). This is consistent with earlier study findings of risk factors for delirium consisting of age >65 years, male gender, functional impairment at admissions in populations outside the inpatient rehabilitation facility setting [29]. These risk factors, though non-modifiable, are characteristics of the majority of patients admitted to rehabilitation facilities, which puts most of these patients at risk for delirium. Additionally, while prior studies have found that patients with delirium have increased rates of respiratory illness, renal illness and substance disorders, this study’s population did not have statistically significant differences in comorbidities or BMI when comparing the delirium and non-delirium groups [2,5,30].
Of note, patients scoring positively for delirium were exactly proportional to the primary diagnosis type of neurologic injury and non-neurologic injuries (50%) (Table 1). Figure 1 further demonstrates the various diagnoses within the delirium population including non-neurologic diagnoses such as orthopedic, cardiac, pulmonary, and multi-trauma. This indicates that delirium, a temporary cognitive dysfunctional state, is equally present in patients admitted for non-neurologic diagnoses. Because of this, all medical personnel working in the inpatient rehabilitation facility setting must be vigilant and trained in assessing for delirium.
Figure 1.
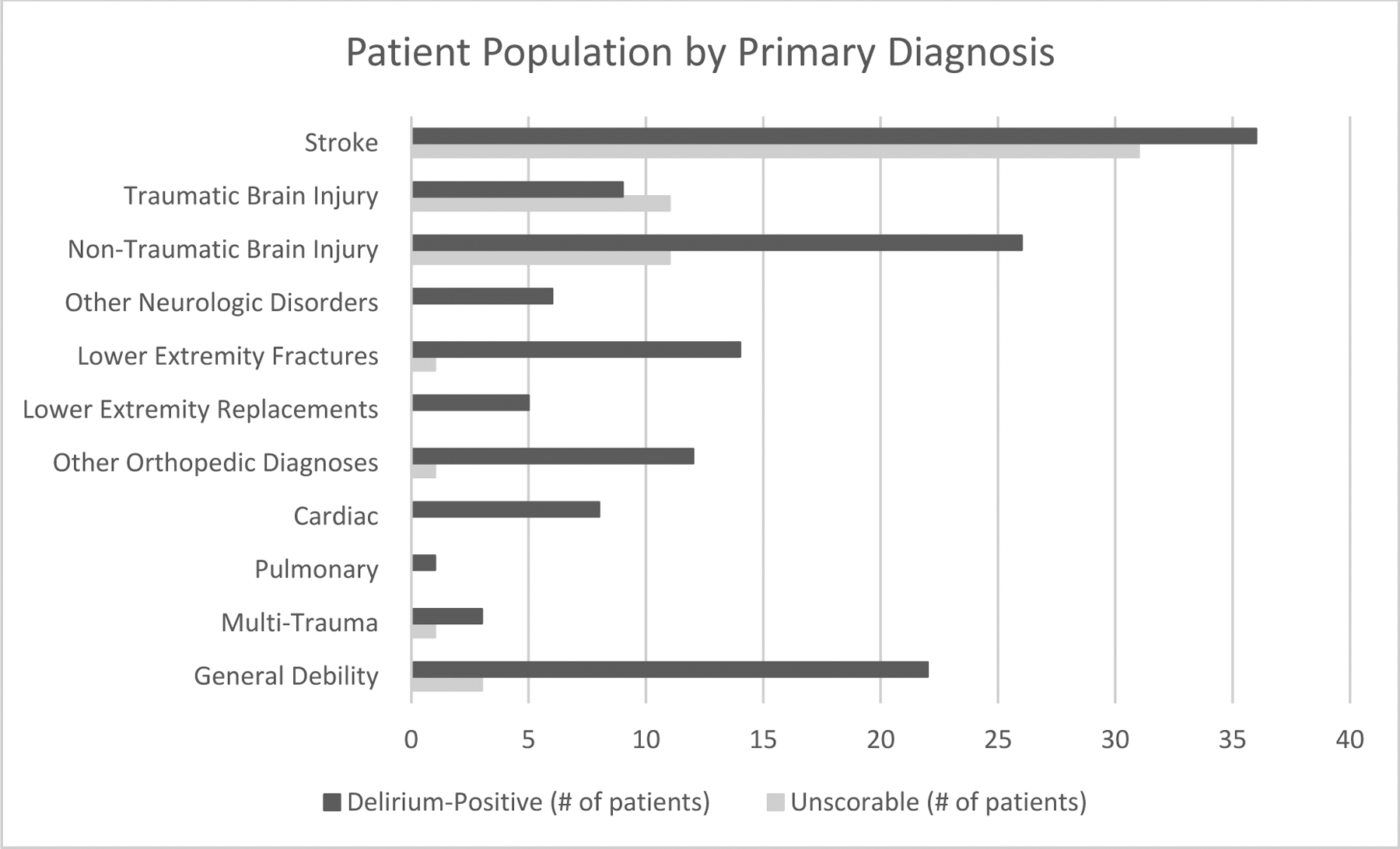
Patient population by primary diagnosis.
Delirium: additional outcomes
Delirium has long been associated with poor outcomes post-hospitalization. These outcomes, including length of stay and discharges home, in addition to acute care transfers, are monitored by the Centers for Medicare & Medicaid Services (CMS) as quality indicators of the IRFs. Studies in the general hospital population have found longer lengths of stay, decreased functional outcomes, and higher likelihood of discharges to nursing home versus home in the delirium population [31]. The results of this study demonstrate that, in the IRF setting, there are similar findings of lower motor and cognitive functional measures at discharge. The delirium group had longer lengths of stay and fewer discharges home, which were statistically significant when compared to the non-delirium group. Moreover, the statistically significant decreased gain in motor function for the delirium group represents an important clinical point. Theoretically, the patients in an IRF with acute changes in mental status may have limited carryover from their time in therapy, resulting in impaired advances in mobility. This translates to loss of motor gain for these patients who are not only admitted for neurologic diagnoses but also for those with orthopedic or traumatic diagnoses. There was a significant gain in cognitive FIM seen in the delirium population. Studies have identified 30–40% of the underlying causes of delirium include physiologic conditions that can be easily identified and prevented including, medical illness (e.g. dehydration), medication side effects, or neurological disorders [4,5]. It is plausible that interdisciplinary approaches in the IRF setting could be effective in resolving these temporary cognitive impairments.
There was a small portion of patients (3.8%) who were not scored during this study’s screening process, mainly due to communication difficulties which are analyzed, for the purpose of this study, as a separate group. While the unscorable group had a statistically significant higher proportion of acute care transfers compared to the non-delirium group, being screened as unscorable did not prove to be an independent risk factor for acute care transfers. When considering the unscorable group, which has not been described in the literature previously, there is a noticeable increased proportion of neurologic conditions (89.8%) compared to 50% in the non-delirium group on admission with lower FIM motor and cognitive scores compared to the non-delirium group (table 1). Also, increased proportions of comorbidities (dementia and cancer) in the unscorable group approached statistical significance and may result in an increased risk of acute care transfer. The unscorable group had similarly low functionality, increased length of stay and lower discharges home when compared to the non-delirium group. This study proposes that this group is inherently at higher risk for some of the same poor outcomes seen in the group that was positive for delirium at admission.
LIMITATIONS
Assessment of delirium was performed at admission as a protocol. Those with positive results at baseline were continuously reassessed for delirium resolution. However, those with negative results at baseline were not reassessed. This may have resulted in underestimation of prevalence of delirium. This potential misclassification would result in a bias towards non-significant results (i.e. no difference in transfers between the delirium and non-delirium group). In spite of this possibility, this study finds that positive screening of delirium was a significant predictor of transfers to acute care hospitals. A future study is recommended to characterize the serial assessments of these patients to further understand the natural progression of this condition. While delirium screening identified patients at risk of transfer to acute care hospitals, considering the complexity of the patient being transferred, there could be other factors for transfer to acute care hospitals. Lastly, further studies will be necessary to understand the unscorable population and its increased risk of acute care transfers within that population.
CONCLUSION
Delirium is as prevalent and associated with negative outcomes in the IRF setting as it has been previously reported in other post-acute care settings. Delirium screening independently predicts patients’ transfer to acute care hospitals from an inpatient rehabilitation facility, which is clinically significant as it is a modifiable risk factor. Since delirium is potentially reversible, the findings of this study suggest that early screening for delirium could successfully identify patients that are high-risk for transfers to the acute care hospital. The diversity of the population in this study suggests applicability to other large freestanding IRFs.
Acknowledgements:
The authors thank Anthony Lee, M. D. and Neil Jasey, M. D. for assisting in staff delirium care training as well as the staff who participated in admission 3D-CAM screening. We have no conflicts of interest to disclose.
Financial support: MO-P and AMB were supported by the Kessler Foundation and Wallerstein Foundation for Geriatric Improvement, the American Heart Association (12SDG33660442, Boukrina PI), the Charles and Anne Serraino Foundation, the National Institutes of Health/National Center for Medical Rehabilitation Research (R01HD058301, Barrett PI) and the National Institutes of Health/National Institute of Aging (R24 AG054259, Inouye PI).
Footnotes
This study was approved by the Institutional Review Board.
Financial disclosures: none
REFERENCES
- [1].Morandi A, Jackson JC. Delirium in the Intensive Care Unit: A Review. Neurol Clin 2011;29:749–63. doi: 10.1016/j.ncl.2011.08.004. [DOI] [PubMed] [Google Scholar]
- [2].Turco R, Bellelli G, Morandi A, Gentile S, Trabucchi M. The Effect of Poststroke Delirium on Short-Term Outcomes of Elderly Patients Undergoing Rehabilitation. J Geriatr Psychiatry Neurol 2013;26:63–8. doi: 10.1177/0891988713481265. [DOI] [PubMed] [Google Scholar]
- [3].Stelmokas J, Gabel N, Flaherty JM, Rayson K, Tran K, Anderson JR, et al. Delirium Detection and Impact of Comorbid Health Conditions in a Post-Acute Rehabilitation Hospital Setting. PLoS One 2016;11:1–8. doi: 10.1371/journal.pone.0166754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Inouye SK, Bogardus ST, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, et al. A Multicomponent Intervention to Prevent Delirium in Hospitalized Older Patients. N Engl J Med 1999;340:669–76. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- [5].Marcantonio ER, Kiely DK, Simon SE, Orav EJ, Jones RN, Murphy KM, et al. Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc 2005;53:963–9. doi: 10.1111/j.1532-5415.2005.53305.x. [DOI] [PubMed] [Google Scholar]
- [6].Inouye SK, Westendorp RGJJ, Saczynski JS. Delirium in elderly people. vol. 383 Elsevier Ltd; 2014. doi: 10.1016/S0140-6736(13)60688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the Functional Independence Measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil 1993;74:531–6. doi: 10.1016/0003-9993(93)90119-U. [DOI] [PubMed] [Google Scholar]
- [8].Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: 2015. [Google Scholar]
- [9].Ouslander JG, Naharci I, Engstrom G, Shutes J, Wolf DG, Alpert G, et al. Root Cause Analyses of Transfers of Skilled Nursing Facility Patients to Acute Hospitals: Lessons Learned for Reducing Unnecessary Hospitalizations. J Am Med Dir Assoc 2016;17:256–62. [DOI] [PubMed] [Google Scholar]
- [10].National Quality Forum. NQF Report on 2017 Activities to Congress and the Secretary of the Department of Health and Human Services. 2018.
- [11].Deshpande A, Millis S, Zafonte R, Hammond F, Wood D. Risk factors for acute care transfer among traumatic brain injury patients: Articles+. Arch Phys Med Rehabil 1997;78:p350–2. [DOI] [PubMed] [Google Scholar]
- [12].Daras LC, Ingber MJ, Deutsch A, Hefele JG, Perloff J. Geographic Region and Profit Status Drive Variation in Hospital Readmission Outcomes Among Inpatient Rehabilitation Facilities in the United States. Arch Phys Med Rehabil 2018;99:1060–6. doi: 10.1016/j.apmr.2017.11.011. [DOI] [PubMed] [Google Scholar]
- [13].Marcantonio ER, Ngo LH, O’Connor M, Jones RN, Crane PK, Metzger ED, et al. 3D-CAM: derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: a cross-sectional diagnostic test study. Ann Intern Med 2014;161:554–61. doi: 10.7326/M14-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Oh-Park M, Chen P, Romel-Nichols V, Hreha K, Boukrina O, Barrett AM. Delirium Screening and Management in Inpatient Rehabilitation Facilities. Am J Phys Med Rehabil 2018;97:754–62. doi: 10.1097/PHM.0000000000000962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Guerini F, Frisoni GB, Morghen S, Speciale S, Bellelli G, Trabucchi M. Clinical Instability as a Predictor of Negative Outcomes Among Elderly Patients Admitted to a Rehabilitation Ward. J Am Med Dir Assoc 2018;11:443–8. doi: 10.1016/j.jamda.2009.10.005. [DOI] [PubMed] [Google Scholar]
- [16].American Psychiatric Association., American Psychiatric Association. DSM-5 Task Force Diagnostic and statistical manual of mental disorders : DSM-5. American Psychiatric Association; 2013. [Google Scholar]
- [17].Hosker C, Ward D. Hypoactive delirium. BMJ 2017;357:1–8. doi: 10.1136/bmj.j2047. [DOI] [PubMed] [Google Scholar]
- [18].Stall N, Wong CL. Hospital-acquired delirium in older adults. CMAJ 2014;186:E61. doi: 10.1503/cmaj.130299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Inouye SK. Delirium in Older Persons. N Engl J Med 2006;354:1157–65. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- [20].Rigney TS. Delirium in the hospitalized elder and recommendations for practice. Geriatr Nurs n.d.;27:151–7. doi: 10.1016/j.gerinurse.2006.03.014. [DOI] [PubMed] [Google Scholar]
- [21].Young J, Inouye SK. Delirium in older people. BMJ 2007;334:842–6. doi: 10.1136/bmj.39169.706574.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Andrew MK, Freter SH, Rockwood K. Prevalence and outcomes of delirium in community and non-acute care settings in people without dementia: A report from the Canadian study of health and aging. BMC Med 2006;4:1–6. doi: 10.1186/1741-7015-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: A systematic review. J Am Geriatr Soc 2002;50:1723–32. doi: 10.1046/j.1532-5415.2002.50468.x. [DOI] [PubMed] [Google Scholar]
- [24].Kosar CM, Thomas KS, Inouye SK, Mor V. Delirium During Postacute Nursing Home Admission and Risk for Adverse Outcomes. J Am Geriatr Soc 2017;65:1470–5. doi: 10.1111/jgs.14823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Marcantonio ER, Flacker JM, Michaels MM, Resnick NM. Recovery After Hip Fracture 2000:618–24. [DOI] [PubMed]
- [26].Hammond FM, Horn SD, Smout RJ, Chen D, DeJong G, Scelza W, et al. Acute Rehospitalizations During Inpatient Rehabilitation for Spinal Cord Injury. Arch Phys Med Rehabil 2013;94:S98–105. doi: 10.1016/j.apmr.2012.11.051. [DOI] [PubMed] [Google Scholar]
- [27].Asher A, Roberts PS, Bresee C, Zabel G, Riggs RV., Rogatko A. Transferring Inpatient Rehabilitation Facility Cancer Patients Back to Acute Care (TRIPBAC). PM&R 2014;6:808–13. doi: 10.1016/j.pmrj.2014.01.009. [DOI] [PubMed] [Google Scholar]
- [28].Schneider JC, Gerrard P, Goldstein R, DiVita MA, Niewczyk P, Ryan CM, et al. Predictors of transfer from rehabilitation to acute care in burn injuries. J Trauma Acute Care Surg 2012;73:1596–601. doi: 10.1097/TA.0b013e318270d73d. [DOI] [PubMed] [Google Scholar]
- [29].Cullen E, Balas MC. Delirium monitoring and management in the acute care setting. Nurse Pract 2017;42:37–42. doi: 10.1097/01.NPR.0000526764.53348.d1. [DOI] [PubMed] [Google Scholar]
- [30].Mehta S, Cook D, Devlin JW, Skrobik Y, Meade M, Fergusson D, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Crit Care Med 2015;43:557–66. doi: 10.1097/CCM.0000000000000727. [DOI] [PubMed] [Google Scholar]
- [31].McCusker J, Cole M, Dendukuri N, Belzile E, Primeau F. Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ 2001;165:575–83. [PMC free article] [PubMed] [Google Scholar]


