Abstract
The paper is based on the data from 92 males less than 45 years of age who underwent coronary angiography at Goa Medical College during the period July 2018 to February 2019. The objectives include to estimate the prevalence of erectile dysfunction (ED) and its risk factors, and to evaluate the pattern of coronary artery disease (CAD) among these patients. The ED prevalence was 46.2%. Diabetes, hypertension and alcohol intake showed significant association with ED; and these patients were almost three more likely to have a coronary blockade compared to those not reporting ED. This concurrence between ED and CAD makes a strong ground for routine inquiry in sexual history of young males with one or more cardiovascular risk factors.
Keywords: Erectile dysfunction, Coronary artery disease, Prevalence, Patterns
1. Introduction
Erectile dysfunction (ED) and coronary artery disease (CAD) share a common pool of risk factors.1, 2, 3 Atherosclerosis, inflammation and endothelial dysfunction mark the pathophysiological cascade that underlies these disorders. Patients with ED tend to have a severe CAD with multiple vessel involvement compared to those without ED.1,4,5 Given the fact that ED precedes the clinical presentation of CAD, routine enquiry in this aspect of the personal history of a young male with one or more conventional cardiovascular (CV) risk factors could aid in early diagnosis of CAD. This paper is based on the data from the patients who underwent coronary angiography (CAG) in Goa Medical College Hospital and aims to estimate the prevalence of ED and its risk factors, and to correlate ED with the severity of CAD based on the number of vessels involved.
2. Materials and methods
An observational descriptive study was launched in July 2018 at the Department of Cardiology, Goa Medical College Hospital, to study the sociodemographic, clinical and laboratory correlates of the patients undergoing CAG. Till February 2019, 972 patients were worked up, 92 of which were males aged less than 45 years. The data pertaining to these 92 patients was analysed in fulfilment of the objectives of this research paper. The patients were explained about how cardiovascular disease (CVD) and ED shared a common pool of risk factors and the role of ED as a surrogate marker for the extent of vascular damage/endothelial dysfunction. The patients were explained that ED was not uncommon among young males with conventional CVD risk factors, and having built a rapport with the patient to open up on the sensitive topic a direct question was put—“Do you get a penile erection sufficient to enjoy sexual intercourse to your satisfaction?” The answer to this question was taken as Yes or No on most of the occasions in previous 6 months to, respectively, indicate the absence or presence of ED in the patient. The outcome of CAG was categorized as normal, that is, blockage not necessitating a coronary intervention; single vessel disease (SVD); double vessel disease (DVD) and triple vessel disease (TVD).
The data were entered and analysed in SPSS for windows, version 22. The percentages were calculated and compared using the chi-square test (χ2) of significant difference in proportion at 95% confidence interval (CI) level.
3. Results
3.1. Prevalence of ED and its risk factors (Table 1)
Table 1.
Sociodemographic and clinical correlates of ED.
| ED (Erectile dysfunction) | N | ED + (%) | χ2 | p |
|---|---|---|---|---|
| Age group (years) | ||||
| 31–35 | 9 | 5 (55.6%) | 1.205 | 0.547 |
| 36–40 | 39 | 20 (51.3%) | ||
| 41–45 | 44 | 18 (40.9%) | ||
| Education | ||||
| Illiterate | 4 | 4 (100%) | 6.874 | 0.076 |
| Primary | 4 | 2 (50%) | ||
| Up to tenth | 46 | 17 (37%) | ||
| Graduate | 38 | 20 (52.6%) | ||
| DM | ||||
| Present | 26 | 17 (65.4%) | 5.061 | 0.024 |
| Absent | 66 | 26 (39.4%) | ||
| Duration of DM (years) | ||||
| 1–5 | 16 | 8 (50%) | 2.76 | 0.09 |
| 6–10 | 10 | 9 (87.5%) | ||
| HT | ||||
| Present | 38 | 23 (60.5%) | 4.94 | 0.02 |
| Absent | 54 | 20 (37%) | ||
| Duration of HT (years) | ||||
| 1–5 | 28 | 15 (53.6%) | 2.15 | 0.14 |
| 6–10 | 10 | 8 (80%) | ||
| Dyslipidaemia | ||||
| Present | 26 | 15 (57.7%) | 1.747 | 0.186 |
| Absent | 66 | 28 (42.4%) | ||
| Tobacco | ||||
| Yes | 16 | 11 (68.7%) | 3.77 | 0.052 |
| No | 76 | 32 (42.1%) | ||
| Alcohol | ||||
| Yes | 30 | 20 (66.7%) | 7.101 | 0.007 |
| No | 62 | 23 (46.8%) | ||
| BMI | ||||
| Underweight | 6 | 1 (16.7%) | 2.411 | 0.492 |
| Normal | 32 | 15 (46.9%) | ||
| Overweight | 14 | 7 (50%) | ||
| Obese | 40 | 20 (50%) | ||
BMI = body mass index. All values less than 0.05 in the last column are statistically significant, and represented in bold.
Prevalence of ED was 46.2% (43 of 92). Diabetes mellitus (DM), Hypertension (HT) and alcohol consumption were significantly associated with the presence of ED.
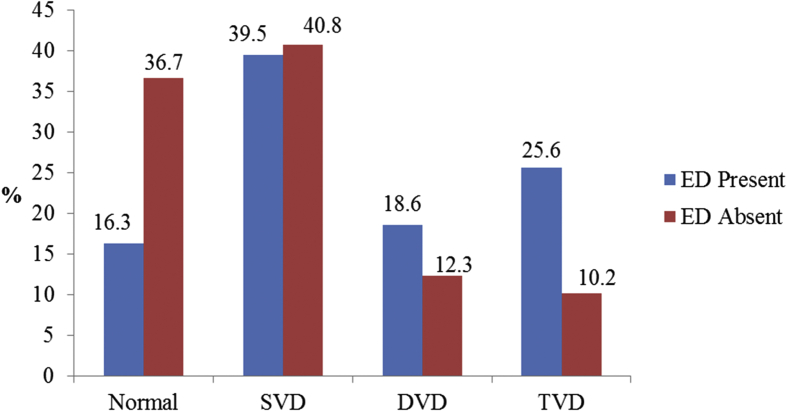
3.2. Patterns of CAD (Fig. 1)
Fig. 1.
Patterns of CAD among the patients with/without ED.
Those with ED were 2.98 times (1.1–8.08) more likely to have an adverse outcome on CAG compared to those not reporting ED. The prevalence of DVD and TVD was higher among the patients reporting ED as compared to those not reporting ED, but the figures just fell short of statistical significance (χ2 = 7.2585, p = 0.064).
3.3. Doctor–patient dialogue on ED
Only 11.6% (5 of 43) had reported the matter to their treating doctor, and in none of the instances was there a primary inquiry about the condition from the medical care provider. Embarrassment was the universally cited reason for not opening up the topic with their doctor. Although 44.1% (19 of 43) resorted to over the counter phosphodiesterase inhibitor (PDEI) treatment as and when required, 11.6% (5 of 43) used PDEI recommended by their medical care provider, and 30.2% (13 of 43) resorted to traditional healers and AYUSH (Ayurveda, Yoga & Naturopahy, Unani, Siddha and Homeopathy) practitioners for relief.
4. Discussion
We used the single question–based diagnosis of self-reported ED in our study, as advocated by O'Donnell et al6 for research studies. Our study population composed of young males with one or more conventional CV risk factors, thereby accounting for the prevalence estimate of 46.2%. Similar studies in India4 and abroad7 have estimated comparative figures to be 50–70%, the eligible patients being all males without an age bar thus accounting for higher prevalence of ED. None of the study subjects had any history of previous coronary intervention or IHD.
The proportion did not differ significantly across the sociodemographic variables (Table 1). DM and HT seemed to be significantly associated with ED (Table 1), the respective odds ratio (OR) being 2.906 (1.127–7.491) and 2.61 (1.11–6.12), and the prevalence of ED further increased with the duration of DM and HT. The patients reporting ED had a higher average fasting and random blood sugar levels, HbA1c level, systolic blood pressure and diastolic blood pressure levels, but the sample size constrained the statistical significance. No statistically significant link could be deduced between dyslipidaemia and ED. All the patients with dyslipidaemia were already on statin therapy, and reaped the benefits of its pleiotropic effects. Use of alcohol (Table 1) beyond the acceptable limit was significantly associated with ED compared to its use in acceptable limits or no use (OR = 3.39; 95% CI 1.35–8.49). Alcohol in small amounts improves erection and increases libido because of its vasodilatory effect and anxiety suppression; however, its long-term use can cause hypogonadism and polyneuropathy leading to sexual dysfunction.8 Use of tobacco (Table 1), although seemed to be associated, failed to demonstrate a statistically significant relationship with ED (p = 0.052). An adverse effect of tobacco on erectile function is well documented in medical literature, and is predominantly mediated through smoke-induced inhibition of neuronal and endothelial nitric oxide synthase (NOS), damage to the vascular endothelium, and impaired NOS-mediated vasodilation.9
The patterns of CAD differed among these patients based on the presence or absence of ED (Fig. 1). The prevalence of CAD among those with ED and without ED was, respectively, 83.7% and 63.3% (p = 0.056). Half of the CAG-documented CAD patients in our study had ED, whereas 35% of the non-CAD patients reported an ED. This is lower than the ED prevalence of 88.5% and 64.2% in CAD and non-CAD patients as estimated by Salem et al.10 The difference in prevalence could be attributed to the relatively younger age group in our study, as explained before. Patients with ED were almost three times more likely (OR = 2.98; 1.1–3.08) to have coronary vessel blockade involving at least one coronary compared to the non-ED patients. A similar study by Greenstein et al.5 estimated that of the 40 men who underwent CAG, 37.5% had an SVD, 20% had a DVD and 42.5% had a TVD; the comparative figures in our study being 39.5%,18.6% and 25.6%, respectively. It may be noted that the average age of the study participants in Greenstein's study was 56.6 years (SD 1.3), whereas in our study it was 39.91 years (SD 20.9); and the study by Greenstein et al. did not have a normal coronaries category.
Physician inertia in proactive routine enquiry into the sexual history of patients surfaced up once again through this study. Despite there being a conclusive evidence linking ED with endothelial dysfunction—penis, the barometer of endothelial health as it was pronounced by McCollough11—the routine questioning on this aspect does not seem to happen in clinical settings. As many as 62% of the primary care physicians in Nigeria would not elicit a sexual history unless the patient brought it up,12 and in our study, this percentage was nil.
5. Conclusion
This is one of the very few studies in India, which correlates ED with angiographically substantiated CAD, not just the risk factors for CAD. Restriction of study population age group to less than 45 years resulted in a limited sample size. However, considering the aim of the study—to evaluate ED as a predictor of otherwise silent CVDs—with the intention to encourage medical care providers to proactively seek history of ED to facilitate screening (early identification) of those at risk of CVDs, restriction of the age group to less than 45 years was thought to be more specific and relevant. Increasing burden of CVDs, high concurrence of ED and CAD, and a common pool of risk factors for both (ED and CAD) makes a strong case in support of the routine inquiry about ED in young males with one or more CV risk factors.
Funding
The study did not involve any external source of funding.
Ethical permission
The data used for the paper were extracted from the parent study on clinicosocial and laboratory characteristics of patients undergoing CAG at the Department of Cardiology, GMCH, which was approved by the Institutional Ethics Committee of Goa Medical College, Bambolim, Goa.
Declaration of competing interest
All authors have none to declare.
References
- 1.Sai Ravi Shanker A., Phanikrishna B., Bhakathavatsala Reddy C. Association between erectile dysfunction and coronary artery disease and it’s severity. Indian Heart J. 2013 Mar;65(2):180–186. doi: 10.1016/j.ihj.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langer R., Sharma E., Langer B., Gupta R.K., Kumari R., Majeed M. Erectile dysfunction: prevalence and determinants among T2DM men attending a tertiary care hospital in northern India. Int Surg J. 2019;6(4):1115–1119. [Google Scholar]
- 3.Ugwumba F.O., Okafor C.I., Nnabugw Prevalence of, and risk factors for erectile dysfunction in male type 2 diabetic outpatient attendees in Enugu, South East Nigeria. Ann Afr Med. 2018;17(4):215–220. doi: 10.4103/aam.aam_3_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar J., Bhatia T., Kapoor A. Erectile dysfunction precedes and is associated with severity of coronary artery disease among Asian Indians. J Sex Med. 2013;10(5):1372–1379. doi: 10.1111/jsm.12041. [DOI] [PubMed] [Google Scholar]
- 5.Greenstein A., Chen J., Miller H., Matzkin H., Villa Y., Braf Z. Does severity of ischemic coronary disease correlate with erectile function? Int J Impot Res. 1997;9(3):123–126. doi: 10.1038/sj.ijir.3900282. [DOI] [PubMed] [Google Scholar]
- 6.O'Donnell A.B., Araujo A.B., Goldstein I., McKinlayJB The validity of a single-question self-report of erectile dysfunction-results from the Massachusetts male aging study. J Gen Intern Med. 2005;20(6):515–519. doi: 10.1111/j.1525-1497.2005.0076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jackson G., Montorsi P., Adams M.A. Cardiovascular aspects of sexual medicine. J Sex Med. 2010;7(4):1608–1626. doi: 10.1111/j.1743-6109.2010.01779.x. [DOI] [PubMed] [Google Scholar]
- 8.Prabhakaran D.K., Nisha A., Varghese P.J. Prevalence and correlates of sexual dysfunction in male patients with alcohol dependence syndrome: a cross-sectional study. Indian J Psychiatr. 2018;60(1):71–77. doi: 10.4103/psychiatry.IndianJPsychiatry_42_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kovac J.R., Labbate C., Ramasamy R., Tang D., Lipshultz L.I. Effects of cigarette smoking on erectile dysfunction. Andrologia. 2015;47(10):1087–1092. doi: 10.1111/and.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salem S., Abdi S., Mehrsai A. Erectile dysfunction severity as a risk predictor for coronary artery disease. J Sex Med. 2009;6(12):3425–3432. doi: 10.1111/j.1743-6109.2009.01515.x. [DOI] [PubMed] [Google Scholar]
- 11.McCullough A.R. The penis as a barometer of endothelial health. RevUrol. 2003;5(Suppl.7):S3–S8. [PMC free article] [PubMed] [Google Scholar]
- 12.Ariba A.J., Oladapo O.T., Iyaniwura C.A., Dada O.A. Management of erectile dysfunction: perceptions and practices of Nigerian primary care clinicians. S Afr Fam Pract. 2007;49(9):16. [Google Scholar]