Coronavirus disease 2019 (COVID-19), primarily affecting respiratory systems, has become pandemic and spread worldwide. Acute kidney injury (AKI) has been reported as a severe complication of COVID-19 with a higher risk of mortality [1], but the incidence of AKI among those infected with COVID-19 is currently only based on reports from small case series and retrospective studies [2, 3]. Therefore, in this work, we aim to perform a systematic review and meta-analysis of published articles to quantify the incidence of AKI in COVID-19 patients.
We performed a systematic search via PUBMED and EMBASE using the keywords “COVID-19” and “acute kidney injury” to identify relevant observational studies, such as case series and cohort studies published between 2019 and May 11, 2020. We also manually examined the reference lists of included studies and reviewed the AKI reports in epidemiological features and clinical courses of COVID-19 patients in high-profile general medicine journals (e.g., BMJ, JAMA, Lancet, and NEJM). Two independent reviewers (YTC and SCS) assessed articles, including title, abstract, and full text to determine whether studies were eligible for inclusion. In cases of divergences, results were discussed with a third reviewer (YCC). All statistical analyses were performed using MedCalc for Windows, version 15.0 (MedCalc Software, Ostend, Belgium). The incidence of AKI is expressed as proportion and 95% confidence interval (CI) using the random effects model and presented as a forest plot. We used the Cochran Q test to detect heterogeneity among studies, with a p value < 0.10 indicating significant heterogeneity. We calculated I2 statistic to measure the proportion of total variation in study estimates attributed to heterogeneity.
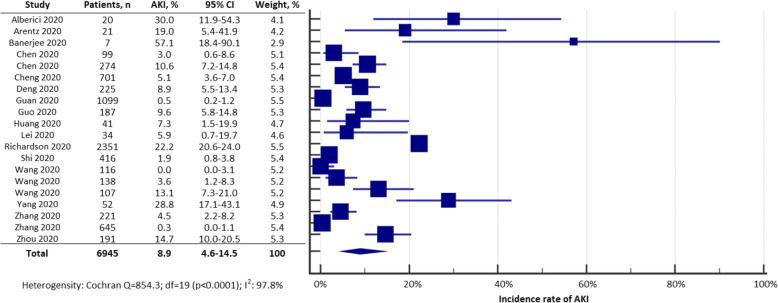
Of 65 articles screened, we excluded 45: 7 studies were duplicates, 8 studies were irrelevant, 9 studies failed to report the number of patients in the study cohort, and 21 studies did not report AKI data. Our final analysis included 20 articles comprising 6945 patients from China, Italy, the UK, and the USA. Demographic data for the included articles are summarized in Table 1. Notably, most of the studies (80%) were reported from China. We found the incidence of AKI was 8.9% (95% CI 4.6–14.5) in COVID-19 patients, but there was evidence of statistical heterogeneity among the studies with I2 = 97.8% and p < 0.001 (Fig. 1).
Table 1.
Study characteristics
| Author and year | City/country | Male (%) | Age (median)* | Settings | Patients with kidney transplantation (%) | Mechanical ventilation (%) | RRT (%) | ARDS (%) | Overall mortality (%) |
|---|---|---|---|---|---|---|---|---|---|
| Alberici 2020 [4] | Brescia/Italy | 80 | 59 | Hospitalization | 100 | 10 | 5 | 55 | 25 |
| Arentz 2020 [5] | Washington/USA | 52 | 70 | ICU | NR | 71 | NR | 95 | 52 |
| Banerjee 2020 [6] | London/UK | 57 | 54 | Hospitalization | 100 | 29 | 43 | 29 | 14 |
| Chen 2020 [7] | Wuhan/China | 68 | 56 | Hospitalization | NR | 4 | 9 | 17 | 11 |
| Chen 2020 [8] | Wuhan/China | 62 | 62 | Hospitalization | NR | 6 | 1 | 72 | 41 |
| Cheng 2020 [9] | Wuhan/China | 52 | 63 | Hospitalization | NR | 14 | NR | NR | 16 |
| Deng 2020 [10] | Wuhan/China | 55 | 54 | Hospitalization | NR | 9 | NR | 48 | 48 |
| Guan 2020 [11] | Wuhan/China | 58 | 47 | Hospitalization | NR | 2 | 1 | 3 | 1 |
| Guo 2020 [12] | Wuhan/China | 49 | 59 | Hospitalization | NR | 24 | NR | 25 | 23 |
| Huang 2020 [13] | Wuhan/China | 73 | 49 | Hospitalization | NR | 10 | 7 | 29 | 15 |
| Lei 2020 [14] | Wuhan/China | 41 | 55 | Hospitalization | NR | 15 | 3 | 32 | 21 |
| Richardson 2020 [15] | New York/USA | 60 | 63 | Hospitalization | NR | 12 | 3 | NR | 21 |
| Shi 2020 [16] | Wuhan/China | 49 | 64 | Hospitalization | NR | 8 | 1 | 23 | 14 |
| Wang 2020 [17] | Wuhan/China | 58 | 54 | Hospitalization | NR | NR | NR | 10 | 6 |
| Wang 2020 [18] | Wuhan/China | 54 | 56 | Hospitalization | NR | 12 | 1 | 20 | 4 |
| Wang 2020 [19] | Wuhan/China | 53 | 51 | Hospitalization | NR | 19 | NR | 26 | 18 |
| Yang 2020 [20] | Wuhan/China | 67 | 60 | ICU | NR | 42 | 17 | 67 | 62 |
| Zhang 2020 [21] | Wuhan/China | 49 | 55 | Hospitalization | NR | 12 | 2 | 22 | 5 |
| Zhang 2020 [22] | Zhejiang/China | 51 | 45 | Hospitalization | NR | 1 | 0 | 2 | NR |
| Zhou 2020 [23] | Wuhan/China | 62 | 56 | Hospitalization | NR | 17 | 5 | 31 | 28 |
*In studies not reporting the median, age would be represented by the mean
ARDS acute respiratory distress syndrome, ICU intensive care unit, NR not reported, RRT renal replacement therapy
Fig. 1.
Forest plot of pooled incidence of AKI in COVID-19 patients from included studies
Previous studies reported the incidence of AKI largely from small case series or cohorts of COVID-19 patients, but our findings indicated that nearly 9 out of 100 developed AKI among a total of 6945 COVID-19 patients. This was close to the incidence rate of AKI in patients with community-acquired pneumonia [24].
Several mechanisms are possible for AKI in COVID-19 patients, including multi-organ dysfunction syndrome, SARS-CoV-2 direct kidney infection [25], AKI following acute respiratory distress syndrome (ARDS), infection-related generalized mitochondrial failure, and cytokine storm syndrome. Early recognition and treatment of AKI may limit associated complications such as long-term chronic kidney disease or end-stage kidney disease [26].
This study has several limitations. First, since the majority of included studies came from China and the USA, the generalizability of our findings into other countries may be limited. Second, clinical heterogeneity between studies should be noted, whereby detailed information on patient characteristics was lacking in the published articles. For example, two studies included patients post kidney transplantation, and the reported incidences of AKI were higher than in other studies which lacked information on how many patients had had kidney transplantation. With the disease burden of COVID-19 still increasing every day, we hope our synthesis can raise clinical awareness, early recognition, and intervention for AKI in patients hospitalized with COVID-19 for first-line healthcare providers.
Acknowledgements
None.
Abbreviations
- AKI
Acute kidney injury
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
Authors’ contributions
YCY and SCS contributed equally to this work. YCY and SCS: critical analysis, interpretation of the data, and drafting of the manuscript. MJH and YCC: study supervision and administrative, technical, or material support. The authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
This original article has not been published and under consideration by another journal.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yih-Ting Chen and Shih-Chieh Shao contributed equally to this work.
References
- 1.Ali H, Daoud A, Mohamed MM, Salim SA, Yessayan L, Baharani J, Murtaza A, Rao V, Soliman KM. Survival rate in acute kidney injury superimposed COVID-19 patients: a systematic review and meta-analysis. Ren Fail. 2020;42(1):393–397. doi: 10.1080/0886022X.2020.1756323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ronco C, Reis T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat Rev Nephrol. 2020;16(6):308–310. doi: 10.1038/s41581-020-0284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97(5):824–828. doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, Pola A, Maffei C, Possenti S, Zambetti N, Moscato M, et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97(6):1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323(16):1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banerjee D, Popoola J, Shah S, Ster IC, Quan V, Phanish M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97(6):1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deng Y, Liu W, Liu K, Fang YY, Shang J, Zhou L, Wang K, Leng F, Wei S, Chen L, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J. 2020. [DOI] [PMC free article] [PubMed]
- 11.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020. [DOI] [PMC free article] [PubMed]
- 13.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, Zhan LY, Jia Y, Zhang L, Liu D, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020:100331. [DOI] [PMC free article] [PubMed]
- 15.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, and the Northwell C-RC, Barnaby DP, Becker LB, Chelico JD, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020. [DOI] [PMC free article] [PubMed]
- 16.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, et al. Association of Cardiac Injury with Mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020. [DOI] [PMC free article] [PubMed]
- 17.Wang L, Li X, Chen H, Yan S, Li D, Li Y, Gong Z. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol. 2020;51(5):343–348. doi: 10.1159/000507471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. [DOI] [PMC free article] [PubMed]
- 19.Wang D, Yin Y, Hu C, Liu X, Zhang X, Zhou S, Jian M, Xu H, Prowle J, Hu B, et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24(1):188. doi: 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang X, Yu Y, Xu J, Shu H, Ja X, Liu H, Wu Y, Zhang L, Yu Z, Fang M, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, Peng Z, Pan H. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang X, Cai H, Hu J, Lian J, Gu J, Zhang S, Ye C, Lu Y, Jin C, Yu G, et al. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis. 2020;94:81–87. doi: 10.1016/j.ijid.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akram AR, Singanayagam A, Choudhury G, Mandal P, Chalmers JD, Hill AT. Incidence and prognostic implications of acute kidney injury on admission in patients with community-acquired pneumonia. Chest. 2010;138(4):825–832. doi: 10.1378/chest.09-3071. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoste EAJ, Kellum JA, Selby NM, Zarbock A, Palevsky PM, Bagshaw SM, Goldstein SL, Cerdá J, Chawla LS. Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14(10):607–625. doi: 10.1038/s41581-018-0052-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.