Abstract
Background/Objective
The manifestation of functional impairment in patients’ daily lives and interference with things they value is poorly understood. If values are compromised in patients, as theory suggests, social contexts (and the lack thereof) are especially important – though this is currently unexplored. We therefore examined whether daily values-consistent behavior was associated with the importance of a value and whether it involved social or non-social activity.
Method
Using Event Sampling Methodology, we examined daily values-consistent behavior in 57 transdiagnostic inpatients and 43 transdiagnostic outpatients at the beginning of treatment. Patients’ values-consistent behavior, its importance, and (social vs non-social) context was sampled six times per day during a one-week intensive longitudinal examination.
Results
Across both groups, the probability of subsequent values-consistent behavior increased if (1) it was judged as more important by the patient or (2) if it was embedded in a social context. The probability of reporting values-consistent behavior was higher for outpatients than inpatients.
Conclusions
Clinicians are encouraged to examine the values of their patients more closely and to especially monitor important and/or social values. Incorporating these into clinical work might increase patients’ values-consistent behavior, which can play a role in reducing suffering.
Keywords: Transdiagnostic, Event Sampling Methodology (ESM), Consistent behavior, Values, Quasi-experiment
Resumen
Antecedentes/Objetivo
La interferencia funcional en la experiencia cotidiana y los valores personales de pacientes está insuficientemente estudiada. Si sus valores son perturbados, los contextos sociales –y su carencia– son especialmente importantes, pero esto permanece inexplorado. Examinamos si los comportamientos coherentes con los valores están asociados a la importancia acordada e implicación en actividades sociales/no sociales.
Método
Se empleó metodología de muestreo de eventos para examinar la coherencia del comportamiento diario con los valores de 57 pacientes en clínica hospitalaria y 43 en clínica ambulatoria al comienzo de un tratamiento transdiagnóstico. A través de una investigación longitudinal intensiva durante siete días, el comportamiento coherente con los valores, su importancia y el contexto de la actividad en curso (social/no social) fueron muestreados seis veces por día.
Resultados
En ambos grupos, la probabilidad de comportamiento coherente con los valores aumentó cuando (1) este era considerado como más importante y (2) cuando este se produjo en un contexto social. La probabilidad de tal comportamiento fue mayor para los pacientes en tratamiento ambulatorio que para aquellos en tratamiento clínico.
Conclusiones
Se recomida explorar los valores de los pacientes, particularmente aquellos juzgados como más importantes y/o sociales. Su incorporación en la práctica clínica podría promover la coherencia entre valores y comportamientos subsecuentes.
Palabras clave: Transdiagnóstico, Event Sampling Methodology (ESM), Comportamiento coherente, Valores, Cuasi-experimento
One criterium common to all DSM categories is that symptoms must cause a clinically significant impairment in functioning (American Psychiatric Association, 2000). However, functioning tends to be measured on an abstracted level (e.g., through assessing general working ability or satisfaction with working capacity; Trompenaars, Masthoff, Van Heck, Hodiamont, & De Vries, 2005). Information about how daily routines are implemented or stymied are usually measured retrospectively, while information assessed in a real-time fashion in participants’ natural environment is largely missing. As a result, little systematic knowledge exists about the daily lives of patients as they present for treatment (Wersebe, Lieb, Meyer, Hofer, & Gloster, 2018). Patients’ everyday lives are assumed to be distinguishable from individuals without a diagnosis. The omnipresence of the impairment in functioning across all DSM categories merits investigating a broad swath of diagnoses. For example, patients diagnosed with obsessive-compulsive disorder spend a substantial amount of time engaging in obsessions and compulsions (e.g., hand washing, ordering, checking) or patients diagnosed with depression who feel worthless or guilty often contribute to impairment in social, occupational, or other important areas of functioning (Kupferberg, Bicks, & Hasler, 2016). Another example are patients diagnosed with agoraphobia, who avoid places or situations from which escape might be difficult or embarrassing or in which help may not be available (American Psychiatric Association, 2000), thereby restricting their travel possibilities. Whereas symptoms capture part of the impairment, they do not inform about factors that exacerbate the functional impairment nor do they indicate when and how they are able to successfully navigate through daily life.
Investigating patients’ everyday life also has clinical implications. Daily life is impacted by adverse life events (such as death of a loved one or romantic breakups), which have been related to more depressive symptoms (Keller & Nesse, 2006). For example, a divorce can lead to social bonds being lost. Loss of social bonds, in turn, affects daily life and, in more severe cases, also daily functioning (Keller & Nesse, 2006). Therefore, regardless of whether stressors occur daily or as major life events, actively engaging in values may have a pivotal effect on subsequent suffering (Gloster et al., 2017).
However, perceiving something as important and acting or behaving in the direction of that value are two different things. In order to properly assess such behaviors, it is important to capture both the activities patients’ value and whether they actually engage in such activities. Behaviors that are connected to goals and values are positively associated with social functioning (McCracken, Chilcot, & Norton, 2015). In patients there is an observable discrepancy between values and behavior (Čolić et al., 2020, Hoyer et al., 2019). In the Acceptance and Commitment Therapy (ACT)-literature, such a discrepancy has been shown to contribute to lower levels of well-being (Gloster et al., 2015, Hayes et al., 2006). Increasing values-consistent behavior (i.e., behavior that is consistent with one’s values) precedes reductions in suffering in outpatients with panic disorder (Gloster et al., 2017). However, which factors are associated with increased behavior connected to goals and values remains an open question. Current instruments attempting to capture the congruence between values and behavior correspond to a very specific time point in life (Ivanoff, Jang, Smyth, & Linehan, 1994), or collect data in a retrospective fashion (Wilson, Sandoz, Kitchens, & Roberts, 2010). Therefore, concerns regarding biases introduced by retrospective recall are raised (Rinner et al., 2019), while the question about what is important to patients in their everyday life, and whether there is a difference between in- and outpatients, remains open.
When investigating patients’ daily lives, it is important to capture the context in which they are acting. One of the most important contexts for humans is the social context (e.g., with a close friend or family member, in a group of strangers, alone, etc.; e.g., Rubin & Stuart, 2018). The social context is important regarding our health and well-being. For instance, social interaction had a motivating effect on participants, which were then more likely to continue exercising (Nielsen et al., 2014). The social context is especially important to examine in inpatient treatment as it likely differs from outpatient treatment. Inpatients usually stay in the hospital for at least one night, are more dependent on nursing care (Campos Andrade, Lima, Pereira, Fornara, & Bonaiuto, 2013), and are potentially in contact with other fellow patients. Outpatients depend less and have less contact with medical and nursing care, and spend less time in the health care setting. A hospital’s social environment likely has different relevance for inpatients and outpatients (Campos Andrade et al., 2013). It is thus essential to consider the treatment setting to account for differing social contexts the patients are in. While patients may already live in a specific daily social context, inpatients in particular may form a new form of social context, specific to their treatment. Outpatients might more or less stay in their specific social context of their daily life. More research is needed to better understand the mechanisms that influence a patient and their social context.
To answer the questions of what in- and outpatients value in their everyday life, what significance daily social interactions have, and what increases the probability that things people value translate into actual values-consistent behavior, it is necessary to understand patients’ behavior in their natural environment as opposed to in the laboratory or by asking them to think about across several months and estimate an average (Myin-Germeys et al., 2018). Event Sampling Methodology (ESM) allows precisely this examination.
The present paper’s aim is to investigate the everyday life of in- and outpatients and the importance of daily behaviors and, more specifically, whether daily social (i.e., with other people) or non-social (i.e., without other people) behaviors impacted their values-consistent behavior. For the sake of clarity and brevity, we will henceforth use the term “consistent behavior” when referring to “values-consistent behavior”.
Towards this aim, we explored four research questions. First, in- and outpatients would report different probabilities of engagement in life areas (e.g. work, hobby, relaxing etc.) important to them (research question 1). Second, in- and outpatients would report different probabilities of consistent behavior (research question 2). Third, patients would show consistent behavior more frequently the more important the value domain was to them (research question 3a), and this would differ between in- and outpatients (research question 3b). Fourth, patients would show consistent behavior more frequently if the valued domain was social (research question 4a), and this would differ between in- and outpatients (research question 4a).
Method
Participants
Participants (inpatients, n = 57; outpatients, n = 43) were recruited from two specialized clinics (inpatient and outpatient) from ongoing intake procedures. The mean age across the whole sample was 34.45 years (SD = 11.88, range: 18 to 65 years), and 48% of the participants were female. The mean age for the inpatients was 33.51 years (SD = 10.82, range: 18 to 65 years), and 42.11% of the participants were female. The mean age for the outpatients was 35.80 years (SD = 13.14, range: 18 to 64 years), and 55.81% of the participants were female. Participants represent a subset of patients recruited for a larger ongoing study on transdiagnostic treatment non-responding patients (see Villanueva, Meyer, Rinner et al., 2019). Inclusion criteria were: Minimum 18 years of age, ability to speak German sufficiently, present for therapy and ability to attend sessions, and signing an informed consent statement. Exclusion criteria were acute suicidal intent, acute substance dependency, active mania, previous experience with ACT, and inability to read or complete assessments. Otherwise all diagnoses were included (Villanueva, Meyer, Rinner et al., 2019). Participants presented with the following disorders: Affective disorders (35.45%), phobias and other anxiety disorders (37.79%), obsessive-compulsive disorders (13.30%), somatoform disorders (6.43%), impulse control disorders (3.97%), and attention deficit hyperactivity disorder (0.94%). When participants entered the clinic, medication was optimized when necessary, as determined by the attending physician in consideration of patient preference.
Instruments and procedure
This study reports on a seven-day phase of Event Sampling Methodology (ESM) from an overarching clinical trial. Participants completed informed consent procedures during the first week of treatment before data collection. During this first week, participants entered a seven-day phase of ESM, for which participants carried a study-issued smartphone. They kept the smartphone for seven days, after which they handed it back to the study personnel. The study was approved by the Ethics Committee of northwestern and central Switzerland (Ethikkommission Nordwest- und Zentralschweiz; EKNZ): Project 2165/13. For more details on the exact procedure, please see Villanueva, Meyer, Rinner et al. (2019).
Event Sampling Methodology (ESM)
Understanding participants’ social behavior requires collecting data in participants’ natural environment. Implementing ESM through usage of a smartphone allows the examination of patients’ daily life, including the assessment of moods, thoughts, symptoms or behaviors, environmental and social contexts, all of which change over time. Thus, ecologically valid data can be collected in a real-time fashion while capturing dynamic changes of variables. Since human memory is subject to recall bias, ESM also reduces the effect of recall bias through real-time data collection (Gloster et al., 2008, Myin-Germeys et al., 2018, Rinner et al., 2019).
Assessment
All participants completed the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; Wittchen, Wunderlich, Gruschwitz, & Zaudig, 1997) to determine diagnostic status at the beginning of treatment. We used the SCID-I (current diagnosis), which has moderate to excellent values for reliability and validity (DeFife and Westen, 2012, Lobbestael et al., 2011). Diagnoses were also rated on the Anxiety Disorders Interview Schedule (ADIS) severity rating scale (Brown, DiNardo, & Barlow, 1994). The diagnosis with the highest severity score was defined as the primary diagnosis.
ESM data were collected six times a day using signal-contingent ESM on the smartphone every three hours (e.g., 8am, 11am, 2 pm, 5 pm, 8 pm, and 11 pm). ESM data collection was adjusted based on individual daily parameters of patients (e.g., waking time of participants, fixed breaks at work etc.). Participants responded to items on the smartphone with regard to multiple aspects of their behavior: First, they were asked about their plans and intentions (“What is the most important thing you are going to do in the next three hours?”), and asked to categorize it into one of the following value domains: Working/studying, commute, media usage, interacting with family, interacting with others, being alone/bored, household, hobby (except physical activity), physical activity, eating/drinking, or enjoying/relaxing. Participants could choose only one domain, therefore choosing none or more than one was not possible.
Second, in the next questionnaire three hours later, they were asked about their past behavior (“What was most important to you in the last three hours?”) and asked to categorize it into the same previously mentioned domains. This item was not included in the morning questionnaire. The degree to which the planned and past behavior occurred in the same domain was the basis for the categorization of consistent vs. inconsistent behavior. For example, assuming the implementation of ESM at 8am, 11am, 2 pm, 5 pm, 8 pm, and 11 pm, each questionnaire was paired with the following questionnaire to compare the domains in which the planned and past behavior had occurred (e.g., 8am was compared to 11am, 11am was compared to 2 pm, etc.). Consequently, only the 8am questionnaire was not comparable to a preceding questionnaire, and the 11 pm questionnaire was not comparable to a following questionnaire because in both cases patients were assumed to be asleep.
Third, they were asked about the importance of the past valued behavior: “To what degree did you really want to spend your time like this?” and “To what degree does this behavior correspond to the way you want to live your life?”, both on a scale from 0-100 (not at all to very much). Further, some behavior happens in a social context (i.e., in interaction with other people) and some behavior happens outside of a social context (i.e., without interaction with other people). We subsequently dichotomized value domains into “social domains” vs. “non-social domains” to investigate patients’ consistent behavior in social vs non-social contexts. Social domains included Working/studying, interacting with family, interacting with others, and eating/drinking. Non-social domains included the remaining domains, i.e., commute, media usage, being alone/bored, household, hobby (except physical activity), physical activity, and enjoying/relaxing. Examples that were listed by patients included the following: therapy or working in the laboratory (working/studying), going to the clinic or going home (commute), watch TV or listen to music (media usage), talking to the brother or playing with the son (interacting with family), arguing for my rights or make small talk over breakfast (interacting with others), waiting or feeling lonely (being alone/bored), tidying up or grocery shopping (household), reading or playing an instrument (hobby [except physical activity], going jogging or going for a walk (physical activity), eating dinner or drinking tea (eating/drinking), and sleeping or lazing around (enjoying/relaxing).
Statistical analysis
Data collected from ESM studies are repeated measures with interdependent observations of data nested within individuals. Data was included in the analyses if a participant answered more than 50% of the smartphone reminders. Twenty two participants completed less than 50% of ESM time points and were therefore removed from the data set. In consideration of the structure of the data, binomial Generalized Linear Mixed Models (GLMMs) were implemented for all research questions. For research question 1 (i.e., in- and outpatients would report different frequencies of engagement in life areas important to them), a GLMM was set up for each individual domain, resulting in 11 models, with treatment setting as the predictor. The outcome for research questions 3a and 4a was defined as consistent behavior, while the predictors were importance of the domain (research question 3a, patients would show consistent behavior more frequently the more important the value domain was to them) or social or non-social context of the domain (research question 4a, patients would show consistent behavior more frequently if the value domain was social). Treatment setting was included in these models as an additional predictor, but not as an interaction term (research question 2). Interaction effects between importance of the domain and treatment setting (research question 3b, there would be differences between in- and outpatients with respect to the relationship between consistent behavior and the importance of the domain) and social or non-social context of the domain and treatment setting (research question 4b, there would be differences between in- and outpatients with respect to the relationship between consistent behavior and social or non-social context of the domain) were calculated in separate models. GLMMs contained a random intercept to account for the dependency among repeated measures.
Results
Overall, retained participants responded to 83.87% of queried assessments. The average importance attached to the behavior was 71.95 for inpatients and 70.13 for outpatients (on a scale from 0-100), which did not differ between groups (OR = 0.99, p = .86, 95% CI, [0.86, 1.14]). Inpatients and outpatients did not differ in terms of age (OR = 0.98, p = .86, 95% CI, [0.80, 1.20]) or sex (OR = 1.86, p = .76, 95% CI, [0.03, 96.63]). For research question 1, we compared the probabilities of each domain between the two groups. Frequencies for each domain for inpatients and outpatients can be found in Table 1. Results indicated that inpatients reported interacting with others and physical activity with significantly higher probability than outpatients. Outpatients reported Working/studying, and media usage significantly more often than inpatients. Enjoying/relaxing was rated as marginally more important for inpatients, and household was rated as marginally more important for outpatients.
Table 1.
Average probability (across the week) of participants’ most important value domain reported per 3-h time window, by in- and outpatients.
| Probability (%) |
Treatment setting (Inpatient = 1; Outpatient = 2) |
|||
|---|---|---|---|---|
| Value Domain | Inpatient | Outpatient | OR (95% CI) | p |
| Working/studying | 4.95 | 24.59 | 0.08 (0.04, 0.19) | < .00*** |
| Commute | 4.46 | 4.79 | 0.90 (0.54, 1.53) | .71 |
| Media usage | 3.50 | 5.89 | 0.55 (0.31, 0.97) | .04* |
| Interacting with family | 7.97 | 7.83 | 0.89 (0.53, 1.47) | .64 |
| Interacting with others | 25.89 | 11.05 | 3.19 (2.13, 4.77) | < .00*** |
| Being alone/bored | 2.95 | 2.12 | 1.67 (0.70, 4.01) | .25 |
| Household | 6.18 | 8.84 | 0.68 (0.42, 1.08) | .09 |
| Hobby (excluding exercise) | 5.01 | 4.05 | 0.72 (0.32, 1.62) | .43 |
| Physical activity | 7.97 | 4.60 | 2.23 (1.15, 4.34) | .01* |
| Eating/drinking | 8.92 | 7.92 | 1.11 (0.68, 1.83) | .68 |
| Enjoying/relaxing | 22.18 | 18.32 | 1.41 (0.97, 2.05) | .06 |
Note: *p < .05. **p < .01. ***p < .001; OR: Odds ratio; CI: Confidence interval. Based on n = 2542.
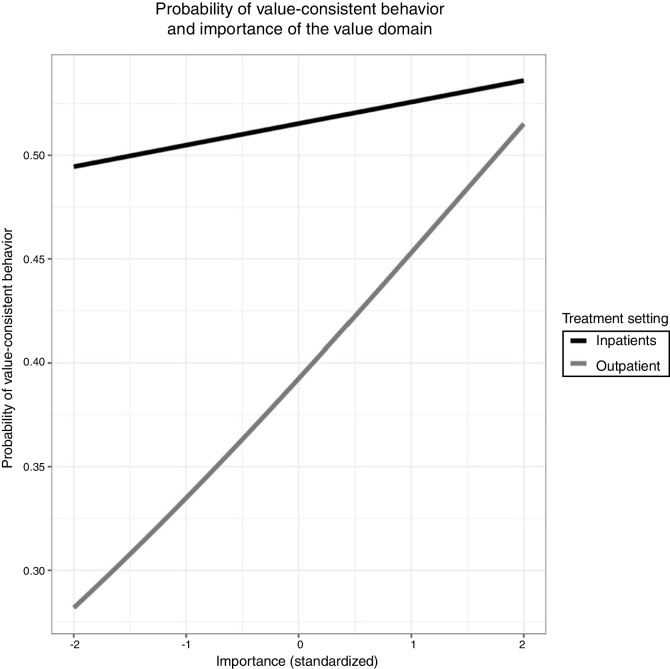
Results for research question 3a indicated that more consistent behavior was shown if the domain was judged as more important. Further, outpatients generally reported behaving more consistently than inpatients, regardless of importance (research question 2). Research question 3b showed that the interaction between importance and treatment setting (inpatients) was significant. This suggests that though for both groups the probability of consistent behavior increased if the importance of that domain increased, it did even more so for the inpatients. Results for research questions 2, 3a, and 3b can be found in Table 2 and Figure 1.
Table 2.
Values-consistent behavior as a function of importance, treatment setting, social context, and their interactions.
| Values-consistent behavior |
|||
|---|---|---|---|
| Predictors | OR (95% CI) | p | |
| RQ 2 | Tx setting | 0.61 (0.46, 0.81) | < .00*** |
| RQ 3a | Importance | 1.31 (1.10, 1.59) | .003** |
| RQ 3b | Importance x tx setting | 1.43 (1.02, 2.00) | .04* |
| RQ 4a | Non-social vs social | 1.77 (1.31, 2.39) | < .00*** |
| RQ 4b | Social vs non-social x tx setting | 0.47 (0.32, 0.71) | < .00*** |
Note: *p < .05. **p < .01. ***p < .001; tx setting: Treatment setting; OR: Odds ratio; CI: Confidence interval. RQ: Research question; RQ 2: Research question 2; RQ 2a: Research question 2a; RQ 2b: Research question 2b; RQ 3a: Research question 3a; RQ 3b: Research question 3b.
Figure 1.
Association between importance of the value domain (standardized) and probability of values-consistent behavior in the two treatment settings inpatients and outpatients.
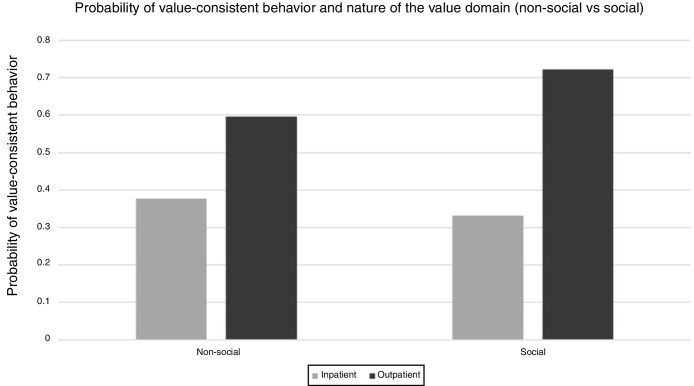
Research question 4a examined whether the patients’ consistent behavior was related to the (social vs. non-social) context of the domain. Research question 4b investigated whether the patients’ consistent behavior was related to the treatment setting, or to the interaction between social vs non-social domains and treatment setting. Results for research question 4a indicated that more consistent behavior was shown if the domain was social. Results for research question 4a suggest a significant interaction between the context of the domain and treatment setting (outpatients). This suggests that though for both groups the probability of consistent behavior increased if the domain was social, it did even more so for the outpatients. Results for research questions 4a and 4b can be found in Table 2 and Figure 2.
Figure 2.
Probability of values-consistent behavior by treatment setting (inpatients or outpatients) and context of the value domain (social vs non-social).
Discussion
This study examined the everyday life of in- and outpatients. More specifically, we examined whether the importance participants attached to an activity, and the (social or non-social) context of an activity impacted the extent to which they exhibited values-consistent behavior. The results suggest three main findings. First, in- and outpatients value different areas of life during the beginning of treatment. Second, more consistent behavior was shown in both groups the more important the domain was to the patients. Outpatients generally showed higher levels of consistent behavior than the inpatients. However, at higher levels of importance of a domain, the probability of consistent behavior increased significantly for the inpatients. Third, the context of the domain (social vs. non-social) proved to be important: The probability of consistent behavior was higher in social than in non-social domains. This was especially important for outpatients: If the domain was social, the probability of consistent behavior increased significantly for the outpatients.
Value domains and treatment setting
Several reasons may account for inpatients reporting that interacting with others, exercise, and (marginally) relaxing and enjoying their time as being important more often than outpatients. While this might reflect their real values, it might also be a function of their social context. First, inpatients experience social isolation and low social support (Ferguson et al., 2005). Thus, the possibility of interacting with others regularly in the clinic may become an essential part of their daily life. Note that inpatients reported specific importance for interacting with others, and not with family. Inpatients living in the same clinic usually spend the majority of the day together. Our result reflects that this time spent together indeed is important for inpatients – even though it does not always seem to be. Alternately, it may reflect the change in social interactions experienced when patients check in to an inpatient hospital. Second, the fact that inpatients attached more importance to exercising and enjoying/relaxing than outpatients might point to an increased awareness of the need of self-care. When inpatients neglect their self-care, this may include exercise or enjoying/relaxing. Being pulled out of one’s usual environment and placed into a new daily environment, as in an inpatient setting, may also provide patients with more opportunities to practice self-care. Alternatively, inpatients may simply not have had as many opportunities to engage in domains that outpatients considered important. This may especially be relevant for working/studying.
Outpatients, on the other hand, valued working/studying, media usage, and (marginally) household tasks more often than the inpatients. That outpatients valued working/studying more than inpatients is not altogether surprising, since these patients usually work while being in psychotherapy, while inpatients do not. Yet, it may carry significance: Possibly attaching a strong value to one’s work/school/studies is preventing outpatients from getting worse. It could be that engaging in something for more than 40 hours a week without valuing it, is the type of problem that might tip the balance from presenting for outpatient to presenting for inpatient treatment. Further, outpatients valued using media (such as TV or internet) more often than inpatients. This might have several reasons: First, 24.56% of our outpatients were diagnosed with an anxiety disorder. There is a positive association between media use and anxiety (Vannucci, Flannery, & Ohannessian, 2017) and patients suffering from Social Anxiety or Major Depressive Disorder engage significantly more often in social interactions via their phones, compared to a control group (Villanueva, Meyer, Miché et al., 2019). Thus, this high reporting of using media might be a manifestation of patients with an anxiety disorder. Second, outpatients might be using the internet to stay in touch with others. If outpatients have a lot of stressors in their life (e.g., running from A to B because of work/school/studies, running errands, doing chores etc.) using technology might facilitate social contact, both for social and practical purposes (Baecker, Sellen, Crosskey, Boscart, & Barbosa Neves, 2014). For inpatients, this need might arise less, either because of a strong focus on oneself and one’s disorder or because of social isolation. Household tasks might have been important for outpatients because they felt it needed to be done or because they derived satisfaction from getting things done. Considering the present results, clinicians might want to examine patients’ values and value domains and incorporate those into the clinical work. Working on the patients’ personal and deeply held values might increase the patients’ motivation for therapy and aid them to lead a more fulfilling life (Hayes et al., 2006).
Being consistent when things get important
In this study, outpatients generally reported behaving more consistent than inpatients (regardless of importance). For inpatients, increased consistent behavior was related to an increase in the importance of the domain. One reason for these relationships might be that, possibly due to more severe symptoms, inpatients focus more strongly on some behaviors, which might not include values-consistent ones. More severe symptoms might in fact hinder patients from even knowing what is important to them, let alone behaving consistently to values. Clinicians might want to consider investigating patients’ values and find the ones that are most important, especially with inpatients. Increasing valued behaviors has been shown to precede reduction in suffering (Gloster et al., 2017). Attempting to increase values-consistent behavior could initially be focused on those most important values first to reduce suffering more efficiently.
Being consistent when things get social
Consistent with our expectations, social domains were associated with more consistent behavior across both groups. For the outpatients, social domains were associated with increased consistent behavior. This is consistent with previous cross-sectional research, which found patients’ valued behaviors in social domains to be judged as more important and more valued than in non-social domains (Wersebe et al., 2017). The present result based on fine-grained ESM data collected every three hours extends this finding into patients’ everyday lives. The replicability of the importance of social domains across data sets and data collection methods suggests a salient target for research and therapy.
The positive association between consistent behavior and social domains found in outpatients might have several reasons: First, outpatients tend to have more social contact than inpatients (Ferguson et al., 2005), and therefore more opportunities to experience social domains as important. Due to possibly less severe symptoms they might also have more opportunities to behave in consistency with their values. Second, in order to be considered a functioning individual in today’s society, some participation in social life is usually expected. Thus, social desirability (i.e., a tendency to respond in a way that corresponds with current social norms and standards; Perinelli & Gremigni, 2016) might render social domains more important to outpatients. Third, outpatients might be able to better differentiate what is important to them than inpatients. Additionally, as an outpatient, one may also simply have more capacity for social matters. Clinicians might want to examine patients’ values and find the ones that are embedded in a social context. Initially focusing on social domains can possibly increase values-consistent behavior in outpatients, which in turn might aid to reduce suffering (Gloster et al., 2017). Our results further underscore the importance of group therapy. Group therapy has been shown to be an effective approach for treatment, with patients reporting to be satisfied with the treatment (e.g., Weck, Gropalis, Hiller, & Bleichhardt, 2015), and treatment effects persisting or improving over a 12-month follow-up (Weck et al., 2015). Our results suggest that social value domains were associated with more behavior that is consistent to what one values, and it is possible that this association may underlie treatment satisfaction and persistence of treatment effects. Our results also suggest transdiagnostic relevance, similar to unwanted mental intrusions, which were shown to be of importance cross-culturally and transdiagnostically (Pascual-Vera et al., 2019). This makes the group setting an even more effective approach, since it can possibly be implemented across different diagnoses.
Limitations
The present study had four main limitations. First, ESM is a self-report measure and as such relies on reports of participants, rather than observations of participants. However, it is considered the current gold standard for data collection in people’s daily life, and due to the fine-grained information captured is considered a more accurate measure of real-life behavior than questionnaires alone (Myin-Germeys et al., 2018). Second, categorizing value domains into social vs non-social is complex, because some domains might be social in some cases and non-social in others. For instance, working could happen both in a social or in a non-social context, depending on the job itself, the participant’s position within a company or institution, and the company or institution itself (e.g. somebody who works predominantly alone in a library vs somebody who works predominantly in interaction with others as a waiter in a restaurant). Eating/drinking, hobby, physical activity, and enjoying/relaxing might for some people happen more often in the presence of other people while others prefer to do these things alone, thus, for them they happen in a more non-social context. Future research might consider adding more items so participants categorize behaviors into social and non-social themselves, and items to investigate what factors determine whether behavior happens in a social or non-social context. Nonetheless, because the previous categorization of a valued behavior into one of eleven general categories was done by the patients themselves, we can still more accurately depict the experience of patients in their everyday naturalistic environment, than if we had categorized the behaviors. Third, participants reported on what was important to them and what will be important to them. Yet, we could not verify that they actually did what they reported. To verify whether consistent behavior was really carried out, future research must establish a verification process that considers participants’ personal privacy. Fourth, although the overarching study collected variables with the intent to examine values, behavioral consistency, and social context in a transdiagnostic group of patients, the patients were not randomized across the exploratory research questions. As such, appropriate caution should be made in the interpretation of the results.
Conclusion
This study provides new insights into the everyday life of in- and outpatients, their values, how important daily social interactions are to them, and what contributes to values-consistent behavior. To our knowledge, this is the first study to investigate these aspects in a sample of transdiagnostic in- and outpatients, using state-of-the-art ESM. Clinical implications of this study include closer examination of patients’ values: Especially important and social domains might merit special consideration by the clinician. Focusing on these in clinical work might increase patients’ values-consistent behavior, which might be followed by a reduction in suffering (Gloster et al., 2017) and enabling the patients to lead a more fulfilling life. Overall, this study adds to the current knowledge of how the daily life of in- and outpatients might contribute to mechanisms that maintain or alleviate their suffering.
Acknowledgments
We thank Jannis Behr, Christine Bratschi, Silvio Deplazes, Maria Dickson, Nadine Farronato, Julia Fricker, Vanya Gocheva, Peter Haag, Philip Hinüber, Eveline Hug, Lea Jenny, Dennis Koroma, Katrin Meier, Andrea Neuckel, Christine Oehler, Katrin Pinhard, Suna Polat, Ken Rohr, Sara Schmid, Katrin Schudel, Isabell Schumann, Stefanie Urech, Andrea Vitt, and Janina Weber, who supported us in their role as therapists, and Kristina Domonell, Claudia Gassmann, Lorenz Gschwind, Manuel Jahwari, Elisabeth Jufer, Veronika Kuhweide, Patrick Rytz, Rolf Salathé-Buser who supported us in their role as nurses. We further thank Judith Alder, Barbara Annen, Herbert Assaloni, Thomas Eugster, Silvia Hatebur, Jan Martz, Mirjam Tanner, and Michael Waadt, who helped us assess therapy integrity in their role as ACT experts. Further, we also thank Vanessa Aeschbach, Lukas Bosse, Doreen Eckhardt, and Elena Pauli for their help with the data preparation and data processing. Finally, we wish to thank Denise Berger, Zelda Bernardi, Juliane Burbach, Martina Christen, Sabrina Doering, Pranvera Islami, Eliane Knörr, Sarah Kuhn, Stefanie Litschi, Silvia Mangada, Johannes Massell, Manuel Massell, Andrea Schumacher, Raphael Schwaier, Fenna Vogel, Tobias Voll, Noemi Walder, Eva Weinzierl, Hannah Zimmermann, and Sascha Zimmermann for their help with the data collection, and Fabio Coviello, Ruben Meyer, Moritz Mücke, and Nicolas Scharowski for their help in administering the heat induction test. This research was funded by the Swiss National Science Foundation (grant number PP00P1_163716/1).
References
- American Psychiatric Association . 4th ed. American Psychological Association; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Baecker R., Sellen K., Crosskey S., Boscart V., Barbosa Neves B. Proceedings of the 16th International ACM SIGACCESS Conference on Computers & Accessibility. 2014. Technology to Reduce Social Isolation and Loneliness Technology to Reduce Social Isolation and Loneliness. [DOI] [Google Scholar]
- Brown T.A., DiNardo P.A., Barlow D.H. Anxiety Disorders Interview Schedule for DSM-IV: Client Interview Schedule. adult vers. Graywind Publications Incorporated; 1994. Diagnosis; p. 77. [Google Scholar]
- Campos Andrade C., Lima M.L., Pereira C.R., Fornara F., Bonaiuto M. Inpatients’ and outpatients’ satisfaction: The mediating role of perceived quality of physical and social environment. Health and Place. 2013;21:122–132. doi: 10.1016/j.healthplace.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Čolić J., Bassett T.R., Latysheva A., Bader K., Hatzinger M., Mikoteit T., Lieb R., Gloster A., Hoyer J. Depersonalization and derealization in embarrassing social interactions: An experience sampling study in social phobia, major depression and controls. Depression and Anxiety. 2020 doi: 10.1016/j.janxdis.2020.102189. Advanced Online Publication. 10/1016/janxdis.2020.102189. [DOI] [PubMed] [Google Scholar]
- DeFife J., Westen D. Empirically-informed clinical interviewing for personality disorders. In: Levy R., Ablon J., Kachele H., editors. Psychodynamic psychotherapy research: Evidence-based practice and practice-based evidence. Springer; New York, NY: 2012. pp. 553–569. [DOI] [Google Scholar]
- Ferguson C.J., Averill P.M., Rhoades H., Rocha D., Gruber N.P., Gummattira P. Social isolation, impulsivity and depression as predictors of aggression in a psychiatric inpatient population. Psychiatric Quarterly. 2005;76:123–137. doi: 10.1007/s11089-005-2335-1. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Klotsche J., Ciarrochi J., Eifert G., Sonntag R., Wittchen H.U., Hoyer J. Increasing valued behaviors precedes reduction in suffering: Findings from a randomized controlled trial using ACT. Behaviour Research and Therapy. 2017;91:64–71. doi: 10.1016/j.brat.2017.01.013. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Richard D.C.S., Himle J., Koch E., Anson H., Lokers L., Thornton J. Accuracy of retrospective memory and covariation estimation in patients with obsessive-compulsive disorder. Behaviour Research and Therapy. 2008;46:642–655. doi: 10.1016/j.brat.2008.02.010. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Sonntag R., Hoyer J., Meyer A.H., Heinze S., Ströhle A., Eifert G., Wittchen H.U. Treating treatment-resistant patients with panic disorder and agoraphobia using psychotherapy: A randomized controlled switching trial. Psychotherapy and Psychosomatics. 2015;84:100–109. doi: 10.1159/000370162. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hoyer J., Čolić J., Grübler G., Gloster A.T. Valued Living Before and After CBT. Journal of Contemporary Psychotherapy. 2019 doi: 10.1007/s10879-019-09430-x. [DOI] [Google Scholar]
- Ivanoff A., Jang S.J., Smyth N.J., Linehan M.M. Fewer reasons for staying alive when you are thinking of killing yourself: The brief reasons for living inventory. Journal of Psychopathology and Behavioral Assessment. 1994;16:1–13. doi: 10.1007/BF02229062. [DOI] [Google Scholar]
- Keller M.C., Nesse R.M. The evolutionary significance of depressive symptoms: Different adverse situations lead to different depressive symptom patterns. Journal of Personality and Social Psychology. 2006;91:316–330. doi: 10.1037/0022-3514.91.2.316. [DOI] [PubMed] [Google Scholar]
- Kupferberg A., Bicks L., Hasler G. Social functioning in major depressive disorder. Neuroscience and Biobehavioral Reviews. 2016;69:313–332. doi: 10.1016/j.neubiorev.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Lobbestael J., Leurgans M., Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology and Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- McCracken L.M., Chilcot J., Norton S. Further development in the assessment of psychological flexibility: A shortened Committed Action Questionnaire (CAQ-8) European Journal of Pain (United Kingdom) 2015;19:677–685. doi: 10.1002/ejp.589. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I., Kasanova Z., Vaessen T., Vachon H., Kirtley O., Viechtbauer W., Reininghaus U. Experience sampling methodology in mental health research: new insights and technical developments. World Psychiatry. 2018;17:123–132. doi: 10.1002/wps.20513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen G., Wikman J.M., Jensen C.J., Schmidt J.F., Gliemann L., Andersen T.R. Health promotion: The impact of beliefs of health benefits, social relations and enjoyment on exercise continuation. Scandinavian Journal of Medicine and Science in Sports. 2014;24(SUPPL.1):66–75. doi: 10.1111/sms.12275. [DOI] [PubMed] [Google Scholar]
- Pascual-Vera B., Akin B., Belloch A., Bottesi G., Clark D.A., Doron G., Fernández-Alvarez H., Ghisi M., Gómez B., Inozu M., Jiménez-Ros A., Moulding R., Ruiz M.A., Shams G., Sica C. The cross-cultural and transdiagnostic nature of unwanted mental intrusions. International Journal of Clinical and Health Psychology. 2019;19:85–96. doi: 10.1016/j.ijchp.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perinelli E., Gremigni P. Use of Social Desirability Scales in Clinical Psychology: A Systematic Review. Journal of Clinical Psychology. 2016;72:534–551. doi: 10.1002/jclp.22284. [DOI] [PubMed] [Google Scholar]
- Rinner M.T.B., Meyer A.H., Mikoteit T., Hoyer J., Imboden C., Hatzinger M., Bader K., Lieb R., Miché M., Wersebe H., Gloster A.T. General or specific? The memory–experience gap for individuals diagnosed with a major depressive disorder or a social phobia diagnosis, and individuals without such diagnoses. Memory. 2019;27:1194–12003. doi: 10.1080/09658211.2019.1640252. [DOI] [PubMed] [Google Scholar]
- Rubin M., Stuart R. Kill or cure? Different types of social class identification amplify and buffer the relation between social class and mental health. Journal of Social Psychology. 2018;158:236–251. doi: 10.1080/00224545.2017.1327405. [DOI] [PubMed] [Google Scholar]
- Trompenaars F.J., Masthoff E.D., Van Heck G.L., Hodiamont P.P., De Vries J. Content validity, construct validity, and reliability of the WHOQOL-Bref in a population of Dutch adult psychiatric outpatients. Quality of Life Research. 2005;14:151–160. doi: 10.1007/s11136-004-0787-x. [DOI] [PubMed] [Google Scholar]
- Vannucci A., Flannery K.M., Ohannessian C.M.C. Social media use and anxiety in emerging adults. Journal of Affective Disorders. 2017;207(July 2016):163–166. doi: 10.1016/j.jad.2016.08.040. [DOI] [PubMed] [Google Scholar]
- Villanueva J., Meyer A.H., Miché M., Wersebe H., Mikoteit T., Hoyer J., Imbsoden C., Bader K., Hatzinger M., Lieb R., Gloster A.T. Social Interaction in Depression, Social Phobia, and Controls: The Importance of Affect. Journal of Technology in Behavioral Science. 2019:1–10. doi: 10.1007/s41347-019-00121-x. [DOI] [Google Scholar]
- Villanueva J., Meyer A.H., Rinner M.T.B., Firsching V.J., Benoy C., Brogli S., Walter M., Bader K., Gloster A.T. “Choose Change”: Design and Methods of an Acceptance and Commitment Therapy Effectiveness Trial for Transdiagnostic Treatment-Resistant Patients. BMC Psychiatry. 2019;19:1–12. doi: 10.1186/s12888-019-2109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weck F., Gropalis M., Hiller W., Bleichhardt G. Effectiveness of cognitive-behavioral group therapy for patients with hypochondriasis (health anxiety) Journal of Anxiety Disorders. 2015;30:1–7. doi: 10.1016/j.janxdis.2014.12.012. [DOI] [PubMed] [Google Scholar]
- Wersebe H., Lieb R., Meyer A.H., Hofer P., Gloster A.T. The link between stress, well-being, and psychological flexibility during an Acceptance and Commitment Therapy self-help intervention. International Journal of Clinical and Health Psychology. 2018;18:60–68. doi: 10.1016/j.ijchp.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wersebe H., Lieb R., Meyer A.H., Hoyer J., Wittchen H.U., Gloster A.T. Changes of valued behaviors and functioning during an Acceptance and Commitment Therapy Intervention. Journal of Contextual Behavioral Science. 2017;6:63–70. doi: 10.1016/j.jcbs.2016.11.005. [DOI] [Google Scholar]
- Wilson K.G., Sandoz E.K., Kitchens J., Roberts M. The valued living questionnaire: Defining and measuring valued action within a behavioral framework. Psychological Record. 2010;60:249–272. doi: 10.1007/BF03395706. [DOI] [Google Scholar]
- Wittchen H.-U., Wunderlich U., Gruschwitz S., Zaudig M. Hogrefe; Göttingen: 1997. Strukturiertes klinisches Interview für DSM-IV, Achse-I (SKID) [Google Scholar]