Abstract
Physical traumas are tragic and multifaceted injuries that suddenly threaten life. Although it is the third most common cause of death in all age groups, one out of four trauma patients die due to thoracic injury or its complications. Blunt injuries constitute the majority of chest trauma. This indicates the importance of chest trauma among all traumas. Blunt chest trauma is usually caused by motor vehicle accident, falling from height, blunt instrument injury and physical assault. As a result of chest trauma, many injuries may occur, such as pulmonary injuries, and these require urgent intervention. Chest wall and pulmonary injuries range from rib fractures to flail chest, pneumothorax to hemothorax and pulmonary contusion to tracheobronchial injuries. Following these injuries, patients may present with a simple dyspnea or even respiratory arrest. For such patient, it is important to understand the treatment logic and to take a multidisciplinary approach to treat the pulmonary and chest wall injuries. This is because only 10% of thoracic trauma patients require surgical operation and the remaining 90% can be treated with simple methods such as appropriate airway, oxygen support, maneuvers, volume support and tube thoracostomy. Adequate pain control in chest trauma is sometimes the most basic and best treatment. With definite diagnosis, the morbidity and mortality can be significantly reduced by simple treatment methods.
Keywords: Blunt chest trauma, Rib fractures, Pneumothorax, Hemothorax, Pulmonary contusion, Pain management
Introduction
Trauma is the third leading cause of death in all age groups after cardiovascular diseases and cancer.1 However, trauma is the most common cause of death in the age of first four decades.2 Although trauma-related injuries can occur in many parts of body, one out of four trauma patients die due to thoracic injury or its complications.3
Chest trauma remains a serious problem as high-speed vehicle accidents increase. Thoracic trauma occurs in approximately 60% of patients with polytrauma and has a mortality of 20%–25%.4, 5, 6
Trauma can be divided into two types: penetrating and blunt. Penetrating injuries such as penetrating, cutting and firearm injuries are disruptive to tissue integrity. Blunt injuries can cause damage to organs and structures under the tissue without disrupting the integrity of the tissue. Falling from height, traffic accidents and occupational accidents are main mechanisms of blunt injuries. Considering that 70% of all chest traumas constitute blunt injuries, the importance of blunt injuries is understood.7, 8, 9 In addition, blunt chest trauma accounts for 15% of all trauma cases in the world.10,11 The mortality rate is hard to evaluate as the causes of death in blunt chest trauma may be due to pulmonary and nonpulmonary complications.12
In the primary survey of chest trauma patients, 6 life-threatening conditions (airway obstruction, tension pneumothorax, open pneumothorax, massive hemothorax, flail chest, pericardial tamponade) should be immediately investigated and treated.13 Of note, 5 of the 6 most fatal causes indicate pulmonary and chest wall injuries in the trauma patient. The following potentially life-threatening injuries should be immediately investigated: pulmonary contusion, tracheobronchial injuries, diaphragmatic injuries, myocardial injury, thoracic aortic disruption, and esophageal injury. Similarly, 2 of these 6 conditions are pulmonary injuries due to trauma. Although trauma usually involves many tissues and organs, these life-threatening conditions show how important pulmonary injuries are in trauma patients.
Chest wall and pulmonary injuries caused by blunt thoracic trauma include many organs, tissues and systems. Therefore, a multidisciplinary approach is needed for these patients. It is very important that 10% or less of blunt chest trauma patients require surgical treatment, and the remaining patients can be treated conservatively,3,11,14 with a number of simple treatments such as appropriate airway assesment, oxygen support,15 tube thoracostomy,16 volume resuscitation,5 pulmonary toilet and adequate pain control.17
In addition, the age of the patient is important when evaluating a blunt chest trauma. While a trauma in the pediatric age group may not cause a chest wall injury due to bone elasticity, it may lead to serious complications and even death in the elderly population. It also can be interpreted that even if there is a serious trauma in the pediatric age group, the number of fractures may not be high due to bone elasticity, but in the elderly population the number of bone fractures may be high even in a slight trauma.
There are many risk factors that affect morbidity and mortality in blunt chest trauma. Despite patient's age, other important variables included the presence of bone fractures and the number of fractures, mechanical ventilation, as well as pre-existing chronic lung diseases, co-existing head injury, hypotension and extra thoracic organ injury.18, 19, 20, 21, 22, 23, 24 In addition, low Glasgow coma scale (GCS) score in chest trauma patients is highly predictive of mortality.25
Chest traumas are continuously increasing and many patients with chest trauma die before hospitalization despite using simple treatment methods. The cause of the mortality and morbidity in blunt chest trauma is mostly due to delayed pulmonary complications.17 It is worth to notice that the preventable in-hospital mortality rate in trauma patients is between 4% and 60% worldwide.26,27 We believe that blunt thoracic trauma and associated pulmonary injuries were not discussed together enough. So we will examine these injuries that can manifest themselves in many ways.
Mechanism of injury
We mentioned that blunt traumas were defined as injuries that organs and structures were injured without disrupting tissue integrity. Blunt traumas can also be classified according to their mechanisms. The mechanism of blunt trauma can be listed as motor vehicle accident, occupational accident and fall. It is important to know the mechanism of blunt injury for a rapid diagnosis and treatment, because there are specific injuries caused by different mechanisms, and the mechanism of injury is an independent factor of mortality.28
The severity of injury may depend on the strength and duration of the blunt impact as well as the acceleration-deceleration injury and compression damage that occur during trauma. There are four mechanisms of blunt chest trauma: (1) direct impacts on the thorax, (2) thorax compression, (3) acceleration/deceleration injuries, and (4) blast injuries.29,30
The best example of acceleration-deceleration damage is motor vehicle accident.3 The most common condition is the sudden and high-speed deceleration of the anterior thorax, resulting in injury to the vascular structures, bones, soft tissues and organs.31 At the same time, the presence of steering wheel deformity caused by the driver hitting the steering wheel increases thoracic injuries, complications and mortality.32,33 Thoracic compression is usually caused by crush, occupational accident and fall from height.
Most of the blunt thoracic trauma are caused by motor vehicle accidents (includes pedestrian accidents) and falls from height.14,34,35 Motor vehicle accidents are the most common cause of severe thorax trauma.36,37 In motor vehicle accidents, the most common trauma patients are pedestrians, vehicle drivers and motorcyclists, respectively.38 Most of the blunt thoracic traumas resulted from motor vehicle accidents and falls from height which required hospitalization.1
It is important to know acceleration-deceleration injury and thoracic compression in blunt chest trauma. Because it will be easier to understand the chest wall and pulmonary injuries caused by these traumas.
Clinical findings
In a blunt trauma, clinical findings revealed that all structures in the thorax can be damaged, such as chest wall tissues, thoracic cage, ribs, lung, pleura, large vessels, diaphragm, heart and mediastinal structures. Patient history and physical examination may have been pushed to the second plan with the development of imaging methods in medicine. However, patient history and physical examination are still an integral part of the diagnosis. It is true that patient history and physical examination are insufficient for diagnosis of trauma patients,39 but they form the basis of a holistic approach to diagnosis with imaging methods. Symptoms of patients may contain a lot of valuable information and assist in diagnosis and treatment. Signs and symptoms of thoracic trauma include: cyanosis of fingers, lips or face, dispnea, tachpnea or bradipnea, contusion, laceration, perforations, distension and other specific traumatic findings, hemoptysis, signs of shock (hypoperfusion), tracheal deviation, paradoxical movement of the chest wall, distension jugular veins, decreased or absent breathing sounds, pain and especially pain related to respiratory function, failure of chest expansion in normal inspiration.40
Respiratory distress is a serious problem in individuals with blunt chest trauma. Patients with respiratory distress may breathe with nasal flaring, using accessory muscles, intercostal and subcostal retractions, and signs such as tachypnea. The patient's lungs may not be equally involved in breathing. Paradoxical respiration can be observed and immediate diagnosis of flail chest can be made and thereafter rapid intervention can be performed. In the case of flail chest, it may not always be possible to see paradoxical movement due to pain. But does it always make sense to take X-rays without physical examination, while in some cases where inspection is sufficient for diagnosis?
As in all trauma patients, vital signs are one of the best indicators of blunt thoracic trauma. Findings such as tachycardia and hypotension are very valuable. Ecchymoses can be detected and the patient may have a cyanotic appearance. The presence of the Beck Triad (distended neck veins, hypotension, muffled heart sounds) may indicate cardiac tamponade. Skin color and pulse can provide information about many conditions.
Signs such as seatbelt sign or steering wheel deformity are indicators for high-energy blunt thoracic trauma. These signs should be carefully observed by inspection. Blunt thoracic trauma patiens may have tracheal deviation and deformities of the chest wall may be observed. These trauma patients may have multiple tissue contusions and laserations. In addition, these patients may have crepitation, subcutaneous emphysema, and tenderness over the ribs. As a lot of valuable information can be obtained by inspection and palpation, the trauma patient should be examined by removing the clothes.
Complaints such as decreased breathing sounds and pleuritic pain may occur. In cases of high mortality such as tension pneumothorax, hyperresonance can be taken in percussion. In contrast, dulness can be taken in hemothorax. The presence of hypovolemic shock findings in the patient while taking dulness in percussion suggests hemothorax.41 However, it should be noted that tension pneumothorax, flail chest or pericardial tamponade may cause shock, but may not always caused by hypovolemia.42
Early diagnosis and treatment are important for the prevention of the mortality and complications in patients with blunt thoracic trauma. For this reason, history and physical examination are an integral part of the approach to these patient. However, it should be noted that some trauma patients may not have these symptoms or may be nonspecific.11 Advanced examination and imaging methods are very valuable and more sensitive for diagnosis.
Chest wall related injuries
Thoracic cage
The most common injury in blunt thoracic trauma is chest wall injury, which also includes rib fractures. When bone fractures are mentioned, not only rib fractures but also clavicle and sternum fractures should be considered.
A study of 4205 trauma patients by Demirhan et al.10 showed the incidence of chest wall injuries such as rib, sternum and clavicle fractures was 36.1% in chest trauma. According to a study by Brasel et al.43 in 17,308 patients with hospitalized rib fractures, the average mortality rate was 4%. Considering that rib fractures were quite common in blunt chest trauma, the importance of mortality rate was understood.
Isolated rib fractures are not fatal. However, the rib fractures are usually accompanied by additional damage such as damage of pleura and lung tissue, pneumothorax, hemothorax, pulmonary contusion and parenchymal laceration, etc. The affacted rib usually fractured from the point of blunt impact or from the posterolateral bend, which is the most vulnerable part.44
The first two ribs are strongly attached to the musculoskelatal system, making them more difficult to break. Thus, the first rib fractures have a high mortality rate of 36% according to the study of Richardson er al.45 Because it can cause injury to the subclavian vessels and brachial plexus. Fracture of the first ribs is a high risk indicator for tracheobronchial, vascular, cardiac and pulmonary injuries.46
Middle zone ribs 4 to 9 are heavily exposed to blunt trauma.47 Fractures of these midzone ribs are often associated with injuries such as pulmonary contusion, laceration, hemothorax and pneumothorax.48 Anteroposterior compression of the thorax causes midshaft fractures by bending the ribs outwards.49
Rib fractures can cause various injuries and pulmonary complications as well as intraabdominal organ injuries. Although the last two ribs are more mobile and less fractured, fractures may result in liver, spleen and kidney injuries.50
The number of rib fractures and the age of the trauma patient are the most important indicators of mortality and morbidity.24,51, 52, 53, 54, 55 Patients with 3 or more rib fractures, even if isolated, have an increased risk of complications such as pulmonary contusion and pneumonia.56,57 According to study of Holcomb et al.58 the mortality rate of 7 or more rib fractures is 29%.
The problem caused by bone fractures in blunt chest trauma is based on three main reasons: hypoventilation due to pain, impaired gas exchange due to parenchymal damage, and alteration of breathing mechanics.59 These mechanisms should be evaluated and considered in treatment.
Weakened diaphragm and intercostal muscles, decreased muscle mass and loss of alveoli are associated with altered respiratory mechanics in the elderly population. These changes result in decreased lung volume and function, and impaired gas exchange due to reduced respiratory reserve. With these changes, elderly patients with bone fractures have an increased risk of hypoventilation, atelectasis and pneumonia.59 The first symptom in rib fractures is pain, which increases with deep inspiration. Patients may also have point tenderness. Decreased lung sounds may also be present. Retention of pulmonary secretions and pneumonia may occur due to pain caused by rib fractures.59 Therefore, adequate pain control is important in these patients.
Compared with young patients, clinical symptoms may appear later in the elderly population. Patients with isolated bone fractures may be reported as minor trauma. However, the incidence of pneumonia and mortality in elderly patients with rib fractures is twice as high as in young patients.49 Therefore, the elderly population should be followed closely even if there is a minor trauma.49 There are studies showing that the number of rib fractures in the elderly group is not correlated with mortality.60 This is due to the coexistence of osteopenic changes and other underlying diseases.56,61
Rib fractures are more common in adults than in pediatric group. Because children's ribs are more flexible. Therefore, pulmonary injuries in children may occur without significant injuries to chest wall.47 If a pediatric trauma patient has rib fractures, this should give an idea that the trauma is severe and may result in high mortality.62
In addition, contusion of chest wall tissue is another common problem in blunt trauma.6 These minor incidents do not cause serious problems and therefore they are not widely reported. However, contusion and abrasion of chest wall tissue can cause bleeding by injuring vessels in the skin, subcutaneous tissue, and muscles.63 In severe trauma patients, this type of bleeding can be persistent and cause problems.64 Contusion of chest wall tissue should be kept in mind, although it is often ignored in the medical literature.
Although bone fractures are the most common cause of blunt injuries in chest traumas, they may also be a group of patients with various intrathoracic injuries but without bone fractures.65 According to the study by Shorr et al.,66 this rate is 24.7% and the most common injury in this patient group was pneumothorax and hemothorax. This result shows that blunt chest trauma can cause various injuries and impacts without bone fractures.
Although an important injury of chest trauma is rib fractures, other bone structures in the thorax should also be considered. Sternal fractures are usually caused by anterior blunt chest trauma of the steering wheel as a result of motor vehicle accidents.67 Sternal fractures may cause vascular injury, as well as pulmonary and myocardial contusions. Electrocardiography and cardiac enzymes should be evaluated in sternal fractures.68,69 Rib fractures, pulmonary contusion, pneumothorax, hemothorax and even cranial injuries, spinal fractures and extremity traumas may associate with sternal fractures.70
Physical examination is insensitive in the diagnosis of bone fractures.71 X-Ray is a first-line imaging method, but unable to detect up to 50% of rib fractures in trauma patients.72, 73, 74 Computed tomography (CT) is useful not only for the diagnosis of bone fractures, but also for other injuries such as pulmonary laceration associated with rib fractures.75
With decreasing of inspiratory capacity and clearance of pulmonary secretions, the patients cannot cough because of pain, adequate pain control is important for the elimination of pulmonary secretions. Aggressive pain control is important to prevent atelectasis in patients, to increase the functional residual and vital capacity.76 There are three points in the treatment of bone fractures: (1) pain control, (2) management of pulmonary dysfunction, and (3) surgical fixation.77 An approach should be taken to prevent complications such as pneumonia and empyema in patients with bone fractures. Patients should be managed by considering the accompanying injuries and treated with a multidisciplinary approach.
Flail chest
Flail chest is a condition in which three or more contiguous ribs are broken at least in two parts. Basically, flail chest occurs when a segment of the chest wall is disconnected from the rest of chest wall. As the flail segment loses its continuity, the chest wall paradoxically moves in different directions during inspiration and expiration. In the inspiration, the ribs move outward while the flail chest moves inward; in the expiration, the opposite occurs. This is called paradoxical motion.
Flail chest is often caused by blunt trauma to the thorax, such as direct blows, falls from height, and car accidents. Flail chest is usually not alone, but with additional injuries like extrathoracic organ injuries, shock and blood loss. The mortality rate varies between 10% and 20% in patients with such additional injuries.78, 79, 80, 81, 82 A trauma strong enough to form a flail segment may also cause parenchymal contusion. As a result of parenchymal contusion, the breathing mechanism is impaired and edema and even necrosis may occur with pulmonary tissue bleeding. The presence of pulmonary contusion is highly predictive of morbidity. Flail chest is also closely associated with injuries such as hemothorax and pneumothorax.83,84
The main problem in these patients is the parenchymal injury caused by the flail chest, as well as the pain caused by rib fractures worsen the patient's condition. The presence of pain reduces tidal volume and may suppress the cough reflex, leading to atelectasis and pneumonia.85 At the same time, paradoxical movement makes breathing difficult and can cause respiratory failure.
Paradoxical motion may not be seen because the breathing is shallow due to pain, therefore, the diagnosis can be difficult. However, flail chest can be diagnosed with careful inspection, palpation, percussion and auscultation at a high rate of 90% sensitivity and 98% specificity.86 For this reason, flail chest patients should be examined by removing the clothes in order to perform a careful physical examination. Although patients may have a good clinical appearance, they should be kept under close observation since their condition may deteriorate. Paradoxical respiratory movement is typical for the diagnosis. Patients may also have severe chest pain and signs of respiratory distress, such as tachypnea.
Chest X-ray (CXR) can be used for diagnosis, but CT scan is more effective. It is especially valuable in the diagnosis of blunt injury and parenchymal contusion. Flail chest may occur as a result of bone fractures as well as the separation of the costochondral junction. However, CXR may not show the separation of the costochondral junction.49 Considering that CXR cannot detect up to 50% of bone fractures,63 the diagnosis of flail chest should be made according to clinical findings such as paradoxical respiration.87
These patients should firstly undergo airway-breathing-circulation (ABC) procedures. Frequent monitoring of vital signs is important in all trauma patients. Pulmonary physiotherapy, adequate pain control, endotracheal intubation, mechanical ventilation and close follow-up should then be performed. Oxygenation is also important in these patients. Prolonged intubation increases morbidity and mortality by increasing the risk of pneumonia.88,89 In the study of 3467 patients with flail chest, Dehghan et al.81 found the incidence of pneumonia, acute respiratory distress syndrome (ARDS) and sepsis were 21%, 14% and 7%, respectively.
Open reduction and internal fixation (ORIF) is also involved in flail chest treatment. Although ORIF is not generally accepted yet, there are data indicating that it shortens the stay in the intensive care unit (ICU) and reduces the complications if there is indication.90, 91, 92, 93 ORIF method is becoming more common. It should also be kept in mind that pulmonary contusion is a relative contraindication for ORIF.94
After the recovery period, flail chest patients may experience long-term disabilities such as dyspnea, chronic pain, exercise intolerance and delay in return to work.67,95, 96, 97 The fact that chronic pain may occur in patients with acute severe pain requires consideration of the psychosocial effects of this injury.
Pleura related injuries
Traumatic pneumothorax
Pneumothorax is a clinical entity that is caused by the presence of air between the visceral and the parietal pleura. In short, air trapped between the lung and the chest wall, because the accumulated air in related side of the lung collapsed.
Pneumothorax is the most common life-threatening injury in blunt thoracic trauma.98 Pneumothorax can be seen in 40%–50% of patients with all types of thoracic trauma.99,100 Therefore, pneumothorax should not be overlooked in trauma patients. It can lead to symptoms ranging from mild chest pain to cardiovascular collapse and death.98
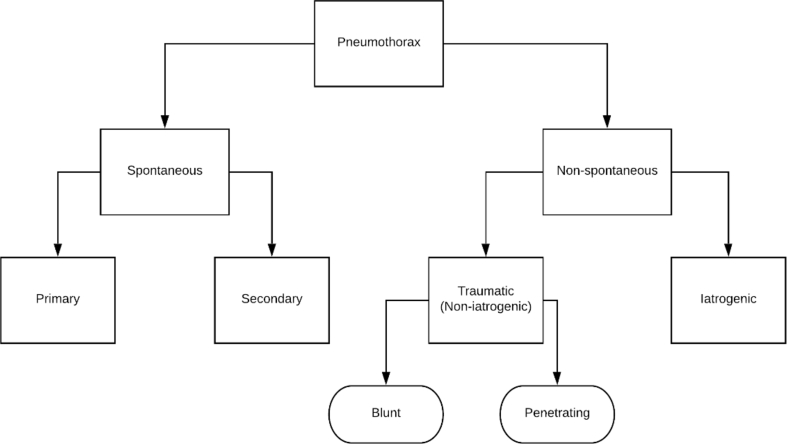
Pneumothorax can be examined as spontaneous and non-spontaneous (Fig. 1). We can define spontaneous pneumothorax as non-traumatic pneumothorax, and these are pneumothoraces that occurs without trauma or in the presence of an underlying precipitating factor. Trauma is the major cause of nonspontaneous pneumothorax. However, it should be kept in mind that iatrogenic causes such as transthoracic needle aspiration, subclavian vein catheterization, thoracentesis, biopsy and mechanical ventilation also bring to pneumothorax.101 In trauma patients, complications due to diagnostic and therapeutic procedures should not be ignored. The deterioration of the patient's condition after a medical procedure could suggest iatrogenic causes. Even a very small pneumothorax can lead to hemodynamic instability and severe respiratory failure.102,103
Fig. 1.
Clinical classification of pneumothorax.
Pneumothorax can occur in blunt chest trauma in four mechanisms: (1) alveolar rupture due to increased alveolar pressure, (2) paperbag effect (occurs if epiglottis is closed during sudden pressure increase in tracheobronchial tree),40 (3) acceleration-deceleration injury, (4) rib fractures damaging the pleura. In the early period, patients may have chest pain, dyspnea, anxiety, tachypnea, tachycardia and hyperrezonance and decreased respiratory sounds on the pneumothorax side.104, 105, 106 In the late period, signs such as decreased consciousness, tracheal deviation, hypotension, distension of cervical veins and cyanosis may be seen.104, 105, 106 The main fear is the development of tension pneumothorax.
In tension pneumothorax, air enters the pleural space at each inspiration, while the air in the pleural space cannot escape from the pleural space due to the one-way valve mechanism. Due to the continuous accumulation of air in the pleura, the lung collapses, hypoxia becomes severe, and hypotension occurs. It also affects the other lung by sliding to the opposite side and causing cardiovascular collapse. In pneumothorax, the patient may have tachypnea and tachycardia, hyperresonance can be obtained in percussion and tracheal deviation may be seen in late phase.107 The presence of air in the pleural cavity with mediastinal shift makes us think of tension pneumothorax.
Clinical findings and physical examination are very valuable for diagnosis of pneumothoraces. The absence of respiratory sounds, presence of subcutaneous emphysema and desaturation in mechanical ventilation are close to 100% in the diagnosis of tension pneumothorax.108 In addition, imaging methods take an important place. CT is the most effective method in the diagnosis of pneumothorax.75 CXR also occupies an important role in diagnosis. However, in some pneumothoraces, air in the pleural cavity may not be visible on CXR. Occult pneumothoracis (OPTX) is an example of this type of pneumothorax. OPTX is a type of pneumothorax that cannot be detected by CXR but can be detected by CT and ultrasound. In this instance, we can diagnose OPTX using CT. CXR cannot diagnose more than half of pneumothorax cases.109,110 OPTX occurs in 2%–20% of patients with blunt trauma.111, 112, 113 In addition, OPTX develops in 51% of trauma patients with pneumothorax.114 It is a serious condition, because it may eventually develop into tension pneumothorax.115 Therefore, OPTX should be kept in mind in patients with risky conditions such as subcutaneous emphysema, rib fractures and pulmonary contusion.109,116 In the presence of subcutaneous emphysema, rib fractures and pulmonary contusion, the patient should be evaluated by chest CT to exclude pneumothorax.117
The method of ultrasound evaluation of the lung is now becoming widely used. Imaging methods such as CXR and CT may cause problems in polytrauma patients and especially in cases requiring spinal immobilization. According to the study of Blaivas et al.,118 CXR has a sensitivity of 75.5% and a specificity of 100%, while the sensitivity of ultrasound is 98.1% and specificity 99.2%, respectively. Ultrasound is particularly important in patients who are not eligible for CXR and CT. Also ultrasound is not invasive and the patient is not exposed to radiation.
Pneumothorax treatment requires a holistic approach including monitoring, resting, oxygen supply and tube thoracostomy. Treatment should begin with the principles of ABC approach to the trauma patient. The patient's airway continuity, breathing and circulation should be monitored repeatedly. Giving 100% oxygen support to the patient increases the absorption of air from the pleural cavity.15 Additional oxygen therapy instead of room air accelerates the reabsorption of air four-fold.119 In addition, upright position may be beneficial in patients unless there is a contraindication such as spinal injury.104 The gold standard in treatment is tube thoracostomy. Advanced trauma life support recommends tube thoracostomy for all traumatic pneumothorax cases due to the risk of tension pneumothorax.49 In addition, if mechanical ventilation support is required, the risk of tension pneumothorax increases considerably and tube thoracostomy is mandatory.120,121 However, the general clinical approach to OPTX is to provide continuous monitoring as long as the patient is stable and asymptomatic,122,123 because tube thoracostomy is associated with the morbidity.124, 125, 126
General principles such as air elimination, reducing air leakage, healing pleural fistula, promoting re-expand and preventing future recurrances are applied in the treatment of pneumothorax.127 Supportive therapy, oxygen therapy, needle decompression and tube thoracostomy methods are used in general treatment. Thoracotomy for pleurodesis or video assisted thoracoscopic surgery (VATS) may be used in more advanced cases.
Traumatic hemothorax
Hemothorax is defined as the fluid between visceral and parietal pleura to be 50% or more of peripheral blood hematocrit. Hemothorax cannot be distinguished from blood color when the hematocrit of pleural fluid is greater than 5% of blood hematocrit.128 A blunt and penetrating trauma may result in massive hemothorax with intercostal arteries, laceration of the lung, or rupture of large vessels of the mediastinum.129 Hemothorax may be due to rib fracture after blunt trauma or may develop without rib fracture. Hemothorax and hemopneumothorax occur in almost one in three trauma patients with thoracic injuries.130 Hemothorax can be caused by many things, but the most common cause is trauma.131 In blunt traumas, the hemothorax is usually caused by injury to the intercostal vessels or interparenchymal pulmonary vessels due to rib fractures.132 It may even occur due to vertebral fractures.
According to the study by Liman et al.,60 the rate of hemo/pneumothorax was 6.7% in trauma patients without rib fractures, while 24.9% in those with one or two rib fractures and 81.4% in those with more than two rib fractures, respectively. According to some medical literature, the presence of three or more rib fractures is inevitable for hemothorax.133 Therefore, it is very important to evaluate the incidence of hemothorax in a patient with thoracic trauma regardless of the mechanism.
As a result of hemothorax, hypovolemia symptoms may occur in patients due to blood loss. It should be noted that up to 6 L blood can accumulate in the pleural space.87 These patients may develop hemodynamic instability due to hypovolemia. At the same time, hemothorax can cause atelectasis in the lungs and cause respiratory distress. Flattening of the neck veins, hypotension, tachycardia, decreased breathing sound, dullness in the percussion examination of the injured area should suggest hemothorax. Complications such as pneumonia, retained hemothorax, empyema, fibrothorax, respiratory distress may occur as a result of hemothorax. As it can be seen, the condition called hemothorax is life-threatening not only with pulmonary events, but in many other ways. As a result, it is necessary to remember the other complications caused by blunt trauma besides hemothorax.
In hemothorax, the condition called retained hemothorax may arise due to inability to perform early tube thoracostomy, insufficient drainage or iatrogenic reasons due to interventions. A retained clot in the pleural space as a result of hemothorax is a primary predisposing factor for post-traumatic empyma.134,135 In a study of 2261 trauma patients by Eren et al.,136 the incidence of posttraumatic empyema was 3.1% in patients with chest trauma. The only source of microorganisms that cause post-traumatic infections is not airways but also tube thoracostomy.137 In addition to posttraumatic empyema, if the retained clots cannot be drained, fibrothorax may occur, causing adhesions and impaired lung function.138
In addition, in minor trauma patients, the hemothorax cannot be detected at first, but may occur after a while, which is called delayed hemothorax. The incidence of delayed hemothorax in the first 2 weeks was 7.3%–12%.139,140 Therefore, follow-up and observation are important in patients with chest trauma. Due to the risk of delayed hemothorax and pneumothorax, all discharged patients need to be recalled after 2 weeks.
It is essential to start with physical examination in the diagnosis of hemothorax. In a study by Bokhari et al.,141 the sensitivity and specificity of using auscultation in the diagnosis of hemopneumothorax due to blunt trauma was found to be 100% and 99.8% in hemodynamically stable patients, respectively.141 CXR imaging is also used in the classical way in the diagnosis of hemothorax. The blunting of the costophrenic angle or partial or complete opacities in the hemithorax may suggest hemothorax.4 It may not always be possible to detect hemothorax with CXR. Most of the hemothoraces detected by CT cannot be detected by CXR.142 In the upright film, 200–300 mL of blood is sufficient in the pleural space to detect the hemothorax,143 whereas 1000 mL of blood is required for the presence of opacity on the chest radiograph in the supine position.130,144 For these reasons, CT is now the gold standard. In addition, the use of ultrasound has become more common in recent years, because it is very useful for nonstable patients who cannot take CT. The use of ultrasound can also prevent unnecessary tube thoracostomy and reduce the related complications.145 However, in extremely obese patients and subcutaneous emphysema, ultrasound imaging may cause problems.146 Today, ultrasound is used in ICUs where CT is unavailable or patient transport is not possible.147
One of the most important steps in the management of hemothorax is early intervention. Because blood loss can be severe enough to cause sudden vascular collapse. It is noteworthy that patients with massive hemothorax caused by large vessels often die before being hospitalized.148 In addition to hypovolemia, altered lung mechanics due to pulmonary compression also have an impact on the clinic in the acute phase.149 Tube thoracostomy is the most commonly used method for the management and treatment of hemothorax. The aim of tube thoracostomy are (1) to clear the pleural space as much as possible (2) to provide re-expansion of the lungs (3) to create a buffer effect by contacting the lung with the parietal pleura (4) to measure the amount of blood lost and (5) to reduce the risk of complications such as empyema and fibrothorax.16,87,150,151 After tube thoracostomy, the continuation of radiopacity on thorax radiograph indicates that blood coagulates in the pleural space.
In addition, there are studies showing that it is an effective method to monitorize and observe the patient instead of tube thoracostomy in smaller hemothorax, yet a consensus has not been reached on this subject.152,153 A small hemothorax can be resorbed in a few weeks, but this is still controversial because of the complications that hemothorax can cause.133
VATS is an effective method in cases of inadequate drainage and retained hemothorax. In the study conducted by Lin et al.,154 early application of VATS procedure decreased the risk of empyema and shortened the duration of ventilator dependence. If the patient has massive hemothorax, i.e. >1500 mL of blood or 200 mL of bleeding per hour for at least 4 h from chest tube, thoracotomy is preferred as an acute intervention.155 However, hemodynamic instability findings such as shock, uncontrollable bleeding and major vascular injuries should also be taken into consideration for the indication of thoracotomy. Fibrinolytic agents may also be used in therapy. Although fibrinolytic agents are used in combination with tube thoracostomy, studies on this subject are insufficient.
Pulmonary parenchyma and airway related injuries
Pulmonary contusion
Pulmonary contusion is defined as pulmonary destruction with alveolar hemorrhage, which usually occurs as a result of blunt chest trauma without laceration.156, 157, 158 In case of severe blunt thoracic trauma, pulmonary contusion should always be investigated.
The incidence of pulmonary contusion in patients with blunt chest trauma varies between 17% and 75% and this corresponds to a very large proportion.159, 160, 161 Pulmonary contusion is common, especially in high-speed trauma caused by motor vehicle accident and is usually associated with rib fractures.66,162,163 Pulmonary contusion is the most common injury associated with bone fractures, especially in the adult age group and is highly predictive of mortality.49 Three-quarters of patients with pulmonary contusion have accompanying rib fractures, but contusion may occur without bone fracture, especially in the pediatric group.164, 165, 166
Pulmonary contusion occurs when kinetic energy is transmitted to the lung parenchyma.167 As a result, bleeding and inflammation occur in the pulmonary tissue and pulmonary edema occurs. Bleeding and edema cause serious changes in the lung tissue.168 One of these serious changes is hypoxia, which is the most common outcome in pulmonary contusion.169 Parenchymal destruction reaches its maximum within the first 24 h.90 In addition, immune function deteriorates due to the release of local inflammatory agents and the patient may become susceptible to infections.170 Not only the injured part of the lung but also other parts of the lung are affected as a result of these processes.5 However, there are many things that remain to be elucidated in the mechanism of trauma-induced pulmonary contusion, and the pathophysiology of inflammation may be different from which we have known.157,171, 172, 173
Pulmonary contusion can often coexist with the flail chest, and most such patients suffer from dyspnea, decreased exercise tolerance, and chest pain on the side of the injury.174 Mortality of pulmonary contusion varies between 10% and 25%.175 However, other concomitant injuries usually cause mortality.176
Classically, CXR is the first modality for imaging diagnosis. Focal or diffuse homogeneous opacification is the basis of diagnosis on chest radiography. However, contusion may not be seen in one or more of the three patients by CXR.113,158 Therefore, CT is very valuable and sensitive in the diagnosis of pulmonary contusion. The recovery of a noncomplex pulmonary contusion may be observed on CXR between 48 h and 72 h, but complete recovery may take up to 14 days.29 Ultrasound is also highly sensitive and specific in the diagnosis of pulmonary contusion.162
Clinically, chest pain, dyspnea and tachypnea may be present. Hypoxemia and hypercarbia may occur, especially due to contusion associated with other injuries.177 In such patients, early intubation before hypoxia and hypercarbia develops has an impact on mortality.178 However, the clinical findings in pulmonary contusion are quite variable and some patients may be asymptomatic at first. Even if the presence of contusion appears in CXR or CT, the clinical condition varies from asymptomatic to respiratory compromise.168 If infection or ARDS does not occur, the clinical condition may slowly correct itself. Pulmonary contusion is an independent predictor of complications such as pneumonia, ARDS and multiple organ dysfunction syndrome (MODS).179,180
The treatment logic of pulmonary contusion is supportive therapy. Supportive methods such as frequent follow-up of vital signs, oxygen support, pain control, early mobilization and chest physiotherapy are used in patients. It is also very important to protect euvolemia in cases of pulmonary contusion. Abnormal fluid accumulation in the interstitial and intraalveolar space is the most important pathology of pulmonary contusion.181 Fluid replacement is necessary in trauma patients to ensure adequate blood volume, but as fluid overload in pulmonary contusion may worsen pulmonary edema, proper fluid balance should be maintained and, if necessary, diuretics should be used.156, 157, 158,182 As with any trauma patient, non-invasive respiratory supports should be preferred before invasive respiratory support.94 Patients who require invasive mechanical ventilator support are at risk of developing ventilator-induced barotrauma and pneumonia, and contusion already increases the risk of pneumonia. Furthermore, pharmacological treatments are insufficient for the treatment of pulmonary contusion. Steroid and empirical antibiotic use are still controversial.158,162,183,184
Pulmonary laceration
Pulmonary laceration is the injury that occurs in the parenchymal tissue of the lung. In contrast, parenchymal structure is intact in pulmonary contusion.65 Pulmonary laceration is usually caused by penetrating injuries, but nonpenetrating injuries can also cause pulmonary laceration.160 The incidence of pulmonary laceration in blunt chest trauma varies between 4.4% and 12%.160,185, 186, 187 Pulmonary laceration has not been sufficiently reported in the medical literature.
Pulmonary lacerations can be divided into four subtypes.188,189 Type 1: lacerations are caused by compression-induced lung rupture (most common type). Type 2: lacerations are caused by compression and occur in the lower lobes and paraspinal region. Type 3: lacerations are usually seen as a result of pleural puncture of rib fractures and are associated with pneumothorax. Type 4: lacerations are caused by rupture of pleural adhesions and have no characteristic radiological findings. Since bone elasticity is high in the pediatric group, pulmonary laceration may occur without bone fracture, similar to pulmonary contusion.190 Therefore, type 1 laceration is the most common in young patients.191
Lacerations not only cause bleeding and respiratory distress. Pulmonary lacerations also cause air leakage and this is the most common cause of pneumothorax in blunt traumas.49 Hemothorax or pneumothorax may develop if the laceration extends to the pleural cavity.192 Deep pulmonary lacerations can be seen in 50% of patients with intrathoracic hemorrhage in blunt chest trauma.193 As a result of laceration, the circulating blood can pass into the airway and thoracic cavity and the patient may have hemorrhagic shock or even drown in his/her own blood.193
Pneumatocele may develop if air enters pulmonary cavities, and hemato-pneumatocele may occur if both air and blood are involved.194,195 When the bleeding is resolved, it can become a traumatic pneumatocele and may be infected.182,196
Like all trauma patients, a complete physical examination should be performed and lung sounds should be listened bilaterally in patients with suspected pulmonary laceration. Respiratory sounds may be decrased on the side of pulmonary laceration. It is difficult to detect pulmonary lacerations with CXR. Because pulmonary lacerations usually overlap with concomitant pulmonary contusions.75,197 Pulmonary lacerations can be detected in CT at a high rate.198
The severity of pulmonary laceration is various and the treatment should be shaped accordingly. Hemodynamic instability due to bleeding should be prevented and appropriate fluid resuscitation should be performed. Supportive treatment should be applied and chest tube should be used if necessary. Surgical interventions may be necessary if bleeding cannot be controlled. Pulmonary lacerations heal later than contusions and may last for several months.189 Major and bilateral lacerations may be an independent risk factor for mortality.187 Pulmonary lacerations can be managed by tube thoracostomy or thoracoscopic surgery and even lung resection may be necessary.199,200
Tracheobronchial injury
Tracheobronchial injury is the injury to the trachea, bronchi and tracheobronchial tree. Although tracheobronchial injury is rare, it is the most severe form of chest trauma and has a fatal course.201
The incidence of tracheobronchial injury ranges from 0.8% to 5%.112,202,203 However, the incidence of tracheobronchial injury is very difficult to measure, because most of the patients die before reaching a hospital, or developed mortal complications after injury.204,205 The pre-hospital mortality rate was up to 81%.206 The incidence of tracheobronchial injury increases with high speed transportation in traffic.207 But also the number of patients with tracheobronchial injury who reach the hospital alive increases with improved ambulance services.208
Tracheobronchial injury occurs through three mechanisms209: (1) a sudden anterior to posterior force above the carina level, (2) severe compression injury with the glottis closed, and (3) tear of cricoid and carina adhesions of the trachea in a rapid deceleration.
Diagnosis of tracheobronchial injury is very difficult. The majority of patients with tracheobronchial injury cannot be confirmed immediately.210 It is necessary to be very skeptical to make the diagnosis because tracheobronchial injury is difficult to be distinguished from other accompanying injuries.211,212 Patients may have dyspnea, hemoptysis, stridor, subcutaneous-mediastinal emphysema, and respiratory distress.199,213 Tracheobronchial injury should be considered in patients with persistent atelectasis, pneumomediastinum, pneumothorax, massive air leak despite chest tube, subcutaneous emphysema, hemoptysis, and phonation changes.168,214, 215, 216 However, tracheobronchial injuries may also be due to iatrogenic causes and endotracheal intubation and dilated tracheostomy constitute 92% of iatrogenic tracheobronchial injuries.217,218 Iatrogenic causes should be kept in mind and tracheobronchial injury should be considered in case of sudden changes in the patient's condition as a result of medical interventions.
The first imaging modality for the diagnosis of tracheobronchial injury is CXR, but CXR is not sufficient and there are no specific findings.219 Pneumomediastinum and cervical emphysema are the most sensitive indicators for tracheobronchial injuries on radiological imaging.220 The majority of tracheobronchial injuries are anatomically close to the carina, therefore, the diagnosis of tracheobronchial injury can be difficult radiologically.213,221 CT may be preferred, but bronchoscopy is the most valuable method for early diagnosis.222, 223, 224
Although tracheobronchial injuries cause severe respiratory distress in patients, positive pressure ventilation is contraindicated in tracheobronchial injury because it may exacerbate the condition.215 For this reason, rapid diagnosis and surgical treatment of tracheobronchial injuries are prominent.225 Esophageal injury associated with tracheobronchial injuries should also be checked because complications such as mediastinitis and tracheoesophageal fistula may develop if missed.212 Infections are important because late deaths in tracheobronchial injuries are usually caused by sepsis and MODS.226
The main logic of treatment in tracheobronchial injury is to maintain airway continuity and to repair the injury. If necessary, tracheostomy or cricotomy can be performed to ensure airway continuity.227 Since tracheobronchial injuries are fatal, surgical intervention is often preferred.64 Although standard treatment is surgical, conservative treatments may be effective in some patients.228,229 However, there is no consensus on the indications of conservative treatment.230 In surgical treatment, primary repair with suture, lobectomy and pneumoctomy can be performed. Treatment methods such as fibrin glue may also be used, but are not generally accepted.231
General management of patients with blunt chest trauma
We mentioned in the introduction that trauma was the leading cause of death in age of first four decades of life. Rapid diagnosis and treatment of trauma, including blunt chest trauma, is more important than other cases. Because in accidents, 50%–60% of deaths occur at the time of accident and 25%–30% occur within the first 24 h.232, 233, 234
The principles of approach to trauma patients should always be applied. In primary survey, airway, breathing, circulation, disability, exposure (ABCDE) approach should be performed. Head injury and hemorrhage are the major causes of early death in all trauma patients.235,236 It may not be enough that the airway is open and functioning. The rate, depth and pattern of respiration are also important. In addition, airway obstruction, tension pneumothorax, open pneumothorax, massive hemothorax, flail chest and cardiac tamponade, which are the six mortal conditions that can be seen in a chest trauma, must be detected at the primary survey.
After the ABCDE principles, the injury severity should be evaluated by considering vital signs, mechanism of injury, patient complaints, and general clinical presentation.57 However, the clinical appearance can often be misleading at the first time and complications may take 48–72 h to emerge.237,238 The mechanism of trauma can provide rapid diagnosis and treatment by providing information about how the injury occurred. History and physical examination is essential to quickly detect major injuries such as tension pneumothorax, massive hemothorax and flail chest. In physical examination, an asymmetry in the chest should be examined, palpation should be performed to detect crepitation and auscultation should not be omitted. Although physical examination is considered to be insufficient for diagnosis most time, it is still valuable and necessary. Contrary to popular idea, physical examination has a very high sensitivity and specificity, especially in the diagnosis of hemopneumothorax.141 Clinically stable patients who are considered to have no serious injuries following high-energy trauma are at risk of serious complications.57 Therefore, patients should always be examined with a skeptical mentality. Even if patients do not have serious symptoms, they should be followed up for 2 weeks after the trauma, because of the risk of complications such as delayed hemothorax, delayed pneumothorax and OPTX.139
Hemorrhage may occur due to various injuries in blunt traumas and it may be difficult to diagnose them. Bleeding is the most common cause of shock in trauma patients.49 Hemodynamic status can be examined by checking the patient's consciousness, pulse, bleeding and skin color. The presence of prehospital hypotension is indicative of serious damage.57 A proper fluid resuscitation is required for these patients.
Management in patients with blunt chest trauma is mainly provided by early mobilization, adequate pain control, proper fluid resuscitation, and appropriate respiratory support.238,239 One of the main goals of the treatment for fatal pulmonary complications is to correct respiratory failure. Pulmonary contusion as a result of blunt chest trauma is usually represented as respiratory failure. Rib fractures may also disrupt the physiological structure of the chest wall and lead to respiratory failure.
Respiratory failure may be due to direct pulmonary injuries caused by blunt chest trauma or indirectly due to traumatic brain injury. In this instance, it should be kept in mind that the patient's respiratory distress may be due to brain damage.240 There may also be complex conditions that involving both brain and lung injury.241 It is interesting to note that traumatic brain injuries are usually associated with thoracic injuries and 29% of traumatic brain injuries are associated with pulmonary contusion.242 In addition, hypercoagulability in trauma patients leads to pulmonary embolism, resulting in respiratory failure.64
In order to control respiratory failure, it is necessary to optimize ventilation, maintain oxygenation and ventilation/perfusion ratio, and avoid ventilator-related lung injuries.241 Invasive mechanical ventilation may be used depending on the severity of pulmonary injuries. However, mechanical ventilation increases mortality.214 To note, if a patient has pneumothorax, it should be corrected first because positive pressure ventilation can exacerbate pneumothorax.29 Therefore, invasive ventilation methods should not be used in these patients unless necessary. Early noninvasive ventilation may reduce the need for intubation.151 Prone position can also be used to help patients with respiratory distress.243 Rapid mobilization of patients with pulmonary physiotherapy is considered a key factor in preventing thrombosis, embolism and pulmonary complications such as pneumonia, respiratory failure and ARDS.55,113,244
CXR is the primary diagnostic tool for detecting injuries resulting from thoracic trauma, but CT is more sensitive.245,246 In patients with severe blunt chest trauma confirmed by CT, 65% significant intrathoracic injuries cannot be found by CXR.247 Also, ultrasound is valuable in blunt thoracic trauma, because it is quick and practical.
Monitoring of vital signs should be done frequently and treatment should be performed to prevent from complications. It should be noted that patients with blunt chest trauma are usually a polytrauma patient and should take a holistic approach.248 In addition, arterial blood gas, complete blood count, electrolytes, cardiac markers, serum lactate levels, blood typing and coagulation tests may be requested in chest trauma patients.148,249 Electrocardiography should be performed for cardiac events. Acidosis and hypoxia may also occur in a trauma patient. The presence of hypovolemia and vascular collapse in the trauma patient is associated with mortality so it is important to be noticed. Therefore, appropriate volume resuscitation and acidosis treatment is very important in trauma patients.
Conditions such as pneumothorax and pulmonary contusion require oxygen support to the patients. In addition, patients should receive pulmonary physiotherapy such as deep breathing exercises, aerosol therapy, active cough maneuvers and incentive spirometry.250 Adequate pain control is essential to solve respiratory problems caused by chest trauma. Analgesics with pulmonary physiotherapy are important for the prevention of complications such as pneumonia and atelectasis in patients.251 Imaging techniques such as CXR, CT, and ultrasound takes an important place in diagnosis and treatment of chest trauma cases. If necessary, specific treatments such as needle decompression, tube thoracostomy, and thoracotomy should be performed.
The importance of adequate pain control
According to the International Association for the Study of Pain, pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.252 In addition to being a multifaceted condition, pain is a risk factor that can cause most of the morbidity associated with blunt chest trauma. The presence of pain may impair the ability of the person to breathe, impairing ventilatory function, further exacerbating impaired lung mechanics caused by inflammation and possible contusion already present in a blunt trauma patient. In addition, it causes the retention of pulmonary secretions which further suppresses the patient's cough reflex. Therefore, the cough reflex suppressed by pain leads to atelectasis and increases morbidity. Accordingly, if a patient with lung injury is not treated appropriately and an appropriate analgesia is not performed, the present systemic inflammation results in decreased lung compliance, ventilation-perfusion mismatch, hypoxemia and respiratory distress, respectively.253,254 Inadequate pain control can lead to insufficent sleep, undernutrition, psychological stress, depression, agitation, rhytmic disorders, prolonged recovery and limitation of normal daily activities.255, 256, 257 Untreated pain can have adverse effects on the hemodynamic stability, gastrointestinal system and renal functions and may lead to conditions such as tachycardia and hypercoagulability.258, 259, 260 Timely and adequate pain control in thoracic trauma will not only reduce complications but also reduce hospital stay and costs.261,262
Nonsteroidal anti-inflammatory drugs (NSAIDs), systemic opioids or regional analgesia methods such as epidural analgesia, intrapleural analgesia, intercostal nerve block, and thoracic paravertebral block can be used for pain control. Multimodal methods (e.g. combination of opiods and NSAIDs) are also used.
The advantage of epidural analgesia over systemic opioids is that they are non-sedating, and patients can perform pulmonary physiotherapy more appropriately because they are awake.260 However, skilled personnels are needed for epidural analgesia which may lead to hypotension.263,264 Another method is that systemic opioids provide aggressive pain control, but the resulting systemic effects can lead to sedation, hypoventilation, suppression of cough reflex, and respiratory failure.251
Intrapleural analgesia is performed by applying local anesthetic agent to the pleural space and does not cause hypotension.265 However, there is a possibility that the anesthetic agent will drain from the chest tube and local anesthesia may lead to systemic toxicity.17,265 Intercostal nerve block, another pain control method, provides highly effective analgesia and does not cause central nervous system depression but increases the risk of pneumothorax due to multiple injections.253 Thoracic paravertebral block is also easier than epidural analgesia in addition to providing effective analgesia because there is no risk of spinal cord injury but a risk of tissue puncture and pneumothorax.17
All methods have advantages and disadvantages, there is no perfect one. Therefore, the clinician should choose the most appropriate method according to the patient's condition, contraindications, side effects and severity of trauma. Even effective analgesia is affected by factors such as the patient's ethnicity and anxiety.266
Inadequate pain control can make the patients to experience posttraumatic stress and chronic pain.267 Some patients had suffered from pain for 6 years since discharged,250 and 50% of patients with blunt chest trauma may continue to suffer within the first three months.263 Chronic pain and depression are common in trauma patients during the recovery period.268 Prevention of chronic pain is also very important for many reasons such as delaying return to work,269,270 which, interestingly, depends not only on physical impairments but also on psychological problems.271
Morbidity and mortality in blunt chest trauma are common in the community. It is interesting to note that 8 of the 43 cases mentioned in the Edwin Smith Papyrus, written thousands of years ago, had chest injuries, and even at that time, chest injuries accounted for 20%–25% of all trauma cases.272 Chest wall, pulmonary, mediastinal and diaphragmatic structures may be injured in chest trauma. However, it should be kept in mind that every chest trauma patient may also be a polytrauma patient and the accompanying injuries should be examined carefully. Therefore, history and physical examination should not be missed, imaging methods should be used appropriately, and the patient should be treated with rapid diagnosis and treatment. In addition, the long-term outcome of trauma patients should be taken into account, complications should be prevented and pain should be managed. Therefore, management of the trauma patient is a long-term and holistic approach including prehospital management, emergency care, intensive care unite and post-injury period. Since surgical intervention in blunt chest trauma is required in a small number of patients, many patients can be treated with conservative methods or simple procedures such as tube thoracostomy.
Trauma and blunt chest injuries are also serious psychosocioeconomic problem worldwide. Patients with chest trauma should be treated not only for pulmonary and non-pulmonary injuries, but also for psychological effects, which may delay return to work as well.
Funding
Nil.
Ethical Statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Jones K.W. Thoracic trauma. Surg Clin. 1980;60:957–981. doi: 10.1016/S0039-6109(16)42194-8. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Ten leading causes of death and injury. https://www.cdc.gov/injury/wisqars/LeadingCauses.html
- 3.LoCicero J., Mattox K.L. Epidemiology of chest trauma. Surg Clin. 1989;69:15–19. doi: 10.1016/S0039-6109(16)44730-4. [DOI] [PubMed] [Google Scholar]
- 4.Broderick S.R. Hemothorax: etiology, diagnosis, and management. Thorac Surg Clin. 2013;23:89–96. doi: 10.1016/j.thorsurg.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Khandhar S.J., Johnson S.B., Calhoon J.H. Overview of thoracic trauma in the United States. Thorac Surg Clin. 2007;17:1–9. doi: 10.1016/j.thorsurg.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Milisavljevic S., Spasic M., Arsenijevic M. Thoracic trauma. In: Cagini L., editor. Current Concepts in General Thoracic Surgery. InTech; 2012. [DOI] [Google Scholar]
- 7.Marts B., Durham R., Shapiro M. Computed tomography in the diagnosis of blunt thoracic injury. Am J Surg. 1994;168:688–692. doi: 10.1016/S0002-9610(05)80146-1. [DOI] [PubMed] [Google Scholar]
- 8.Blair E., Topuzlu C., Davis J.H. Delayed or missed diagnosis in blunt chest trauma. J Trauma. 1971;11:129–145. doi: 10.1097/00005373-197102000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Harrison M. Traumatic pneumothorax: a review of current practices. Br J Hosp Med. 2014;75:132–135. doi: 10.12968/hmed.2014.75.3.132. [DOI] [PubMed] [Google Scholar]
- 10.Demirhan R., Onan B., Oz K. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg. 2009;9:450–453. doi: 10.1510/icvts.2009.206599. [DOI] [PubMed] [Google Scholar]
- 11.Eghbalzadeh K., Sabashnikov A., Zeriouh M. Blunt chest trauma: a clinical chameleon. Heart. 2018;104:719–724. doi: 10.1136/heartjnl-2017-312111. [DOI] [PubMed] [Google Scholar]
- 12.Eastern Association for the Surgery of Trauma. 2003. Pain management in blunt thoracic trauma (BTT): an evidence-based outcome evaluation. 2nd Review.https://www.east.org/Content/documents/practicemanagementguidelines/thoracic-blunt-trauma-pain-management.pdf [Google Scholar]
- 13.Cubasch H., Degiannis E. The deadly dozen of chest trauma. Cont Med Educ. 2004;22 [Google Scholar]
- 14.Chrysou K., Halat G., Hoksch B. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients—still a relevant problem? Scand J Trauma Resuscitation Emerg Med. 2017;25:42. doi: 10.1186/s13049-017-0384-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chadha T.S., Cohn M.A. Noninvasive treatment of pneumothorax with oxygen inhalation. Respiration. 1983;44:147–152. doi: 10.1159/000194541. [DOI] [PubMed] [Google Scholar]
- 16.Daly R.C., Mucha P., Pairolero P.C. The risk of percutaneous chest tube thoracostomy for blunt thoracic trauma. Ann Emerg Med. 1985;14:865–870. doi: 10.1016/S0196-0644(85)80635-1. [DOI] [PubMed] [Google Scholar]
- 17.Simon B.J., Cushman J., Barraco R. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59:1256–1267. doi: 10.1097/01.ta.0000178063.77946.f5. [DOI] [PubMed] [Google Scholar]
- 18.Battle C.E., Hutchings H., Evans P.A. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43:8–17. doi: 10.1016/j.injury.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Ziegler D.W., Agarwal N.N. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–979. doi: 10.1097/00005373-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Manay P., Satoskar R., Karthik V. Studying morbidity and predicting mortality in patients with blunt chest trauma using a novel clinical score. J Emergencies, Trauma, Shock. 2017;10:128–133. doi: 10.4103/JETS.JETS_131_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ekpe E.E., Eyo C. Determinants of mortality in chest trauma patients. Niger J Surg. 2014;20:30–34. doi: 10.4103/1117-6806.127107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emircan S., Ozgüç H., Akköse Aydın S. Factors affecting mortality in patients with thorax trauma. Ulus Travma Acil Cerrahi Derg. 2011;17:329–333. doi: 10.5505/tjtes.2011.76158. [DOI] [PubMed] [Google Scholar]
- 23.Dougall A.M., Paul M.E., Finely R.J. Chest trauma--current morbidity and mortality. J Trauma. 1977;17:547–553. [PubMed] [Google Scholar]
- 24.Bergeron E., Lavoie A., Clas D. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478–485. doi: 10.1097/01.TA.0000037095.83469.4C. [DOI] [PubMed] [Google Scholar]
- 25.Kulshrestha P., Munshi I., Wait R. Profile of chest trauma in a level I trauma center. J Trauma. 2004;57:576–581. doi: 10.1097/01.TA.0000091107.00699.C7. [DOI] [PubMed] [Google Scholar]
- 26.Roy N., Kizhakke Veetil D., Khajanchi M.U. Learning from 2523 trauma deaths in India- opportunities to prevent in-hospital deaths. BMC Health Serv Res. 2017;17:142. doi: 10.1186/s12913-017-2085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan O., Hiorns M. Chest trauma. Eur J Radiol. 1996;23:23–34. doi: 10.1016/0720-048X(96)01030-3. [DOI] [PubMed] [Google Scholar]
- 28.Haider A.H., Chang D.C., Haut E.R. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153:138–142. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 29.Oikonomou A., Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging. 2011;2:281–295. doi: 10.1007/s13244-011-0072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wintermark M., Schnyder P. Introduction to blunt trauma of the chest. In: Schnyder P., Wintermark M., editors. Radiology of Blunt Trauma of the Chest. Springer Berlin Heidelberg; Berlin, Heidelberg: 2000. pp. 1–7. [DOI] [Google Scholar]
- 31.Cassuto J., Ezuddin N., Danton G. Blunt chest trauma: a radiologic approach and review. Curr Radiol Rep. 2018;6:23. doi: 10.1007/s40134-018-0279-3. [DOI] [Google Scholar]
- 32.Chen R., Gabler H.C. Risk of thoracic injury from direct steering wheel impact in frontal crashes. J Trauma Acute Care Surg. 2014;76:1441–1446. doi: 10.1097/TA.0000000000000222. [DOI] [PubMed] [Google Scholar]
- 33.Newgard C.D., Lewis R.J., Kraus J.F. Steering wheel deformity and serious thoracic or abdominal injury among drivers and passengers involved in motor vehicle crashes. Ann Emerg Med. 2005;45:43–50. doi: 10.1016/j.annemergmed.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Yadollahi M., Arabi A.H., Mahmoudi A. Blunt thoracic injury mortality and clinical presentation. Trauma Mon. 2018;23 doi: 10.5812/traumamon.13079. [DOI] [Google Scholar]
- 35.Martin T.J., Eltorai A.S., Dunn R. Clinical management of rib fractures and methods for prevention of pulmonary complications: a review. Injury. 2019;50:1159–1165. doi: 10.1016/j.injury.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 36.Grubmüller M., Kerschbaum M., Diepold E. Severe thoracic trauma – still an independent predictor for death in multiple injured patients? Scand J Trauma Resuscitation Emerg Med. 2018;26:6. doi: 10.1186/s13049-017-0469-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Narayanan R., Kumar S., Gupta A. An analysis of presentation, pattern and outcome of chest trauma patients at an urban level 1 trauma center. Indian J Surg. 2018;80:36–41. doi: 10.1007/s12262-016-1554-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Veysi V.T., Nikolaou V.S., Paliobeis C. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. Int Orthop. 2009;33:1425–1433. doi: 10.1007/s00264-009-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beal A.L., Ahrendt M.N., Irwin E.D. Prediction of blunt traumatic injuries and hospital admission based on history and physical exam. World J Emerg Surg. 2016;11:46. doi: 10.1186/s13017-016-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mistovich J.J., Hafen B.Q., Karren K.J. Brady Prentice Hall Health; Upper Saddle River, NJ: 2000. Prehospital Emergency Care. [Google Scholar]
- 41.Jones L. Chest trauma. Anaesth Intensive Care Med. 2008;9(9):394–397. doi: 10.1016/j.mpaic.2008.07.005. [DOI] [Google Scholar]
- 42.Hughes R.K. Thoracic trauma. Ann Thorac Surg. 1965;1:778–804. doi: 10.1016/S0003-4975(10)66827-0. [DOI] [PubMed] [Google Scholar]
- 43.Brasel K.J., Guse C.E., Layde P. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34:1642–1646. doi: 10.1097/01.CCM.0000217926.40975.4B. [DOI] [PubMed] [Google Scholar]
- 44.Karlson K.A., French A. Initial evaluation and management of rib fractures. https://www.uptodate.com/contents/initial-evaluation-and-management-of-rib-fractures UpToDate.
- 45.Richardson J.D., McELVEIN R.B., Trinkle J.K. First rib fracture: a hallmark of severe trauma. Ann Surg. 1975;181:251–254. doi: 10.1097/00000658-197503000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mirvis S.E. Diagnostic imaging of acute thoracic injury. Semin Ultrasound CT MRI. 2004;25:156–179. doi: 10.1016/j.sult.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 47.Mattox K.L., Moore E.E., Feliciano D.V. seventh ed. McGraw-Hill Publishing; New York, NY: 2012. Trauma. [Google Scholar]
- 48.Kani K.K., Mulcahy H., Porrino J.A. Thoracic cage injuries. Eur J Radiol. 2019;110:225–232. doi: 10.1016/j.ejrad.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 49.ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, International ATLS working group Advanced trauma life support (ATLS): the ninth edition. J Trauma Acute Care Surg. 2013;74:1363–1366. doi: 10.1097/TA.0b013e31828b82f5. https://corescholar.libraries.wright.edu/surg/122/ [DOI] [PubMed] [Google Scholar]
- 50.Senekjian L., Nirula R. Rib fracture fixation. Crit Care Clin. 2017;33:153–165. doi: 10.1016/j.ccc.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 51.Sırmalı M., Türüt H., Topçu S. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardio Thorac Surg. 2003;24:133–138. doi: 10.1016/S1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 52.Easter A. Management of patients with multiple rib fractures. Am J Crit Care. 2001;10:320–327. quiz 328-329. [PubMed] [Google Scholar]
- 53.Flagel B.T., Luchette F.A., Reed R.L. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138:717–723. doi: 10.1016/j.surg.2005.07.022. ; discussion 723-725. [DOI] [PubMed] [Google Scholar]
- 54.Stawicki S.P., Grossman M.D., Hoey B.A. Rib fractures in the elderly: a marker of injury severity: rib fractures IN the elderly. J Am Geriatr Soc. 2004;52:805–808. doi: 10.1111/j.1532-5415.2004.52223.x. [DOI] [PubMed] [Google Scholar]
- 55.Sharma O.P., Oswanski M.F., Jolly S. Perils of rib fractures. Am Surg. 2008;74:310–314. doi: 10.1177/000313480807400406. [DOI] [PubMed] [Google Scholar]
- 56.Lee R.B., Bass S.M., Morris J.A. Three or more rib fractures as an indicator for transfer to a level I trauma center: a population-based study. J Trauma. 1990;30(6):689–694. doi: 10.1097/00005373-199006000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Legome E. Initial evaluation and management of blunt thoracic trauma in adults. https://www.uptodate.com/contents/initial-evaluation-and-management-of-blunt-thoracic-trauma-in-adults UpToDate.
- 58.Holcomb J.B., McMullin N.R., Kozar R.A. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196:549–555. doi: 10.1016/S1072-7515(02)01894-X. [DOI] [PubMed] [Google Scholar]
- 59.May L., Hillermann C., Patil S. Rib fracture management. BJA Educ. 2016;16:26–32. doi: 10.1093/bjaceaccp/mkv011. [DOI] [Google Scholar]
- 60.Liman S., Kuzucu A., Tastepe A.I. Chest injury due to blunt trauma. Eur J Cardio Thorac Surg. 2003;23:374–378. doi: 10.1016/s1010-7940(02)00813-8. [DOI] [PubMed] [Google Scholar]
- 61.Hildebrand F., Andruszkow H., Pape H.-C. Chest trauma: classification and influence on the general management. In: Pape H.-C., Peitzman A.B., Rotondo M.F., editors. Damage Control Management in the Polytrauma Patient. Springer International Publishing; Cham: 2017. pp. 79–95. [DOI] [Google Scholar]
- 62.Garcia V.F., Gotschall C.S., Eichelberger M.R. Rib fractures in children: a marker of severe trauma. J Trauma. 1990;30:695–700. [PubMed] [Google Scholar]
- 63.Wintermark M., Schnyder P. Trauma of the chest wall. In: Schnyder P., Wintermark M., editors. Radiology of Blunt Trauma of the Chest. Springer Berlin Heidelberg; Berlin, Heidelberg: 2000. pp. 9–27. [DOI] [Google Scholar]
- 64.Ho M.L., Gutierrez F.R. Chest radiography in thoracic polytrauma. Am J Roentgenol. 2009;192:599–612. doi: 10.2214/AJR.07.3324. [DOI] [PubMed] [Google Scholar]
- 65.Altoos R., Carr R., Chung J. Selective common and uncommon imaging manifestations of blunt nonaortic chest trauma: when time is of the essence. Curr Probl Diagn Radiol. 2015;44:155–166. doi: 10.1067/j.cpradiol.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 66.Shorr R.M., Crittenden M., Indeck M. Blunt thoracic trauma analysis of 515 patients. Ann Surg. 1987;206:200–205. doi: 10.1097/00000658-198708000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eckstein M., Henderson S.O. Thoracic trauma. In: Marx J.A., Hockberger R.S., Walls R.M., editors. Rosen's Emergency Medicine – Concepts and Clinical Practice. Elsevier; 2010. pp. 387–413. [DOI] [Google Scholar]
- 68.Antonacci F., Renaud S., Mazzucco A. Chest wall and diaphragmatic injuries. In: Aseni P., De Carlis L., Mazzola A., editors. Operative Techniques and Recent Advances in Acute Care and Emergency Surgery. Springer International Publishing; Cham: 2019. pp. 273–280. [DOI] [Google Scholar]
- 69.Zreik N.H., Francis I., Ray A. Blunt chest trauma: bony injury in the thorax. Br J Hosp Med. 2016;77:72–77. doi: 10.12968/hmed.2016.77.2.72. [DOI] [PubMed] [Google Scholar]
- 70.Odell D.D., Peleg K., Givon A. Sternal fracture: isolated lesion versus polytrauma from associated extrasternal injuries—analysis of 1,867 cases. J Trauma Acute Care Surg. 2013;75:448–452. doi: 10.1097/TA.0b013e31829e227e. [DOI] [PubMed] [Google Scholar]
- 71.DeLuca S.A., Rhea J.T., O'Malley T.O. Radiographic evaluation of rib fractures. Am J Roentgenol. 1982;138:91–92. doi: 10.2214/ajr.138.1.91. [DOI] [PubMed] [Google Scholar]
- 72.Langdorf M.I., Medak A.J., Hendey G.W. Prevalence and clinical import of thoracic injury identified by chest computed tomography but not chest radiography in blunt trauma: multicenter prospective cohort study. Ann Emerg Med. 2015;66:589–600. doi: 10.1016/j.annemergmed.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Carrero R., Wayne M. Chest trauma. Emerg Med Clin. 1989;7:389–418. doi: 10.1016/j.mpaic.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 74.Davis S., Affatato A. Blunt chest trauma: utility of radiological evaluation and effect on treatment patterns. Am J Emerg Med. 2006;24:482–486. doi: 10.1016/j.ajem.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 75.Thoongsuwan N., Kanne J.P., Stern E.J. Spectrum of blunt chest injuries. J Thorac Imag. 2005;20:89–97. doi: 10.1097/01.rti.0000148210.89718.f5. [DOI] [PubMed] [Google Scholar]
- 76.Keel M., Meier C. Chest injuries – what is new? Curr Opin Crit Care. 2007;13:674–679. doi: 10.1097/MCC.0b013e3282f1fe71. [DOI] [PubMed] [Google Scholar]
- 77.Majercik S., Pieracci F.M. Chest wall trauma. Thorac Surg Clin. 2017;27:113–121. doi: 10.1016/j.thorsurg.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 78.Bastos R., Calhoon J.H., Baisden C.E. Flail chest and pulmonary contusion. Semin Thorac Cardiovasc Surg. 2008;20:39–45. doi: 10.1053/j.semtcvs.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 79.Borman J.B., Aharonson-Daniel L., Savitsky B. Unilateral flail chest is seldom a lethal injury. Emerg Med J. 2006;23:903–905. doi: 10.1136/emj.2006.037945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Naidoo K., Hanbali L., Bates P. The natural history of flail chest injuries. Chin J Traumatol. 2017;20:293–296. doi: 10.1016/j.cjtee.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dehghan N., de Mestral C., McKee M.D. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462–468. doi: 10.1097/TA.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 82.Clark G.C., Schecter W.P., Trunkey D.D. Variables affecting outcome in blunt chest trauma: flail chest vs. Pulmonary Contusion: J Trauma Inj Infect Crit Care. 1988;28:298–304. doi: 10.1097/00005373-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 83.Ciraulo D.L., Elliott D., Mitchell K.A. Flail chest as a marker for significant injuries. J Am Coll Surg. 1994;178:466–470. [PubMed] [Google Scholar]
- 84.Getz P., Mommsen P., Clausen J.-D. Limited influence of flail chest in patients with blunt thoracic trauma – a matched-pair analysis. In Vivo. 2019;33:133–139. doi: 10.21873/invivo.11449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Offner P.J., Moore E.E. Pulmonary complications of blunt chest injury. Clin Pulm Med. 1998;5:36–44. doi: 10.1097/00045413-199801000-00005. [DOI] [Google Scholar]
- 86.Ludwig C., Koryllos A. Management of chest trauma. J Thorac Dis. 2017;9:S172–S177. doi: 10.21037/jtd.2017.03.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Glinz W. Springer Berlin Heidelberg; Berlin, Heidelberg: 1981. Chest Trauma. [DOI] [Google Scholar]
- 88.Gunduz M., Unlugenc H., Ozalevli M. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005;22:325–329. doi: 10.1136/emj.2004.019786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lafferty P.M., Anavian J., Will R.E. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Jt Surg-Am. 2011;93:97–110. doi: 10.2106/JBJS.I.00696. [DOI] [PubMed] [Google Scholar]
- 90.Coughlin T.A., Ng J.W.G., Rollins K.E. Management of rib fractures in traumatic flail chest: a meta-analysis of randomised controlled trials. Bone Jt J. 2016;98-B:1119–1125. doi: 10.1302/0301-620X.98B8.37282. [DOI] [PubMed] [Google Scholar]
- 91.Swart E., Laratta J., Slobogean G. Operative treatment of rib fractures in flail chest injuries: a meta-analysis and cost-effectiveness analysis. J Orthop Trauma. 2017;31:64–70. doi: 10.1097/BOT.0000000000000750. [DOI] [PubMed] [Google Scholar]
- 92.Granetzny A., Abd El-Aal M., Emam E. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4:583–587. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 93.Marasco S.F., Davies A.R., Cooper J. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216:924–932. doi: 10.1016/j.jamcollsurg.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 94.Pharaon K.S., Marasco S., Mayberry J. Rib fractures, flail chest, and pulmonary contusion. Curr Trauma Rep. 2015;1:237–242. doi: 10.1007/s40719-015-0026-7. [DOI] [Google Scholar]
- 95.Landercasper J., Cogbill T.H., Lindesmith L.A. Long-term disability after flail chest injury. J Trauma Inj Infect Crit Care. 1984;24:410–414. doi: 10.1097/00005373-198405000-00007. [DOI] [PubMed] [Google Scholar]
- 96.Nirula R., Diaz J.J., Trunkey D.D. Rib fracture repair: indications, technical issues, and future directions. World J Surg. 2009;33:14–22. doi: 10.1007/s00268-008-9770-y. [DOI] [PubMed] [Google Scholar]
- 97.Beal S.L., Oreskovich M.R. Long-term disability associated with flail chest injury. Am J Surg. 1985;150:324–326. doi: 10.1016/0002-9610(85)90071-6. [DOI] [PubMed] [Google Scholar]
- 98.Wilson H., Ellsmere J., Tallon J. Occult pneumothorax in the blunt trauma patient: tube thoracostomy or observation? Injury. 2009;40:928–931. doi: 10.1016/j.injury.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 99.Haynes D., Baumann M. Management of pneumothorax. Semin Respir Crit Care Med. 2010;31:769–780. doi: 10.1055/s-0030-1269837. [DOI] [PubMed] [Google Scholar]
- 100.Bridges K.G., Welch G., Silver M. CT detection of occult pneumothorax in multiple trauma patients. J Emerg Med. 1993;11:179–186. doi: 10.1016/0736-4679(93)90517-b. [DOI] [PubMed] [Google Scholar]
- 101.Sassoon C.S.H., Light R.W., O'Hara V.S. Iatrogenic pneumothorax: etiology and morbidity. Respiration. 1992;59:215–220. doi: 10.1159/000196061. [DOI] [PubMed] [Google Scholar]
- 102.Lewis F.R., Jr., Blaisdell F.W., Schlobohm R.M. Incidence and outcome of posttraumatic respiratory failure. Arch Surg. 1977;112:436–443. doi: 10.1001/archsurg.1977.01370040088014. [DOI] [PubMed] [Google Scholar]
- 103.Reuter M. Trauma of the chest. Eur Radiol. 1996;6:707–716. doi: 10.1007/BF00187678. [DOI] [PubMed] [Google Scholar]
- 104.Sharma A., Jindal P. Principles of diagnosis and management of traumatic pneumothorax. J Emergencies, Trauma, Shock. 2008;1:34–41. doi: 10.4103/0974-2700.41789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Berlot G., Massarutti D., Carchietti E. Treatment of acute pneumothorax in the field. In: Gullo A., editor. Anaesthesia, Pain, Intensive Care and Emergency Medicine — A.P.I.C.E. Springer Milan; Milano: 2005. pp. 683–691. [DOI] [Google Scholar]
- 106.Arshad H., Young M., Adurty R. Acute pneumothorax. Crit Care Nurs Q. 2016;39:176–189. doi: 10.1097/CNQ.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 107.Driscoll P., Gwinnutt C., Goodall O. Thoracic trauma. In: Driscoll P.A., Gwinnutt C.L., Jimmerson C.L., editors. Trauma Resuscitation. Macmillan Education UK; London: 1993. pp. 67–101. [DOI] [Google Scholar]
- 108.de Lesquen H., Avaro J.P., Gust L. Surgical management for the first 48 h following blunt chest trauma: state of the art (excluding vascular injuries) Interact Cardiovasc Thorac Surg. 2015;20:399–408. doi: 10.1093/icvts/ivu397. [DOI] [PubMed] [Google Scholar]
- 109.Ball C.G., Kirkpatrick A.W., Laupland K.B. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59:917–925. doi: 10.1097/01.ta.0000174663.46453.86. [DOI] [PubMed] [Google Scholar]
- 110.Rowan K.R., Kirkpatrick A.W., Liu D. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT—initial experience. Radiology. 2002;225:210–214. doi: 10.1148/radiol.2251011102. [DOI] [PubMed] [Google Scholar]
- 111.Ball C.G., Kirkpatrick A.W., Feliciano D.V. The occult pneumothorax: what have we learned? Can J Surg. 2009;52:E173–E179. [PMC free article] [PubMed] [Google Scholar]
- 112.Zreik N.H., Francis I., Ray A. Blunt chest trauma: soft tissue injury in the thorax. Br J Hosp Med. 2016;77:78–83. doi: 10.12968/hmed.2016.77.2.78. [DOI] [PubMed] [Google Scholar]
- 113.Dennis B.M., Bellister S.A., Guillamondegui O.D. Thoracic trauma. Surg Clin. 2017;97:1047–1064. doi: 10.1016/j.suc.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 114.Wolfman N.T., Myers W.S., Glauser S.J. Validity of CT classification on management of occult pneumothorax: a prospective study. Am J Roentgenol. 1998;171:1317–1320. doi: 10.2214/ajr.171.5.9798871. [DOI] [PubMed] [Google Scholar]
- 115.Hill S.L., Edmisten T., Holtzman G. The occult pneumothorax: an increasing diagnostic entity in trauma. Am Surg. 1999;65:254–258. [PubMed] [Google Scholar]
- 116.Khan H.S., Wadood A., Ayyaz M. Occult pneumothorax: what do we need to do? J Coll Physicians Surg Pak. 2018;28:S31–S32. doi: 10.29271/jcpsp.2018.03.S31. [DOI] [PubMed] [Google Scholar]
- 117.Omar H.R., Abdelmalak H., Mangar D. Occult pneumothorax, revisited. J Trauma Manag Outcome. 2010;4:12. doi: 10.1186/1752-2897-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Blaivas M., Lyon M., Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844–849. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 119.Northfield T.C. Oxygen therapy for spontaneous pneumothorax. Br Med J. 1971;4:86–88. doi: 10.1136/bmj.4.5779.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zarogoulidis P., Kioumis I., Pitsiou G. Pneumothorax: from definition to diagnosis and treatment. J Thorac Dis. 2014;6:S372–S376. doi: 10.3978/j.issn.2072-1439.2014.09.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Leech C., Porter K., Steyn R. The pre-hospital management of life-threatening chest injuries: a consensus statement from the Faculty of Pre-Hospital Care. Trauma. 2017;19:54–62. doi: 10.1177/1460408616664553. Royal College of Surgeons of Edinburgh. [DOI] [Google Scholar]
- 122.Ball C.G., Hameed S.M., Evans D. Canadian Trauma Trials Collaborative. Occult pneumothorax in the mechanically ventilated trauma patient. Can J Surg. 2003;46:373–379. [PMC free article] [PubMed] [Google Scholar]
- 123.Yadav K., Jalili M., Zehtabchi S. Management of traumatic occult pneumothorax. Resuscitation. 2010;81:1063–1068. doi: 10.1016/j.resuscitation.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 124.Etoch S.W., Bar-Natan M.F., Miller F.B. Tube thoracostomy: factors related to complications. Arch Surg. 1995;130:521–526. doi: 10.1001/archsurg.1995.01430050071012. [DOI] [PubMed] [Google Scholar]
- 125.Bailey R.C. Complications of tube thoracostomy in trauma. J Accid Emerg Med. 2000;17:111–114. doi: 10.1136/emj.17.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Farooq U., Raza W., Zia N. Classification and management of chest trauma. J Coll Physicians Surg Pak. 2006;16:101–103. doi: 10.2006/JCPSP.101103. [DOI] [PubMed] [Google Scholar]
- 127.Huang Y., Huang H., Li Q. Approach of the treatment for pneumothorax. J Thorac Dis. 2014;6:416–420. doi: 10.3978/j.issn.2072-1439.2014.08.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Azfar Ali H., Lippmann M., Mundathaje U. Spontaneous Hemothorax: a comprehensive review. Chest. 2008;134:1056–1065. doi: 10.1378/chest.08-0725. [DOI] [PubMed] [Google Scholar]
- 129.Tsai F.C., Chang Y.S., Lin P.J. Blunt trauma with flail chest and penetrating aortic injury. Eur J Cardio Thorac Surg. 1999;16:374–377. doi: 10.1016/S1010-7940(99)00230-4. [DOI] [PubMed] [Google Scholar]
- 130.Bozzay J.D., Bradley M.J. Management of post-traumatic retained hemothorax. Trauma. 2019;21:14–20. doi: 10.1177/1460408617752985. [DOI] [Google Scholar]
- 131.Boersma W.G., Stigt J.A., Smit H.J. Treatment of haemothorax. Respir Med. 2010;104:1583–1587. doi: 10.1016/j.rmed.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 132.Yu H., Isaacson A.J., Burke C.T. Management of traumatic hemothorax, retained hemothorax, and other thoracic collections. Curr Trauma Rep. 2017;3:181–189. doi: 10.1007/s40719-017-0101-3. [DOI] [Google Scholar]
- 133.Sinha P., Sarkar P. Late clotted haemothorax after blunt chest trauma. J Accid Emerg Med. 1998;15:189–191. doi: 10.1136/emj.15.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Stewart R.M., Corneille M.G. Common complications following thoracic trauma: their prevention and treatment. Semin Thorac Cardiovasc Surg. 2008;20:69–71. doi: 10.1053/j.semtcvs.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 135.Majercik S., Vijayakumar S., Olsen G. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg. 2015;210:1112–1117. doi: 10.1016/j.amjsurg.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 136.Eren S., Esme H., Sehitogullari A. The risk factors and management of posttraumatic empyema in trauma patients. Injury. 2008;39:44–49. doi: 10.1016/j.injury.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 137.Chou Y.P., Kuo L.C., Soo K.M. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardio Thorac Surg. 2014;46:107–111. doi: 10.1093/ejcts/ezt523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Villegas M.I., Hennessey R.A., Morales C.H. Risk factors associated with the development of post-traumatic retained hemothorax. Eur J Trauma Emerg Surg. 2011;37:583–589. doi: 10.1007/s00068-010-0064-3. [DOI] [PubMed] [Google Scholar]
- 139.Misthos P., Kakaris S., Sepsas E. A prospective analysis of occult pneumothorax, delayed pneumothorax and delayed hemothorax after minor blunt thoracic trauma. Eur J Cardio Thorac Surg. 2004;25:859–864. doi: 10.1016/j.ejcts.2004.01.044. [DOI] [PubMed] [Google Scholar]
- 140.Plourde M., Émond M., Lavoie A. Cohort study on the prevalence and risk factors for delayed pulmonary complications in adults following minor blunt thoracic trauma. CJEM. 2014;16:136–143. doi: 10.2310/8000.2013.131043. [DOI] [PubMed] [Google Scholar]
- 141.Bokhari F., Brakenridge S., Nagy K. Prospective evaluation of the sensitivity of physical examination in chest trauma. J Trauma Inj Infect Crit Care. 2002;53:1135–1138. doi: 10.1097/00005373-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 142.Trupka A., Kierse R., Waydhas C. Shock room diagnosis in polytrauma. Value of thoracic CT. Unfallchirurg. 1997;100:469–476. doi: 10.1007/s001130050144. [DOI] [PubMed] [Google Scholar]
- 143.Demetriades D., Talving P., Inaba K. Chest trauma. In: Oestern H.-J., Trentz O.L., Uranues S., editors. Head, Thoracic, Abdominal, and Vascular Injuries. Springer Berlin Heidelberg; Berlin, Heidelberg: 2011. pp. 223–255. [DOI] [Google Scholar]
- 144.Feden J.P. Closed lung trauma. Clin Sports Med. 2013;32:255–265. doi: 10.1016/j.csm.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 145.Chung M.H., Hsiao C.Y., Nian N.S. The benefit of ultrasound in deciding between tube thoracostomy and observative management in hemothorax resulting from blunt chest trauma. World J Surg. 2018;42:2054–2060. doi: 10.1007/s00268-017-4417-5. [DOI] [PubMed] [Google Scholar]
- 146.Staub L.J., Biscaro R.R.M., Kaszubowski E. Chest ultrasonography for the emergency diagnosis of traumatic pneumothorax and haemothorax: a systematic review and meta-analysis. Injury. 2018;49:457–466. doi: 10.1016/j.injury.2018.01.033. [DOI] [PubMed] [Google Scholar]
- 147.Mowery N.T., Gunter O.L., Collier B.R. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011;70:510–518. doi: 10.1097/TA.0b013e31820b5c31. [DOI] [PubMed] [Google Scholar]
- 148.Conn A. Chest trauma. In: Legome E., Shockley L.W., editors. Trauma: A Comprehensive Emergency Medicine Approach. Cambridge University Press; Cambridge: 2011. pp. 190–212. [Google Scholar]
- 149.Parry G.W., Morgan W.E., Salama F.D. Management of haemothorax. Ann R Coll Surg Engl. 1996;78:325–326. [PMC free article] [PubMed] [Google Scholar]
- 150.Ball C.G., Lord J., Laupland K.B. Chest tube complications: how well are we training our residents? Can J Surg. 2007;50:450–458. [PMC free article] [PubMed] [Google Scholar]
- 151.Chiumello D., Coppola S. Oxford Textbook of Critical Care. second ed. Oxford University Press; 2016. Management of pleural effusion and haemothorax. [DOI] [Google Scholar]
- 152.Wells B.J., Roberts D.J., Grondin S. To drain or not to drain? Predictors of tube thoracostomy insertion and outcomes associated with drainage of traumatic hemothoraces. Injury. 2015;46:1743–1748. doi: 10.1016/j.injury.2015.04.032. [DOI] [PubMed] [Google Scholar]
- 153.Demetri L., Martinez Aguilar M.M., Bohnen J.D. Is observation for traumatic hemothorax safe? J Trauma Acute Care Surg. 2018;84:454–458. doi: 10.1097/ta.0000000000001793. [DOI] [PubMed] [Google Scholar]
- 154.Lin H.L., Huang W.Y., Yang C. How early should VATS be performed for retained haemothorax in blunt chest trauma? Injury. 2014;45:1359–1364. doi: 10.1016/j.injury.2014.05.036. [DOI] [PubMed] [Google Scholar]
- 155.Meyer D.M. Hemothorax related to trauma. Thorac Surg Clin. 2007;17:47–55. doi: 10.1016/j.thorsurg.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 156.Požgain Z., Kristek D., Lovrić I. Pulmonary contusions after blunt chest trauma: clinical significance and evaluation of patient management. Eur J Trauma Emerg Surg. 2018;44:773–777. doi: 10.1007/s00068-017-0876-5. [DOI] [PubMed] [Google Scholar]
- 157.Ganie F.A., Lone H., Lone G.N. Lung contusion: a clinico-pathological entity with unpredictable clinical course. Bull Emerg Trauma. 2013;1:7–16. [PMC free article] [PubMed] [Google Scholar]
- 158.Wanek S., Mayberry J.C. Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20:71–81. doi: 10.1016/S0749-0704(03)00098-8. [DOI] [PubMed] [Google Scholar]
- 159.Bader A., Rahman U., Morris M. Pulmonary contusions in the elderly after blunt trauma: incidence and outcomes. J Surg Res. 2018;230:110–116. doi: 10.1016/j.jss.2018.04.049. [DOI] [PubMed] [Google Scholar]
- 160.Elmali M., Baydin A., Nural M.S. Lung parenchymal injury and its frequency in blunt thoracic trauma: the diagnostic value of chest radiography and thoracic CT. Diagn Interv Radiol. 2007;13:179–182. [PubMed] [Google Scholar]
- 161.Allen G.S., Cox C.S., Moore F.A. Pulmonary contusion: are children different. J Am Coll Surg. 1997;185:229–233. doi: 10.1016/S1072-7515(01)00920-6. [DOI] [PubMed] [Google Scholar]
- 162.Cohn S.M., DuBose J.J. Pulmonary contusion: an update on recent advances in clinical management. World J Surg. 2010;34:1959–1970. doi: 10.1007/s00268-010-0599-9. [DOI] [PubMed] [Google Scholar]
- 163.Balcı A.E., Balcı T.A., Eren Ş. Unilateral post-traumatic pulmonary contusion: findings of a review. Surg Today. 2005;35:205–210. doi: 10.1007/s00595-004-2925-z. [DOI] [PubMed] [Google Scholar]
- 164.Stern E. Imaging of blunt and penetrating trauma to the pulmonary parenchyma. In: Karmy-Jones R., Nathens A., Stern E.J., editors. Thoracic Trauma and Critical Care. Springer US; Boston, MA: 2002. pp. 159–164. [DOI] [Google Scholar]
- 165.Roux P., Fisher R.M. Chest injuries in children: an analysis of 100 cases of blunt chest trauma from motor vehicle accidents. J Pediatr Surg. 1992;27:551–555. doi: 10.1016/0022-3468(92)90443-B. [DOI] [PubMed] [Google Scholar]
- 166.Berland M., Oger M., Cauchois E. Pulmonary contusion after bumper car collision: case report and review of the literature. Respir Med Case Rep. 2018;25:293–295. doi: 10.1016/j.rmcr.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.O'Connor J.V., Kufera J.A., Kerns T.J. Crash and occupant predictors of pulmonary contusion. J Trauma. 2009;66:1091–1095. doi: 10.1097/TA.0b013e318164d097. [DOI] [PubMed] [Google Scholar]
- 168.O'Connor J., Adamski J. The diagnosis and treatment of non-cardiac thoracic trauma. J Roy Army Med Corps. 2010;156:5–14. doi: 10.1136/jramc-156-01-02. [DOI] [PubMed] [Google Scholar]
- 169.Mizushima Y., Hiraide A., Shimazu T. Changes in contused lung volume and oxygenation in patients with pulmonary parenchymal injury after blunt chest trauma. Am J Emerg Med. 2000;18:385–389. doi: 10.1053/ajem.2000.7317. [DOI] [PubMed] [Google Scholar]
- 170.Bradley M., Okoye O., DuBose J. Risk factors for post-traumatic pneumonia in patients with retained haemothorax: results of a prospective, observational AAST study. Injury. 2013;44:1159–1164. doi: 10.1016/j.injury.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 171.Horst K., Andruszkow H., Weber C.D. Thoracic trauma now and then: a 10 year experience from 16,773 severely injured patients. PloS One. 2017;12 doi: 10.1371/journal.pone.0186712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Rendeki S., Molnár T.F. Pulmonary contusion. J Thorac Dis. 2019;11:S141–S151. doi: 10.21037/jtd.2018.11.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Perl M., Gebhard F., Brückner U.B. Pulmonary contusion causes impairment of macrophage and lymphocyte immune functions and increases mortality associated with a subsequent septic challenge. Crit Care Med. 2005;33:1351–1358. doi: 10.1097/01.CCM.0000166352.28018. A9. [DOI] [PubMed] [Google Scholar]
- 174.Tanaka H., Yukioka T., Yamaguti Y. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–732. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 175.Arjun P., Najeeb A.A., Ramachandran R. Lung contusion. Lung India. 2018;35:263–264. doi: 10.4103/lungindia.lungindia_81_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Allen G.S., Coates N.E. Pulmonary contusion: a collective review. Am Surg. 1996;62:895–900. [PubMed] [Google Scholar]
- 177.Garzon A.A., Seltzer B., Karlson K.E. Physiopathology of crushed chest injuries. Ann Surg. 1968;168(1):128–136. doi: 10.1097/00000658-196807000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Richardson J.D., Adams L., Flint L.M. Selective management of flail chest and pulmonary contusion. Ann Surg. 1982;196:481–487. doi: 10.1097/00000658-198210000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Horst K., Simon T.P., Pfeifer R. Characterization of blunt chest trauma in a long-term porcine model of severe multiple trauma. Sci Rep. 2016;6:39659. doi: 10.1038/srep39659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Miller P.R., Croce M.A., Bee T.K. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51:223–230. doi: 10.1097/00005373-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 181.Richardson J.D., Franz J.L., Grover F.L. Pulmonary contusion and hemorrhage—crystalloid versus colloid replacement. J Surg Res. 1974;16:330–336. doi: 10.1016/0022-4804(74)90051-1. [DOI] [PubMed] [Google Scholar]
- 182.Karmy-Jones R., Jurkovich G.J. Blunt chest trauma. Curr Probl Surg. 2004;41:223–380. doi: 10.1016/j.cpsurg.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 183.Miller D.L., Mansour K.A. Blunt traumatic lung injuries. Thorac Surg Clin. 2007;17:57–61. doi: 10.1016/j.thorsurg.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 184.Tovar J.A. The lung and pediatric trauma. Semin Pediatr Surg. 2008;17:53–59. doi: 10.1053/j.sempedsurg.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 185.Moghissi K. Laceration of the lung following blunt trauma. Thorax. 1971;26:223–228. doi: 10.1136/thx.26.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Abdel Bary M., Branscheid D., Mertzlufft F. Long term management of thoracic trauma in a high frequency trauma center; what have we learned? J Egypt Soc Cardio-Thorac Surg. 2018;26:73–81. doi: 10.1016/j.jescts.2017.12.004. [DOI] [Google Scholar]
- 187.Huber S., Biberthaler P., Delhey P. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU®) Scand J Trauma Resuscitation Emerg Med. 2014;22:52. doi: 10.1186/s13049-014-0052-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Hollister M., Stern E.J., Steinberg K.P. Type 2 pulmonary laceration: a marker of blunt high-energy injury to the lung. Am J Roentgenol. 1995;165:1126. doi: 10.2214/ajr.165.5.7572488. [DOI] [PubMed] [Google Scholar]
- 189.Kaewlai R., Avery L.L., Asrani A.V. Multidetector CT of blunt thoracic trauma. Radiographics. 2008;28:1555–1570. doi: 10.1148/rg.286085510. [DOI] [PubMed] [Google Scholar]
- 190.Haxhija E.Q., Nöres H., Schober P. Lung contusion-lacerations after blunt thoracic trauma in children. Pediatr Surg Int. 2004;20:412–414. doi: 10.1007/s00383-004-1165-z. [DOI] [PubMed] [Google Scholar]
- 191.Caterino U. Computed tomography changing over time in type 1 pulmonary laceration. Ann Emerg Med. 2009;54:156–157. doi: 10.1016/j.annemergmed.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 192.Mirka H., Ferda J., Baxa J. Multidetector computed tomography of chest trauma: indications, technique and interpretation. Insights Imaging. 2012;3:433–449. doi: 10.1007/s13244-012-0187-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Nishiumi N., Inokuchi S., Oiwa K. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg. 2010;89:232–238. doi: 10.1016/j.athoracsur.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 194.Carson D., Edwards R. Core curriculum illustration: pulmonary laceration. Emerg Radiol. 2017 doi: 10.1007/s10140-017-1547-x. [DOI] [PubMed] [Google Scholar]
- 195.Ota H., Kawai H., Togashi S. Video-assisted minithoracotomy for pulmonary laceration with a massive hemothorax. Case Rep Emerg Med. 2014;2014:454970. doi: 10.1155/2014/454970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Van Hise M.L., Primack S.L., Israel R.S. CT in blunt chest trauma: indications and limitations. Radiographics. 1998;18:1071–1084. doi: 10.1148/radiographics.18.5.9747608. [DOI] [PubMed] [Google Scholar]
- 197.Mirvis S.E., Shanmuganathan K. Trauma radiology: Part II. Diagnostic imaging of thoracic trauma: review and update. J Intensive Care Med. 1994;9:179–190. doi: 10.1177/088506669400900403. [DOI] [PubMed] [Google Scholar]
- 198.Gao F., Shi H., Wang R. The performance of multi-slice spiral CT in pulmonary laceration and its application value. Med Imaging Process Technol. 2018;1 doi: 10.24294/mipt.v1i1.403. [DOI] [Google Scholar]
- 199.Yeh D.D., Lee J. Trauma and blast injuries. In: Mason R.J., Thom V.C.B., editors. Murray and Nadel's Textbook of Respiratory Medicine. Elsevier; 2016. pp. 1354–1366. e4. [DOI] [Google Scholar]
- 200.George R.B., Light R.W., Matthay M.A., editors. Chest Medicine: Essentials of Pulmonary and Critical Care Medicine. fifth ed. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 201.Bingol-Kologlu M., Fedakar M., Yagmurlu A. Tracheobronchial rupture due to blunt chest trauma: report of a case. Surg Today. 2006;36:823–826. doi: 10.1007/s00595-005-3240-z. [DOI] [PubMed] [Google Scholar]
- 202.Miller B.S., Shafi S., Thal E.R. Damage control in complex penetrating tracheal injury and silicone T-tube. J Trauma. 2008;64:E18–E20. doi: 10.1097/01.ta.0000196762.43093.c9. [DOI] [PubMed] [Google Scholar]
- 203.Misao T., Yoshikawa T., Aoe M. Bronchial and cardiac ruptures due to blunt trauma. Gen Thorac Cardiovasc Surg. 2011;59:216–219. doi: 10.1007/s11748-010-0638-3. [DOI] [PubMed] [Google Scholar]
- 204.Baumgartner F., Sheppard B., de Virgilio C. Tracheal and main bronchial disruptions after blunt chest trauma: presentation and management. Ann Thorac Surg. 1990;50:569–574. doi: 10.1016/0003-4975(90)90191-8. [DOI] [PubMed] [Google Scholar]
- 205.Roxburgh J.C. Rupture of the tracheobronchial tree. Thorax. 1987;42:681–688. doi: 10.1136/thx.42.9.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Cheaito A., Tillou A., Lewis C. Traumatic bronchial injury. Int J Surg Case Rep. 2016;27:172–175. doi: 10.1016/j.ijscr.2016.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Kirsh M.M., Orringer M.B., Behrendt D.M. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann Thorac Surg. 1976;22:93–101. doi: 10.1016/S0003-4975(10)63961-6. [DOI] [PubMed] [Google Scholar]
- 208.Taskinen S.O., Salo J.A., Halttunen P.E.A. Tracheobronchial rupture due to blunt chest trauma: a follow-up study. Ann Thorac Surg. 1989;48:846–849. doi: 10.1016/0003-4975(89)90683-8. [DOI] [PubMed] [Google Scholar]
- 209.Shemmeri E., Vallières E. Blunt tracheobronchial trauma. Thorac Surg Clin. 2018;28:429–434. doi: 10.1016/j.thorsurg.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 210.Kiser A.C., O'Brien S.M., Detterbeck F.C. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg. 2001;71:2059–2065. doi: 10.1016/S0003-4975(00)02453-X. [DOI] [PubMed] [Google Scholar]
- 211.Saad R., Jr., Gonçalves R., Dorgan Neto V. Tracheobronchial injuries in chest trauma: a 17-year experience. Rev Col Bras Cir. 2017;44:194–201. doi: 10.1590/0100-69912017002014. [DOI] [PubMed] [Google Scholar]
- 212.Farzanegan R., Alijanipour P., Akbarshahi H. Major airways trauma, management and long term results. Ann Thorac Cardiovasc Surg. 2011;17:544–551. doi: 10.5761/atcs.oa.11.01679. [DOI] [PubMed] [Google Scholar]
- 213.Rossbach M.M., Johnson S.B., Gomez M.A. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg. 1998;65:182–186. doi: 10.1016/S0003-4975(97)01001-1. [DOI] [PubMed] [Google Scholar]
- 214.Saillant N.N., Sein V. Management of severe chest wall trauma. J Emerg Crit Care Med. 2018;2 doi: 10.21037/jeccm.2018.04.03. 41-41. [DOI] [Google Scholar]
- 215.Self M.L., Mangram A., Berne J.D. Nonoperative management of severe tracheobronchial injuries with positive end-expiratory pressure and low tidal volume ventilation. J Trauma. 2005;5:1072–1075. doi: 10.1097/01.ta.0000188643.67949.82. [DOI] [PubMed] [Google Scholar]
- 216.Mohammadzadeh A.R., Kayalha H. Delayed diagnosis of bronchial transection following blunt chest trauma. Asian Cardiovasc Thorac Ann. 2017;25:540–543. doi: 10.1177/0218492317728665. [DOI] [PubMed] [Google Scholar]
- 217.Schneider T., Volz K., Dienemann H. Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg. 2009;8:571–576. doi: 10.1510/icvts.2008.196790. [DOI] [PubMed] [Google Scholar]
- 218.Evagelopoulos N., Tossios P., Wanke W. Tracheobronchial rupture after emergency intubation. Thorac Cardiovasc Surg. 1999;47:395–397. doi: 10.1055/s-2007-1013183. [DOI] [PubMed] [Google Scholar]
- 219.Wong E.H., Knight S. Tracheobronchial injuries from blunt trauma. ANZ J Surg. 2006;76:414–415. doi: 10.1111/j.1445-2197.2006.03738.x. [DOI] [PubMed] [Google Scholar]
- 220.Dertsiz L., Arici G., Arslan G. Acute tracheobronchial injuries: early and late term outcomes. Ulus Travma Acil Cerrahi Derg. 2007;13:128–134. [PubMed] [Google Scholar]
- 221.Platz J.J., Fabricant L., Norotsky M. Thoracic trauma. Surg Clin. 2017;97:783–799. doi: 10.1016/j.suc.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 222.Johnson S.B. Tracheobronchial injury. Semin Thorac Cardiovasc Surg. 2008;20:52–57. doi: 10.1053/j.semtcvs.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 223.Dominguez E., De La Torre C., Sánchez A.V. Severe tracheobronchial injuries: our experience. Eur J Pediatr Surg. 2015;25:71–76. doi: 10.1055/s-0034-1386642. [DOI] [PubMed] [Google Scholar]
- 224.Mahmodlou R., Sepehrvand N. Tracheobronchial injury due to blunt chest trauma. Int J Crit Illn Inj Sci. 2015;5:116–118. doi: 10.4103/2229-5151.158417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Flynn A.E., Thomas A.N., Schecter W.P. Acute Tracheobronchial Injury: J Trauma. 1989;29:1326–1330. doi: 10.1097/00005373-198910000-00005. [DOI] [PubMed] [Google Scholar]
- 226.Chu C.P., Chen P.P. Tracheobronchial injury secondary to blunt chest trauma: diagnosis and management. Anaesth Intensive Care. 2002;30:145–152. doi: 10.1177/0310057X0203000204. [DOI] [PubMed] [Google Scholar]
- 227.Welter S. Repair of tracheobronchial injuries. Thorac Surg Clin. 2014;24:41–50. doi: 10.1016/j.thorsurg.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 228.Gómez-Caro A., Ausín P., Moradiellos F.J. Role of conservative medical management of tracheobronchial injuries. J Trauma. 2006;61:1426–1435. doi: 10.1097/01.ta.0000196801.52594.b5. [DOI] [PubMed] [Google Scholar]
- 229.Carretta A., Melloni G., Bandiera A. Conservative and surgical treatment of acute posttraumatic tracheobronchial injuries. World J Surg. 2011;35:2568–2574. doi: 10.1007/s00268-011-1227-z. [DOI] [PubMed] [Google Scholar]
- 230.Alassal M.A., Ibrahim B.M., Elsadeck N. Traumatic intrathoracic tracheobronchial injuries: a study of 78 cases. Asian Cardiovasc Thorac Ann. 2014;22:816–823. doi: 10.1177/0218492313516777. [DOI] [PubMed] [Google Scholar]
- 231.Rocco G., Allen M. Bronchial repair with pulmonary preservation for severe blunt trauma. Thorac Cardiovasc Surg. 2001;49:231–233. doi: 10.1055/s-2001-16099. [DOI] [PubMed] [Google Scholar]
- 232.Sobrino J., Shafi S. Timing and causes of death after injuries. SAVE Proc. 2013;26:120–123. doi: 10.1080/08998280.2013.11928934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Tsai Y., Lin K., Huang T. Outcomes of patients with blunt chest trauma encountered at emergency department and possible risk factors affecting mortality. J Med Sci. 2017;37:97–101. doi: 10.4103/jmedsci.jmedsci_123_16. [DOI] [Google Scholar]
- 234.Trunkey D.D. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am. 1983;249:28–35. doi: 10.1038/scientificamerican0883-28. [DOI] [PubMed] [Google Scholar]
- 235.Pfeifer R., Teuben M., Andruszkow H. Mortality patterns in patients with multiple trauma: a systematic review of autopsy studies. PloS One. 2016;11 doi: 10.1371/journal.pone.0148844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Shackford S.R., Mackersie R.C., Holbrook T.L. The epidemiology of traumatic death. A population-based analysis. Arch Surg. 1993;128:571–575. doi: 10.1001/archsurg.1993.01420170107016. [DOI] [PubMed] [Google Scholar]
- 237.Bellone A., Bossi I., Etteri M. Factors associated with ICU admission following blunt chest trauma. Canc Res J. 2016;2016:3257846. doi: 10.1155/2016/3257846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Battle C., Hutchings H., Evans P.A. Blunt chest wall trauma: a review. Trauma. 2013;15:156–175. doi: 10.1177/1460408613488480. [DOI] [Google Scholar]
- 239.Dongel I., Coskun A., Ozbay S. Management of thoracic trauma in emergency service: analysis of 1139 cases. Pak J Med Sci. 2013;29:58–63. doi: 10.12669/pjms.291.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Koutsoukou A., Katsiari M., Orfanos S.E. Respiratory mechanics in brain injury: a review. World J Crit Care Med. 2016;5:65–73. doi: 10.5492/wjccm.v5.i1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Noorbakhsh M.R., Kriley I.R. Management of severe respiratory failure in complex trauma patients. J Emerg Crit Care Med March. 2018;2(3):26. http://jeccm.amegroups.com/article/view/4132/4733 [Google Scholar]
- 242.Dai D., Yuan Q., Sun Y. Impact of Thoracic Injury on Traumatic Brain Injury Outcome. In: Woloschak G.E., editor. vol. 8. 2013. (PloS One). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Guérin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 244.Witt C.E., Bulger E.M. Comprehensive approach to the management of the patient with multiple rib fractures: a review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open. 2017;2 doi: 10.1136/tsaco-2016-000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ustaalioglu R., Yildirim M., Cosgun H. Thoracic traumas: a single-center experience. Turk Thorac J. 2015;16:59–63. doi: 10.5152/ttd.2015.4413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Traub M., Stevenson M., McEvoy S. The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury. 2007;38:43–47. doi: 10.1016/j.injury.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 247.Trupka A., Waydhas C., Hallfeldt K.K.J. Value of thoracic computed tomography in the first assessment of severely injured patients with blunt chest trauma: results of a prospective study. J Trauma. 1997;43:405–412. doi: 10.1097/00005373-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 248.Shorr R.M., Rodriguez A., Indeck M.C. Blunt chest trauma in the elderly. J Trauma. 1989;29:234–237. doi: 10.1097/00005373-198902000-00016. [DOI] [PubMed] [Google Scholar]
- 249.Elbaih A. Patterns and management of chest injuries patients and its outcome in emergency department in suez canal university hospital, Egypt. Med Sci Int Med J. 2017;1 doi: 10.5455/medscience.2016.05.8567. [DOI] [Google Scholar]
- 250.Aswegen H van, Reeve J., Beach L. Physiotherapy management of patients with major chest trauma: results from a global survey. Trauma. 2019 doi: 10.1177/1460408619850918. 146040861985091. [DOI] [Google Scholar]
- 251.Gabram S.G.A., Schwartz R.J., Jacobs L.M. Clinical management of blunt trauma patients with unilateral rib fractures: a randomized trial. World J Surg. 1995;19:388–393. doi: 10.1007/BF00299166. [DOI] [PubMed] [Google Scholar]
- 252.Loeser J.D., Treede R.D. The kyoto protocol of IASP basic pain terminology. Pain. 2008;137(3):473–477. doi: 10.1016/j.pain.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 253.Karmakar M.K., Ho A.M. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54:615–625. doi: 10.1097/01.TA.0000053197.40145.62. [DOI] [PubMed] [Google Scholar]
- 254.Papadakos P.J., Karcz M., Lachmann B. Mechanical ventilation in trauma. Curr Opin Anaesthesiol. 2010;23:228–232. doi: 10.1097/ACO.0b013e328336ea6e. [DOI] [PubMed] [Google Scholar]
- 255.Unsworth A., Curtis K., Asha S.E. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resuscitation Emerg Med. 2015;23:17. doi: 10.1186/s13049-015-0091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Brett S., Waheed U. Pain control in the intensive care unit. In: Vincent J.L., editor. Intensive Care Medicine. Springer New York; New York, NY: 2003. pp. 348–354. [DOI] [Google Scholar]
- 257.Zohar Z., Eitan A., Halperin P. Pain relief in major trauma patients: an Israeli perspective. J Trauma. 2001;51:767–772. doi: 10.1097/00005373-200110000-00024. [DOI] [PubMed] [Google Scholar]
- 258.Cohen S.P., Christo P.J., Moroz L. Pain management in trauma patients. Am J Phys Med Rehabil. 2004;83:142–161. doi: 10.1097/01.PHM.0000107499.24698. CA. [DOI] [PubMed] [Google Scholar]
- 259.Peek J., Beks R.B., Kingma B.F. Epidural analgesia for severe chest trauma: an analysis of current practice on the efficacy and safety. Crit Care Res Pract. 2019;2019:4837591. doi: 10.1155/2019/4837591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Gage A., Rivara F., Wang J. The effect of epidural placement in patients after blunt thoracic trauma. J Trauma Acute Care Surg. 2014;76:39–46. doi: 10.1097/TA.0b013e3182ab1b08. [DOI] [PubMed] [Google Scholar]
- 261.Ahmadi A., Bazargan-Hejazi S., Heidari Zadie Z. Pain management in trauma: a review study. J Inj Violence Res. 2016;8:89–98. doi: 10.5249/jivr.v8i2.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Bulger E.M., Arneson M.A., Mock C.N. Rib fractures in the elderly. J Trauma. 2000;48:1040–1047. doi: 10.1097/00005373-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 263.Kourouche S., Buckley T., Munroe B. Development of a blunt chest injury care bundle: an integrative review. Injury. 2018;49:1008–1023. doi: 10.1016/j.injury.2018.03.037. [DOI] [PubMed] [Google Scholar]
- 264.Malekpour M., Hashmi A., Dove J. Analgesic choice in management of rib fractures: paravertebral block or epidural analgesia? Anesth Analg. 2017;124:1906–1911. doi: 10.1213/ANE.0000000000002113. [DOI] [PubMed] [Google Scholar]
- 265.Galvagno S.M., Smith C.E., Varon A.J. Pain management for blunt thoracic trauma: a joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016;81:936–951. doi: 10.1097/TA.0000000000001209. [DOI] [PubMed] [Google Scholar]
- 266.Berben S.A., Meijs T.H., van Dongen R.T. Pain prevalence and pain relief in trauma patients in the Accident & Emergency department. Injury. 2008;39:578–585. doi: 10.1016/j.injury.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 267.Carrie C., Stecken L., Cayrol E. Bundle of care for blunt chest trauma patients improves analgesia but increases rates of intensive care unit admission: a retrospective case-control study. Anaesth Crit Care Pain Med. 2018;37:211–215. doi: 10.1016/j.accpm.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 268.Yeo T.P. Long-term sequelae following blunt thoracic trauma. Orthop Nurs. 2001;20:35–47. doi: 10.1097/00006416-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 269.Devji T., Hussain F.N., Bhandari M. The impact of trauma on society. In: Pape H.C., Sanders R., Borrelli J., editors. The Poly-Traumatized Patient with Fractures. Springer Berlin Heidelberg; Berlin, Heidelberg: 2016. pp. 1–7. [DOI] [Google Scholar]
- 270.Carrie C., Guemmar Y., Cottenceau V. Long-term disability after blunt chest trauma: don't miss chronic neuropathic pain! Injury. 2019;50:113–118. doi: 10.1016/j.injury.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 271.Senn-Reeves J.N., Staffileno B.A. Long-term outcomes after blunt injury to the boney thorax: an integrative literature review. J Trauma Nurs. 2013;20:56–66. doi: 10.1097/JTN.0b013e318286629b. [DOI] [PubMed] [Google Scholar]
- 272.Savetamal A., Livingston D.H. Thoracic wall injuries: ribs, sternal scapular fractures, hemothoraces, and pneumothoraces. In: Asensio J.A., Trunkey D.D., editors. Current Therapy of Trauma and Surgical Critical Care. Elsevier; 2008. pp. 252–261. [DOI] [Google Scholar]