“So far as any single place could claim the honor of being the seat of the scientific revolution, the distinction must belong to Padua.”
Herbert Butterfield, 1957
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has wreaked havoc globally, with an ominous morbidity and mortality impact.1 , 2 Indeed, croronavirus disease 2019 (COVID-19) still represents a formidable challenge for pathophysiology, prognostication, management, and rehabilitation. This holds even truer given the conflicting reports accrued so far for several purportedly effective interventions.1 , 3 , 4 Although substantial steps have been accomplished in terms of diagnostic yield, even recognizing early infection is still quite challenging. Each country has addressed COVID-19 in its own way, with variable results. Perusing data on China's experience with the virus brings forward several questions in terms of completeness and truthfulness of reporting, with substantial skepticism despite several authoritative reports.5 For instance, to date, China has reported fewer COVID-19-related deaths than many smaller countries where COVID-19 spread much later (eg, The Netherlands). Countries and healthcare systems that have acted with a global vision, but also with a firm and proactive local hand, have seen the best results in terms of deaths and system derangement. Conversely, countries with a loose policy (either initially such as the United Kingdom or throughout such as Sweden) have already paid an enormous toll of life and pain, and hypothetically will continue to do so.6
As any family interaction recapitulates society interactions at large, so local management practices of SARS-CoV-2, with their successes and failures, remind us of more global efforts at managing this pandemic, and thus may offer important insights for current practitioners, as well as for those facing similar threats in the near or long-term future.
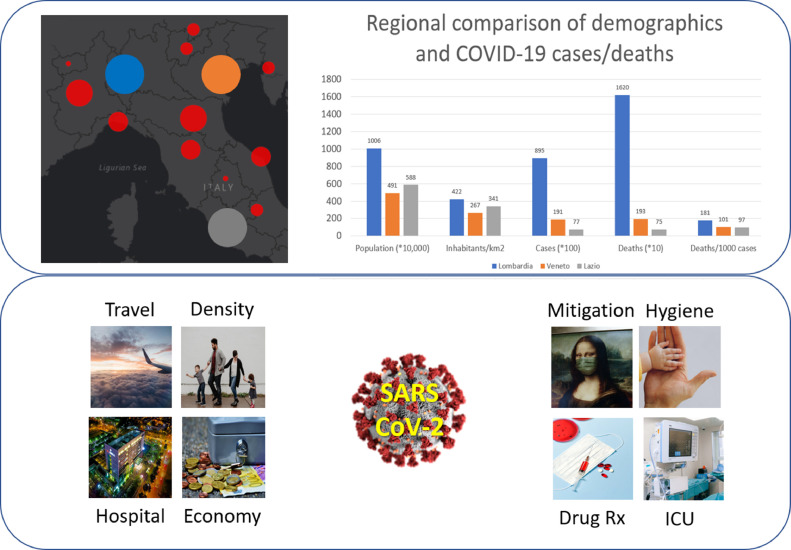
In the present issue, Pasin et al.7 provide important insights on the real-world challenges faced by Veneto (a region in Northeast Italy with almost 5 million inhabitants) healthcare professionals when in late February to early March 2020 they tackled the COVID-19 breakthrough without much guidance from the World Health Organization or the Italian national government.8 Although this article represents a case study in regional and local healthcare delivery, sharing the same strengths and limitations of any observational study exploiting compiled data, it can poignantly inform current practitioners and hopefully even future healthcare managers and stakeholders. Indeed, despite being close to one another, and facing the same mortal threat of SARS-CoV-2 almost concomitantly, Veneto largely succeeded, whereas Lombardy (another large region on Northern Italy) largely and loudly failed. For instance, to date, Veneto has had many fewer cases of COVID-19 than Lombardy, as well as deaths (Fig 1 ). This holds true even taking into account population and density, as also shown by the staggering 1.79 relative risk of dying if infected by SARS-CoV-2 in Lombardy in comparison to Veneto.9 Although several reasons might explain the failure of Lombardy, it is more constructive to emphasize best practices put forward in Veneto that included a multidimensional effort based on shared decision-making aimed at local containment, forceful mitigation, expansion of intensive care unit and stepdown unit facilities, selective intubation protocols, and so on. In particular, the choice to increase nurse- to- patient ratio, emphasizing the role of nursing and paramedic personnel, was a smart one, as was the decision to adopt relatively restrictive intubation protocols and liberal use of ultrasound guidance.5 , 10 Although sparingly adopted, prone positioning for noninvasive ventilation contributed to Veneto's success, as did selective use of extracorporeal membrane oxygenation based on precise hemodynamic data11, which, despite the theoretical benefits, may actually serve simply as a bridging strategy if used too liberally.12, 13, 14
Fig 1.
Comparative results of 3 Italian regions (Lombardy, Veneto, and Latium) in facing the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection and the ensuing coronavirus disease 2019 (COVID-19) pandemic (top panel), and potential hurdles and ways to effectively manage this emergency (bottom panel). COVID-19, coronavirus-associated disease-2019; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2.
Not all that glitters is gold, though. In retrospect, we may consider some opinions and premises too optimistic, and the same applies to the shotgun approach to medical therapy administered to patients with COVID-19, without convincing data in support of any drug treatment (eg, hydroxychloroquine). Accordingly, Veneto, as well as many other early combatants in the fight against SARS-CoV-2, failed to exploit this chronological advantage to design and implement one or more platforms and pragmatic randomized trials, which could have proved crucial to better treat subsequent patients and even more so by informing other practitioners elsewhere. Considering that most institutions in Veneto used a common electronic health record, adding a brief consent form and randomization module would have been easy, and it would have generated a veritable database of scientifically sound data on best management practices for COVID-19.
Another missing piece was the non-COVID-19 burden of morbidity and mortality in Veneto. Indeed, it is becoming apparent that many deaths directly due to COVID-19 were not appropriately attributed to this condition. In addition, delays in care for other severe conditions (eg, acute myocardial infarction) have caused untoward deaths during these frantic months.14 , 15 In the future, efforts at managing SARS-CoV-2 or similarly dreadful infections should consider direct countermeasures for such emergencies, but also the best way to maintain top- quality care and networks for other conditions. Conversely, lockdown measures limiting environmental pollution may also have contributed to favorable clinical results for several chronic conditions.16 , 17
In conclusion, while hopefully Italy and Europe have already seen the worst of the COVID-19 emergency, it is always important to self-criticize prior actions and interventions in an explicit and constructive fashion. Without indulging in self-complacency, the Italian region of Veneto has combined evidence-based medicine with time-tested public health interventions, as well as a global vision with a local proactive stance, successfully controlling the morbidity and mortality impact associated with the spread of SARS-CoV-2 within its borders in the early months of 2020.
Conflict of Interest
Dr. Biondi-Zoccai has consulted for Replycare.
References
- 1.Berlin D.A., Gulick R.M., Martinez F.J. Severe covid-19 [e-pub ahead of print] N Engl J Med. 2020 doi: 10.1056/NEJMcp2009575. Accessed on July 1, 2020. [DOI] [PubMed] [Google Scholar]
- 2.Biondi Zoccai G., Landoni G., Carnevale R., Cavarretta E., Sciarretta S., Frati G. SARS-CoV-2 and COVID-19: Facing the pandemic together as citizens and cardiovascular practitioners. Minerva Cardioangiol. 2020;68:61–64. doi: 10.23736/S0026-4725.20.05250-0. [DOI] [PubMed] [Google Scholar]
- 3.Infusino F., Cimino S., Lombardi M. Relationship between ACE-inhibitors, ARBs and SARS-CoV-2 infection: Where are we [e-pub ahead of print]? Minerva Cardioangiol. 2020 doi: 10.23736/S0026-4725.20.05271-8. Accessed on July 1, 2020. [DOI] [PubMed] [Google Scholar]
- 4.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang E., Mei W., Shang Y. Chinese Association of Anesthesiologists expert consensus on the use of perioperative ultrasound in coronavirus disease 2019 patients. J Cardiothorac Vasc Anesth. 2020;34:1727–1732. doi: 10.1053/j.jvca.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saglietto A., D'Ascenzo F., Zoccai G.B. COVID-19 in Europe: The Italian lesson. Lancet. 2020;395:1110–1111. doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasin L., Sella N., Correale C. Regional COVID-19 network for coordination of SARS-CoV-2 outbreak in Veneto. Italy [e-pub ahead of print] 2020 doi: 10.1053/j.jvca.2020.05.005. Accessed on July 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mugnai G., Bilato C. Covid-19 in Italy: Lesson from the Veneto Region. Eur J Int Med. 2020 doi: 10.1016/j.ejim.2020.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Italian Government - Dipartimento della Protezione Civile - Attività sui rischi - Rischio sanitario - Emergenze - Emergenza Coronavirus. Available at: http://www.protezionecivile.gov.it/attivita-rischi/rischio-sanitario/emergenze/coronavirus. Accessed on July 1, 2020.
- 10.Ma L., Song K., Huang Y. Coronavirus disease-2019 (COVID-19) and cardiovascular complications [e-pub ahead of print] J Cardiothorac Vasc Anesth. 2020 doi: 10.1053/j.jvca.2020.04.041. Accessed on July 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rozental O., Thalappillil R., White R.S. Hemodynamic monitoring options in COVID-19 [e-pub ahead of print] J Cardiothorac Vasc Anesth. 2020 doi: 10.1053/j.jvca.2020.04.050. Accessed on July 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marullo A.G., Cavarretta E., Biondi-Zoccai G. Extracorporeal membrane oxygenation for critically ill patients with coronavirus-associated disease 2019: An updated perspective of the European experience [e-pub ahead of print] Minerva Cardioangiol. 2020 doi: 10.23736/S0026-4725.20.05328-1. Accessed on July 1, 2020. [DOI] [PubMed] [Google Scholar]
- 13.Haye G., Fourdrain A., Abou-Arab O. COVID-19 Outbreak in France: Setup and activities of a mobile extracorporeal membrane oxygenation team during the first 3 weeks [e-pub ahead of print] J Cardiothorac Vasc Anesth. 2020 doi: 10.1053/j.jvca.2020.05.004. Accessed on July 1, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaushal M., Schwartz J., Gupta N. Patient demographics and extracorporeal membranous oxygenation (ECMO)-related complications associated with survival to discharge or 30-day survival in adult patients receiving venoarterial (VA) and venovenous (VV) ECMO in a quaternary care urban center. J Cardiothorac Vasc Anesth. 2019;33:910–917. doi: 10.1053/j.jvca.2018.08.193. [DOI] [PubMed] [Google Scholar]
- 15.Versaci F., Scappaticci M., Calcagno S. ST-elevation myocardial infarction in the COVID-19 era [e-pub ahead of print] Minerva Cardioangiol. 2020 doi: 10.23736/S0026-4725.20.05343-8. Accessed on July 1, 2020. [DOI] [PubMed] [Google Scholar]
- 16.Biondi-Zoccai G., Frati G., Gaspardone A. Impact of environmental pollution and weather changes on the incidence of ST-elevation myocardial infarction [e-pub ahead of print] Eur J Prev Cardiol. 2020 doi: 10.1177/2047487320928450. Accessed on July 1, 2020. [DOI] [PubMed] [Google Scholar]
- 17.Versaci F., Biondi-Zoccai G., Giudici A.D. Climate changes and ST-elevation myocardial infarction treated with primary percutaneous coronary angioplasty. Int J Cardiol. 2019;294:1–5. doi: 10.1016/j.ijcard.2019.07.006. [DOI] [PubMed] [Google Scholar]