Abstract
Men whose sexual behaviors place them at risk of HIV often exhibit a “cluster” of risky behaviors, including alcohol misuse and violence against women. Called the “Substance Abuse, Violence and AIDS (SAVA) syndemic,” this intersecting set of issues is poorly understood among heterosexual men in sub-Saharan Africa. We conducted a baseline survey with a cohort of men in an informal, peri-urban settlement near Johannesburg during the period of Jan – Aug 2016. Audio-assisted, self-completed questionnaires on tablets measured an index of risky sex (inconsistent condom use, multiple and risky partnerships, transactional sex), recent physical or sexual violence against women (using the Multicountry Study instrument), alcohol misuse (Alcohol Use Disorders Tool), and gender attitudes (Gender Equitable Men’s Scale). We used linear and logistic regression to test for syndemic interaction on multiplicative and additive probability scales. We used structural equation modeling to test whether assumptions around serially causal epidemics hold true in these data. Of 2,454 men, 91.8% reported engaging in one or more types of risky sex. Similarly, a high number of participants reported one or more SAVA conditions (1783, 71.6%). After controlling for socio-demographics, higher scores on the risky sex index were independently predicted by men’s recent violence use, problem drinking, and inequitable gender views. Those men reporting partner violence perpetration, problem drinking, and inequitable gender views had more than 12-fold greater odds of risky sex compared to counterparts with no syndemic conditions. A three-way interaction of alcohol use, gender inequitable views, and IPV perpetration was associated with a 16 percent relative increase in risky sex. On the additive scale, significant two-way interactions existed between alcohol use and gender inequitable views, and between gender inequitable views and IPV perpetration. A structural equation model illustrated that gender norms predict violence, which in turn predict alcohol misuse, increasing both IPV perpetration and risky sex. These data are consistent with a syndemic model of HIV risk among heterosexual men. Projects that target a single condition may have limited success, given that alcohol, gender norms, and violence are co-occurring, with interactions that produce greater odds of HIV risky behaviors. Targeting the intersections between these syndemic conditions may help prevent HIV among heterosexual men in peri-urban African settings.
Keywords: syndemics, HIV risk, alcohol use, intimate partner violence, informal settlements
Introduction
HIV risk has long been seen as intertwined with other health challenges such as intimate partner violence and alcohol misuse. The term “SAVA syndemic” (standing for “substance abuse, violence, AIDS”) was coined by medical anthropologists to highlight the concurrent, intersecting, and mutually reinforcing nature of these particular health problems (Singer & Clair, 2003).
Syndemics literature has important traits to distinguish it from typical epidemiological analysis. First, unlike the concept of comorbidity – which means that two conditions co-occur alongside one another – syndemic theory involves the interaction between social and disease conditions (Singer et al., 2017). The theory posits that it is the synergistic clustering of conditions, rather than the simple summation of additional symptoms, that influence the health burden of a specific population (Tsai & Burns, 2015). Tsai (2018) posits three models of syndemics: they can be “synergistically interacting”, which means the interaction between conditions amplifies health burdens (Singer & Clair, 2003); they can be “mutually causal”, which means each condition simultaneously influences the nature of the other (Singer, 2006); they can also be “serially causal”, where the effects of one condition snowballs into other conditions (Coie et al., 1993; Ferlatte et al., 2014).
SAVA, and syndemics more broadly, have been examined among women in the U.S. (Feingold, 2009; Gonzalez-Guarda et al., 2011; Illangasekare et al., 2013; Meyer et al., 2011), with newer research using the construct to explain dynamics among women in low- and middle-income settings (Russell et al., 2013; Ulibarri et al., 2011). Others have explored SAVA among samples that include both men and women (Salas-Wright, 2015; Senn, Carey, & Vanable, 2010). A growing body of research has applied a syndemics lens to data from men who have sex with men (Chakrapani et al., 2019a; Safren et al., 2018; Tomori et al., 2018). Yet, within each of these distinct populations, the focus of SAVA has traditionally bebeen on the experience of violence victimization and HIV risk.
Our previous qualitative work was the first, to our knowledge, to consider the application of the SAVA syndemic to heterosexual men’s violence perpetration (Hatcher et al., 2014). We found that the same beliefs about manhood that drive IPV perpetration seem to influence men’s alcohol use and their sexual risk behaviors. Drawing on that publication and others, Fleming and colleagues (2016) theorized that several gendered norms influence men’s HIV risk: the belief that male sex drive is uncontrollable; the desire to perform sexually; and, a need to retain power over others, which recognizes the role of men’s use of violence.
These qualitative findings and theoretical assertions align with quantitative data on the nature of men’s intersecting health behaviors. We know, for example, that men who enact IPV engage in higher levels of sexual risk behaviors, including inconsistent condom use (Raj et al., 2006; Townsend et al., 2011a), transactional sex (Dunkle et al., 2006; Townsend et al., 2011a), and casual partnerships (Christofides et al., 2014; Dunkle et al., 2006). One recent paper from South Africa used latent class analysis to distinguish between men with high violence/antisocial behavior (which tracked with multiple partners, use of a sex worker, transactional sex, and drug use), or moderate violence/promiscuous behavior (which tracked with multiple partners and transactional sex, but not the other behaviors) (Jewkes & Morrell, 2018). However, Jewkes and Morrell did not build problem drinking into their classes, and HIV status was not shown to be significantly associated. So, while the paper adds considerably to the literature, it does not fully represent a SAVA syndemic lens.
While the mechanisms linking men’s IPV perpetration and men’s HIV risk remain unexplored, there is growing evidence for an association. Problematic alcohol use is strongly associated with HIV risk, including transactional sex, casual partnership and reduced condom use (Kalichman et al., 2007; Townsend et al., 2011b; Townsend et al., 2010). Lastly, alcohol and IPV perpetration have been shown to have a statistically significant relationship in multiple meta-analyses (Foran & O’Leary, 2008; Schumacher et al., 2001; Stith et al., 2004), though again mechanistic understanding of this association is limited. Only one other paper has, to our knowledge, simultaneously examined alcohol, violence perpetration, and HIV risk among heterosexual men. Okafor and colleagues (2018) found a significant additive interaction of problem drinking and violence perpetration on men’s reports of multiple sex partners.
To unpack syndemics among heterosexual men, it is essential to recognize that gender inequalities are a key backdrop to the conditions of alcohol use, IPV perpetration, and HIV risk. This is consistent with a deep body of evidence showing that men’s gendered identities, or “masculinities”, strongly shape their health (Mankowski & Maton, 2010; Morrell et al., 2012; Peralta et al., 2010). Masculine norms around risk-taking, virility, and resilience have been associated with risky sex in the form of multiple partnerships, lower condom use, and transactional sex (Nyanzi et al., 2009; Santana et al., 2006; Townsend et al., 2011a). In southern Africa, dominant forms of masculinity, which are predicated on heterosexuality (Luyt, 2012), are often associated with problem alcohol use (Morojele et al., 2006; Peralta et al., 2010). This is, in part, because men’s capacity for drinking is sometimes used as a way to demonstrate their strength and “manliness” (Courtenay, 2000). Qualitative findings from rural South Africa have highlighted how men use taverns (or informal alcohol venues) as a social space to display their dominance and willingness to take risks (Hatcher et al., 2014; Rich et al., 2015).
Despite increasing public health interest in syndemics, there remain key conceptual and methodological shortcomings in the current evidence base. Tsai and colleagues have shown, through a series of papers, the misalignment between syndemic theory and the quantitative methods used in much of the syndemics literature (Tsai, 2018). The authors note that most papers rely on summing the total number of syndemic conditions of individuals (Tsai & Burns, 2015), a technique that is insufficient to demonstrate disease interaction or synergistic effects (Tsai, 2018; Tsai & Venkataramani, 2016). The rationale for better quantitative models of syndemics is that program and policy can only be guided if data accurately portrays how related conditions work together to influence health outcomes.
We examine whether data among heterosexual men living in a peri-urban setting near Johannesburg support a gendered SAVA syndemic approach. Cross-sectional data from the baseline of a cluster-randomized control trial is analyzed through regression and structural equation modeling techniques.
Methods
Setting
The trial was conducted in a semi-formal ‘township” located near Johannesburg, South Africa. The peri-urban settlement took form in the mid-1990s, when a period of accelerated migration to urban areas occurred after the 1994 democratic election. In the township where our work takes place, predominately black families and single men used the area as a “landing pad” that was closer to cities to seek employment. The area is home to roughly half a million people (exact estimates are unknown as the most recent census, conducted in 2011, stated that there were 140,000 residents (Statistics South Africa, 2012)). Migration from other African countries and internal migration is among the highest in South Africa (Peberdy et al., 2017). The township is a densely populated marginalized area, which lacks basic infrastructure and adequate housing provision. Most residents live in government-subsidized housing or informal tin shacks. Many parts of the township are informal and lack basic services such as electricity, running water, sanitation, roads, sewerage and rubbish removal. Recent papers estimate that half the population in the settlement is unemployed (Mahajan, 2014). Compared to neighboring suburbs, the township has markedly worse living conditions, higher poverty, and residents report lower levels of personal safety (Mushongera et al., 2017). Furthermore there are limited public services and minimal social or recreational facilities.
Data collection
Trained research assistants recruited male participants who lived in the area for at least 12 months and were 18–40 years old. The rationale for this particular age group is that younger men typically use violence more than older counterparts, and the trial was testing a violence prevention intervention. Interested men were told about the study through outreach efforts within neighborhood “clusters” and a volunteer sample was recruited.
Details of the study can be found elsewhere (Christofides et al., 2018). Briefly, following written informed consent, participants took part in audio-computer assisted structured interview (ACASI) on a 7-inch Android tablet computer using the Open Data Kit software. ACASI allows data to be collected about sensitive topics while ensuring anonymity and confidentiality. Data collection occurred in private locations within study neighborhoods such as a community hall, restaurant, or yard. ACASI was conducted in the language of participant choice (English, isiZulu, Tswana, or Sepedi). Electronic data collection provides a standardized method that minimizes user bias and improves data quality as it precludes data entry of paper forms. Security of data can be improved through use of electronic data collection (versus using paper forms), since data is uploaded to an encrypted server at the end of each day. The server is housed at the university and had been purpose-built for this study.
Measures
A structured questionnaire asked participants a series of items, self-completed using ACASI.
Outcome measure.
Risky sex was measured through multiple items related to HIV risk in the extant literature. Numbers of partners in the past year were summed from 1 item asking about the total number of main partners and categorized into no partners, low number of past-year partners (1 or 2), moderate number (3–7), high number (8–15), and very high number (16 or more). A participant was considered to have a high number of partners if he reported within the highest quartile (8 or more partners). Types of risky sex were summed from dichotomous measures of past-year risky relationships: ever having sex with a sex worker, ever having a makhwapheni (an isiZulu term meaning “side dish” which typically denotes a second main partner who is a longer-term relationship), or ever having a one-night-stand (score 0–3). Condom use was measured by a single item asking “How often have you used condoms in the last 12 months?” with answers on a four-point likert scale (never, sometimes, often, always). Consistent condom use was measured as a response of “always”. Transactional sex was measured using the Medical Research Council’s 5-item measure for transactional sex among casual partners (MRC, 2010). These asked about whether participants thought a once-off sex partner or any makhwapheni or casual partner had sex with them in the past 12 months because she may receive a range of items (e.g. cell phone, gifts, food, a place to stay). Transactional sex was defined as a positive answer to one or more of the five questions and summed to create an intensity scale (0–5). Men giving gifts for transactional sex is conceptually distinct from having sex with a sex worker, since the latter implies a specific negotiation of a cash exchange (Jewkes et al., 2012b). Any risky sex was a binary outcome, indicating that a participant responded positively to one or more of the four risky behaviors.
SAVA Conditions.
Intimate partner violence was measured using an adapted version of the questionnaire from the South African Medical Research Council’s Study on Men’s Health and Relationships (Fulu et al., 2013; Jewkes et al., 2011), which is an adaptation of the World Health Organization (WHO) multi-country study instrument (Garcia-Moreno et al., 2006). The questionnaire includes likert-type behavioral items concerning physical and sexual violence. We defined IPV perpetration as any use of physical violence and/or any use of sexual violence in the past 12 months. The 8 items of physical/sexual IPV perpetration were summed to create a continuous measure of IPV intensity (0–24). Harmful alcohol use was measured using the Alcohol Use Disorders Identification Test (AUDIT), a 10-item likert-type scale designed to measure alcohol consumption and identify risks for alcohol abuse and dependence (Saunders et al., 1993). An AUDIT score ≥8 is considered consistent with problem drinking, and we also summed the items to create a continuous variable of alcohol use (0–40). Gender Attitudes were measured using the Gender Equitable Men’s Scale (Pulerwitz & Barker, 2008), which we divided into tertiles, calling the top tertile “inequitable views”. Similarly, we summed the total scale to devise a continuous score (11–44).
Covariates.
Education asked about years of schooling and whether the participant completed high school matriculation. Age in years and relationship status were assessed using items from the United Nations Multi-country Study. Employment asked about frequency of employment over the past year (never, sometimes, often, always). Housing was measured by the type of structure the participant lived in (e.g. single room, shack, stand-alone house). Informal housing was considered living in a shack. Food security was measured using the 3-item Household Hunger Scale (Deitchler et al., 2010). Migrancy was assessed by the province of the participant’s birth and coded as a dichotomous outcome with migrancy indicating birth outside of Gauteng Province, where the study was conducted.
Analysis
We model our reporting structure on that used in Chakrapani et al. (2018) in an effort to build consistency across syndemics literature. We first calculated descriptive statistics and the co-occurrence of SAVA conditions. Next, we used logistic regression to assess the bivariate and multivariate relationship between sociodemographics and SAVA conditions and the outcomes of interest: a dichotomous measure of any reported risky sex in the past year.
We assessed for interactions on both the additive and multiplicative scales using linear probability regression models with product terms. In order to compare models with the same degrees of freedom, we fitted three linear regression models with one product term at a time, controlling for socio-demographics of age, education, relationship status, and adjusting for clustering. We included product terms representing two-way interactions between alcohol use, IPV perpetration, and gender inequitable views. Based on guidance from Vanderweele and Knol (2014), we calculated excess risk due to additive interaction for binary exposures using logistic regression.
Interactions on the multiplicative scale were assessed using multivariable logistic regression, adding two-way and three-way interactions between alcohol use, IPV perpetration, and gender inequitable views, and estimating the multiplicative interaction parameters. After fitting the logistic regression models, we used the attributable proportion (AP) which measures the proportion of the risk in the doubly exposed group that is due to the interaction itself (VanderWeele & Vansteelandt, 2014). If the estimated semi-elasticities are significant, it implies interaction is present on the multiplicative scale. The estimated semi-elasticities can also be interpreted as the percent relative change in the outcome that can be attributed to the joint effect of two (or more) exposures, above and beyond their independent associations with the outcome.
To test the model of serially causal epidemics, we used the sem command in Stata (version 14; College Station, Texas, USA). We specified continuous variables for the SAVA conditions and sociodemographic controls. HIV risky sex was constructed as a latent variable comprised of measured variables: total partner numbers, partner types, condom use frequency, and total types of transactional sex. Confirmatory factor analysis suggested that the data fit well with this latent variable construction. SEM with maximum likelihood with missing values estimation was used to test pathways between gender inequality (GEM score), intensity of IPV perpetration (score on the WHO multi-country study instrument), and problem drinking (AUDIT score), and the latent construct of risky sex. Bivariate regression and evidence from extant literature was used to guide preliminary model building. Model modifications were performed based on modification indices and theoretical plausibility. After deriving a path model solution, the latent construct was regressed on age, education, and relationship status and nonsignificant paths were trimmed. Measures for model fit included a parsimonious measure (root-mean-square error of approximation [RMSEA]) and incremental measures (comparative fit index [CFI], Tucker-Lewis index [TLI]). Acceptable model fit assumed the model met the following criteria: RMSEA<0.05, CFI≥0.95, TLI≥0.95.
Ethical considerations
Study procedures aligned to ethical recommendations of the University of Witwatersrand and of the United Nations Multi-Country Study on Men and Violence (Fulu & Jewkes, 2014). Researchers received intensive training on VAW, the study protocol, collecting sensitive information, and ensuring data quality and participant confidentiality. The study was described as a project about men’s lives and relationships, rather than about violence, to prevent undue stigma for study participation (Jewkes et al., 2012a). Prospective participants were informed that participation was voluntary, that they may withdraw at any stage, skip any question and that there are no adverse effects should they decide not to participate. They signed informed consent forms before participation and were reimbursed for their time through a cash payment of R50 (approximately US $3.50).
Results
Of 2,394 men included in the analysis, just over a third had completed high school education (39.9%, Table 1). Most were in a relationship (83.6%) with just over one-third living with their partner (39.2%). The majority had migrated from another province or country (73.2%) and just under half lived in informal housing, such as a shack (45.4%). Poverty was prevalent, with 873 (36.5%) men reporting unemployment throughout the course of the past year and 44% reporting household hunger in the past month.
Table 1:
Descriptive data on cohort n=2,454
| Median (IQR) or Number (%) | |
|---|---|
| Socio-demographics | |
| Age (years) | 27 (23–32) |
| High school education | 979 (39.9%) |
| Partnered, living together | 932 (39.2%) |
| Partnered, living apart | 1055 (44.4%) |
| Single | 391 (16.4%) |
| Migrant | 1795 (73.2%) |
| Lives in informal housing | 1114 (45.4%) |
| Unemployed | 873 (36.5%) |
| Household hunger | 1089 (44.4%) |
| Risky sex in past year | |
| Any transactional sex | 1104 (45.0%) |
| Inconsistent condom use | 1622 (73.9%) |
| Partner number | 3 (1–8) |
| Used sex worker | 444 (21.6%) |
| Khwapheni | 1490 (60.7%) |
| One-night stand | 1394 (56.8%) |
| Ever risky sex | 2190(91.5%) |
IQR: inter-quartile range
Prevalence of risky sex
A large majority of participants (91.5%) reported engaging in one or more types of risky sex in the past year. The commonest form of risky sex was inconsistent condom use (73.9%), with the majority reporting a one-night stand (56.8%) or makhwapeni (60.7%) in the past year. Roughly half of the cohort (45.0%) reported using one or more forms of transactional sex and one in five (21.6%) had had sex with a sex worker in the past year.
Co-occurrence of SAVA syndemic conditions
Nearly three-quarters of the sample (71.6%) reported one or more SAVA syndemic conditions (Figure 1). Problem drinking, inequitable gender views, and perpetration of IPV frequently co-occurred: while only 77 (3.3%) reported inequitable gender views and problem drinking, 175 (7.4%) held such gender views and perpetrated IPV, while 346 (14.6%) exhibited problem drinking and IPV perpetration. Nearly one in ten participants (n=210, 8.9%) reported all three SAVA syndemic behaviors of inequitable views, problem drinking, and IPV perpetration.
Fig 1.
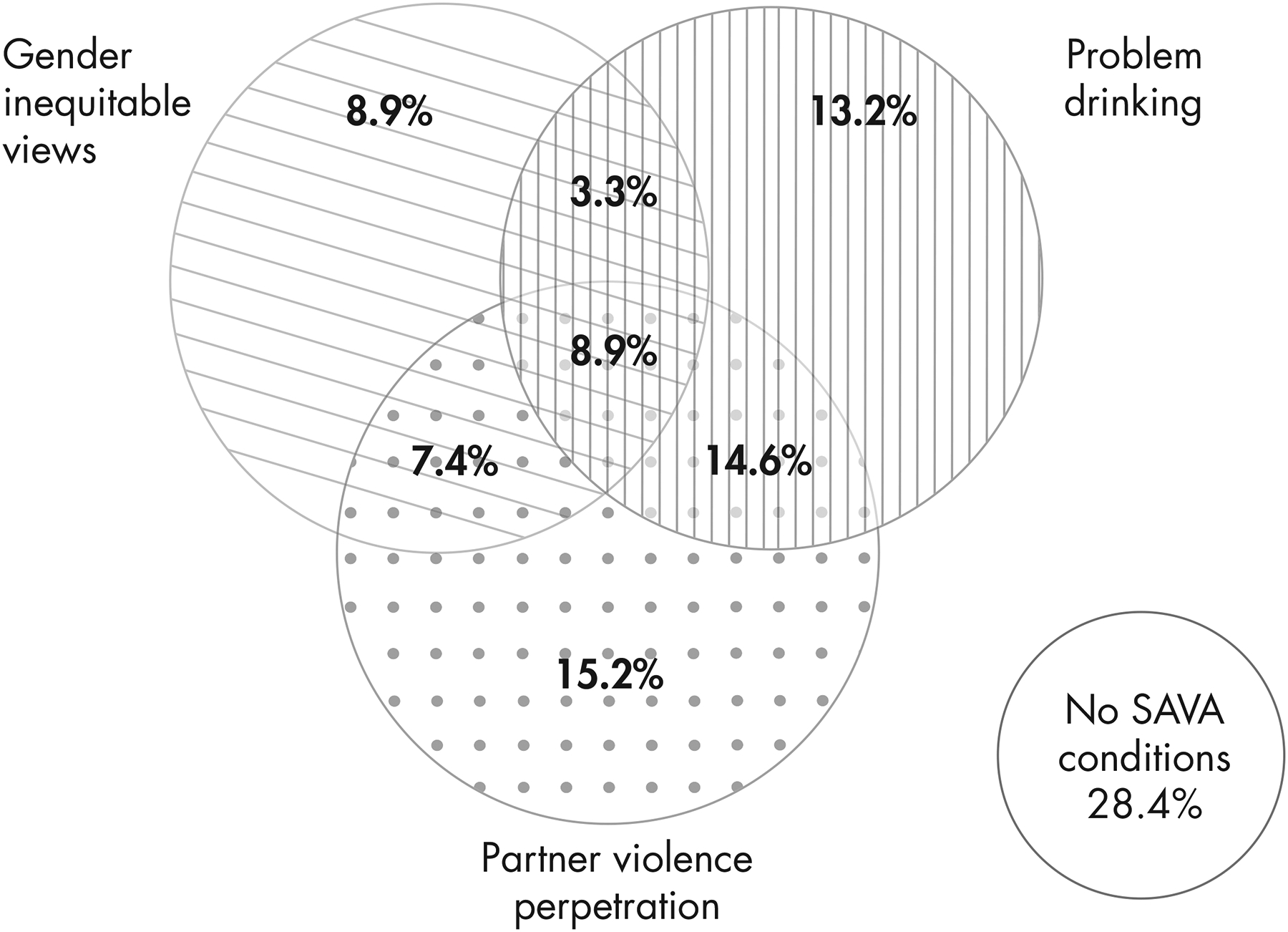
Co-occurence of SAVA syndemic conditions (n=2,394)
In univariate logistic regression (Table 2), men who completed high school education, and who were partnered but living apart, had lower odds of reporting risky sex. Socio-demographics of age, migrancy, and living in informal housing were associated with risky sex at the p<0.20 level, and thus were retained in the final model.
Table 2:
Unadjusted estimates and full linear model of SAVA syndemic and any risky sex (n=2394)
| Any Risky Sex | ||
|---|---|---|
| OR (95% CI) | AOR (95% CI) | |
| Sociodemographics | ||
| Age, in years | 0.98 (0.96–1.01) | 0.98 (0.96–1.01) |
| High school education (vs. not) | 0.66 (0.49–0.88) ** | 0.78 (0.571.06) |
| Partnered, living apart | 0.55 (0.41–0.73) *** | 0.48 (0.35–0.65) *** |
| Migrant | 0.78 (0.56–1.10) | 0.82 (0.57–1.18) |
| Lives in informal housing | 0.79 (0.59–1.06) | 0.86 (0.63– 1.16) |
| Employed, past year | 0.93 (0.81–1.07) | - |
| Household hunger, past month | 0.97 (0.73–1.30) | - |
| Gendered SAVA syndemic | ||
| No SAVA conditions | - | ref |
| Inequitable gender views only | - | 1.51 (0.92–2.50) |
| Problem drinking only | - | 1.60 (1.05–2.45) * |
| Any IPV perpetration only | - | 2.66 (1.61–4.37) *** |
| Gender views * Alcohol | - | 5.00 (1.53–16.32) ** |
| Gender views * Violence | - | 4.80 (206–11.23) *** |
| Alcohol * Violence | - | 4.92 (2.69–8.97) *** |
| Gender views * Alcohol * Violence | - | 12.56 (3.92–40.22) *** |
p=0.07
p<0.05
p<0.01
p<0.001
OR: odds ratio; CI: confidence interval; VAW: violence against women
After controlling for socio-demographics (Table 2), reporting risky sex was independently predicted by SAVA syndemic conditions. On its own, problem drinking significantly increased odds of risky sex (adjusted odds ratio [AOR] 1.60, 95% confidence interval [CI] 1.05–2.45). Recent IPV perpetration on its own was associated with 2.66 higher odds of risky sex (95%CI 1.61–4.37). A combination of two SAVA syndemic conditions was associated with roughly five-fold increased odds of risky sex (AOR of 5.00, 4.80, 4.92 for combinations of gender views/alcohol, gender views/IPV, alcohol/IPV, respectively). Those men reporting all SAVA syndemic conditions (partner violence perpetration, problem drinking, and inequitable gender views) had more than 12-fold greater odds of risky sex (AOR 12.56, 95%CI 3.92–40.22).
Model of synergistically interacting epidemics
We used logistic regression models with product terms to assess for multiplicative interactions. In order to compare models with the same degrees of freedom, we fitted three logistic regression models with one product term at a time, controlling for socio-demographics of age, education, relationship status, and adjusting for clustering (Models 1–3 in Table 3). In all three models, the main effects of alcohol, gender views, and IPV perpetration had statistically significant associations with risky sex. The joint effect of gender inequitable views and IPV perpetration, above and beyond their individual associations with risky sex, was associated with a 45 percent relative increase in the outcome (95%CI 0.00–0.89, p = .046). The joint effect of gender inequitable views and problem alcohol use was also associated with increased odds of risky sex (attributable proportion [AP]=0.60, 95%CI 0.21–0.98).
Table 3:
Marginal effect of SAVA syndemic conditions and any risky sex: Multiplicative interaction in logistic regression models (n=2394)
| Model 1: Two-way product term Alcohol * Violence | Model 2: Two-way product term Gender * Alcohol | Model 3: Two-way product term Gender * Violence | |
|---|---|---|---|
| Estimated semi-elasticity (95% CI), p value | Estimated semi-elasticity (95% CI), p value | Estimated semi-elasticity (95% CI), p value | |
| Gendered SAVA syndemic | |||
| Alcohol * Violence | 0.35 (−0.01–0.76) p=0.098 | ||
| Gender views * Alcohol | 0.60 (0.21–0.99) p=0.002 | ||
| Gender views * Violence | 0.45 (0.00–0.89) p=0.046 |
CI: confidence interval
Bold denoted p<0.05; All models adjusted for age, education, relationship status, and clustering by neighborhood
We used logistic regression models to estimate interactions on the additive scale (Table 4). In logistic regression models that included main effects and one two-way product term at a time, we found evidence for departures from additivity for the two-way product terms of problem alcohol use and violence (b=0.31, 95%CI 0.11–0.50, p=0.002) (Table 4). These non-zero, positive, and statistically significant estimates measure the proportion of the risk in the doubly exposed group that is due to the interaction itself.
Table 4:
Marginal effect of SAVA syndemic conditions and any risky sex: Additive interaction in logistic regression models (n=2394)
| Model 1: Two-way product term Alcohol * Violence | Model 2: Two-way product term Gender * Alcohol | Model 3: Two-way product term Gender * Violence | |
|---|---|---|---|
| b (95% CI), p value | b (95% CI), p value | b (95% CI), p value | |
| Gendered SAVA syndemic | |||
| Alcohol * Violence | 0.31 (0.11–0.50) p=0.002 | ||
| Gender views * Alcohol | .11 (−0.15–0.38) p=0.416 | ||
| Gender views * Violence | 0.22 (−0.04–0.49) p=0.106 |
CI: confidence interval
Bold denoted p<0.05; All models adjusted for age, education, relationship status, and clustering by neighborhood
Structural equation model of serially causal epidemics
In a structural equation model, we fitted risky sex as a latent variable comprised of: number of past-year partners, total types of risky sex, condom frequency in past 12 months, total types of transactional sex. The latent construct had better fit without the measured construct of condom frequency, so this was removed for final model. We used theory to inform an initial path model of gender inequitable views leading to alcohol misuse and IPV perpetration, ultimately leading to risky sex. Once this path model fitted the data we added in socio-demographic controls (age, education, relationship status). The final structural equation model has strong fit (RMSEA 0.027, 95%CI 0.015–0.039; CFI 0.994; TLI 0.982), suggesting that a gendered SAVA syndemic model aligns well with these data.
Discussion
We found that a high proportion of male participants in a peri-urban South African study reported one or more SAVA syndemic conditions (71.6%). Alcohol misuse, gender inequitable views, and IPV perpetration co-occurred and analyses were consistent within multiple ways of examining syndemics. Any past-year risky sexual behaviors was reported among a majority of participants (91.8%). In models of synergistically interacting epidemics, using both additive and multiplicative scales, we found evidence of two-way and three-way interaction between alcohol, gender inequity, and IPV perpetration. In a structural equation model of serially causal epidemics, gender inequality predicted both alcohol misuse and IPV, with all three in turn predicting risky sex.
Only one previous study has explored SAVA using quantitative data among heterosexual male respondents (Okafor et al., 2018). In addition, prior research from South Africa used latent class analysis to demonstrate that masculinity, IPV perpetration, and HIV risk often track together (Jewkes & Morrell, 2018). Our findings extend this research in three important ways. Firstly, our study unpacks how the additive effect of SAVA conditions may worsen HIV risk behaviors in both additive and multiplicative ways. We found that SAVA conditions tend to co-occur and that their interaction measurably worsens HIV risk. That the interaction itself is responsible for increased HIV risk among men means that no program addressing only one SAVA condition in isolation will make inroads in reducing men’s risky sexual behaviors.
Secondly, our latent concept of HIV risk represents a more nuanced outcome measure as compared to other recent studies that examine crude dichotomous outcomes of individual risk behaviors (e.g. multiple sex partners vs. not) (Jewkes & Morrell, 2018; Okafor et al., 2018). Unlike Jewkes & Morrell’s cohort from two provinces that spanned rural areas, towns, and a major city, our sample lived within a peri-urban township characterized by high levels of deprivation and economic insecurity. This is an important setting for future research, given that peri-urban settlements represent the fastest population growth globally, and have increasingly intractable health challenges due to their relatively lower access to services and economic opportunity (Ezeh et al., 2017).
These data offer additional empirical evidence to theoretical syndemics literature by illustrating synergistic interaction and causal mediation. Our findings are consistent with recent syndemic analyses in a large sample of men who have sex with men in India (Chakrapani et al., 2019b), by demonstrating two- and three-way interactions between violence, alcohol, and HIV risk. Our study was distinct from the Indian sample, since we recruited primarily heterosexual men living in a peri-urban settlement characterized by high levels of poverty and unemployment. This suggests preliminarily evidence that violence, alcohol, and HIV risk operate in syndemic ways across various settings and population groups, though that assertion would require additional research to confirm.
In our structural equation model, it is challenging disentangle whether gender attitudes are part of the syndemic condition themselves, or if they are a structural force that frames the SAVA syndemic. Both arguments fit the current syndemics literature. In a special issue in The Lancet, Singer and colleagues (2017) explain that syndemics concern “the disease interaction and the social, environmental, or economic factors that cluster with the diseases and shape their interaction.” Within this definition, gender inequitable views held by men could be framed as a social factor that clusters and shapes HIV risk. Certainly, other social and structural forces (e.g. immigration, food insecurity, economic inequality) have been implicated within syndemic definitions (Mendenhall, 2014, 2016; Okafor et al., 2018). Conversely, in the same Lancet issue, Tsai and colleagues (2017) explain that “the field can achieve more efficient population-level prevention of the disease burden wrought by syndemics if attention is shifted towards elimination of the large-scale social forces that condition the distributions of individual-level risk factors … but [these] have largely gone unmodeled (p.981).” In this regard, men’s gender inequitable views could be interpreted in our own data as a social force that is now modeled as a condition influencing individual risk.
Limitations
These data should be interpreted in light of several limitations. Due to the use of convenience sampling, these findings are not generalizable, and no claims can be made about the overall prevalence of conditions in these communities. The cross-sectional nature of the data is a considerable weakness, limiting the ability to determine causality. We addressed this by reversing the direction of arrows to test for potential bidirectional nature of the relationships and found that the presented SEM holds the strongest fit. Nevertheless, future analysis should use longitudinal data to confirm the proposed relationships. Self-report of men’s IPV perpetration and gender views is currently the state of the science for IPV and gender research. The anonymity of ACASI may assist with accurate reporting of IPV by men by limiting social desirability bias. However, future studies should enhance the AUDIT reporting through biomarkers of alcohol use. Self-report of HIV risk behaviors is less than ideal, and SAVA syndemics among heterosexual men could be explored in future using HIV incidence data. We were unable to test the mutually causal model of syndemics using STATA, but this should be explored in future research.
Implications for programming and policy
Scholars have suggested that transforming constraining aspects of masculinity may improve the health and well-being of both women and men (Gibbs et al., 2019b; Mankowski & Maton, 2010). This research refines that broad call by offering programmatic strategies that may lead to marked gains in reducing gender inequitable and HIV risk behaviors. Many HIV prevention programs focus on behavior alone, rather than considering the cluster of syndemic issues that heterosexual men face in their daily lives. Future programs should target syndemic conditions of gender beliefs, alcohol misuse, and IPV perpetration alongside sexual health. Targeting the intersection of these topics, rather than a single topic in a ‘programmatic silo’, will have the most impact on the harmful synergy of HIV risk, alcohol, violence, and gender. Certainly, there is still more to be done to untangle the relative influence of various syndemic conditions on HIV risk (Tsai & Burns, 2015), but as others note, these analytical advances should not preclude the simultaneous development of promising interventions (Stall et al., 2015).
An important consideration is the willingness of participants who display multiple syndemic conditions to take part in an intervention. It is plausible that those with all three SAVA conditions (who have twelve times the odds of engaging in risky sexual behaviors) may be the least likely to enroll in a program offered in their community. In some settings, this has not posed a limitation to engaging men in an intervention (Gibbs et al., 2019a). Yet, perhaps a “broad” intervention (those targeting the entire community) should be coupled with a “deep” intervention that assists the most at-risk men with deeply held beliefs and behaviors. One example for men who both abuse alcohol and perpetrate IPV is a “common elements treatment approach” delivered to individuals over the course of 6–12 weekly sessions (Kane et al., 2017).
Conclusion
A gendered syndemic model of HIV risk among heterosexual men fits well with data from peri-urban South Africa. A syndemics approach suggests that targeting a single condition may be less efficacious than simultaneously addressing alcohol, gender norms, and violence as co-occuring, interacting drivers of HIV risk. Strategically preventing HIV risk among heterosexual men living in peri-urban settings is essential if we are to ensure the health of men, women, and children globally.
Fig 2.
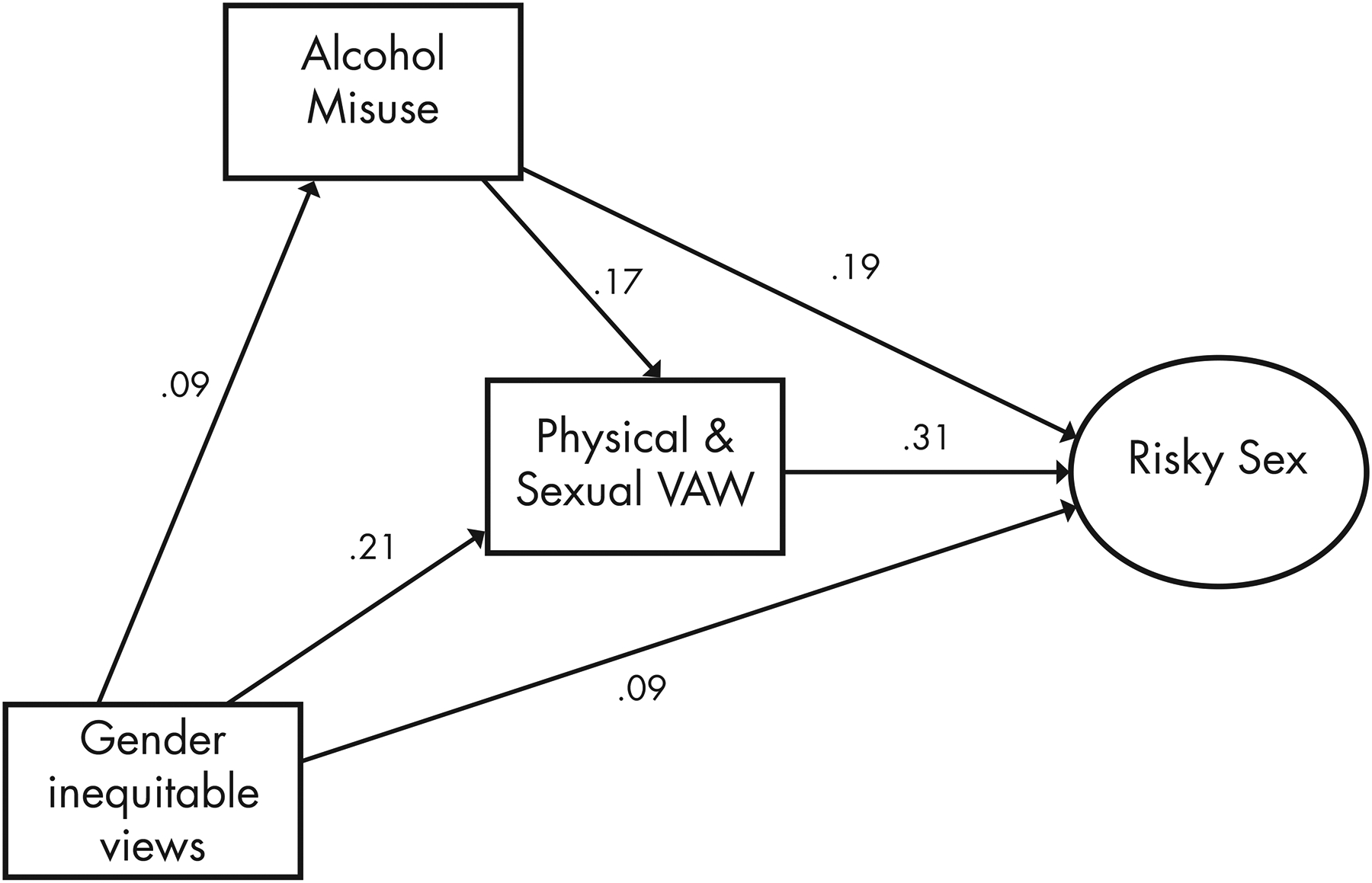
Structural equation model of serially causal SAVA epidemics among heterosexual men (n = 2,423)
All values are standardized and p<0.001. Model controls for age, education, housing type, and relationship status. Goodness of model fi t Chi-square = 60.61 (df = 15); CFI = 0.979; RMSEA = 0.035 (90% CI 0.026 – 0.045).
Table 5:
Structural equation model (n=2,423)
| Standardized estimate OR (95% CI) | p value | ||||
|---|---|---|---|---|---|
| Alcohol | |||||
| <- Gender views | 0.11 | 0.04 | - | 0.13 | <0.001 |
| Recent VAW | |||||
| <- Alcohol | 0.09 | 0.13 | 0.21 | <0.001 | |
| <- Gender views | 0.21 | 0.17 | 0.25 | <0.001 | |
| Risky sex | |||||
| <- Alcohol | 0.12 | 0.14 | 0.23 | <0.001 | |
| <- Recent VAW | 0.28 | 0.26 | 0.36 | <0.001 | |
| <- Gender views | 0.11 | 0.04 | 0.13 | <0.001 | |
| -> Partner number | 0.64 | 0.51 | 0.60 | <0.001 | |
| -> Types of risk | 0.76 | 0.78 | 0.87 | <0.001 | |
| -> Transactional sex | 0.76 | 0.63 | 0.71 | <0.001 | |
p<0.05
p<0.01
p<0.001
OR: odds ratio; CI: confidence interval; VAW: violence against women
Research Highlights.
Heterosexual men’s risky sex overlaps with alcohol and violence against women.
We used a “gendered syndemic” lens to explore substance use, violence, and HIV/AIDS (SAVA).
We found gender norms predict violence, which leads to alcohol and risky sex.
Targeting syndemics among heterosexual men may ensure health in peri-urban settings.
This is among the first papers to offer quantitative support for syndemic theory.
Acknowledgments:
We wish to acknowledge the fieldwork team and facilitators involved in the study, as well as the participants for sharing their data.
Funding: This study is funded through the What Works To Prevent Violence? A Global Programme on Violence Against Women and Girls (VAWG) funded by the UK Government’s Department for International Development (DFID). We also received funding from the South African Medical Research Council Social Innovation Bond, with support from the Global Fund to Fight Malaria, AIDS, and Tuberculosis. However, the views expressed do not necessarily reflect the funders’ policies and the funders had no role in study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the paper for publication.
Footnotes
Competing Interests: None declared.
References
- Chakrapani V, Kaur M, Newman PA, Mittal S, & Kumar R (2019a). Syndemics and HIV-related sexual risk among men who have sex with men in India: influences of stigma and resilience. Cult Health Sex, 21, 416–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V, Lakshmi PVM, Tsai AC, Vijin PP, Kumar P, & Srinivas V (2019b). The syndemic of violence victimisation, drug use, frequent alcohol use, and HIV transmission risk behaviour among men who have sex with men: Cross-sectional, population-based study in India. SSM Popul Health, 7, 100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christofides NJ, Hatcher AM, Pino A, Rebombo D, McBride RS, Anderson A, et al. (2018). A cluster randomised controlled trial to determine the effect of community mobilisation and advocacy on men’s use of violence in periurban South Africa: study protocol. BMJ Open, 8, e017579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christofides NJ, Jewkes RK, Dunkle KL, McCarty FA, Shai NJ, Nduna M, et al. (2014). Perpetration of physical and sexual abuse and subsequent fathering of pregnancies among a cohort of young South African men: a longitudinal study. BMC public health, 14, 947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coie JD, Watt NF, West SG, Hawkins JD, Asarnow JR, Markman HJ, et al. (1993). The science of prevention: a conceptual framework and some directions for a national research program. American psychologist, 48, 1013. [DOI] [PubMed] [Google Scholar]
- Courtenay WH (2000). Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Soc Sci Med, 50, 1385–1401. [DOI] [PubMed] [Google Scholar]
- Deitchler M, Ballard T, Swindale A, & Coates J (2010). Validation of a measure of household hunger for cross-cultural use. Washington, DC: Food and Nurtrition Technical Assistance II Project (FANTA-2), Acedemy for Educational Development. [Google Scholar]
- Dunkle KL, Jewkes RK, Nduna M, Levin J, Jama N, Khuzwayo N, et al. (2006). Perpetration of partner violence and HIV risk behaviour among young men in the rural Eastern Cape, South Africa. Aids, 20, 2107–2114. [DOI] [PubMed] [Google Scholar]
- Ezeh A, Oyebode O, Satterthwaite D, Chen YF, Ndugwa R, Sartori J, et al. (2017). The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet, 389, 547–558. [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). SAVA Latina: Addressing the interplay of substance abuse, violence, and AIDS affecting Hispanic women (Part 1). Mental Health AIDS, 10, 4–8. [Google Scholar]
- Ferlatte O, Hottes TS, Trussler T, & Marchand R (2014). Evidence of a syndemic among young Canadian gay and bisexual men: Uncovering the associations between anti-gay experiences, psychosocial issues, and HIV risk. Aids and Behavior, 18, 1256–1263. [DOI] [PubMed] [Google Scholar]
- Fleming PJ, DiClemente RJ, & Barrington C (2016). Masculinity and HIV: Dimensions of Masculine Norms that Contribute to Men’s HIV-Related Sexual Behaviors. AIDS Behav, 20, 788–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foran HM, & O’Leary KD (2008). Alcohol and intimate partner violence: A meta-analytic review. Clinical Psychology Review, 28, 1222–1234. [DOI] [PubMed] [Google Scholar]
- Fulu E, & Jewkes R (2014). Replicating the UN Multi-Country Study on men and violence: Understanding why some men use violence against women and how we can prevent it. Bangkok, Thailand: Partners for Prevention. [Google Scholar]
- Fulu E, Warner X, Miedema S, Jewkes R, Roselli T, & Lang J (2013). Why do some men use violence against women and how can we prevent it? Findings from the UN Multi-country study on men and violene in Asia and the Pacific. Bangkok: UNDP, UNFPA, UN Women, UNV. [Google Scholar]
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, & Watts CH (2006). Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet, 368, 1260–1269. [DOI] [PubMed] [Google Scholar]
- Gibbs A, Dunkle K, Washington L, Sikweyiya Y, Willan S, Shai N, et al. (2019a). Factors associated with young people’s attendance at an IPV prevention intervention in informal settlements in South Africa: A prospective analysis. Global Public Health, 1–12. [DOI] [PubMed] [Google Scholar]
- Gibbs A, Hatcher A, Jewkes R, Sikweyiya Y, Washington L, Dunkle K, et al. (2019b). Associations between lifetime traumatic experiences and HIV-risk behaviours amongst young men living in informal settlements in South Africa: A cross-sectional analysis and structural equation model. J Acquir Immune Defic Syndr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Vasquez EP, Urrutia MT, Villarruel AM, & Peragallo N (2011). Hispanic women‚Äôs experiences with substance abuse, intimate partner violence, and risk for HIV. Journal of Transcultural Nursing, 22, 46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher AM, Ndlovu N, Colvin C, & Dworkin S (2014). Intimate partner violence among rural South African men: alcohol use, sexual decision-making, and partner communication. Cult Health Sex, epub, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illangasekare S, Burke J, Chander G, & Gielen A (2013). The syndemic effects of intimate partner violence, HIV/AIDS, and substance abuse on depression among low-income urban women. J Urban Health, 90, 934–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Dartnall E, & Sikweyiya Y (2012a). Ethical and Safety Recommendations for Research on the Perpetration of Sexual Violence. Pretoria, South Africa: Sexual Violence Research Initiative, Medical Research Council. [Google Scholar]
- Jewkes R, & Morrell R (2018). Hegemonic masculinity, violence, and gender equality: Using latent class analysis to investigate the origins and correlates of differences between men. Men and Masculinities, 21, 547–571. [Google Scholar]
- Jewkes R, Morrell R, Sikweyiya Y, Dunkle K, & Penn-Kekana L (2012b). Transactional relationships and sex with a woman in prostitution: prevalence and patterns in a representative sample of South African men. BMC public health, 12, 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Sikweyiya Y, Morrell R, & Dunkle K (2011). The relationship between intimate partner violence, rape and HIV amongst South African men: a cross-sectional study. PLoS One, 6, e24256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, & Jooste S (2007). Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci, 8, 141–151. [DOI] [PubMed] [Google Scholar]
- Kane JC, Skavenski Van Wyk S, Murray SM, Bolton P, Melendez F, Danielson CK, et al. (2017). Testing the effectiveness of a transdiagnostic treatment approach in reducing violence and alcohol abuse among families in Zambia: study protocol of the Violence and Alcohol Treatment (VATU) trial. Glob Ment Health (Camb), 4, e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyt R (2012). Constructing hegemonic masculinities in South Africa: The discourse and rhetoric of heteronormativity. Gender and Language, 6, 47–77. [Google Scholar]
- Mahajan S (2014). Economic of South African townships: special focus on Diepsloot. A World Bank study. Washington DC: World Bank Group. [Google Scholar]
- Mankowski ES, & Maton KI (2010). A community psychology of men and masculinity: historical and conceptual review. Am J Community Psychol, 45, 73–86. [DOI] [PubMed] [Google Scholar]
- Mendenhall E (2014). Syndemic suffering in Soweto: violence and inequality at the nexus of health transition in South Africa. Annals of Anthropological Practice, 38, 300–316. [Google Scholar]
- Mendenhall E (2016). Syndemic Suffering: Rethinking Social and Health Problems among Mexican Immigrant Women. Understanding and Applying Medical Anthropology, 164. [Google Scholar]
- Meyer JP, Springer SA, & Altice FL (2011). Substance abuse, violence, and HIV in women: a literature review of the syndemic. Journal of Women’s Health, 20, 991–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CD, Nkowane AM, et al. (2006). Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med, 62, 217–227. [DOI] [PubMed] [Google Scholar]
- Morrell R, Jewkes R, & Lindegger G (2012). Hegemonic Masculinity/Masculinities in South Africa Culture, Power, and Gender Politics. Men and Masculinities, 15, 11–30. [Google Scholar]
- MRC. (2010). War at Home: Preliminary findings of the Gauteng Gender Violence Prevalence Study Johannesburg,: Gender Links and the Medical Research Council. [Google Scholar]
- Mushongera D, Zikhali P, & Ngwenya P (2017). A multidimensional poverty index for Gauteng province, South Africa: evidence from Quality of Life Survey data. Social Indicators Research, 130, 277–303. [Google Scholar]
- Nyanzi S, Nyanzi-Wakholi B, & Kalina B (2009). Male Promiscuity The Negotiation of Masculinities by Motorbike Taxi-Riders in Masaka, Uganda. Men and Masculinities, 12, 73–89. [Google Scholar]
- Okafor CN, Christodoulou J, Bantjes J, Qondela T, Stewart J, Shoptaw S, et al. (2018). Understanding HIV Risk Behaviors Among Young Men in South Africa: A Syndemic Approach. AIDS Behav. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peberdy S, Harrison P, & Dinath Y (2017). Uneven spaces: core and periphery in the Gauteng City-Region. Johannesburg: Gauteng City Regional Observatory, University of the Witwatersrand and University of Johannesburg. [Google Scholar]
- Peralta RL, Tuttle LA, & Steele JL (2010). At the intersection of interpersonal violence, masculinity, and alcohol use: The experiences of heterosexual male perpetrators of intimate partner violence. Violence against women, 16, 387–409. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, & Barker G (2008). Measuring attitudes towards gender norms among young men in Brazil: Development and psychometric evaluation of the GEM scale. Men and Masculinities, 10, 322–338. [Google Scholar]
- Raj A, Santana MC, La Marche A, Amaro H, Cranston K, & Silverman JG (2006). Perpetration of intimate partner violence associated with sexual risk behaviors among young adult men. Am J Public Health, 96, 1873–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich EP, Nkosi S, & Morojele NK (2015). Masculinities, alcohol consumption, and sexual risk behavior among male tavern attendees: A qualitative study in North West Province, South Africa. Psychology of Men & Masculinity, 16, 382. [Google Scholar]
- Russell BS, Eaton LA, & Petersen-Williams P (2013). Intersecting epidemics among pregnant women: alcohol use, interpersonal violence, and HIV infection in South Africa. Current HIV/AIDS Reports, 10, 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Blashill AJ, Lee JS, O’Cleirigh C, Tomassili J, Biello KB, et al. (2018). Condom-use self-efficacy as a mediator between syndemics and condomless sex in men who have sex with men (MSM). Health Psychol, 37, 820–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santana MC, Raj A, Decker MR, La Marche A, & Silverman JG (2006). Masculine gender roles associated with increased sexual risk and intimate partner violence perpetration among young adult men. J Urban Health, 83, 575–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Feldbau-Kohn S, Slep AMS, & Heyman RE (2001). Risk factors for male-to-female partner physical abuse. Aggression and violent behavior, 6, 281–352. [Google Scholar]
- Singer M (2006). A dose of drugs, a touch of violence, a case of AIDS, part 2: Further conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology, 34, 39. [Google Scholar]
- Singer M, Bulled N, Ostrach B, & Mendenhall E (2017). Syndemics and the biosocial conception of health. The Lancet, 389, 941–950. [DOI] [PubMed] [Google Scholar]
- Singer M, & Clair S (2003). Syndemics and Public Health: Reconceptualizing Disease in Bio-Social Context. Medical Anthropology Quarterly, 17, 423–441. [DOI] [PubMed] [Google Scholar]
- Stall R, Coulter RW, Friedman MR, & Plankey MW (2015). Commentary on “Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept” by A. Tsai and B. Burns [DOI] [PubMed]
- Statistics South Africa. (2012). Statistical release (Revised) Census 2011. Statistics South Africa Pretoria
- Stith SM, Smith DB, Penn CE, Ward DB, & Tritt D (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10, 65–98. [Google Scholar]
- Tomori C, McFall AM, Solomon SS, Srikrishnan AK, Anand S, Balakrishnan P, et al. (2018). Is there synergy in syndemics? Psychosocial conditions and sexual risk among men who have sex with men in India. Soc Sci Med, 206, 110–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Jewkes R, Mathews C, Johnston LG, Flisher AJ, Zembe Y, et al. (2011a). HIV risk behaviours and their relationship to intimate partner violence (IPV) among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Behav, 15, 132–141. [DOI] [PubMed] [Google Scholar]
- Townsend L, Ragnarsson A, Mathews C, Johnston LG, Ekstrom AM, Thorson A, et al. (2011b). “Taking care of business”: alcohol as currency in transactional sexual relationships among players in Cape Town, South Africa. Qual Health Res, 21, 41–50. [DOI] [PubMed] [Google Scholar]
- Townsend L, Rosenthal SR, Parry CD, Zembe Y, Mathews C, & Flisher AJ (2010). Associations between alcohol misuse and risks for HIV infection among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Care, 22, 1544–1554. [DOI] [PubMed] [Google Scholar]
- Tsai AC (2018). Syndemics: A theory in search of data or data in search of a theory? Soc Sci Med, 206, 117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, & Burns BF (2015). Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Soc Sci Med, 139, 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, & Venkataramani AS (2016). Syndemics and Health Disparities: A Methodological Note. AIDS Behav, 20, 423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Ulloa EC, Lozada R, Fraga MA, Magis-Rodriguez C, et al. (2011). Injection drug use as a mediator between client-perpetrated abuse and HIV status among female sex workers in two Mexico-US border cities. AIDS Behav, 15, 179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, & Vansteelandt S (2014). Invited commentary: Some advantages of the relative excess risk due to interaction (RERI)--towards better estimators of additive interaction. Am J Epidemiol, 179, 670–671. [DOI] [PMC free article] [PubMed] [Google Scholar]


