Highlights
-
•
COVID-19 infection could led to a pro-inflammatory and pro-thrombotic state.
-
•
Cerebrovascular involvement may occur in COVID-19 infection even in young patients.
-
•
Physicians should be aware that stroke may be the first COVID-19 manifestation.
Keywords: Coronavirus, COVID-19, Prothrombotic state, Stroke, Vertebrobasilar disease
Dear Editor,
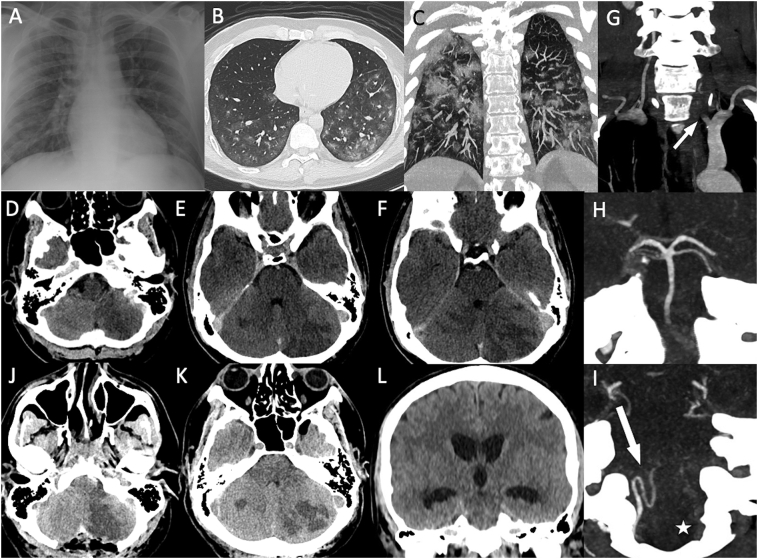
A 33-years-old man was admitted to the Emergency Department (ED) on March 23, 2020 because of the acute onset of occipital headache, retching and balance disorder. In the last 10-days he complained cough and occasional fever. Arterial blood gas analysis revealed only mild hypoxemia. Blood test showed increased C-reaction protein (CRP) (2.90 mg/dl; NR 0–0.5 mg/dL), mild thrombocytosis (454,000/μL; NR 150,000-450,000/μL) and elevated lactate dehydrogenase (LDH) (573 U/L; NR 208–378 U/L). Brain computed tomography (CT)-scan was unremarkable, while chest-X-Ray showed bilateral basal patchy airspace opacities (Fig. 1, A). High resolution CT chest scan confirmed the presence of bilateral ground-glass opacities compatible with interstitial lung disease (Fig. 1, B—C). A diagnosis of acute interstitial pneumonia suggestive for COVID-19 infection was made and the patient was hospitalized in the COVID Unit. A treatment with hydroxychloroquine (400 mg/day) together with Danuravir (800 mg/daily) and Fondaparinux 2.5 mg/daily subcutaneously was started. Seven hours later during routine morning visit in the COVID Unit the attending physician reported no changes in respiratory function, but the patient was drowsy with slurred speech and left lateral gaze palsy. Headache worsened and he was not able to flex his head without vomiting. Brain CT-scan revealed the presence of bilateral cerebellar ischemic lesions in the territories of the left posterior inferior cerebellar artery (PICA), bilateral anterior inferior cerebellar artery (AICA) and bilateral superior cerebellar artery (SCA) (Fig. 1, D-F). CT-angiography (CTA) demonstrated an abrupt opacification cutoff in the preforaminal segment V1 of the left vertebral artery (VA) with a subsequent occlusion of the vessel lumen up to V4 intracranial segment (Fig. 1, G-I), associated with an abrupt opacification cutoff of left PICA and AICA bilaterally, highly suggestive for intraluminal thrombosis. Blood test examination were repeated showing an inflammatory response and hypercoagulable state as suggested by the increased CRP (2.76 mg/dl), increased D-dimer (3728 ng/ml; NR < 250 ng/mL), mild thrombocytosis (466,000/μL), increased fibrinogen (486 mg/dL) and elevated LDH (558 U/L). Two nasopharyngeal swabs were positive for SARS-CoV-2 on rRT-PCR assay. Because of the fast deterioration, the patient underwent a urgent neurosurgical decompression of the posterior cranial fossa (Fig. 1, J, K). The patient was then transferred to the Intensive Care Unit requiring invasive mechanical ventilation but after two days an external ventricular drainage was placed because a new brain CT scan shown triventricular obstructive hydrocephalus (Fig. 1, L). Currently, on May, 4 the patient is still under invasive mechanical ventilation in the intensive care unit of our Hospital.
Fig. 1.
Chest x-ray performed at admission showed bilateral basal patchy airspace opacities (A). High resolution CT chest scan revealed the presence of bilateral ground-glass opacities compatible with interstitial lung disease with a visual score of approximately 50% of involvement compared to the sum of both lungs (B, C). Brain CT scan revealing the presence of bilateral cerebellar hypodensities compatible with ischemic lesions in the territories of the left PICA, bilateral AICA and bilateral SCA (D-F). CTA demonstrated an abrupt opacification cutoff in the preforaminal segment V1 of the left dominant vertebral artery (G, white arrow) with a subsequent occlusion of the vessel lumen up to V4 intracranial segment (I, white star) and a retrograde opacification of the upper basilar artery through posterior communicating arteries (H). Postoperative CT scan performed after the occipital craniectomy showed the presence of the bilateral cerebellar ischemic lesions together and a compression of the fourth ventricle (J,K). Brain CT scan performed two days after the craniectomy showed the presence of triventricular obstructive hydrocephalus (L).
Little is known about central nervous system involvement during COVID-19 infection and the neuroinvasive potential of SARS-CoV-2 [1]. Reported neurological manifestations in COVID-19 patients include: headache, altered consciousness, skeletal muscle damage and cerebrovascular diseases [[2], [3], [4]]. Our case underlines that acute cerebrovascular disorders may represent a possible early phenomenon of COVID-19 infection with a devastating clinical impact and in absence of pre-existing vascular risk factor. This is in line with a recent report of five patients younger than 50 years presented with new-onset symptoms of large-vessel ischemic stroke and affected by a concomitant COVID-19 infection [5]. Moreover, our patient went to the ED only for the appearance of ischemic posterior circulation symptoms (occipital headache, retching and balance disorder) and not for COVID-related respiratory symptoms (at that time the pulmonary involvement was paucisymptomatic). This is an important point considering that headache is a common symptoms in COVID-19 patients (13.1%) [2] underlying the risk that COVID-19 infection could at the same time be responsible but also masking acute neurological conditions in the ED, that are currently struggling with the COVID-19 outbreak. In this setting the risk is that acute headache could be attributable only to the infection and not to an underlying acute neurological condition [2]. The presence of an increased inflammatory response and a hypercoagulable state may represent a potential source of vascular complications in COVID-19 infection, usually occurring 7–14 days after the onset of the infection [6]. Indeed in our patient we found increased values of D-dimer, platelet count, fibrinogen and LDH all indicative of a prothrombotic state that has been previously reported in COVID-19 patients [2,7,8]. D-dimer value greater than 1 μg/mL at admission is associated with fatal outcome of COVID-19 [9]. We did not perform Brain-MRI and MR-Angiography, due to the patient's condition with the need of surgical treatment and ICU admission. This did not allow to exclude the presence of VA dissection as a possible cause of the VA occlusion together with the hypercoagulable state. In conclusion, in COVID-19 infection, stroke may be caused by a pro-inflammatory and pro-thrombotic state not only in the lung parenchyma, directly attached by virus, but also at the systemic level [10]. Physicians should be aware that thrombotic diseases as stroke may be the first manifestation of hospital access of patients with mild COVID-19 infection.
Authorship
Dr. F. Cavallieri: conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the article, final approval of the version to be submitted.
Dr. A. Marti: acquisition of data, analysis and interpretation of data, drafting the article, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. A. Fasano: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. A. Dalla Salda: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. A. Ghirarduzzi: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. C. Moratti: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. L. Bonacini: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. R. Ghadirpour: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. R. Pascarella: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. F. Valzania: acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version to be submitted.
Dr. M. Zedde: conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, final approval of the version to be submitted.
All authors have approved the final article.
Disclosures
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical standards
Due to the severe patient's condition we were unable to obtain written informed consent from the patient and the patient had not any family member.
Declaration of Competing Interest
None.
References
- 1.Sun T., Guan J. Novel coronavirus and central nervous system. Eur J Neurol. 2020 Mar 26 doi: 10.1111/ene.14227. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 2.Mao L., Jin H., Wang M. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 Apr 10 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020 Apr 15;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu K., Pan M., Xiao Z., Xu X. Neurological manifestations of the coronavirus (SARS-CoV-2) pandemic 2019–2020. J Neurol Neurosurg Psychiatry. 2020;91(6):669–670. doi: 10.1136/jnnp-2020-323177. (jnnp-2020-323177) [DOI] [PubMed] [Google Scholar]
- 5.Oxley T.J., Mocco J., Majidi S. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020 Apr 28;382(20) doi: 10.1056/NEJMc2009787. e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li T., Lu H., Zhang W. Clinical observation and management of COVID-19 patients. Emerg Microbes Infect. 2020;9:687–690. doi: 10.1080/22221751.2020.1741327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. (blood.2020006000) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 11;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. (9pii: S0140–6736(20)30566-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hess D.C., Eldahshan W., Rutkowski E. COVID-19-related stroke. Transl Stroke Res. 2020:1–4. doi: 10.1007/s12975-020-00818-9. [DOI] [PMC free article] [PubMed] [Google Scholar]