Abstract
Jonathan Cylus and Peter Smith consider how measurement of wellbeing might be used to set public sector priorities
Consensus is emerging that the narrow metrics of prosperity traditionally used in economic debates, such as per capita gross domestic product (GDP), are not fit for purpose.1 Interest is growing in considering more holistic metrics to monitor societal progress, with several attempts at developing and using alternative indicators.2 Examples include the gross national happiness metrics used in Bhutan and the living standards framework developed by New Zealand’s treasury to monitor societal wellbeing and inform budgetary priorities. Within Europe, Finland prioritised the economy of wellbeing in its 2019 European Union presidency programme.3
There is much interest in policy circles in the concept of wellbeing, but to what end? And what might a so called “economy of wellbeing” mean for the health sector? We review evidence on the measurement and determinants of wellbeing and consider how this might be used to set public sector priorities.
How can we conceptualise wellbeing?
The concept of wellbeing is often used interchangeably with concepts such as happiness or social welfare, although some commentators have explored distinctions between them.4 In practice, a common approach has been to assess an individual’s wellbeing through survey questions about their life satisfaction using simple self-assessment questions such as, “How satisfied are you with your life nowadays?” This question forms the basis for many wellbeing measurement initiatives.
A respondent’s answer to the question depends on numerous observable and unobservable influences and experiences. Country rankings based on individual assessments of life satisfaction in the 2019 World Happiness Report, for example, were heavily influenced by factors such as income, social support, and health, with a substantial residual not explained by any measured factors.5 Furthermore, responses are likely to be conditioned by the expectations of the respondent.
Given the inherently complex and vague nature of life satisfaction as a concept, efforts have been made to develop measurement frameworks that rely on more objective factors that may contribute to wellbeing. An early example was the human development index, which incorporates health, education, and income into a single composite metric.6 More recently, the better life initiative of the Organisation for Economic Cooperation and Development (OECD) captures data on topics such as housing, income, jobs, work-life balance, and life satisfaction, and allows analysts to create composite measures of wellbeing by attaching their own relative weights to the metrics.7 This flexibility is likely to be important for securing local acceptance of the wellbeing approach. More localised approaches include the guidance on measuring the impact of social enterprises on wellbeing from the UK’s New Economics Foundation think tank.8
Implications for public priority setting
The principle underlying the wellbeing approach for government is that priorities for public spending should be guided by the extent to which a programme can improve population wellbeing (given its expenditure requirements). In most countries, governments are organised into specific ministerial sectors, each with their own distinct objectives and performance metrics. The diversity across sectors makes comparison of the societal contributions made by different sectors almost impossible and the task of allocating resources between sectors somewhat arbitrary and unsystematic. The dominant analytic approach to valuing additional spending in the health sector has taken the form of incremental cost effectiveness analysis, in which the benefits of additional health spending are assessed in terms of health outcomes, often measured in quality adjust life years (QALYs) or their disability adjusted life years counterpart.9 Other sectors use metrics specific to their own aims, which can rarely be compared directly with the health metric.
For example, how can a finance minister compare, say, the value of additional QALYs produced by the health sector with an improvement in results produced by the education sector in the form of improved PISA scores (the standardised metrics for international comparison of school attainment)?10
We could consider creating a single measure capturing wellbeing with which to assess and compare social progress, as well as to allocate resources to different sectors of the economy according to their relative contribution to wellbeing.11 If governments could measure the contribution of each sector to an overarching common concept of wellbeing, it would, in principle, be possible to adopt a better informed and more systematic approach towards allocating resources between sectors. While this approach most obviously applies to centralised systems of government, in which resource allocation decisions are made by a central authority, such as a finance ministry, it can equally be applied to most systems of government in which such resource allocation depends on governmental policy decisions.
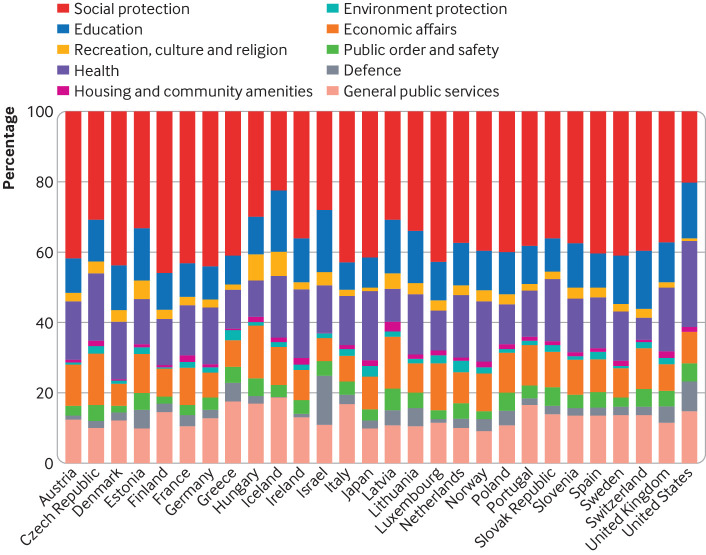
Figure 1 shows the distribution of public sector expenditures in OECD countries in 2017. The health sector varies as a share of public expenditure, from 9% in Latvia to 24% in the United States. With the 2019 World Happiness Report as an example, variations in health explain about 15% of the variations between countries in average happiness, with the largest contributions coming from social support (26%) and income (20%). If priorities were set strictly according to a wellbeing agenda, we might expect some alignment with these determinants.
Fig 1.
How OECD countries allocate their public expenditures (OECD, 2019)12
It is unclear whether a wellbeing approach will—or should—lead to any dramatic shifts in public spending priorities. For one, numerous public expenditure items do not seem to feature in an empirical study of what drives life satisfaction but are essential to a functioning society. For example, provision of safe water is unlikely to be a strong predictor of reported wellbeing in a high income country where there is virtually no variation across the population in access to clean water, and respondents may take its existence for granted. However, this should not imply water and sanitation should receive less funding. Indeed, likely in recognition of this challenge, New Zealand’s wellbeing budget is applied only to spending at the margin, to around 4% of total public expenditure.13
Effect on health systems
The wellbeing agenda has caused a stir within the health policy community. It is argued that, since good health is a key component of wellbeing, a shift in policy attention from traditional economic metrics towards societal wellbeing should translate into increased resources for health systems.2 13 Indeed, within a country, health—especially mental health—accounts for much of the variation in wellbeing.14 The health system in most countries makes a major contribution to health. For example, analysis of the effect of health system spending on health outcomes suggests that the cost per QALY in England is about £13 000 (€15 000; $16 000),15 and analogous estimates are emerging from other high income countries.16 The equivalent costs in low and middle income countries are more difficult to estimate but are likely to be much lower.17 So, the argument goes, health system spending is money well spent. Moreover, there is good evidence that health is a key input to educational attainment, labour market participation, and productivity, strengthening the argument for more health spending to promote wellbeing.18
Yet somewhat paradoxically, the wellbeing agenda could lead to reductions in budget allocations for health systems. It is well understood that health systems are not the only mechanism for improving health. The social determinants of health movement has underlined the importance for health of sectors such as housing, education, environment, employment, and nutrition and given rise to a health in all policies approach to policy making.19 If credible health related policies can be put in place by these sectors, some health related aspects of wellbeing may be more effectively served by spending outside the health system, especially if those policies also contribute to wellbeing in dimensions additional to health. For example, many have argued that spending on education is a powerful mechanism for improving health and reducing health inequalities.20
Is there a case for investing more in the health sector?
Although health is an important component of wellbeing, it does not necessarily mean that the health system itself should be a priority for additional funding. In exploring any claim that the health system has on resources, it is first necessary to trace the direct and indirect impact of increased health spending on wellbeing and then compare it with the equivalent impact of increased spending on wellbeing in other sectors. The key question is whether the maximum wellbeing gains associated with additional spending are best achieved through additional spending in the health sector.
There are important outputs of the health system, in the form of financial and social protection, that often go unrecognised but are likely to contribute to wellbeing independent of improvements in health. These include the health insurance benefits deriving from the health system and the implicit wealth transfer from richer, healthier people to poorer, sicker people.5 The nature and magnitude of such protection depends on the form of health coverage in a country, but it is a fundamental goal of universal health coverage.
More generally, we might consider the economy of wellbeing agenda as an opportunity to draw greater attention to the multiple pathways by which the health sector contributes to societal wellbeing through furthering the objectives of other sectors.21 As well as being valued in their own right, health outcomes produced by the health sector contribute indirectly to other sectors, most notably but not exclusively, education and economic productivity. For example, by preventing and alleviating the consequences of disability, health systems can help people have longer, more productive working lives and reduce the fiscal and social costs of dependency in older age.18 Or a programme targeted at improving the health of schoolchildren could also lead to improved school attendance and associated improvements in cognitive development. Recently, the European Observatory on Health Systems and Policies and the World Health Organization highlighted evidence of the multiple ways health systems in G20 countries contribute to economic objectives—including wellbeing—for the 2019 G20 health ministers meeting in Japan and the United Nations General Assembly meeting in New York.22
Opportunities and challenges
The use of wellbeing as an organising principle for governments has many attractive features. It can be a unifying concept for assessing government spending priorities and help overcome the tendency for spending programmes to become entrenched in particular ministerial “silos.” However, it also poses practical challenges. Most notably, the complexities of measuring the contributions to wellbeing of vastly different programmes are daunting. Furthermore, there are also philosophical challenges—for example, does an emphasis on improving wellbeing imply that low priority will be given to those who have little capacity to become happier? There are also conceptual debates about whether personal autonomy, in the form of an ability to adapt and self-manage, may be a more appropriate underpinning concept for wellbeing than life satisfaction. 23 24 25 26
The emphasis on wellbeing nevertheless offers many opportunities for the health sector. It could show that additional spending on health contributes positively to wellbeing through multiple pathways, rather than being merely a cost pressure on government finances. However, a focus on wellbeing could also indicate a departure from the reliance on traditional ministry specific budgeting, and so brings with it new challenges for health policy makers.
For policies enacted within the health sector, an important requirement will be to track the implications of those policies for objectives beyond health improvement that have an influence on wellbeing. A first step would be to routinely incorporate health system objectives such as equity and financial protection into conventional economic evaluation techniques such as cost effectiveness analysis.24 25 26 While health ministries should remain guardians of population health, and use health improvement as a prime performance measure, they will need to show that their spending is good use of government funds and show their broader impact on wellbeing.27 The particular importance of mental health as a determinant of wellbeing may suggest the need for a shift away from traditional priorities in the health sector.
Methods such as cost effectiveness analysis (possibly enhanced as above) are likely to remain the cornerstone of assessing the health outcomes of health system spending. However, they will also have to be augmented with estimates of the impact of the health system (negative or positive) on other sectors, such as employment or social protection, which also make important contributions to wellbeing. Consideration of the broader consequences of health systems is more than just an analytic concern and could allow an economy of wellbeing approach, in which all sectors seek to assess the impact of their policies on the objectives of other sectors. In the past, the health sector has advocated a health in all policies approach, which focused attention on the wide set of influences on population health arising from the actions of other sectors. In contrast, a wellbeing approach could require an assessment of the wide set of gains within the sphere of wellbeing that arise from the actions of the health sector.27
Cross sectoral projects, such as programmes to deal with risk factors associated with non-communicable disease, are likely to become particularly important from a wellbeing perspective. These might take the form of programmes to tackle smoking, childhood obesity, or poor nutrition, for example. The benefits (and costs) of such programmes are likely to accrue across several sectors, such as education, social care, and transport. The health sector will need to find ways of working effectively across traditional boundaries to assess the influences of such programmes on wellbeing. Many such programmes are likely to require the commitment of health sector funds to collaborative programmes and the development of effective governance mechanisms to ensure that the objectives of all participating sectors are met.28
The wellbeing agenda is a long way from being implemented comprehensively in any country, and given the analytic challenges some doubts about its feasibility exist. If it is adopted as a unifying principle of government, it will require new ways of thinking about the outcomes arising from health system actions.
Key messages.
Interest is growing in wellbeing as an economic and societal objective
It is not clear what this could mean for health and health systems
Although health makes a large contribution to most measures of wellbeing, there is no guarantee that focusing on wellbeing would lead to more resources for health systems
Health policy makers and analysts should consider new approaches that highlight the multiple direct and indirect pathways by which health systems contribute to wellbeing and ensure that these are incorporated into evaluation methods
Contributors and sources: This article arises from the work of both authors for the European Observatory on Health Systems and Policies and the WHO European Regional Office on an extensive programme of work examining the impact of the health sector on the broader economy. The authors contributed in equal part to all aspects of the paper, which represents a synthesis of much of that work, referred to in the references. PS is guarantor. The views expressed are those of the authors and not necessarily those of WHO.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This paper was commissioned by The BMJ as part of its Health, Wealth, and Profits series. Open access fees are paid by WHO, which had no role in the decision to publish.
References
- 1. Stiglitz J, Sen A, Fitoussi J-P. Commission on the measurement of economic performance and social progress. INSEE, 2009. [Google Scholar]
- 2. Fan VY, Bloom DE, Ogbuoji O, Prettner K, Yamey G. Valuing health as development: going beyond gross domestic product. BMJ 2018;363:k4371. 10.1136/bmj.k4371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Council of the European Union. The economy of wellbeing—council conclusions 2019 https://data.consilium.europa.eu/doc/document/ST-11164-2019-INIT/en/pdf
- 4. O’Donnell G, Oswald AJ. National well-being policy and a weighted approach to human feelings. Ecol Econ 2015;120:59-70. 10.1016/j.ecolecon.2015.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Helliwell J, Layard R, Sachs J. World happiness report 2019. Sustainable Development Solutions Network, 2019. [Google Scholar]
- 6.Anand S, Sen A. Human development index: methodology and measurement. 1994. http://hdr.undp.org/en/content/human-development-index-methodology-and-measurement
- 7.Organization for Economic Cooperation and Development. OECD Better Life Index. 2019. http://www.oecdbetterlifeindex.org/#/01111115111
- 8.What Works Centre for Wellbeing. 2018. How to measure your impact on wellbeing. http://measure.whatworkswellbeing.org
- 9. Drummond M, Sculpher M, Claxton K, Torrance G, Stoddart G. Methods for the economic evaluation of health care programmes. 4th ed Oxford University Press, 2015. [Google Scholar]
- 10. Schleicher A. PISA 2019: insights and interpretations. OECD, 2019. [Google Scholar]
- 11. Frijters P, Clark AE, Krekel C, Layard R. A happy choice: wellbeing as the goal of government. Behavioural Public Policy 2020: 1-40. 10.1017/bpp.2019.39. [DOI] [Google Scholar]
- 12.Organisation for Economic Cooperation and Development. Government expenditure by function (COFOG). OECD Statistics Database, 2019.https://stats.oecd.org/Index.aspx?datasetcode=SNA_TABLE11
- 13. Anderson M, Mossialos E. Beyond gross domestic product for New Zealand’s wellbeing budget. Lancet Public Health 2019;4:e320-1. 10.1016/S2468-2667(19)30109-4 [DOI] [PubMed] [Google Scholar]
- 14. Clark A, Flèche S, Layard R, Powdthavee N, Ward G. The origins of happiness: the science of well-being over the life course. Princeton University Press, 2018 10.2307/j.ctvc77dgq [DOI] [Google Scholar]
- 15. Claxton K, Martin S, Soares M, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess 2015;19:1-503, v-vi. 10.3310/hta19140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stadhouders N, Koolman X, van Dijk C, Jeurissen P, Adang E. The marginal benefits of healthcare spending in the Netherlands: Estimating cost-effectiveness thresholds using a translog production function. Health Econ 2019;28:1331-44. 10.1002/hec.3946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Glob Health 2018;3:e000964. 10.1136/bmjgh-2018-000964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cylus J, Permanand G, Smith P. Making the economic case for investing in health systems: what is the evidence that health systems advance economic and fiscal objectives? World Health Organization, 2018. [Google Scholar]
- 19. World Health Organization Closing the gap in a generation: Health equity through action on the social determinants of health. World Health Organization, 2008. [Google Scholar]
- 20. Hahn RA, Truman BI. Education improves public health and promotes health equity. Int J Health Serv 2015;45:657-78. 10.1177/0020731415585986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yamey G, Beyeler N, Wadge H, Jamison D. Investing in health: the economic case. World Innovation Summit for Health, 2016. [DOI] [PubMed] [Google Scholar]
- 22.European Observatory on Health Systems and Policies. Observatory presents new research on health financing and population ageing at a side event to the G20 health ministers meeting 2019. http://www.euro.who.int/en/about-us/partners/observatory/news/news/2019/11/observatory-presents-new-research-on-health-financing-and-population-ageing-at-a-side-event-to-the-g20-health-ministers-meeting.
- 23. Huber M, Knottnerus JA, Green L, et al. How should we define health? BMJ 2011;343:d4163. 10.1136/bmj.d4163 [DOI] [PubMed] [Google Scholar]
- 24. Cookson R, Mirelman AJ, Griffin S, et al. Using cost-effectiveness analysis to address health equity concerns. Value Health 2017;20:206-12. 10.1016/j.jval.2016.11.027 10.1016/j.jval.2016.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smith PC. Incorporating financial protection into decision rules for publicly financed healthcare treatments. Health Econ 2013;22:180-93. 10.1002/hec.2774 [DOI] [PubMed] [Google Scholar]
- 26. Verguet S, Kim JJ, Jamison DT. Extended cost-effectiveness analysis for health policy assessment: a tutorial. Pharmacoeconomics 2016;34:913-23. 10.1007/s40273-016-0414-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Walker S, Griffin S, Asaria M, Tsuchiya A, Sculpher M. Striving for a societal perspective: a framework for economic evaluations when costs and effects fall on multiple sectors and decision makers. Appl Health Econ Health Policy 2019;17:577-90. 10.1007/s40258-019-00481-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jakab M, Smith P. Cross-sectoral policies to address non-communicable diseases. In: Culyer A, Teerawattananon Y, Isaranuwatchai W, Archer A, eds. Non-communicable disease prevention: best buys, wasted buys and contestable buys. Open Book Publishers, 2019: 129-46. 10.11647/OBP.0195.08 10.11647/OBP.0195.08 [DOI] [Google Scholar]