Abstract
Since the first case of COVID-19 traced in India on 30th January, 2020, the total no. of confirmed cases is amplified. To assess the inter-state diversity in spreading potentiality of COVID-19, the exposure, readiness and resilience capability have been studied. On the basis of the extracted data, the outbreak scenario, growth rate, testing amenities have been analysed. The study reflects that there is an enormous disparity in growth rate and total COVID-19 cases. The major outbreak clusters associated with major cities of India. COVID-19 cases are very swiftly amplifying with exponential growth in every four to seven days in main affected states during first phase of lockdown. The result shows the vibrant disproportion in the aspects of, hospital bed ratio, coronavirus case-hospital bed ratio, provision of isolation and ventilators, test ratio, distribution of testing laboratories and accessibility of test centres all over India. The study indicates the sharp inequality in transmission potentiality and resilience capacity of different states. Every state and union territory are not well-prepared to contain the spreading of COVID-19. The strict protective measures and uniform resilience system must be implemented in every corner of India to battle against the menace of COVID-19.
Keywords: COVID-19, Vulnerability, Inter-state diversity, Outbreak clusters
Highlights
-
•
Major outbreak clusters are associated with major cities of India.
-
•
The growth rate of COVID-19 positive case in India started to slow down and recovery rate is near 50%.
-
•
Covid-19 test rate is still very low in Bihar, Jharkhand, West Bengal and Uttar Pradesh
-
•
Inter-state variations in preparedness and resilience to fight with COVID-19.
1. Introduction
A new respiratory tract infectious disease COVID-19 caused by coronavirus −2019 has emerged out of the city of Wuhan, China [ 1 ] in December 2019, which has already spread worldwide with its deadly effect. Suddenly, it has been transformed into an extraordinary catastrophe towards the world's geopolitical scenario, economic structure and health system [ 2 ]. The magnitude of its aftermath is extraordinary [ 3 ]. Reuters has released a statement of UN Secretary-General, where he has warned that the world will encounter the most challenging emergency situation since World War II with COVID19. On 30th January 2020, World Health Organization (WHO) announced this health disaster as Public Health Emergency of International Concern (PHEIC) and ultimately on 11th March 2020, WHO has considered this disease as a pandemic. This emergency situation has an extensive worst impact on the national economy, social and psychological issues as well as on the international affairs of every affected territories [ 4 ]. WHO has coined a new term ‘infodemic’ [ 5 ] and information circulated through social media would traumatize people in several times [ 6 ]. The prime and initial factor of COVID-19 must be identified as a challenge on the basis of humanitarian ground [ 7 ]. WHO has estimated that worldwide 5,934,936 people are confirmed as diseased till 31st May 2020 while 367,166 people have lost their lives across 216 countries in the world. The outbreak of Coronavirus indicates the deficiency of preparedness of several government worldwide [ 8 ]. In this aspect, India is not an exception. As of 31st May 2020, (the ending date of lockdown) a total number of 1,82,143 COVID −19 positive cases are identified including a no. of 5164 deaths. On this particular date, new confirmed cases of 8380 have been registered in India (covid19india.org) and the country is enlisted among the ten worst affected countries all over the world.
Worldwide all the countries must be united to adopt collaborative measures for enclosing Coronavirus 2019 [ 9 ]. The system of social isolation, quarantine and restriction of physical contact must be prioritized to regulate COVID-19 pandemic [ 10 ]. Range of social distance interventions can make a control on outbreak of the disease and it is seen in Korean case [ 11 ] and more strict prevention and control measures should be taken to slow down the spread of COVID-19 [ 12 ]. Early enforcement of strict intervention would dwindle the no. of positive cases, rapid growth rate and moreover to reduce the pressure on health services so that it can resilience quickly [ 13 ]. India has already adopted necessary efforts to build resilience against this disease including implementation of Epidemic Disease Act- 1897, travel related restrictions, diplomatic gatherings [ 14 ], closure of religious institutions [ 15 ], public curfew, countrywide lockdown in four phases (25 March – 31 May 2020), maintenance of social distancing [ 16 ], awareness campaigning through mass media etc. The govt. and private hospitals are continuously trying their best to arrange isolation wards, home quarantines, ventilators, testing kits under the continuous monitoring of administration as curative steps to control the spread of infection and execute essential diagnosis.
In this context, the fact is noteworthy that every state of India is not equally well-equipped with adequate medical infrastructure to provide necessary health care facilities to the COVID-19 patients. Proper medical amenities are highly inaccessible especially to the citizens residing in the remote areas of different states across the country. The inequal service of health sector in various states promote to flourish the rate of contagion countrywide. The low testing rate, deficiency and miserable condition of quarantine centres, rejection of hospitals for admitting patients, scarcity of ventilation systems – are the regular hazardous phenomena of India surging the country's gross no. of positive COVID-19 cases. The fact is evident that the present alarming situation of India is a definite outcome of sharp interstate disparity in the aspect of necessary remedial readiness and resilience capability to combat against COVID-19. Existing gaps in healthcare infractures and socioeconomic vulnerabilities may lead to sharp jump in outbreak of the virus [ 17 ] Therefore, the assessment of interstate discrepancy in coronavirus outbreak rate and medical accommodations are explicitly imperative to detect the disparity of transmission capability of the states all over India. This study is very crucial not only to focusing the current situation but to also gaining comprehensive idea about the near future scenario and make necessary preparedness to cope with the situation. This paper aims to highlight the inter-state variations in transmission potential of COVID-19 and to assess the exposure, preparedness and resilience capacity in different states in India.
2. Materials and methods
2.1. Data
The present study is based on secondary data sources. State and district wise data regarding the confirmed case of COVID-19 and test records from 30th January to 31st May 2020 have been collected from publicly available portal of covid19india.org. The data is validated by a group of volunteers.
Census of India's report has been used to obtain the state wise population of 2020. COVID-19 test centres locational information has been gathered from the Indian Council of Medical Research (ICMR) official bulletin (01 April 2020). National Health Profile - 2019 report has been used to obtain the state wise hospital bed, per capita health expenditure, poverty ratio and aged population (above 60 years). Slum household information has been gathered from Census of India (2011) slum house section. Several newspaper reports have also been used to interpret the problem in different states and union territories in India.
2.2. Methods
COVID-19 positive case growth rate in different states and Union territories are calculated based on the confirmed cases of present day and previous day. The median values of the growth rate of all phases of lockdown have been identified. Location of COVID-19 test laboratories are mapped and 100 km buffer zone of each laboratories are identified to analyse the accessibility of testing laboratories in different parts of India. Area, which are not covered by 100 km buffer zone is marked with yellow colour to identify the inaccessible zone or the zone of very hard to access the nearest test centres. COVID-19 test ratio (test per 1000 per persons) has been estimated by considering the state wise total number of samples tested till 31st May 2020 and projected population of 2020.
State wise available hospital beds (Government hospitals only) and projected population data are used to calculate the availability of hospital bed ratio in different states. To identify states wise potential for hospital shortages, the COVID-19 confirmed cases and hospital bed ratio has also been calculated. Confirmed cases per 1000 persons in different states have been identified on the basis of projected population (2020) and total confirm cases as of 31st May 2020. Finally, the ratio of confirmed cases (case per 1000 persons) and hospital bed (bed per 1000 persons) are identified. A scatter diagram is prepared to show the relationship between slum population and total positive case.
3. Indian scenario
The first COVID −19 case in India was identified at Thrissur, Kerala on 30th January 2020 and the infected people have returned from Wuhan in China. Followed by the first case, it was restricted to only up to 06 no. of cases till 9th March 2020. However, the number of confirmed cases started to increase and reached to 50 confirmed cases on 11th march and it touched the fig. 1001 on 30th March. Since 31st March, total confirmed case started to jump at exponential rate and it reached to 11,485 confirmed cases including 396 deaths as of 14th April 2020, the end of first lockdown phase ( Fig. 1 ). Till the end of all lockdown phases, 190,648 confirmed case have been reported including 5407 deaths. Maximum case has been reported from the state of Maharashtra (67655) and it is followed by Tamil Nadu (122333), Delhi (19844), Gujrat (16794), Rajasthan (8831) and Madhya Pradesh (8089. These six states share about 75% of total positive case. The North Eastern states shows highly expectant situation with very low no. of positive case. Among the North eastern states, Assam (1340) has reported maximum confirmed cases; while Mizoram [11], Manipur (72), Tripura (316), Arunachal Pradesh [4], Nagaland (43), Meghalaya (27) and Sikkim [1] have reported very minimal confirmed cases with less than 01% of the total positive cases.
Fig. 1.
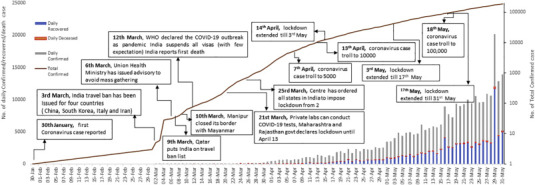
Epidemiologic curve describing daily confirmed, recovery and death cases in India with landmark of major policy/recommendations.
The major outbreak clusters are observed in Western, Southern and North Western part of India. Most of the outbreak hotspots are the major cities like Mumbai, Pune, Thane, Chennai, Delhi, Hyderabad, Jaipur, Indore, Bhopal, Ahmedabad, Bengaluru, with huge population. Four major metropolitan clusters- Delhi, Mumbai, Kolkata and Chennai account for nearly 40% of the total Covid-19 positive cases in India. The districts with more than 500 COVID-19 cases can be recognized as major outbreak clusters and this category includes 57 districts (7.92%) across the country.
Although, Kerala has encountered the first COVOD −19 positive case, but the infection curve was almost flattened with maximum recovery rate (96%) during the second phase of lockdown. But at the end of all lockdown phases (31st May 2020), the scenario has become changed and maximum recovery rate is found in Punjab (88%) followed by Rajasthan (68%), Chhattisgarh (67%), Andhra Pradesh (65%); while Delhi (43%) Jharkhand (40%), Bihar (40%), West Bengal (39%), Kerala (38%) show slow rate of recovery. Recovery rate at national level is counted as 48.18% (Indian Council of Medical Research report). The stated facts revels that there is sharp inter-state variation in outbreak and recovery of the disease and these are related to the response and resilience capacity of the states.
3.1. Coronavirus spreading rate
COVID-19 case in India shows a rapid increasing trend with exponential growth in every four to seven days in major affected states during the first phase of lockdown. Daily COVID-19 data of all the states in India portray huge disparity in number of cases as well as in growth rate. Median value of growth rate at national level is found 13.74, 6.88, 5.58 and 4.88 during first, second, third and fourth phases of lockdown respectively. During the first phase, the states of Madhya Pradesh, Maharashtra, Gujarat, Delhi, Jammu and Kashmir accounted above the national level whereas, some other major states i.e. Bihar, West Bengal, Karnataka, Orissa, Kerala, Assam witnessed very steady growth rate (Fig. 2 ). However, after the end of all lockdown phases (i.e. 31st May 2020) growth rate curve shows declining trends in the states of Punjab, Andhra Pradesh, Gujrat, Madhya Pradesh, Telangana, Rajasthan and Utter Pradesh indicating significant lowering of growth rate ( Fig. 2 ). Some previous study [ 18 ] shows the doubling of the COVID-19 cases in every six days, but this estimation is mismatched in Indian scenario as the total positive cases are immensely disproportionate in different states all over India.
Fig. 2.
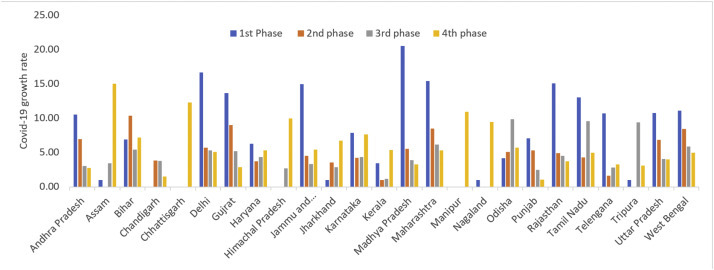
Growth rate of coronavirus case in four lockdown phases (Phase 1: 25 March 2020–14 April 2020 (21 days), Phase 2: 15 April 2020–3 May 2020 (19 days), Phase 3: 4 May 2020–17 May 2020 (14 days) Phase 4: 18 May 2020–31 May 2020 (14 days) in different states. Source: Based on state wise confirmed case, www.covid19india.org
4. Inter-state vulnerability to coronavirus
4.1. Coronavirus case - hospital bed ratio
With the increasing number of coronavirus cases during the last three months creates a fast and massive demand for health care infrastructures. Hospitals in major corona affected states of India have been overturned with coronavirus patients, and the acute shortage of medical equipment is the biggest problem. National Health Profile – 2019 shows that total 735,917 government hospital beds are available in India. The per capita hospital beds in India is 0.55 (per 1000 population) which is noticeably lower than South Korea (11.5), France (6.5), China (4.2) and Italy (3.4) [ 19 ]. The Health Ministry of India has confirmed that 63% casualty have been recorded among the age group of above 60 years whereas 30% death is reported within the age group of 40–60 years. According to WHO, the older population is explicitly identified as vulnerable group to the menace of coronavirus infection. The availability of beds for elderly population in India is 5.18 per 1000 old population.
In terms of availability of hospital beds, 12 states (which are home to 70% population) lie below the national level (0.55 beds per 1000 population). The states of Manipur, Assam, Maharashtra, Odisha, Haryana, Madhya Pradesh, Chhattisgarh, Uttar Pradesh, Gujarat, Jharkhand, Andhra Pradesh and Bihar portray the underprivileged status in this scenario (Fig. 3 ). In terms of beds per 1000 of elderly population, North eastern and Southern states are better-off in this category while Northern and Central India's states have relatively low availability of government hospital beds for elderly population [ 20 ].
Fig. 3.
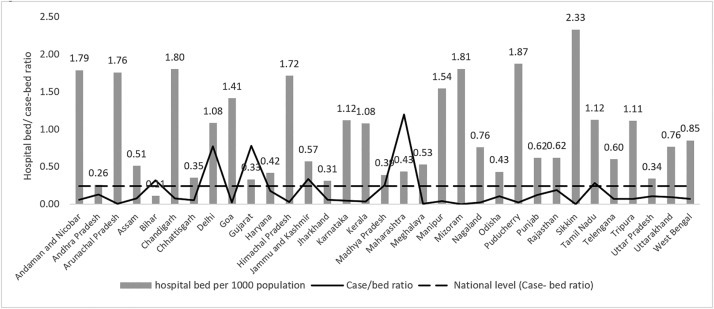
Government hospital bed per 1000 population (2020) and COVID 19 confirmed case (till 16th April) and Hospital bed ratio (case-bed ratio) in different states and UTs in India. Source:www.covid19india.org, National Health profile 2019 and Census of India.
Ratio of coronavirus case to hospital bed is one of the best indicator to identify the states experiencing more coronavirus case with relatively fewer hospital bed. Higher ratio value indicates more cases in respect to available hospital beds to the respective states. The maximum ratio is found in Maharashtra (1.2) followed by Delhi (0.77) and Gujarat (0.77); whereas the North-eastern and eastern states highlight very low ratio (Fig. 3) with remarkably less potential to hospital bed shortage at present scenario. The national ratio is found 0.24 as of 31st May 2020.
Furthermore, isolated bed is the elementary requirement for all coronavirus patients. Like others health care equipment, there is huge disparity in availability of isolation beds in major states across the country. The availability of isolation bed per 1000 persons shows that the states of Andhra Pradesh (0.43), Madhya Pradesh (0.36), Tamil Nadu (0.41), Telangana (0.31) are comparatively in better position whereas the Bihar (0.02), Karnataka (0.02), Uttar Pradesh ((0.02) reveals the poor scenario.
4.2. COVID-19 test ratio
To understand the actual scenario of coronavirus and to know whether the current interventions are adequate or falling short, appropriate data of various administrative unit all over the country in temporal basis is required. Test ratio per thousand people in India is very low (3.19) in respect to Italy (64.15), South Korea (17.77), United Kingdom (41.70) as of 31st May 2020 (https://ourworldindata.org).The number of COVID-19 cases in India are continuing to increase very rapidly, therefore more testing is required in the country. At present in India, ICMR-approved laboratories have a capacity of around 125,000 tests per day and till 31st May, 3,737,027 nos. of samples have been tested (ICMR report). Among the major states, Bihar has tested minimum number of samples (75737) where 110 million people are living. In terms of test ratio, Jammu and Kashmir represents the highest position (13.27) among all states and union territories followed by Goa (8.98), Delhi (8.93), Andhra Pradesh (6.98) and Tamil Nadu (6.96). Inter-sate variation in COVID-19 test ratio is shown in Fig. 4 .
Fig. 4.
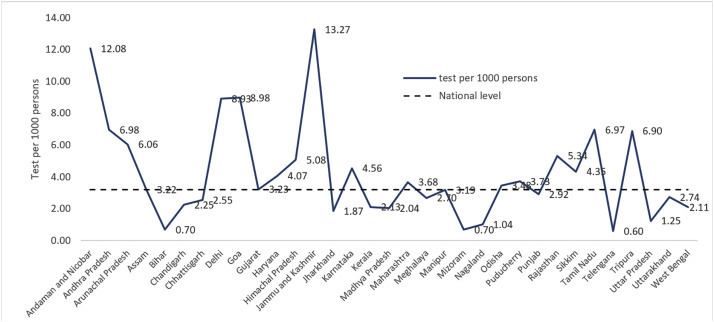
No. of test per 1000 persons in Major states / UTs till 16th April 2020. Source: COVID19India: Patient Database, state wise test data.
4.3. Distribution of test laboratories and accessibility gap
The study reflects another striking fact of unequal distribution of testing centres all over the country. The Department of Health Research under Indian Council of Medical Research (ICMR) has confirmed that there are 126 govt. approved and supported testing laboratories as of 1st April 2020 and 51 private laboratories for COVID-19 as of 31st March 2020 in India. Maharashtra has maximum number of COVID- 19 test laboratories [23] followed by Tamil Nadu [16], Delhi [14], Telangana [14], Kerala [12], Gujarat [10], Karnataka [9], Uttar Pradesh [9] and Rajasthan [8]. Shortage of testing laboratories in several states (e.g. Chandigarh, Chhattisgarh, Goa, Himachal Pradesh, Jharkhand, Manipur, Meghalaya, Puducherry, Punjab, Tripura, Andaman and Nicobar Islands, Sikkim, Ladakh, Arunachal Pradesh etc.) is a matter of serious concern in the aspect of detecting COVID-19 positive cases.
In India, 56.56% area is falling under 100 km. buffer zone of different testing centres and this 100 km buffer area may be considered as maximum limit of accessibility without considering the geographical factors of regional accessibility (Fig. 5 ). The map shows that the extension of testing related service is maximum in the Southern part of the country. Moreover, the Western coastal region and the portion of North, North-west India are well-covered with the services of testing labs. But on the other side, the parts of the Eastern, Central, extreme Northern India are mostly uncovered in this context which increase the magnitude of vulnerability of the people residing in these particular regions.
Fig. 5.
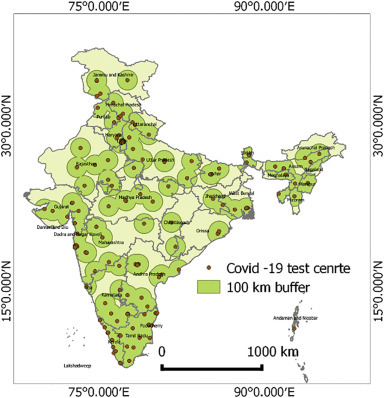
Distribution of COVID-19 test centres and identification of test centre accessible (green colour) and zone (yellow colour) gap. Source: Indian Council of Medical Research. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4.4. Slum population
Slum area is characterised by high population density and shared access to basic amenities which makes them extremely vulnerable for spreading of the coronavirus. The urban population density is conducive to the clustering effect of virus transmission [ 21 ]. Census data (2011) shows that 42% population of India live in slum area. The city Mumbai, which is the most COVID-19 affected city in India, has the largest share of slum dwellers among the big cities. Census data (2011) of India represents that about 50% of slum households accommodate themselves within one single room. Census (2011) data of slums highlights that 58.37% of the slum households in Maharashtra, which is most badly affected state, have not access a private toilet facility inside their premises and 35.4% slum dwellers are compelled to step out of their premises for collecting required drinking water from public taps, tube wells, and wells. The sates of Maharashtra, Tamil Nadu, West Bengal, Gujarat and Delhi share a considerable no. of slum population and hence they have a large no. of COVID-19 positive case (Fig. 6 ).
Fig. 6.
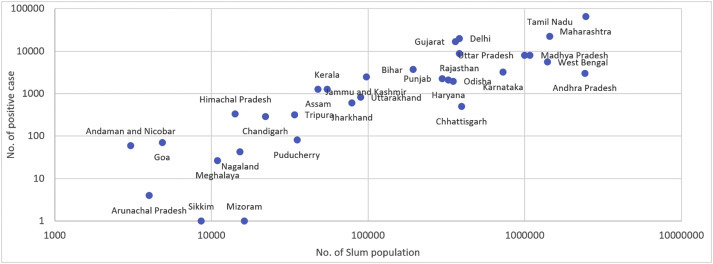
Slum population with no. of COVID-19 positive case till 31 May 2020 in different states.
(Source: Census of India 2011, Slum house, Households amenities and assets.)
Major findings form the above discussions can be summarized in following table-.
Major findings
|
5. Conclusion
Since the first COVID-19 case reported on 20th January 2020, spreading pace is not uniform throughout the county. Presently in India, the intensity of severity and casualty are increasing daily in a steady rate and yet to reach at the peak. The Govt. of India has already issued strict interventions to build resilience for tackling COVID-19 crisis. But there is a sharp disparity among the states and union territories in the ground of hospital beds, ICU units, testing laboratories, ventilators, isolation wards, quarantine arrangements, health expenditure etc. The existing remedial measures are considered to be insufficient in several states according to their present demographic status, socio-economic structure, day-wise increasing trend of positive cases and rate of fatality. Daily growth rate of confirmed case in different states depict that there is a vibrant contrast among the states in India. Thus, it is very hard to project the probable scenario of coronavirus case in different states with fixing a same model in all states.
In this context, the govt. should adopt priority-basis essential actions on the basis of the continuous monitoring of the severity of outbreak hotspots located in different states. Close monitoring and continuous evolution are needed to provide actionable information to the vulnerable populations [ 22 ]. Community-dependent disaster managing system and preparation [ 23 ] is significant to diminish the resultant fatalities and damages [ 8 ]. Although, the present study identifies the outbreak hotspot at district, scaling up of hotspot area identification to village or municipality (local administrative unit) may help to better monitoring system. Most emphasis should be given to enhance the testing activities of the suspected people and enforce them to stay isolated. A strategy of community quarantine could be helpful to prevent the people being exposed to the virus [ 21 ]. The accurate and updated information of every districts across the country must be circulated to prevent the spreading of coronavirus contagion and to build resilience against this disease. So, the development of proportionate resilience system in every part of India is a mostly crucial issue, which can support to achieve speedy and sustainable retrieval from the menace of COVID-19.
Ethical approval
Not applicable.
Author contributions
Kapil Ghosh: Conceptualization, Methodology, Writing – original draft, Writing – review and editing. Nairita Sengupta: Formal analysis, Writing - original draft, Writing – review and editing. Dipanwita Manna: Formal analysis, Writing - original draft, editing. Sunil Kumar De: Conceptualization, Methodology, Writing - original draft, Writing -review and editing.
Major organisations’ website accessed
Census of India. http://censusindia.gov.in/2011-Common/CensusData2011.html.
Coronavirus update. https://www.covid19india.org
Indian council of Medical Research (ICMR). https://icmr.nic.in/content/covid-19
National Health Profile. http://www.cbhidghs.nic.in/showfile.php?lid=1147
Coronavirus pandemic: daily updated research and data. https://ourworldindata.org.
Funding source
None.
Declaration of Competing Interest
The authors declare no conflicts of interest.
References
- 1.Chen S., Yang J., Yang W., Wang C., Barnighausen T. Covid-19 control in China during mass population movements at new year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Djalante R., Lassa J., Setiamarga D., Sudjatma A., Indrawan M., Haryanto B. Review and analysis of current responses to COVID-19 in Indonesia: Period of January to March 2020. Progress in Disaster Science. 2020;Vol 6(100091):1–9. doi: 10.1016/j.pdisas.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UN . 2020. Launch of global humanitarian response plan for COVID-19. [Google Scholar]
- 4.Hua J., Shaw R. Corona virus (COVID-19) “Infodemic” and emerging issues through a data Lens: the case of China. Int. J. Environ. Res. Public Health. 2020;Vol. 17(2309):1–12. doi: 10.3390/ijerph17072309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaroncostas J. How to fight an Infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaw R., Kim Y.K., Hua J. Governance, technology and citizen behaviour in pandemic: lessons from COVID-19 in East Asia. Progress in Disaster Science. 2020;6(100090):1–11. doi: 10.1016/j.pdisas.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mckinsey . 2020. Coronavirus COVID-19: Facts and Insights. [Google Scholar]
- 8.Djalante R., Shaw R., Dewit A. Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai framework. Progress in Disaster Science. 2020;6(10080):1–7. doi: 10.1016/j.pdisas.2020.100080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao W., Zhang J., Meadows M.E., Liu Y., Hua T., Fu B.A. Systematic approach is needed to contain COVID-19 globally. Sci. Bull. 2020;65 doi: 10.1016/j.scib.2020.03.024. 878–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the post pandemic period. Science. 2020 doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shim E., Tariq A., Choi W., Lee Y., Chowel G. Transmission potential and severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuan J., Li M., Lv Gang, Lu K. Monitoring transmissibility and mortality of COVID-19 in Europe. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Economic Forum . 2020. How fast is coronavirus spreading? (March 2020) [Google Scholar]
- 14.Sharfuddin S.A. Vol. 1(2) 2020. CHOGM under COVID cloud. The Round Table, The Commonwealth Journal of International Affairs. [DOI] [Google Scholar]
- 15.Alyanak O. Faith, politics and the COVID-19 pandemic: the Turkish response. Med. Anthropol. 2020 doi: 10.1080/01459740.2020.1745482. [DOI] [PubMed] [Google Scholar]
- 16.Manderson L., Levine S. COVID-16, risk, fear and fall-out. Med. Anthropol. 2020 doi: 10.1080/01459740.2020.1746301. [DOI] [PubMed] [Google Scholar]
- 17.McAleer M. Prevention is better than the cure: risk management of COVID-19. J. Risk Financial Manag. 2020;13(3):46. doi: 10.3390/jrfm13030046. [DOI] [Google Scholar]
- 18.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225) doi: 10.1016/S0140-6736(20)30260-9. 697–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ray D., Bhattacharya R., Wang L., Salvator M., Mohammed S., Halder A. Predictions, Role of Interventions and Effects of a Historic National Lockdown in India’s Response to the the COVID-19 Pandemic: Data Science Call to Arms. Data Science Review. 2020;(Special Issue 1):1–65. doi: 10.1162/99608f92.60e08ed5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh P, Ravi S,Chakraborty S. COVID-19, Is India's health infrastructure equipped to handle an epidemic?(2020), //www.brookings.edu/blog/up-front/2020/03/24/is-indias-healthinfrastructure-equipped-to-handle-an-epidemic/.
- 21.Zhu W., Li X., Wu Y., Xu C., Li L., Yang J. Community quarantine strategy against coronavirus disease 2019 in Anhui: an evaluation based on trauma center patients. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heymann D.L., Shindo N., Scientific W.H.O. Technical advisory Group for Infectious H. COVID19: what is next for public health? Lancet. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen K.M. Community-based disaster preparedness and climate adaptation: local capacity building in the Philippines. Disasters. 2006;30(1):81–101. doi: 10.1111/j.14679523.2006.00308.x. [DOI] [PubMed] [Google Scholar]


