Abstract
Purpose
Trauma is a major health concern. Length of hospital stay (LOS) has been targeted as an important metric to assess trauma care. This study aims to evaluate the risk factors that affect LOS among trauma patients in a trauma center in Southwestern Iran.
Methods
This cross-sectional study was conducted on patients admitted to Rajaee Trauma Center, Shiraz, Iran between January 1, 2018 and December 30, 2018. The inclusion criteria were age above 15 years and having traffic accident injuries, including car, motorcycle and pedestrian injury mechanisms. The exclusion criteria were existing diseases including cardiovascular, cerebral, renal, and pulmonary diseases prior to this study, dead upon arrival or within 48 h after admission, and stay at the hospital for less than 6 h. The risk variables analyzed for prolonged LOS were age, gender, mechanism of traffic accident injury, infection during hospital stay, type of injury, injury severity score, surgery during hospitalization, and survival. Poisson regression was performed to evaluate the partial effects of each covariate on trauma hospitalization (≥3 days as longer stay).
Results
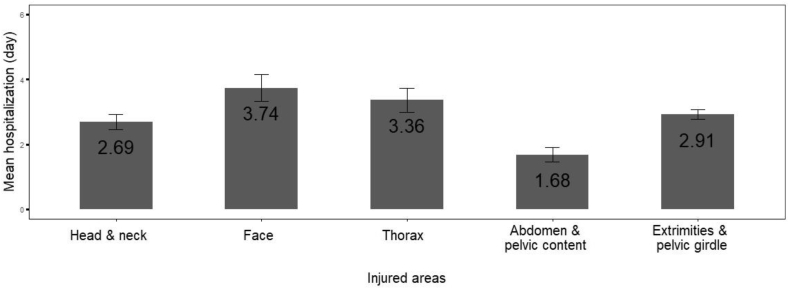
This study was conducted on 14,054 patients with traffic accident injury and the mean age was (33.89 ± 15.78) years. Additionally, 74.35% of the patients were male, with male to female ratio of 2.90. The result of Poisson regression indicated that male patients, higher age, combination of thoracic injuries, onset of infected sites, and surgery patients were more susceptible to have a longer LOS. Considering the site of injury, patients with face injuries followed by those with thorax injuries had the highest means of LOS (3.74 days and 3.36 days, respectively). Simultaneous existence of surgical intervention and infection in a patient had the greatest impact on prolonged LOS.
Conclusion
This study identified that age, gender, mechanism of injury, infection, type of injury, survival, and ISS could lead to prolongation of LOS, but the affect can be reduced by eliminating modifiable risk factors.
Keywords: Length of stay; Trauma; Accidents, traffic; Risk factors
Introduction
Trauma is a major health problem and the fourth leading cause of death worldwide, affecting all age groups.1,2 Trauma patients occupy one out of every eight hospital beds and traumatic injuries kill more than 165,000 patients per year in the United States.3 In Iran, trauma is the second leading cause of death in all age groups. Hence, considerable attentions must be given to trauma care and extreme caution must be taken.4
Length of hospital stay (LOS) is targeted as an important metric to assess trauma care.5 Early intervention and reduced LOS have been long believed to improve the outcomes in trauma patients.6 In this context, some studies have signified the impact that prolonged LOS had on subsequent development of hospital-acquired infections among trauma patients.7 Moreover, reduction in hospital LOS was accompanied with significant reductions in costs.1 Besides, prolonged LOS could lead to waste of resources as well as functional decline.8 Therefore, LOS has been used as an important marker for quality of care, costs, and resource utilization in trauma centers.9
Some studies have declared that a longer LOS amongst trauma patients was associated with an increased hospital mortality, even when controlling the anatomic, demographic, and physiologic factors.6 In contrast, some surveys revealed no relation between mortality and LOS.9 In other words, they indicated no differences between the patients with a long or a short LOS with respect to survival rate.10
LOS for trauma patients varies widely and is dependent on numerous factors. Demographic variables, including age, gender, and race, have all been noted to be non-modifiable effective factors in LOS. In comparison to younger trauma patients, older ones had a longer LOS and a greater need for long-term care. In addition, some studies showed that women were more likely to be discharged sooner. Nonetheless, contradictory results were obtained regarding the impact of race and ethnicity on LOS. Although non-white patients were more likely to be discharged sooner in some studies, there were no differences amongst African-American, Hispanic, and Caucasian patients in this regard.11
Moreover, LOS was found to be significantly associated with trauma score and injury severity.3,5 A study4 revealed that injury severity score (ISS) was the best predictor for LOS. Additionally, post-trauma pain was stated to influence LOS. Prior research showed that if pain restricts the patient's ability or pain develops during therapy, slower recovery procedure and increased LOS are likely to occur.11
Surgical interventions can also influence LOS in trauma patients. In a survey, surgical management of hip fractures was associated with reduced LOS in elderly patients.12 In addition, one of the most important predictors of LOS was complications, which were associated with a 62% increase in LOS. Intensive care unit admission, shock, gunshot wounds, brain injuries, and comorbidities were other less important predictors of LOS.9
Currently, there is a lack of knowledge on variations in LOS as well as the predictors of LOS across trauma centers in Iran. Therefore, the present study aimed to evaluate the risk factors that affect LOS in trauma patients in Southwestern Iran.
Methods
Study design and setting
This cross-sectional study was conducted in Rajaee Trauma Hospital, which is the center of emergency medical services for trauma patients in southwestern Iran. This center consists of 7 general wards, 32 beds each; 6 ICUs, 9 beds each; and 2 emergency wards with 20 beds each. This study was ethically approved by Shiraz University of Medical Sciences.
Data collection
This study was conducted on 14,054 trauma patients between January 1, 2018 and December 30, 2018. Patients with injury as their first diagnosis were detected by an expert physician and were enrolled in the study. They were supervised during their hospitalization by expert physicians until death or discharge.
The inclusion criteria of the study were age above 15 years and having traffic accident injuries. Pediatric patients were not included, since this center only admits patients above 15 years of age. The exclusion criteria were having any pre-existing diseases (including cardiovascular, cerebral, renal, and pulmonary diseases), being dead upon arrival or within 48 h after admission, and staying in the hospital for less than 6 h. Road traffic-related injuries were chosen as the main mechanism of injury and all other mechanisms of injury like burns, poisoning, drowning, suicide attempt, asphyxiation, gunshot injuries, and struck by objects were excluded. The injury mechanism was classified as car, motorcycle and pedestrian accidents.
Moreover, the site of injury for every patient was selected based on the highest abbreviated injury scale (AIS) score. It means that a patient may have multiple trauma sites but only the most severe or critical injured site was chosen as the injured site.
The variables that were analyzed and evaluated as risk factors for prolonged LOS included age, gender, mechanism of traffic accident injury, infection during hospital course, type of injury, ISS, surgery during hospitalization, and survival.
Statistical analysis
The data were analyzed using Stata 14 software and the figures were prepared using R 3.4.3 software for Windows. Descriptive data were analyzed using tables, charts, means, and standard deviations, while analytical data were evaluated via Chi-square test and independent t-test. Poisson regression was also used to evaluate the partial effect of independent covariates on the odds ratio of one extra day of hospitalization as the dependent variable. A two-sided p value less than 0.05 was considered to be statistically significant.
Results
The mean age of patients was (33.89 ± 15.78) years, and 74.35% of the patients were male, with male to female ratio of 2.90. Additionally, 1.21% of the patients died during the study period. Moreover, the patients’ median LOS was 2.85 days, interquartile range (IQR) = 1.00 day. The relation between the study variables and LOS is presented in Table 1. Accordingly, age, gender, mechanism of traffic accident injury, infection, type of injury, survival and ISS were significantly related to LOS. For instance, higher age, being male, face injuries and existing nosocomial infection made the patients more prone to have a longer duration of hospitalization (all p < 0.001). Moreover, ISS was higher in patients with longer LOS in comparison to those with shorter ones (χ2 = −5.76, p < 0.001). Finally, 2.20% of the patients who had longer LOS died. In comparison, only 0.84% of patients with shorter LOS died (χ2 = 43.27, p < 0.001).
Table 1.
Univariate variables based on hospital length of stay (n = 14054).
| Variables | Hospital length of stay (d) |
Statistical value | p value | |
|---|---|---|---|---|
| <3 (n = 10,243) | ≥3 (n = 3811) | |||
| Age (mean ± SD) | 33.16 ± 15.30 | 35.85 ± 16.86 | −9.02 | <0.001 |
| Gender | ||||
| Male | 7352 (71.78) | 3098 (81.29) | 131.88 | <0.001 |
| Female | 2891 (28.22) | 713 (18.71) | ||
| Mechanism of injuries | ||||
| Car accident | 5630 (55.78) | 1605 (44.73) | 129.55 | <0.001 |
| Motorcycle accident | 3095 (30.66) | 1375 (38.32) | ||
| Pedestrian accident | 1369 (13.56) | 608 (16.95) | ||
| Infection | ||||
| Yes | 13 (0.13) | 298 (7.82) | 759.66 | <0.001 |
| No | 10,230 (99.87) | 3513 (92.18) | ||
| Location of injuries | ||||
| Head & Neck | 3018 (29.46) | 800 (20.99) | 305.07 | <0.001 |
| Face | 374 (3.65) | 338 (8.87) | ||
| Thorax | 869 (8.48) | 380 (9.97) | ||
| Abdomen & Pelvic | 776 (7.58) | 146 (3.83) | ||
| Extremities | 5206 (50.82) | 2147 (56.34) | ||
| Outcome | ||||
| Alive | 10,157 (99.16) | 3727 (97.80) | 43.27 | <0.001 |
| Death | 86 (0.84) | 84 (2.20) | ||
| ISS (mean ± SD) | 4.45 (5.94) | 7.42 (7.42) | −5.76 | <0.001 |
SD: standard deviation; ISS: injury severity score.
The results of multivariate Poisson regression between the covariates and LOS are presented in Table 2. It should be noted that male gender was 1.18 times more prone to have a longer LOS than female (p < 0.001). Furthermore, LOS had a direct relationship with age. In other words, patients with higher age were more susceptible to stay in hospital for extra days.
Table 2.
Multivariate Poisson regression between the covariates and hospital length of stay (n = 14054).
| Hospital length of stay | Categories | Exp (β)a | p value | 95% CIb for exp (β) |
|
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age (15–44 years) | 45–64 | 1.19 | <0.001 | 1.16 | 1.22 |
| 65 and more | 1.13 | <0.001 | 1.08 | 1.17 | |
| Gender | Male | 1.18 | <0.001 | 1.15 | 1.22 |
| Injury mechanism (pedestrian) | Car accident | 1.02 | 0.08 | 0.99 | 1.05 |
| Motorcycle accident | 1.03 | 0.01 | 1.01 | 1.07 | |
| Injured area (Head & neck) | Face | 0.98 | 0.42 | 0.93 | 1.02 |
| Thorax | 1.32 | <0.001 | 1.27 | 1.37 | |
| Abdomen & pelvic contain | 0.99 | 0.71 | 0.93 | 1.04 | |
| Extremities | 1.06 | <0.001 | 1.04 | 1.09 | |
| ISS (<8) | 9–15 | 1.37 | <0.001 | 1.33 | 1.40 |
| ≥16 | 1.53 | <0.001 | 1.48 | 1.57 | |
| Infection | Yes | 4.48 | <0.001 | 4.39 | 4.66 |
| Surgery | Yes | 5.36 | <0.001 | 1.66 | 1.80 |
Linear regression coefficient.
Confidence interval of B.
In addition, all injured areas were compared to head & neck injuries. The results indicated that the patients with thoracic injuries were 1.32 times more susceptible to a longer LOS in comparison with those with head and neck injuries (p < 0.001). The patients with infected sites were also 4.48 times more prone to a longer LOS in comparison to those without infection (p < 0.001). Moreover, the patients who were under surgical procedures were 5.36 times more susceptible to stay in hospital for one extra day (p < 0.001). Additionally, LOS was significantly longer in patients with higher severity score.
The mean LOS in patients with different injured areas is depicted in Fig. 1. Accordingly, patients with face injuries followed by thorax injuries had the longest LOS (3.74 days and 3.36 days, respectively).
Fig. 1.
Means of hospitalization in patients with different injured areas.
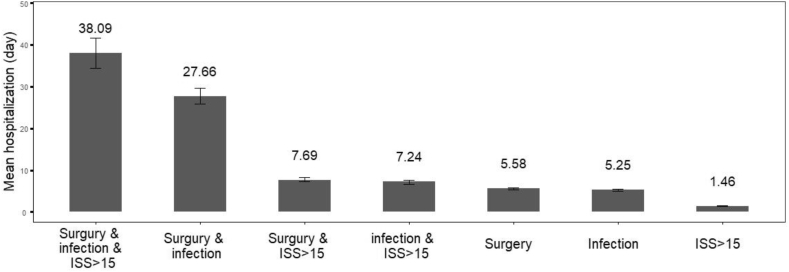
The results of descriptive analysis for the mean LOS based on infection, surgery, and ISS are depicted in Fig. 2. Accordingly, patients with infection, surgery, and ISS >15 had the highest mean of LOS (38.09 days). Moreover, the mean of LOS was 27.66 days among the patients who had infection and underwent surgical procedures simultaneously. Patients who had ISS >15 along with one of the two complications, i.e. surgery and infection had the lowest mean of LOS. Therefore, existence of any surgical intervention with infection in a patient had the highest impact on LOS according to this figure.
Fig. 2.
Descriptive analysis of mean hospitalization based on infection, surgery, and injury severity score.
Discussion
Findings of the present study showed that the LOS of the admitted trauma patients was median 2.85, IQR 1 day, close to what was reported in another study.13 The results also showed that male gender had a bit longer LOS. Another study that investigated the influence of gender on LOS in trauma patients revealed that males were less likely to be discharged sooner.14 In addition, the current study results revealed significant relationship between higher age and prolonged LOS. In confirmation of our results, Brotemarkle et al.11 showed that older trauma patients had longer LOS.
In the present study, the mean LOS was 38.09 days in patients with documented infections along with surgical intervention and ISS >15, which was 27.66 days in patients with infections and surgical intervention. Moreover, infected patients were 4.48 times more prone to stay longer in the hospital in comparison to those without any infections. These findings confirm the great impact of infection on LOS. Our result is consistent with the results of several studies,15,16 showing that infections (such as surgical infections, sepsis, pneumonia, and urinary tract infections) were associated with the greatest LOS and could significantly reduce the rate of discharge. Similarly, a study conducted in Southern-Central United States indicated that nosocomial blood stream infection in adults was significantly related to increased LOS.17 Our recent survey in Iran also showed that The homeless infection that results from hospitalization further leads to increased prolonged hospitalization in trauma patients.18 Another study by Abbasi et al.19 indicated that death following a nosocomial infection was 15 times more likely to happen after 1 week of hospitalization.
The present study results showed that patients who were under surgical procedures were 5.36 times more susceptible to stay in hospital for one day more. On the contrary, a systematic review indicated that operative management of rib fractures and injuries was effective in reducing LOS.20 The observed discrepancies might be attributed to some surgical complications that occurred in our center, which could add 2–3 weeks to LOS.21
Recently, studies have produced contradictory findings regarding the effect of prolonged LOS on mortality. The current study findings show that patients with longer LOS were more prone to die. In contrast to these results and the expectation of high mortality associated with prolonged LOS, another study revealed that injured adult trauma patients who did not die within the first few days and had longer LOS demonstrated a higher ability to survive with an overall survival rate of more than 92%.22 In addition, a study performed in Massachusetts and California revealed that LOS had no significant impacts on death.23
The present study found that LOS was higher in pedestrian and motorcycle accidents compared to car accident injuries. In the same line, a previous study conducted in Iran indicated that longer LOS was associated with being a pedestrian or motorcyclist.24 A recent study in the United States also reported that auto-pedestrian collisions contributed to most delayed discharge from hospitals. These patients experienced 2.3 days of delayed discharge on average.25
Andersen et al.26 showed that increased severity of injury contributed to excessive LOS in acute care settings, which was consistent with another survey27 showing a strong positive correlation between higher ISS and prolonged LOS. Moreover, a study performed on 30,157 trauma patients revealed that patients spent one additional day in ICUs for every five additional points on the ISS.28 As expected, the current study results also proved that the patients with prolonged LOS have significantly higher ISS compared to those with shorter LOS.
In this study, the patients with face and thorax injuries had the highest mean of LOS (3.74 and 3.36 days respectively). In addition, the patients with thorax injuries were 1.32 times more susceptible to hospitalization in comparison to those with head and neck injuries. A study showed that patients with flail chest due to chest injury had a statistically significant increase in both hospital and intensive care unit stay.29 Furthermore, our previous study showed that patients with spinal trauma had a higher LOS in comparison to those without.30
The strength of this study was that it was conducted in a trauma referral center with a large number of trauma patients, which makes the survey more credible. On the other hand, the study had some limitations. For instance, pediatric trauma patients were not included in this study, since this center only accept adult patients. Thus, future studies are recommended to evaluate LOS amongst pediatric trauma patients.
In conclusion, this study identified that age, gender, kinds of accident injury, infection, type of injury, survival, and ISS could affect LOS. Considering the site of injury, the patients with thoracic and face injuries had the highest mean of LOS. Additionally, the nonsurvivors had higher LOS compared to survivors. Thus, LOS can be reduced by eliminating its modifiable risk factors.
Funding
This research was supported with grant number of 1396–01-38-16261 by Shiraz University of Medical Sciences in Shiraz, Iran.
Ethical Statement
This project was approved by the research ethic committee with number of (IR.SUMS.REC.1396.S1028) by Shiraz University of Medical Sciences in Shiraz, Iran.
Acknowledgments
The authors wish to thank Mr. H. Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Declaration of Competing Interest
The authors declare that they have no competing interest.
References
- 1.Fakhry S.M., Couillard D., Liddy C.T. Trauma center finances and length of stay: identifying a profitability inflection point. J Am Coll Surg. 2010;210:817–821. doi: 10.1016/j.jamcollsurg.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 2.Yadollahi M., Zamani M., Jamali K. A survey of accidental fall--induced injuries and mortality in a central trauma hospital in Iran: 2015-2016. Trauma Mon. 2019;24:e14285. doi: 10.5812/traumamon.14285. [DOI] [Google Scholar]
- 3.Weingarten M.S., Wainwright S.T., Sacchetti A.D. Trauma and aging effects on hospital costs and length of stay. Ann Emerg Med. 1988;17:10–14. doi: 10.1016/s0196-0644(88)80494-3. [DOI] [PubMed] [Google Scholar]
- 4.Yousefzadeh Chabok S., Ranjbar Taklimie F., Malekpouri R. Predicting mortality, hospital length of stay and need for surgery in pediatric trauma patients. Chin J Traumatol. 2017;20:339–342. doi: 10.1016/j.cjtee.2017.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore L., Stelfox H.T., Turgeon A.F. Hospital length of stay after admission for traumatic injury in Canada: a multicenter cohort study. Ann Surg. 2014;260:179–187. doi: 10.1097/SLA.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 6.Mowery N.T., Dougherty S.D., Hildreth A.N. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma. 2011;70:1317–1325. doi: 10.1097/TA.0b013e3182175199. [DOI] [PubMed] [Google Scholar]
- 7.Glance L.G., Stone P.W., Mukamel D.B. Increases in mortality, length of stay, and cost associated with hospital-acquired infections in trauma patients. Arch Surg. 2011;146:794–801. doi: 10.1001/archsurg.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore L., Stelfox H.T., Evans D. Hospital and intensive care unit length of stay for injury admissions: a pan-Canadian cohort study. Ann Surg. 2018;267:177–182. doi: 10.1097/SLA.0000000000002036. [DOI] [PubMed] [Google Scholar]
- 9.Shafi S., Barnes S., Nicewander D. Health care reform at trauma centers—mortality, complications, and length of stay. J Trauma. 2010;69:1367–1371. doi: 10.1097/TA.0b013e3181fb785d. [DOI] [PubMed] [Google Scholar]
- 10.Trottier V., McKenney M.G., Beninati M. Survival after prolonged length of stay in a trauma intensive care unit. J Trauma. 2007;62:147–150. doi: 10.1097/01.ta.0000250496.99127.4a. [DOI] [PubMed] [Google Scholar]
- 11.Brotemarkle R.A., Resnick B., Michaels K. Length of hospital stay and discharge disposition in older trauma patients. Geriatr Nurs. 2015;36:S3–S9. doi: 10.1016/j.gerinurse.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Tan S.T., Tan W.P., Jaipaul J. Clinical outcomes and hospital length of stay in 2,756 elderly patients with hip fractures: a comparison of surgical and non-surgical management. Singap Med J. 2017;58:253–257. doi: 10.11622/smedj.2016045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brasel K.J., Lim H.J., Nirula R. Length of stay: an appropriate quality measure? Arch Surg. 2007;142:461–466. doi: 10.1001/archsurg.142.5.461. [DOI] [PubMed] [Google Scholar]
- 14.Liu T., Xie J., Yang F. The influence of sex on outcomes in trauma patients: a meta-analysis. Am J Surg. 2015;210:911–921. doi: 10.1016/j.amjsurg.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell B.G., Ferguson J.K., Anderson M. Length of stay and mortality associated with healthcare-associated urinary tract infections: a multi-state model. J Hosp Infect. 2016;93:92–99. doi: 10.1016/j.jhin.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Ingraham A.M., Xiong W., Hemmila M.R. The attributable mortality and length of stay of trauma-related complications: a matched cohort study. Ann Surg. 2010;252:358–362. doi: 10.1097/SLA.0b013e3181e623bf. [DOI] [PubMed] [Google Scholar]
- 17.Kaye K.S., Marchaim D., Chen T.Y. Effect of nosocomial bloodstream infections on mortality, length of stay, and hospital costs in older adults. J Am Geriatr Soc. 2014;62:306–311. doi: 10.1111/jgs.12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yadollahi M., Kashkooe A., Feyzi M. Risk factors of mortality in nosocomial infected traumatic patients in a trauma referral center in south of Iran. Chin J Traumatol. 2018;21:267–272. doi: 10.1016/j.cjtee.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abbasi H., Bolandparvaz S., Yadollahi M. Time distribution of injury-related in-hospital mortality in a trauma referral center in South of Iran (2010–2015) Medicine. 2017;96:e6871. doi: 10.1097/MD.0000000000006871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuurmans J., Goslings J.C., Schepers T. Operative management versus non-operative management of rib fractures in flail chest injuries: a systematic review. Eur J Trauma Emerg Surg. 2017;43:163–168. doi: 10.1007/s00068-016-0721-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osler T.M., Rogers F.B., Hosmer D.W. Estimated additional hospital length of stay caused by 40 individual complications in injured patients: an observational study of 204,388 patients. J Trauma Acute Care Surg. 2013;74:921–925. doi: 10.1097/TA.0b013e31827e1d5e. [DOI] [PubMed] [Google Scholar]
- 22.Kisat M.T., Latif A., Zogg C.K. Survival outcomes after prolonged intensive care unit length of stay among trauma patients: the evidence for never giving up. Surgery. 2016;160:771–780. doi: 10.1016/j.surg.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 23.Cleary P.D., Greenfield S., Mulley A.G. Variations in length of stay and outcomes for six medical and surgical conditions in Massachusetts and California. J Am Med Assoc. 1991;266:73–79. [PubMed] [Google Scholar]
- 24.Haghparast-Bidgoli H., Saadat S., Bogg L. Factors affecting hospital length of stay and hospital charges associated with road traffic-related injuries in Iran. BMC Health Serv Res. 2013;13:281. doi: 10.1186/1472-6963-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watkins J.R., Soto J.R., Bankhead-Kendall B. What's the hold up? Factors contributing to delays in discharge of trauma patients after medical clearance. Am J Surg. 2014;208:969–973. doi: 10.1016/j.amjsurg.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Andersen J., Sharkey W., Schwartz M.L. Injury severity score, head injury, and patient wait days: contributions to extended trauma patient length of stay. J Trauma. 1992;33:219–220. doi: 10.1097/00005373-199208000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Jubbal K.T., Chen C., Costantini T. Analysis of surfing injuries presenting in the acute trauma setting. Ann Plast Surg. 2017;78:S233–S237. doi: 10.1097/SAP.0000000000001026. [DOI] [PubMed] [Google Scholar]
- 28.Böhmer A.B., Just K.S., Lefering R. Factors influencing lengths of stay in the intensive care unit for surviving trauma patients: a retrospective analysis of 30,157 cases. Crit Care. 2014;18:R143. doi: 10.1186/cc13976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Udekwu P., Roy S., McIntyre S. Flail chest: influence on length of stay and mortality in blunt chest injury. Am Surg. 2018;84:1406–1409. [PubMed] [Google Scholar]
- 30.Yadollahi M., Kashkooe A., Habibpour E. Prevalence and risk factors of spinal trauma and spinal cord injury in a trauma center in Shiraz, Iran. Iran Red Crescent Med J. 2018;20:e14238. doi: 10.5812/ircmj.14238. [DOI] [Google Scholar]