This cohort study compares overall life expectancy and comorbidity-free life expectancy by HIV status for insured adults with and without HIV infection from 2000 to 2016 in the US.
Key Points
Question
Is antiretroviral therapy associated with improved survival among individuals with HIV infection?
Findings
In this cohort study of 39 000 adults with HIV infection and 387 785 adults without HIV infection in the US, individuals with HIV infection lived 6.8 fewer years overall and 9.5 fewer years without major chronic comorbidities, even after initiation of antiretroviral therapy at high CD4 cell counts.
Meaning
The results suggest that life expectancy of adults with HIV infection may be near that of life expectancy of individuals without HIV infection, but greater attention is needed to prevention of comorbidities among individuals with HIV infection.
Abstract
Importance
Antiretroviral therapy (ART) has improved life expectancy for individuals with HIV infection, but recent data comparing life span and comorbidity-free years by HIV status are lacking.
Objective
To quantify the gap in life span and comorbidity-free years by HIV status among adults with access to care.
Design, Setting, and Participants
This matched cohort study used data from insured adults with and without HIV infection (aged ≥21 years) matched 1:10 at medical centers of Kaiser Permanente in northern and southern California and the mid-Atlantic states of Washington DC, Maryland, and Virginia from January 1, 2000, through December 31, 2016. Data were analyzed from September 1, 2019, through March 31, 2020.
Exposures
HIV status and, for individuals with HIV infection, ART initiation at a CD4 cell count of 500/μL or greater.
Main Outcomes and Measures
Overall life expectancy and expected years free of major chronic comorbidities, including chronic liver disease, chronic kidney disease, chronic lung disease, diabetes, cancer, and cardiovascular disease.
Results
Of 39 000 individuals with HIV infection and 387 785 matched uninfected adults, 374 421 (87.7%) were male, with a mean (SD) age of 41.4 (10.8) years. Among 359 244 individuals with known race/ethnicity, 90 177 (25.1%) were non-Hispanic black and 87 191 (24.3%) were Hispanic. From 2000 to 2003, overall life expectancy at age 21 years of age was 37.6 years among individuals with HIV infection and 59.7 years among uninfected adults, (difference, 22.1 years; 95% CI, 20.2-24.0 years). From 2014 to 2016, overall life expectancy at 21 years of age among individuals with HIV infection increased to 56.0 years compared with 65.1 years among uninfected adults (difference, 9.1 years; 95% CI, 7.9-10.2 years). During 2011 to 2016, individuals with HIV infection who initiated ART with a CD4 cell count of 500/μL or greater had a life expectancy at 21 years of age of 57.4 years compared with 64.2 years among uninfected adults (difference, 6.8 years; 95% CI, 5.0-8.5 years). From 2000 to 2003, the expected number of comorbidity-free years remaining at 21 years of age was 11.3 for individuals with HIV infection and 26.6 years for uninfected adults (difference, 15.3 years; 95% CI, 13.9-16.6 years). This difference in comorbidity-free years persisted over time but decreased to 9.5 years (95% CI, 7.7-11.2 years) for individuals with HIV infection who initiated ART at a CD4 cell count of 500/μL or greater.
Conclusions and Relevance
The results suggest that life expectancy of adults with HIV infection may be near that of life expectancy of individuals without HIV infection, but greater attention is needed to prevention of comorbidities among individuals with HIV infection.
Introduction
Combination antiretroviral therapy (ART) has markedly increased life expectancy for individuals with HIV infection in high-income countries,1,2,3,4,5,6 but recent data comparing life span by HIV status are lacking. In a study of life expectancy among individuals with HIV infection and uninfected adults in a large health care system in California, an 8-year difference was found from 2008 to 2011, even with ART initiation at high CD4 cell counts.7 The difference in survival by HIV status may have narrowed in more recent years, but few studies8 have included data after 2011. Moreover, despite many studies9 documenting an excess risk of major chronic comorbidities among individuals with HIV infection, such as cancer10 and cardiovascular disease,11 few have compared the number of healthy life years by HIV status. One study12 found that individuals with HIV infection in Canada lived substantially fewer comorbidity-free years compared with the general population from 1996 to 2012, but the study did not examine trends over time or whether ART initiation at high CD4 cell counts was associated with more healthy years.
Our objective was to quantify the difference in overall life span and comorbidity-free years by HIV status among adults with access to care in the US. We estimated overall and comorbidity-free life expectancy in a large cohort of individuals with HIV infection and demographically similar uninfected adults from the same health care system from 2000 to 2016, focusing on 6 chronic comorbidities. For the most recent years, we assessed whether initiation of ART at high CD4 cell counts was associated with a decrease in the difference of overall or comorbidity-free life expectancy by HIV status.
Methods
Study Setting, Population, and Design
We conducted a matched cohort study of members from Kaiser Permanente in northern California (KPNC) and southern California (KPSC) and the Kaiser Permanente mid-Atlantic states (KPMAS) of Maryland, Virginia, and Washington, DC. These are large integrated health care systems that provide comprehensive medical services to a total of 9.5 million members. The institutional review board at KPMAS approved this study with a waiver of informed consent because the study presented no more than minimal risk and it was not feasible to contact all participants. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.13
Eligible individuals included adults (aged ≥21 years) with and without HIV infection who were members of KPNC, KPSC, or KPMAS at any time from January 1, 2000, to December 31, 2016. HIV status was determined by using HIV registries that included all known cases of HIV infection and AIDS since the early 1980s for KPNC, since 2000 for KPSC, and since 2004 for KPMAS. Individuals not included in the HIV registries were considered to be uninfected. We frequency matched individuals with HIV infection 1:10 to uninfected adults based on age (2-year groups), sex, race/ethnicity, medical center, and calendar year at the start of follow-up, with random selection from the uninfected subgroups defined by each matching factor. The start of follow-up for each person was the earliest date on or after January 1, 2000, when eligibility criteria were met, and individuals were followed until death, health plan disenrollment, or December 31, 2016, whichever occurred first.
Study Measurements
Demographic and Clinical Characteristics
We extracted demographic and clinical data from Kaiser Permanente’s electronic health records, including age at the start of follow-up, sex, self-reported race/ethnicity, neighborhood-level measures of socioeconomic status, CD4 cell count at ART initiation, and overweight or obesity (ie, body mass index >25 [calculated as weight in kilograms divided by height in meters squared]) at any time through the end of follow-up. Substance use variables for descriptive analyses included history of alcohol use disorders, history of drug use disorders, and smoking or tobacco use ever through the end of follow-up. International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision diagnosis codes are provided in the eTable 1 in the Supplement. We used internal HIV registries to obtain data on HIV-transmission risk group (ie, men who have sex with men, heterosexual sex, injection drug use, or other), dates of first ART use, and beginning of known HIV infection.
Comorbidities and Mortality
Analyses of incident comorbidities focused on 6 major chronic conditions: chronic liver disease, chronic kidney disease, chronic lung disease, diabetes, cancer, and cardiovascular disease. We identified comorbidities based on diagnosis, laboratory, or registry data (eTable 1 in the Supplement). In brief, we defined chronic liver disease, chronic lung disease, and cardiovascular disease by inpatient or outpatient diagnoses. We defined chronic kidney disease by at least 2 measures of estimated glomerular filtration rate less than 60 mL/min at least 90 days apart, with the diagnosis date assigned to the first of the 2 laboratory results. We defined diabetes by at least 2 inpatient or outpatient diagnoses or at least 1 prescription indicative of diabetes, excluding possible gestational diabetes and women receiving metformin or thiazolidinedione without other indications of diabetes. We defined cancer as any invasive cancer recorded in internal cancer registries.
We obtained dates of death from electronic health records, state death certificates, and Social Security Administration data sets.
Statistical Analysis
Data analysis was performed from September 1, 2019, through March 31, 2020. We first estimated the incidence of mortality, any comorbidity, and each individual comorbidity among individuals with HIV infection and uninfected adults. When estimating rates of incident comorbidities, we excluded individuals with a history of the comorbidity documented at KPNC, KPSC, or KPMAS in the 2 years before baseline and focused on the first incident comorbidity, whereas mortality analyses included all members of the cohort. We computed crude mortality and comorbidity rates per 100 person-years and 95% CIs.
We then used abridged life tables to estimate the mean number of total and comorbidity-free years of life remaining at 21 years of age for individuals with HIV infection and uninfected adults. We constructed life tables based on standard methods, as previously described.1,14,15,16 In brief, we constructed life tables from age-specific mortality rates for individuals with HIV infection and uninfected adults using 5-year age intervals starting from 21 years, with a final open interval for 81 years or older. For intervals with small sample size (either no deaths or less than 100 person-years in the age interval), we estimated the age-specific mortality rate with the assumption that the rate ratio comparing individuals with HIV infection with uninfected adults was the same as the mean of the rate ratios comparing individuals with HIV infection with uninfected adults in the previous 2 age groups.1 These life tables described the experience that hypothetical cohorts of individuals with HIV infection and uninfected adults would have had if they had the observed age-specific mortality rates from 21 years of age until death. Using variance and SE formulas provided by Chiang,14 we generated 95% CIs for life expectancy estimates (estimate: –1.96 × SE to 1.96 × SE) and differences in life expectancy by HIV status (difference: –1.96 × √[sum of variances] to 1.96 × √[sum of variances]).
Using this life-table approach, we first estimated the overall life expectancy at 21 years of age for individuals with HIV infection and uninfected adults within calendar eras (ie, 2000-2003, 2004-2007, 2008-2010, 2011-2013, and 2014-2016). We then estimated the expected number of comorbidity-free years remaining (ie, comorbidity-free life expectancy) at 21 years of age for individuals with HIV infection and uninfected adults within each calendar era.16 We defined comorbidity-free years as those lived before incident diagnosis of a comorbidity of interest. We estimated comorbidity-free life expectancy for all 6 comorbidities combined and for each comorbidity separately. Finally, we focused on the most recent broad calendar era (2011-2016), which provided a sufficient sample size for estimation of overall and comorbidity-free life expectancy in subgroups defined by CD4 cell count at ART initiation (ie, ≥500/μL and ≥350/μL) and by sex. We conducted analyses in SAS, version 9.4 (SAS Institute Inc) and Microsoft Excel 2016 (Microsoft Corporation).
Results
Study Population
Among 39 000 individuals with HIV infection and 387 785 matched uninfected adults, the mean (SD) age was 41.4 (10.8) years and 374 421 (87.7%) were male (Table 1). Of 359 244 individuals with known race/ethnicity, 90 177 (25.1%) were non-Hispanic black and 87 191 (24.3%) were Hispanic. Of those with known neighborhood-level socioeconomic status, a higher proportion of individuals with HIV infection than uninfected adults lived in neighborhoods with a median annual household income less than $35 000 US dollars (4225 of 29 064 [14.5%] vs 32 980 of 317 301 [10.4%]). Compared with uninfected adults, a higher proportion of individuals with HIV infection had a history of drug use disorders (1740 of 39 000 [4.5%] vs 9208 of 387 767 [2.4%]). Among those with known smoking status and body mass index, a higher proportion of individuals with HIV infection than uninfected adults ever smoked (15 595 of 30 092 [51.8%] vs 116 745 of 286 311 [40.8%]) and a lower proportion were ever overweight or obese (21 028 of 28 727 [73.2%] vs 236 096 of 276 179 [85.5%]).
Table 1. Baseline Characteristics of Individuals With and Without HIV Infection, Kaiser Permanente, 2000-2016a.
| Characteristic | Individuals, No. (%) | |
|---|---|---|
| With HIV infection (n = 39 000) | Without HIV infection (n = 387 767) | |
| Person-years, mean (SD), per person | 5.2 (5.2) | 6.0 (5.4) |
| Reason for end of follow-up | ||
| Health plan disenrollment | 21 608 (55.4) | 207 042 (53.4) |
| End of study period | 14 731 (37.8) | 171 578 (44.3) |
| Death | 2661 (6.8) | 9147 (2.4) |
| Age at baseline, mean (SD), y | 41.4 (10.8) | 41.4 (10.8) |
| Male | 34 236 (87.8) | 340 185 (87.7) |
| Race/ethnicity, No./total No. (%) | ||
| Non-Hispanic white | 14 844/32 988 (45.0) | 147 062/326 256 (45.1) |
| Non-Hispanic black | 8208/32 988 (24.9) | 81 969/326 256 (25.1) |
| Hispanic | 7948/32 988 (24.1) | 79 243/326 256 (24.3) |
| Asian | 1509/32 988 (4.6) | 15 011/326 256 (4.6) |
| Other | 479/32 988 (1.5) | 2971/326 256 (0.9) |
| Neighborhood-level socioeconomic status, No./total No. (%) | ||
| >25% Without a high school education | 7181/29 079 (24.7) | 76 794/317 421 (24.2) |
| Median annual household income <$35 000 | 4225/29 064 (14.5) | 32 980/317 301 (10.4) |
| History of alcohol use disorder | 1368 (3.5) | 12 605 (3.3) |
| History of drug use disorder | 1740 (4.5) | 9208 (2.4) |
| Ever smoking, No./total No. (%) | 15 595/30 092 (51.8) | 116 745/286 311 (40.8) |
| Ever overweight or obese, No./total No. (%) | 21 028/28 727 (73.2) | 236 096/276 179 (85.5) |
| HIV-transmission risk group, No./total No. (%) | ||
| Men who have sex with men | 20 779/29 827 (69.7) | NA |
| Heterosexual sex | 6013/29 827 (20.2) | NA |
| Injection drug use | 2511/29 827 (8.4) | NA |
| Other | 524/29 827 (1.8) | NA |
| Year diagnosed with HIV infection | ||
| Before 1990 | 3271 (8.4) | NA |
| 1990-1999 | 9121 (23.4) | NA |
| 2000-2009 | 16 833 (43.2) | NA |
| 2010 or after | 9775 (25.1) | NA |
| Previous antiretroviral medication use | 7022 (18.0) | NA |
| Initiated antiretroviral therapy during follow-up | 24 880 (63.8) | NA |
| CD4 cell count at antiretroviral therapy initiation, No./total No. (%) | ||
| <200/μL | 7681/27 037 (28.4) | NA |
| 200-349/μL | 6367/27 037 (23.6) | NA |
| 350-499/μL | 5110/27 037 (18.9) | NA |
| ≥500/μL | 7879/27 037 (29.1) | NA |
Abbreviation: NA, not available.
Individuals with HIV infection and uninfected adults were matched based on age (2-year age groups), sex, race/ethnicity, medical center, and initial calendar year of follow-up. Some data were missing on race/ethnicity (15.4% of individuals with HIV infection and 15.9% of uninfected adults), socioeconomic status (25.5% of individuals with HIV infection and 18.2% of uninfected adults), smoking status (22.8% of individuals with HIV infection and 26.2% of uninfected adults), HIV-transmission risk group (23.5% of individuals with HIV infection), and CD4 cell count at antiretroviral therapy initiation (of 15.2% of individuals with HIV infection).
Among individuals with HIV infection with a known HIV-transmission risk group, 20 779 of 29 827 (69.7%) were men who have sex with men. Nearly one-third (12 392 of 39 000 [31.8%]) received a diagnosis of HIV infection before 2000. Of the 31 902 (81.8%) who initiated ART by the end of follow-up, 27 037 (84.8%) had a CD4 cell count measured at the time of ART initiation, of whom 7879 (29.1%) had a CD4 count of 500/μL or greater.
Mortality and Incidence of Comorbidities
Among individuals with HIV infection, there were 2661 deaths, with a mortality rate of 1.3 per 100 person-years (95% CI, 1.3-1.4 per person-years); there were 9147 deaths among uninfected adults, with a mortality rate of 0.4 per 100 person-years (95% CI, 0.4-0.4 per 100 person-years) (Table 2). There were 11 366 individuals with HIV infection and 60 707 uninfected adults with at least 1 of 6 incident comorbidities, with rates of any comorbidity for individuals with HIV infection of 10.0 per person-years (95% CI, 9.8-10.2 person-years) and for uninfected adults of 3.8 per 100 person-years (95% CI, 3.7-3.8 per 100 person-years). When examined individually, crude incidence rates were higher for all comorbidities among individuals with HIV infection compared with uninfected adults. For individuals with HIV infection, incidence rates of comorbidities ranged from 0.4 per 100 person-years (95% CI, 0.4-0.4 per person-years) for cardiovascular disease to 3.5 per 100 person-years (95% CI, 3.4-3.6 per 100 person-years) for chronic lung disease.
Table 2. Mortality and Incidence of Common Comorbidities Among Individuals With and Without HIV Infection, Kaiser Permanente, 2000-2016.
| Outcome | Individuals with HIV infection | Individuals without HIV infection | ||
|---|---|---|---|---|
| Events | Incidence, per 100 person-years (95% CI) | Events | Incidence, per 100 person-years (95% CI) | |
| Mortality | 2661 | 1.3 (1.3-1.4) | 9147 | 0.4 (0.4-0.4) |
| Any comorbidity | 11 366 | 10.0 (9.8-10.2) | 60 707 | 3.8 (3.7-3.8) |
| Chronic disease | ||||
| Liver | 4768 | 2.7 (2.6-2.8) | 10 569 | 0.5 (0.5-0.5) |
| Kidney | 3146 | 1.7 (1.6-1.8) | 10 257 | 0.5 (0.4-0.5) |
| Lung | 5457 | 3.5 (3.4-3.6) | 35 776 | 1.9 (1.9-1.9) |
| Diabetes | 2456 | 1.3 (1.3-1.4) | 21 339 | 1.0 (1.0-1.0) |
| Cancer | 1922 | 1.0 (1.0-1.0) | 10 619 | 0.5 (0.5-0.5) |
| Cardiovascular disease | 813 | 0.4 (0.4-0.4) | 6296 | 0.3 (0.3-0.3) |
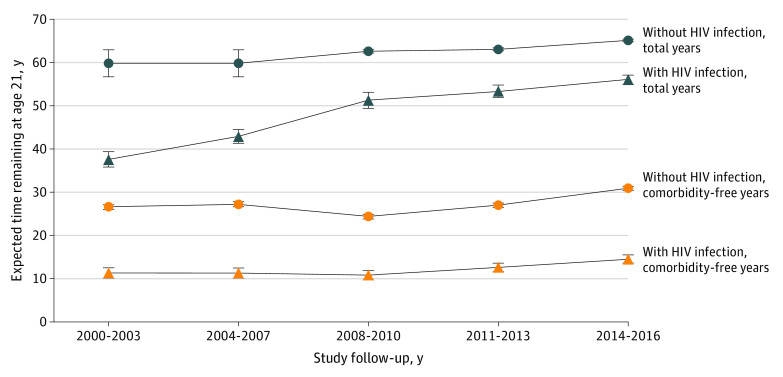
Overall and Comorbidity-Free Life Expectancy
Overall and comorbidity-free life expectancy at 21 years of age for individuals with HIV infection and uninfected adults is shown in Figure 1. From 2000 to 2003, overall life expectancy at 21 years of age was 37.6 for individuals with HIV infection and 59.7 years for uninfected adults (difference, 22.1 years; 95% CI, 20.2-24.0 years). From 2014 to 2016, overall life expectancy at 21 years of age increased to 56.0 years for individuals with HIV infection and to 65.1 years for uninfected adults (difference, 9.1 years; 95% CI, 7.9-10.2 years). From 2011 to 2016, overall life expectancy at 21 years of age for individuals with HIV infection who initiated ART at a CD4 cell count of 500/μL or greater was 57.4 years (95% CI, 55.7-59.1 years) and for uninfected adults was 64.2 years (95% CI, 64.0-64.4 years), corresponding to a difference of 6.8 years (95% CI, 5.0-8.5 years) (Table 3).
Figure 1. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Individuals With and Without HIV Infection, Kaiser Permanente, 2000-2016.
Comorbidity-free years were those lived before incident diagnosis of any of 6 common comorbidities: chronic liver disease, chronic kidney disease, chronic lung disease, diabetes, cancer, or cardiovascular disease. Error bars indicate 95% CIs.
Table 3. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Individuals With and Without HIV Infection and for Individuals With HIV Infection Who Initiated ART at High CD4 Cell Counts, Kaiser Permanente, 2011-2016.
| Outcome | Life expectancy at age 21 y, No. of y (95% CI) | ||||||
|---|---|---|---|---|---|---|---|
| Individuals with HIV infection | Individuals with HIV infection with CD4 cell count ≥500/μL at ART initiation | Individuals without HIV infection | Difference | ||||
| Individuals with HIV infection vs individuals without HIV infection | Individuals with HIV infection with CD4 cell count ≥500/μL at ART initiation vs Individuals without HIV infection | ||||||
| Overall | 54.9 (54.0 to 55.9) | 57.4 (55.7 to 59.1) | 64.2 (64.0 to 64.4) | 9.2 (8.3 to 10.2) | 6.8 (5.0 to 8.5) | ||
| Comorbidity freea | 13.7 (13.0 to 14.4) | 19.5 (17.8 to 21.2) | 29.0 (28.6 to 29.3) | 15.3 (14.5 to 16.1) | 9.5 (7.7 to 11.2) | ||
| Chronic disease | |||||||
| Liver | 33.1 (31.9 to 34.2) | 42.5 (39.8 to 45.1) | 57.6 (57.3 to 57.9) | 24.5 (23.3 to 25.7) | 15.1 (12.5 to 17.8) | ||
| Kidney | 40.2 (39.5 to 41.0) | 42.5 (40.8 to 44.2) | 56.3 (56.0 to 56.5) | 16.1 (15.3 to 16.9) | 13.8 (12.0 to 15.5) | ||
| Lung | 23.4 (22.3 to 24.6) | 31.3 (28.5 to 34.1) | 38.5 (38.0 to 38.9) | 15.0 (13.7 to 16.3) | 7.2 (4.3 to 10.0) | ||
| Diabetes | 44.2 (43.2 to 45.3) | 50.2 (47.9 to 52.4) | 51.7 (51.3 to 52.0) | 7.4 (6.4 to 8.5) | 1.5 (−0.8 to 3.8) | ||
| Cancer | 48.1 (47.0 to 49.1) | 52.6 (50.3 to 54.8) | 58.0 (57.7 to 58.2) | 9.9 (8.8 to 11.0) | 5.4 (3.1 to 7.7) | ||
| Cardiovascular disease | 51.8 (50.9 to 52.7) | 56.4 (54.3 to 58.5) | 60.8 (60.5 to 61.0) | 9.0 (8.0 to 9.9) | 4.4 (2.2 to 6.5) | ||
Abbreviation: ART, antiretroviral therapy.
Comorbidity-free years were those lived before incident diagnosis of any of the 6 common comorbidities.
From 2000 to 2003, the expected number of comorbidity-free years remaining at 21 years of age was 11.3 years for individuals with HIV infection and 26.6 years for uninfected adults, corresponding to a difference of 15.3 years (95% CI, 13.9-16.6 years) (Figure 1). This difference persisted from 2014 to 2016, with a comorbidity-free life expectancy at 21 years of age of 14.5 years for individuals with HIV infection and 30.9 years for uninfected adults, corresponding to a difference of 16.3 years (95% CI, 15.3-17.4 years). From 2011 to 2016, comorbidity-free life expectancy at 21 years of age was 19.5 years for individuals with HIV infection who initiated ART at a CD4 cell count of 500/μL or greater and 29.0 years for uninfected adults, corresponding to a difference of 9.5 years (95% CI, 7.7-11.2 years) (Table 3).
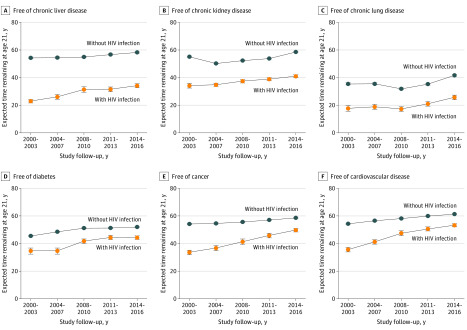
When examining each comorbidity separately, there was a persistent difference in comorbidity-free life expectancy at 21 years of age between individuals with HIV infection and uninfected adults across all calendar eras, although the gap narrowed over time for several comorbidities, most notably diabetes, cancer, and cardiovascular disease (Figure 2). From 2011 to 2016, the difference in comorbidity-free life expectancy at 21 years of age between individuals with HIV infection and uninfected adults ranged from 7.4 years (95% CI, 6.4-8.5 years) for diabetes to 24.5 years (95% CI, 23.3-25.7 years) for chronic liver disease (Table 3).
Figure 2. Comorbidity-Free Life Expectancy at Age 21 Years for Individuals With and Without HIV Infection Stratified by Comorbidity, Kaiser Permanente, 2000-2016.
Error bars indicate 95% CIs.
When restricting the analysis to individuals with HIV infection who initiated ART at a CD4 cell count of 500/μL or greater, the difference in comorbidity-free life expectancy between individuals with HIV infection and uninfected adults decreased for each comorbidity from 2011 to 2016, with no remaining difference for diabetes (Table 3). Results were similar when the analysis was restricted to individuals with HIV infection who initiated ART at a CD4 cell count ≥350/μL (eTable 2 in the Supplement).
Differences were found in overall and comorbidity-free life expectancy by sex from 2011 to 2016. Compared with men, women had a greater difference in overall life expectancy by HIV status compared with men (12.1 years [95% CI, 10.0-14.3 years] vs 9.0 years [95% CI, 8.0-10.0 years]) but a smaller difference in years free of any comorbidity (12.7 years [95% CI, 10.4-15.1 years] vs 15.6 years [95% CI, 14.8-16.5 years]), with variation across individual comorbidities (eTable 3 in the Supplement).
Discussion
In this large cohort of individuals with HIV infection and matched uninfected adults with access to health care in the US, we found a 9.1-year difference in overall life expectancy from 2011 to 2016, and the difference was smaller (6.8 years) for individuals with HIV infection who initiated ART at high CD4 cell counts. We found a large and persistent difference in comorbidity-free years, with individuals with HIV infection living 16.3 fewer healthy years than uninfected adults. For individuals with HIV infection who initiated ART at high CD4 cell counts, this difference was smaller at 9.5 years, with improvements across all comorbidities. Our results suggest that individuals with HIV infection who initiate ART at high CD4 cell counts may reach a similar life span as uninfected adults, but greater attention may be needed to prevention of comorbidities among individuals with HIV infection.
Similar to previous findings from a cohort of KPNC and KPSC members through 2011,7 a remaining disparity in life expectancy by HIV status from 2011 to 2016 was found, even for individuals with HIV infection who initiated ART at high CD4 cell counts. The most recent data on life expectancy for individuals with HIV infection come from the Swiss HIV Cohort Study,8 which found that life expectancy for individuals with HIV infection in Switzerland was 55 years overall from 2006 to 2013 compared with 63 years for a matched random sample of the general population.8 However, in contrast to our findings, life expectancy at 21 years of age was 64 years for individuals with HIV infection who presented at enrollment with CD4 cell counts ≥350/μL, with no remaining difference compared with the general population. Results may differ between the Swiss HIV Cohort Study8 and our study because of differences in access to health care, selection of uninfected comparison groups, and risk factors for mortality across study settings.
Although overall life span has lengthened for individuals with HIV infection, we found a large difference in comorbidity-free life expectancy by HIV status, with no change in this difference over time. Consistent with our results, Hogg et al12 estimated health-adjusted (ie, comorbidity-free) life expectancy at 20 years of age among individuals with HIV infection in Canada, finding that individuals with HIV infection lived approximately 30 fewer years free of cardiovascular, respiratory, liver, and renal diseases, as well as non–AIDS-defining cancers compared with the general population from 1996 to 2012.12 Our study extends this work by examining changes in comorbidity-free life expectancy over time, finding that the difference by HIV status decreased for several comorbidities, particularly diabetes, cancer, and cardiovascular disease. The positive changes we observed for these comorbidities among individuals with HIV infection may be associated with frequent health care visits, which can facilitate access to preventive care, such as cancer screening and smoking cessation programs. Reduced rates of cancer and cardiovascular disease may also be associated with improvements in the tolerability and ease of ART administration,17 with both of these comorbidities associated with immunosuppression among patients with HIV infection.10,18
Our findings suggest that ART initiation at high CD4 cell counts is associated with a longer life span and more comorbidity-free years for individuals with HIV infection, consistent with previous work.1,2,4,7,19 The Strategic Timing of Antiretroviral Treatment trial20 found lower rates of serious AIDS-related and non-AIDS–related events among individuals with HIV infection starting ART with CD4 cell counts of 500/μL or greater compared with deferral until CD4 cell counts decreased below 350/μL.20 In contrast, we observed similar overall life expectancy and comorbidity-free years for individuals with HIV infection who initiated ART with CD4 cell counts ≥500 cells/μL and those who initiated ART with CD4 cell counts ≥350 cells/μL. Nevertheless, our results suggest that, in addition to being associated with increasing overall life span, continued widespread implementation of guidelines supporting ART initiation regardless of CD4 cell count21,22 may be associated with an increased number of comorbidity-free years among individuals with HIV infection, potentially through reduced inflammation or immune activation.23,24
Strengths and Limitations
This study has strengths. First, we used a large, well-characterized cohort of individuals with HIV infection and matched uninfected adults from the same health care system, thus minimizing the selection bias that can be introduced by comparisons to the general population. Moreover, because members had comprehensive medical insurance coverage regardless of public or private plans, differences in morbidity or mortality were unlikely to be attributable to differential access to care. Second, internal HIV registries allowed for high-quality ascertainment of diagnosed HIV infection. In addition, our membership mirrors the age, sex, and race/ethnicity distributions of the surrounding population,25,26 suggesting that our results may be generalizable to other individuals with access to health care.
This study has limitations. First, there may have been some misclassification in our data. For example, misclassification of individuals with undiagnosed HIV infection as uninfected may have resulted in underestimated life expectancies for uninfected adults. However, we expect this to have had a negligible effect on our results given the low prevalence of HIV infection (0.12%) among Kaiser Permanente members.27 Second, rates of comorbidities may have been higher among individuals with HIV infection in part because of increased screening. However, similar use of preventive care, specifically cancer screening, by HIV status in this study population has previously been reported.28,29 Furthermore, even if associated with screening, our results suggest that individuals with HIV infection are living more years with diagnosed comorbidities that require clinical management, with potentially reduced quality of life.
Third, our study was subject to the life-table assumption that age-specific mortality rates are similar across birth cohorts. There was likely some violation of this assumption, possibly resulting in underestimated life expectancies for individuals with HIV infection because younger birth cohorts have experienced greater benefits from recent advances in ART. However, this underestimation may have been minimized by the relative homogeneity of the cohort with respect to birth years (ie, half were born during 1956-1972). Fourth, those who were lost to follow-up may have differed by HIV status (ie, dependent censoring), potentially introducing bias in estimates of mortality or comorbidity rates. Fifth, most individuals with HIV infection and matched uninfected adults were men, reflecting the HIV epidemic in our study settings and potentially limiting generalizability of our results to women.
Conclusions
The results suggest that life expectancy of adults with HIV infection may be near that of life expectancy of individuals without HIV infection, but greater attention is needed to prevention of comorbidities among individuals with HIV infection.
eTable 1. Definitions of Major Chronic Comorbidities and Substance Use Variables
eTable 2. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Individuals With and Without HIV Infection, and for Individuals With HIV Infection Who Initiated ART With CD4 ≥350 Cells/μL, Kaiser Permanente, 2011-2016
eTable 3. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Women and Men With and Without HIV Infection, Kaiser Permanente, 2011-2016
References
- 1.Antiretroviral Therapy Cohort Collaboration . Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293-299. doi: 10.1016/S0140-6736(08)61113-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samji H, Cescon A, Hogg RS, et al. ; North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of IeDEA . Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One. 2013;8(12):e81355. doi: 10.1371/journal.pone.0081355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lohse N, Hansen A-BE, Pedersen G, et al. Survival of persons with and without HIV infection in Denmark, 1995-2005. Ann Intern Med. 2007;146(2):87-95. doi: 10.7326/0003-4819-146-2-200701160-00003 [DOI] [PubMed] [Google Scholar]
- 4.Patterson S, Cescon A, Samji H, et al. ; CANOC collaboration . Life expectancy of HIV-positive individuals on combination antiretroviral therapy in Canada. BMC Infect Dis. 2015;15:274. doi: 10.1186/s12879-015-0969-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrison KM, Song R, Zhang X. Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States. J Acquir Immune Defic Syndr. 2010;53(1):124-130. doi: 10.1097/QAI.0b013e3181b563e7 [DOI] [PubMed] [Google Scholar]
- 6.Wada N, Jacobson LP, Cohen M, French A, Phair J, Muñoz A. Cause-specific life expectancies after 35 years of age for human immunodeficiency syndrome-infected and human immunodeficiency syndrome-negative individuals followed simultaneously in long-term cohort studies, 1984-2008. Am J Epidemiol. 2013;177(2):116-125. doi: 10.1093/aje/kws321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcus JL, Chao CR, Leyden WA, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. J Acquir Immune Defic Syndr. 2016;73(1):39-46. doi: 10.1097/QAI.0000000000001014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gueler A, Moser A, Calmy A, et al. ; Swiss HIV Cohort Study, Swiss National Cohort . Life expectancy in HIV-positive persons in Switzerland: matched comparison with general population. AIDS. 2017;31(3):427-436. doi: 10.1097/QAD.0000000000001335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lerner AM, Eisinger RW, Fauci AS. Comorbidities in persons with HIV: the lingering challenge. JAMA. Published online December 11, 2019. [DOI] [PubMed] [Google Scholar]
- 10.Silverberg MJ, Chao C, Leyden WA, et al. HIV infection, immunodeficiency, viral replication, and the risk of cancer. Cancer Epidemiol Biomarkers Prev. 2011;20(12):2551-2559. doi: 10.1158/1055-9965.EPI-11-0777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drozd DR, Kitahata MM, Althoff KN, et al. Increased risk of myocardial infarction in HIV-infected individuals in North America compared with the general population. J Acquir Immune Defic Syndr. 2017;75(5):568-576. doi: 10.1097/QAI.0000000000001450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hogg RS, Eyawo O, Collins AB, et al. ; Comparative Outcomes And Service Utilization Trends (COAST) study . Health-adjusted life expectancy in HIV-positive and HIV-negative men and women in British Columbia, Canada: a population-based observational cohort study. Lancet HIV. 2017;4(6):e270-e276. doi: 10.1016/S2352-3018(17)30029-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 14.Chiang CL. The life table and its construction. In: Introduction to Stochastic Processes in Biostatistics. John Wiley and Sons; 1968:189-214. [Google Scholar]
- 15.Arias E, Xu J, Kochanek KD. United States life tables, 2016. Natl Vital Stat Rep. 2019;68(4):1-66. [PubMed] [Google Scholar]
- 16.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86(4):347-354. doi: 10.2307/4594169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein DB, Leyden WA, Xu L, et al. Declining relative risk for myocardial infarction among HIV-positive compared with HIV-negative individuals with access to care. Clin Infect Dis. 2015;60(8):1278-1280. doi: 10.1093/cid/civ014 [DOI] [PubMed] [Google Scholar]
- 18.Silverberg MJ, Leyden WA, Xu L, et al. Immunodeficiency and risk of myocardial infarction among HIV-positive individuals with access to care. J Acquir Immune Defic Syndr. 2014;65(2):160-166. doi: 10.1097/QAI.0000000000000009 [DOI] [PubMed] [Google Scholar]
- 19.May MT, Gompels M, Delpech V, et al. ; UK Collaborative HIV Cohort (UK CHIC) Study . Impact on life expectancy of HIV-1 positive individuals of CD4+ cell count and viral load response to antiretroviral therapy. AIDS. 2014;28(8):1193-1202. doi: 10.1097/QAD.0000000000000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lundgren JD, Babiker AG, Gordin F, et al. ; INSIGHT START Study Group . Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795-807. doi: 10.1056/NEJMoa1506816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services . Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Accessed December 4, 2019. https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-treatment-guidelines/0
- 22.World Health Organization . Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. September 2015. Accessed December 4, 2019. https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_eng.pdf?sequence=1 [PubMed]
- 23.Nou E, Lo J, Grinspoon SK. Inflammation, immune activation, and cardiovascular disease in HIV. AIDS. 2016;30(10):1495-1509. doi: 10.1097/QAD.0000000000001109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141-155. doi: 10.1146/annurev-med-042909-093756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon NP. Similarity of the adult Kaiser Permanente membership in northern California to the insured and general population in northern California: statistics from the 2011 California Health Interview Survey. June 19, 2015. Accessed January 17, 2019. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf
- 26.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37-41. doi: 10.7812/TPP/12-031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satre DD, Parthasarathy S, Altschuler A, Silverberg MJ, Storholm E, Campbell CI. Demographic, insurance, and health characteristics of newly enrolled HIV-positive patients after implementation of the Affordable Care Act in California. Am J Public Health. 2016;106(7):1211-1213. doi: 10.2105/AJPH.2016.303126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marcus JL, Chao CR, Leyden WA, et al. Prostate cancer incidence and prostate-specific antigen testing among HIV-positive and HIV-negative men. J Acquir Immune Defic Syndr. 2014;66(5):495-502. doi: 10.1097/QAI.0000000000000202 [DOI] [PubMed] [Google Scholar]
- 29.Lam JO, Hurley LB, Udaltsova N, et al. Colorectal cancer screening in people with and without HIV in an integrated health care setting. J Acquir Immune Defic Syndr. 2019;81(3):284-291. doi: 10.1097/QAI.0000000000002024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Definitions of Major Chronic Comorbidities and Substance Use Variables
eTable 2. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Individuals With and Without HIV Infection, and for Individuals With HIV Infection Who Initiated ART With CD4 ≥350 Cells/μL, Kaiser Permanente, 2011-2016
eTable 3. Overall and Comorbidity-Free Life Expectancy at Age 21 Years for Women and Men With and Without HIV Infection, Kaiser Permanente, 2011-2016