Abstract
Background
The cardiovascular (CV) risk of patients with Type 2 diabetes (T2D) of Indo-Asian descent has never been objectively assessed, although it is documented that they have a higher prevalence of CV disease (CVD).
Aims
To identify groups of Indian patients with asymptomatic T2D who are at high risk of CVD as per the QRISK calculator.
Method
After an adequate power calculation, a nation-wide study of patients with asymptomatic T2D was conducted. The QRISK3 scores of these patients were used to derive a 10-year risk of CV events. High CVD risk was defined as ≥20% risk of CV event in 10 years.
Results
For a total of 1538 patients across 154 outpatient departments, the QRISK3 scores were collated. Median 10-year CVD risk was 22.2%. Mean 10-year CVD risk was 28.4% (standard deviation 22.1%), representing a 5.7-fold increase vs. controls (i.e., matched healthy adults). Absolute CVD risk increased linearly with age. Over 50% of T2D males aged above 45 years had a high (>20%) CVD risk. Women aged more than 55 years had a high risk of CVD. More than 50% of patients with a T2D duration of more than 5 years had a high risk of CVD as per the QRISK3 calculator.
Keywords: Type 2 diabetes, CV risk, QRISK3, Indian patients, Asymptomatic
Abbreviations: MARK, measure of asymptomatic cardiovascular disease risk in Type 2 diabetes; CV, cardiovascular; CVD, CV disease; T2D, Type 2 diabetes; T2DM, Type 2 diabetes mellitus; CAD, coronary artery disease
1. Background
The prevalence of Type 2 diabetes mellitus (T2DM) and associated vascular complications has progressively increased worldwide.1,2 Current estimates suggest that more than 73 million Indian adults suffer from T2DM.1 Of note, globally, every third T2DM patient is estimated to suffer from cardiovascular disease (CVD).3
Studies have suggested an increased CVD risk in South Asian patients.4,5 In patients with CVD, South Asian ethnicity may predispose to higher risk of death compared to other ethnicities.4 CVD accounts for 1 in every 3 deaths in Indian adults aged above 40 years.2
Notably, in T2DM, asymptomatic patients may harbour subclinical coronary artery disease (CAD).6 Its extent is highly variable, going from clinically insignificant plaque, to silent myocardial infarction and death. Limited evidence suggests that patients of South Asian ethnicity may have an increased prevalence of asymptomatic CAD in T2DM.7,8
During the course of routine diabetes check-ups, the use of invasive tests to screen each patient is not feasible nor recommended. Moreover, the existing evidence does not suggest benefits in performing a generalized CV screening of asymptomatic T2DM patients. This is partly due to limited evidence to date supporting clinical outcome improvements by using this approach. In addition, a holistic management of CVD risk forms the fundamental approach of diabetes care regardless of underlying CVD.9 However, advances in pathology, diagnosis and treatment options have significantly improved our limited understanding of cardiovascular diabetology. Although diabetes itself is a major risk factor for CVD, the risk of developing events may differ by several-folds across the T2DM spectrum. Importantly, residual risk of CV events and death has remained a challenge despite existing measures.10,11 Thus, the stratification of CVD risk in T2DM remains an area of clinical interest. As a principle of precision medicine, CVD risk stratification may help individualize management strategies and optimize the value of health care delivery.
The risk of CV events in a real-world setting may be predicted by some simple clinical tools. For example, a clinical score based on the patient's clinical profile may help predict the future risk of CVD events. Such scores derive from observations in long-term studies. To date, numerous CVD risk scores and calculators have been developed (e.g., UKPDS Risk Engine, JBS3, Framingham Risk Score, SCORE, QRISK3, etc.)12, 13, 14, 15 Most of these risk scores, for example, SCORE recommended by the European Society of Cardiology (ESC) specifically recommends against using such scoring systems for CV risk stratification in the diabetic patients.16 In addition, the ESC 2019 guidelines mention the non-applicability of the scoring system on patients of Asian and African origin as it has not been validated in those population.16 Hence, there is a need for an Indian-specific objective CV scoring system. The QRISK3 score was developed by performing specific observations in various ethnicities. These included the Indian ethnicity in the United Kingdom.15 1,59,488 individuals of Indian origin (77,683 males and 81,805 females) were included in the derivation cohort from 1309 practices.15 The risk score created from the derivation cohort was tested on the validation cohort consisting of 49,625 Indian individuals (23,146 males and 26,479 females) with a median follow-up of 4.4 years.15 As patients of Indian ethnicity were also included in the development of QRISK3, this score will be more specifically applicable to Indian patients, based on ethnic differences in CVD risk. Furthermore, QRISK3 can also be used in patients of T2DM (unlike SCORE). In addition, QRISK3 also includes certain reliable and independent CVD risk predictors, which have not been considered in most of the other risk scores (e.g., erectile dysfunction, depression, anxiety, corticosteroid use, autoimmune disease, etc). The QRISK3 score may underestimate the CV risk in the younger population, age being an independent CV risk factor inversely associated with CV risk. However, QRISK3 score has the option to estimate the lifetime CV global risk in such scenarios thereby overcoming this limitation. Given the possible genetic influence of Indian ethnicity, the QRISK3 score represents the most accurate CVD screening tool available (to date) for the Indian population.
Characterization of the burden of CVD in the Indian population has been attempted by numerous analyses.2,17, 18, 19, 20 However, to date, in a routine care setting, limited evidence is available on the CV risk stratification in asymptomatic T2DM patients. To overcome this limitation, in the present study, we analyzed CVD risk profile in Indian outpatient settings. For this real-world analysis, we evaluated QRISK3 scores in asymptomatic T2DM patients who visited outpatient departments in institutions across the country.
2. Methodology
The present real-world analysis was intended to measure asymptomatic CVD risk (MARK) in Indian T2DM outpatient individuals. MARK was designed as a cross-sectional survey involving 154 outpatient departments across India. Adult T2DM patients (aged 25–84 years) were considered for the analysis. The eligibility criteria included absence of symptom(s) suggestive of CVD. Patients with a known history of CVD event (acute coronary syndrome, stroke, or amputation related to peripheral arterial disease) were excluded from the study. At each outpatient department, 10 consecutive eligible patients were included in the survey.
The QRISK3 score was used as the primary parameter for assessment. This score provides information on CVD absolute and relative risks over a 10-year period. Relative risk was calculated based on the CVD risk of a healthy person similar in age, gender and ethnicity. The analysis was designed to provide descriptive observations. Inferential statistics were not applied.
For sample size estimation, certain assumptions were considered. High CVD risk was defined as ≥20% risk of a CVD event over a 10-year period.15 For the MARK survey, it was assumed that in at least 50% of asymptomatic T2DM patients, a high CVD risk would be identified by using the QRISK3 calculator. The maximum margin of error was considered as 3%. Based on these assumptions, to ensure adequate precision of the findings, a minimum of 1112 patients were needed for the survey.
3. Results
A total of 1538 asymptomatic T2DM patients without previous history of CVD event were included in the survey. Demographic patients' characteristics are summarized in Table 1.
Table 1.
Demographics and CVD risk factors.
| Clinical parameter (n = 1538) | N (%) | Mean value | Standard deviation |
|---|---|---|---|
| Age (years) | 54.5 | 11.2 | |
| Gender: | |||
| Male | 897 (58.3) | ||
| Female | 641 (41.7) | ||
| Body mass index (kg/m2) | 27.1 | 4.5 | |
| Systolic blood pressure (mmHg) | 135.4 | 16.6 | |
| Total cholesterol: HDL cholesterol ratio | 4.9 | 1.7 | |
| Duration of T2DM (years): | |||
| ≤5 | 503 (32.7) | ||
| >5–10 | 552 (35.9) | ||
| >10–15 | 297 (19.3) | ||
| >15–20 | 120 (7.8) | ||
| >20 | 66 (4.3) | ||
| Smoking status: | |||
| Non-smoker | 1170 (76.1) | ||
| Ex-smoker | 150 (9.8) | ||
| Light smoker | 136 (8.8) | ||
| Moderate smoker | 57 (3.7) | ||
| Heavy smoker |
25 (1.6) |
||
| Clinical parameter |
Yes, n (%) |
No, n (%) |
Missing, N (%) |
| Angina/heart attack in a 10 relative <60 | 369 (24.0) | 1167 (75.9) | 2 (0.1) |
| Chronic kidney disease (Stage 3, 4 or 5) | 177 (11.5) | 1359 (88.4) | 2 (0.1) |
| Atrial fibrillation | 76 (4.9) | 1460 (94.9) | 2 (0.1) |
| History of migraine | 123 (8) | 1414 (91.9) | 1 (0.1) |
| Rheumatoid arthritis | 81 (5.3) | 1456 (94.7) | 1 (0.1) |
| Systemic lupus erythematosus | 16 (1.0) | 1520 (98.8) | 2 (0.1) |
| Severe mental illness | 36 (2.3) | 1501 (97.6) | 1 (0.1) |
| Erectile dysfunction | 121 (7.9) | 1416 (92.1) | 1 (0.1) |
| Treatment for blood | 968 (62.9) | 570 (37.1) | 0 (0.0) |
| On atypical antipsychotic medication | 31 (2.0) | 1506 (97.9) | 1 (0.1) |
| On regular steroid consumption | 34 (2.2) | 1503 (97.7) | 1 (0.1) |
Median 10-year CVD risk was 22.2%, suggesting that at least half of the patients had a high 10-year CVD risk of ≥20%. The mean 10-year CVD risk was 28.4% (standard deviation (SD) 22.1%). Such result represented a 5.7-fold greater CVD risk vs. controls (i.e., a similar population of healthy adults).
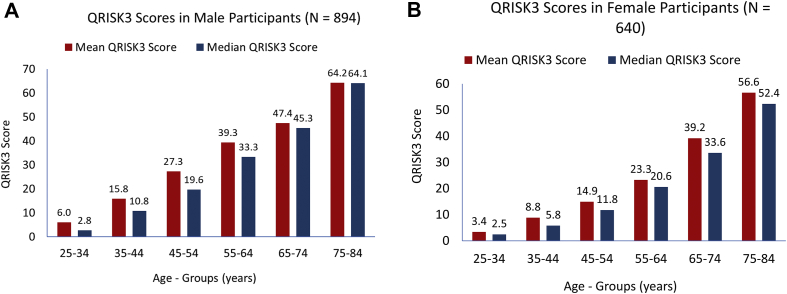
In both genders, a linear increase of the mean 10-year CVD risk was observed with increasing age. Across all age groups, the absolute risk was numerically lower in female vs. male patients. In the age group of 45–54 years, almost 50% of the male patients had high CVD risk (QRISK3 score: mean was 27.3%, and median was 19.6%; Fig. 1A). Female patients in the age group of 55–64 years demonstrated this proportion a decade later (QRISK3 score: mean was 23.3%, and median was 20.6%; Fig. 1B). However, both male and female patients had similar relative increases in CVD risk compared to healthy adults of similar age and gender.
Fig. 1.
Mean 10-year QRISK3 score in different age groups in male participants (n = 894; A) and female participants (n = 640; B).
As age increased, a progressively declining trend of the relative CVD risk was observed. In younger male patients in the age groups of 25–34 and 35–44 years, the CVD risk increased by 6.8-fold and 5.5-fold, respectively. In comparison, male patients in the age groups of 65–74 and 75–84 years had 2.3-fold and 1.8-fold increased CVD risk, respectively. Female patients demonstrated similar trends. Specifically, relative increases of 6.7-fold and 5.6-fold were observed in the age groups of 25–34 and 35–44 years, respectively. In addition, the corresponding increments were 2.4-fold and 2.1-fold in the age groups of 65–74 and 75–84 years, respectively.
The 10-year CVD risk increased linearly with increase in the T2DM duration. Over half of the patients with a T2DM duration of 5–10 years had a high CVD risk (Table 2).
Table 2.
Mean and median 10-year CVD risk according to duration of T2DM.
| T2DM duration (years) | n (%) | Parameter | 10-year QRISK-3 score (%) | Score of a healthy person with the same age, gender and ethnicity (%) | Relative risk |
|---|---|---|---|---|---|
| ≤5 | 503 (32.70) | Mean | 19.46 | 5.11 | 7.46 |
| Median | 13.10 | 3.10 | 3.70 | ||
| Standard deviation | 18.67 | 5.68 | 20.46 | ||
| >5–10 | 552 (35.89) | Mean | 28.38 | 7.53 | 5.37 |
| Median | 21.85 | 5.40 | 3.60 | ||
| Standard deviation | 21.17 | 6.63 | 8.93 | ||
| >10–15 | 297 (19.31) | Mean | 36.00 | 10.06 | 4.59 |
| Median | 29.50 | 7.90 | 3.40 | ||
| Standard deviation | 23.64 | 7.83 | 4.00 | ||
| >15–20 | 120 (7.80) | Mean | 39.93 | 13.82 | 3.56 |
| Median | 38.1 | 11.8 | 2.65 | ||
| Standard deviation | 21.36 | 8.26 | 2.79 | ||
| >20 | 66 (4.29) | Mean | 41.19 | 17.92 | 2.96 |
| Median | 41.05 | 15.95 | 2.25 | ||
| Standard deviation | 18.93 | 11.45 | 2.06 |
4. Discussion
The present study is unique. It is the first nation-wide, real-world analysis of CVD risk in asymptomatic T2DM patients using the QRISK3 calculator, performed in an Indian outpatient setting. In accordance with our baseline assumptions, we found that over half the patients had a high 10-year CVD risk of >20%. The absolute CVD risk was greater in elder patients. However, the relative CVD risk was greater in younger age groups. Thus, as compared to healthy adults with similar demographic profile, T2DM patients in the age group of 25–44 years had a >5-fold increase in CVD risk. This suggests that if a holistic CVD risk management is implemented at a younger age, there may be higher chances of modifying CVD's progressive course. Furthermore, female participants had a lower mean absolute CVD risk compared to male participants, across all age groups. A mean ‘high CVD risk’ of >20% was observed in the age group of 55–64 years in females. On the contrary, this finding was observed a decade earlier in males. These findings may be explained by the possible influence of biologically protective mechanisms in the female patients, which may decline post-menopause.
Both strengths and limitations can be identified in the present study. In our analysis, precision of findings was ensured by meeting the statistical requirements. However, the analysis was not inferential by design and the observations should be considered hypothesis-generating only. In addition, several lifestyle-related issues—for example, chewing tobacco—were not represented in this risk score. This might result in under-estimation of CV risk as these individuals would be enlisted as non-smokers. Among the statistical limitations, SD related to age (11.2 years) and systolic blood pressure (33.2 mmHg) seems wide, which could be due to the influence of outliers. However, the calculated 2-SD for age results in 95% of the age-data falling between 32.1 and 76.9 years, which replicates the age represented in the QRISK3 derivation and validation cohort (25–84 years). Similarly, 95% of data related to systolic blood pressure lies between 102.2 and 168.6 mmHg representing the 2-SD of the mean. The study represented a diverse patient population across the country, with wide variations in the outcome(s) of interest. In such situations, the median value(s) represents the overall prevalence of CVD risk more appropriately, as compared to the mean value(s). In the MARK survey, the median as well as mean values of CVD risk, based on QRISK3 score, were >20%. In abidance with the principle of personalized medicine, CVD risk-stratification using the QRISK3 score, may be a meaningful clinical approach to recognize the underlying CVD risk in every individual asymptomatic patient of Type 2 diabetes (T2D).
The QRISK3 assessment tool includes ethnicity (including Indian) as an option. This may account for the genetic predisposition of Indian ethnicity to CVD risk. However, the influence of environmental factors cannot be understated. Specifically, within the different regions of India itself, wide variations in CVD risk have been observed.18 Thus, although QRISK3 may represent a more pertinent option among the available CVD risk calculators, its validity may still not be fool proof for our setting.
Clinical use of CVD risk calculators may be helpful in stratifying the CVD risk. This is especially true in patients without obvious cardiovascular symptoms. Notably, risk stratification may be helpful in preventing over-medicalization in low-risk patients. Furthermore, it may aid guide high-risk patients to the appropriate measures. CVD is a continuum in T2DM, requiring effective management at various stages. Indeed, small studies from Roos et al7 and Gobardhan et al8 have demonstrated the presence of significant obstructive CAD, in 2 of every 5 asymptomatic T2DM patients from South Asian ethnicity. The high 10-year CVD risk identified by various clinical scores, correlated with an increased risk of subclinical CAD.
5. Conclusion
This is the first ever study from India, which identifies CVD risk in T2D patients who are asymptomatic. This study could have huge ramifications in identifying patients with T2D at high risk who would previously have gone unrecognized and would therefore miss out on treatment with life-altering medications that are now available.
Funding
The survey was performed by PharmEDGE group. The PharmEDGE group has received financial support from Boehringer Ingelheim for this survey.
Author contributions
SG and BS conceptualized the study. JV and MB performed the statistical calculation and prepared the draft manuscript. Final editing was performed by SG, BS and JV.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of interest
All authors have none to declare.
Acknowledgments
The authors acknowledge the effort put in by PharmEDGE group for designing the study along with the authors, collecting data from the concerned physicians, and performing the data analysis. They would also like to acknowledge all the physicians who accepted to participate in the survey.
References
- 1.International Diabetes Federation . vol. 8. 2017. Global factsheet.http://www.diabetesatlas.org/ (IDF Diabetes Atlas). [Google Scholar]
- 2.India State-Level Disease Burden Initiative CVD Collaborators The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health. 2018 Dec;6(12):e1339–e1351. doi: 10.1016/S2214-109X(18)30407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Einarson T.R., Annabel A., Ludwig C., Panton U.H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17:83. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volgman A.S., Palaniappan L.S., Aggarwal N.T. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018 Jul 3;138(1):e1–34. doi: 10.1161/CIR.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 5.Gholap N., Davies M., Patel K., Sattar N., Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Primary Care Diabetes. 2011 Apr 1;5(1):45–56. doi: 10.1016/j.pcd.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Lee C.H., Lee S.W., Park S.W. Diabetes and subclinical coronary atherosclerosis. Diabetes Metabol J. 2018 Oct 1;42(5):355–363. doi: 10.4093/dmj.2018.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roos C.J., Kharagjitsingh A.V., Jukema J.W., Bax J.J., Scholte A.J. Comparison by computed tomographic angiography- the presence and extent of coronary arterial atherosclerosis in South Asians versus Caucasians with diabetes mellitus. Am J Cardiol. 2014;113:1782–1787. doi: 10.1016/j.amjcard.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Gobardhan S.N., Dimitriu-Leen A.C., van Rosendael A.R. Prevalence by computed tomographic angiography of coronary plaques in South Asian and white patients with type 2 diabetes mellitus at low and high risk using four cardiovascular risk scores (UKPDS, FRS, ASCVD and JBS3) Am J Cardiol. 2017;119(5):705–711. doi: 10.1016/j.amjcard.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association Cardiovascular disease and risk management: standards of medical care in diabetes-2019. Diabetes Care. 2019 Jan 1;42:S103–S123. doi: 10.2337/dc19-S010. [DOI] [PubMed] [Google Scholar]
- 10.Kaasenbrood L., Boekholdt S.M., Van Der Graaf Y. Distribution of estimated 10-year risk of recurrent vascular events and residual risk in a secondary prevention population. Circulation. 2016 Nov 8;134(19):1419–1429. doi: 10.1161/CIRCULATIONAHA.116.021314. [DOI] [PubMed] [Google Scholar]
- 11.Rawshani A., Rawshani A., Franzén S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017 Apr 13;376(15):1407–1418. doi: 10.1056/NEJMoa1608664. [DOI] [PubMed] [Google Scholar]
- 12.Bertoluci M.C., Rocha V.Z. Cardiovascular risk assessment in patients with diabetes. Diabetol Metab Syndrome. 2017;9(1):25. doi: 10.1186/s13098-017-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Dieren S., Beulens J.W.J., Kengne A.P. Prediction models risk of cardiovascular disease in patients with type 2 diabetes: a systematic review. Heart. 2012;98:360–369. doi: 10.1136/heartjnl-2011-300734. [DOI] [PubMed] [Google Scholar]
- 14.SCORE Risk Charts The European cardiovascular disease risk assessment model. https://www.escardio.org/Education/Practice-Tools/CVD-prevention-toolbox/SCORE-Risk-Charts [Online] Available at:
- 15.Hippisley-Cox J., Coupland C., Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017 May 23;357:j2099. doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD the Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD) Eur Heart J. 2020;41:255–323. doi: 10.1093/eurheartj/ehz486. [DOI] [PubMed] [Google Scholar]
- 17.Gupta A., Gupta R., Sharma K.K. Prevalence of diabetes and cardiovascular risk factors in middle-class urban participants in India. BMJ Open Diabetes Res Care. 2014 Dec 1;2(1) doi: 10.1136/bmjdrc-2014-000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geldsetzer P., Manne-Goehler J., Theilmann M. Geographic and sociodemographic variation of cardiovascular disease risk in India: a cross-sectional study of 797,540 adults. PLoS Med. 2018 Jun 19;15(6) doi: 10.1371/journal.pmed.1002581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prabhakaran D., Jeemon P., Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016 Apr 19;133(16):1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 20.D’agostino R.B., Vasan R.S., Pencina M.J. General cardiovascular risk profile for use in primary care. Circulation. 2008 Feb 12;117(6):743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.