ABSTRACT
Acute stroke care demands real-time, specialist-led treatment decisions, including thrombolysis and referral for mechanical thrombectomy. Pathways designed to deliver time-critical interventions for stroke patients are under intense pressure due to the impact of COVID-19 pandemic. In response to this unprecedented burden on acute care services, stroke clinicians are having to reconfigure existing clinical pathways both within and between hospitals. Incorporating artificial intelligence and digital communication support into clinical pathways offers an opportunity to mitigate the disruption to acute stroke care. In this case study we describe how Royal Berkshire Hospital, working collaboratively with Brainomix, a UK-based artificial intelligence software company, adopted technological innovation and integrated it into the hyperacute stroke pathway. A case is presented to demonstrate how this innovation can support patient care and deliver successful patient outcomes. We believe this model can be adopted in other hospitals and networks to deliver safe and efficient hyperacute stroke care.
KEYWORDS: Acute stroke, artificial intelligence, AI, COVID-19
Background
COVID-19 preparation has demanded a prompt NHS response, with reconfigurations nationally and within individual trusts progressing apace. These changes include clinicians working outside their parent specialties, dual specialists being redeployed to general medical areas, and the patient pathways in emergency departments (EDs) being redesigned to deal with COVID-19 admissions.
Attention is also being given to the urgent and emergency non-respiratory work that will be impacted by the COVID-19 pandemic. Acute stroke care demands timely clinical evaluation and complex decision-making regarding treatments, discharge and interhospital transfer. Optimising these decisions has never been more important, but additionally the minimisation of person-to-person contact, maintenance of a healthy workforce and enabling contributions from those in social isolation are increasingly important considerations for the sustainable delivery of high-quality care.
Specific challenges facing the delivery of stroke care include managing the increasing demands on stroke specialists, who often have dual accreditation in general medicine, a skillset under increasing demand. The home of acute stroke care is the ED, and it is imperative to maintain standards and minimise disruption in this key area of the hospital.
The Royal College of Physicians (RCP) ethical guidance for frontline staff dealing with the COVID-19 pandemic states that the presence or absence of COVID-19 should not be a limiting factor when making treatment decisions. Where allocation of care between a patient with COVID-19 and another patient without COVID-19 is being considered, care should be prioritised based on national guidelines.1
The NHS guidance for the management of stroke patients during the COVID-19 pandemic recommends that services already using virtual assessment facilities in the stroke pathway out-of-hours should consider using them during normal working hours. It also encourages accelerated introduction of artificial intelligence (AI) decision support and adoption of technology to speed up image interpretation and remote treatment decision making.2 To facilitate the adoption of these innovative approaches, NHS England and NHS Improvement have been given legal assurance by the Information Commissioner's Office (ICO) to support the processing and sharing of information to help the Covid-19 response where there is no practical alternative and the benefits of sharing information outweigh the risk.3
Here we are sharing our experience of changing the stroke pathway at the Royal Berkshire NHS Foundation Trust (RBH, Reading, UK) by fast-tracking the adoption of AI and digital communication. Presentation of this case report is of particular importance to healthcare service providers and researchers tasked with deploying strategies to mitigate the impact which the COVID-19 pandemic presents.
The pre-COVID-19 hyperacute stroke pathway
The Royal Berkshire NHS Foundation Trust (RBH) serves a population of approximately 600,000 and admits approximately 700 patients with stroke annually. The acute stroke service provides 24/7 thrombolysis and a 7-day transient ischemic attack (TIA) service. The average thrombolysis rate is 20–25% of the stroke admissions.
Before the COVID-19 pandemic, the thrombolysis service was delivered by consultant stroke physicians, neurologists and ED physicians working on a rota. The ED was pre-alerted by the ambulance crew to the arrival of an acute stroke patient. The stroke team received the patient in the ED in person.
Decisions for mechanical thrombectomy were made by the on-call stroke/neurology consultant, and the patients could be referred to Oxford University Hospitals or to Charing Cross Hospital depending on service availability.
This model has several vulnerabilities particularly during the COVID-19 crisis:
Delivery of thrombolysis/mechanical thrombectomy referral service relied upon ED physicians.
There was variation in the staffing of the thrombolysis rota at different times of day and at the weekend.
Remote access to brain imaging was available only via Trust computers. This restricted access to imaging for fast decision making, particularly when the non-resident on-call consultant was travelling to or from work.
Communication between the members occurred via telephone only. This had a potential to cause delays when that member was not available to respond.
The COVID-19 hyperacute stroke pathway
Prior to the onset of the COVID-19 pandemic, RBH had successfully introduced the e-Stroke Suite (Brainomix, Oxford, UK) AI software into the hyperacute stroke pathway. The e-Stroke Suite processes non-contrast CT and CT angiography stroke scans in real-time and highlights and quantifies early ischaemic changes (e-ASPECTS).4,5 It also identifies large vessel occlusion and collateral vessel density in the anterior circulation (e-CTA) to the treating clinician.6 The e-Stroke Suite uses both traditional machine learning classifiers and deep learning algorithms to evaluate changes on acute stroke imaging.7 Such approaches are attracting increasing interest, particularly in the field of radiology.8
Fast identification of large vessel occlusion and reliable quantification of the extent of ischaemic injury is crucial to the robust delivery of a mechanical thrombectomy service. The Alberta Stroke Programme Early CT Score (ASPECTS) is a 10-point quantitative topographic CT scan score where 10 regions in the middle cerebral artery territory are each given a point.9 One point is deducted for each region with early ischaemic change. ASPECTS is recommended in European Stroke Organisation and American Heart/Stroke Association guidelines to inform patient selection for mechanical thrombectomy.10,11
The aim of this project was to enable less experienced physicians to make decisions about thrombectomy referrals in a timely manner and reduce the door-in-door-out time for these patients. The modules of the e-Stroke Suite are CE-marked for use in supporting decision making by clinicians of different experiences and have been independently validated in different healthcare systems.12–14
In response to the COVID-19 crisis, RBH fast-tracked the adoption of the additional e-Stroke Cloud capability of the Brainomix software, enabling the use of a smartphone app. The app enables instant access to brain imaging for on-call stroke or neurology consultants wherever they are, alongside the AI decision support. The app also has the functionality to share pseudonymised images outside of the organisation to facilitate referral along the stroke pathway, or to seek expert opinion remotely.
In line with ICO guidelines, RBH has also created a WhatsApp group connecting all the stroke and neurology consultants who cover the thrombolysis rota. When an acute stroke patient arrives in ED (hot/cold ED depending on their COVID-19 status) and when there is no resident stroke or neurology consultant, the patient is rapidly triaged by a front door clinician to ensure the patient is clinically safe to be transferred to the radiology department for imaging. The stroke thrombolysis specialist nurse alerts the stroke or neurology consultant group via WhatsApp with clinical information. One of the non-resident stroke or neurology consultants will respond immediately to take over the management of that patient.
The brain and vascular imaging is processed through the software and the consultants will receive an alert from the app within a few minutes. Consultants can securely access the images remotely via their mobile phone and guide treatment decisions. WhatsApp provided supplementary support to pool the expertise of several specialists during clinical decision making and also provides both audio and video communications available on a mobile device.
Every attempt was made to protect patient-identifiable data and only necessary information was shared in accordance with ICO guidelines.3 The images shared in the Brainomix app only included patient identification number and the date and time of the imaging. These details are crossed checked with the WhatsApp information to mitigate the risk of error in clinical decision making.
The new pathway (Fig 1) has the following advantages:
Fig 1.
Covid-19 hyperacute stroke pathway.
Consultants who are self-isolating with mild COVID-19 symptoms or due to family member illness can take part in the rota and support decision making remotely.
The ED physicians are released from their involvement in stroke pathway to focus on managing COVID-19 admissions.
It facilitates the expansion of stroke and neurology consultant cover to weekends, reducing the variation in the specialist delivery of hyperacute stroke treatment between weekdays and weekends.
Treatment decisions can be made without delay as the Brainomix app provides instant access to imaging.
Pseudonymised images can be shared between hospitals for the purpose of thrombectomy referral.
WhatsApp communication enables more joined up working and decision making and provides instant video access if required. It also facilitates immediate second opinion and advice from peers.
Case presentation
The first patient who was transferred for mechanical thrombectomy since we introduced the new pathway is presented below.
A 70-year-old male with a suspected acute stroke was brought in by ambulance to the Royal Berkshire hospital ‘Cold ED’ on a Sunday. He was previously independent and had history of atrial fibrillation which was treated with ablation in 2005. He was not on anticoagulation.
On examination he had right-sided face, arm and leg hemiparesis, hemisensory loss and hemianopia and dysphasia. His NIHSS (National Institute of Health Stroke Scale) score was 22, indicating a severe stroke.
The stroke specialist nurse alerted the consultant team via WhatsApp. The on-call stroke consultant was driving home from hospital, so was not available to take the call. Another consultant, who was self-isolating due to a family member illness, picked up the call immediately and reviewed the images on the Brainomix app. The AI-processed images confirmed the presence of early ischemia in the left middle cerebral artery (MCA) territory and highlighted the proximal occlusion in the M1 segment of the left MCA (Fig 2a, b). The decision was made immediately to initiate intravenous thrombolysis and a direct referral was made to the neuroscience centre for mechanical thrombectomy. Pseudonymised images were shared to the neuroscience centre via the Brainomix app linked to the cloud server. A decision to transfer the patient was made using these images while traditional image transfer was awaited via the image export portal (IEP).
Fig 2.
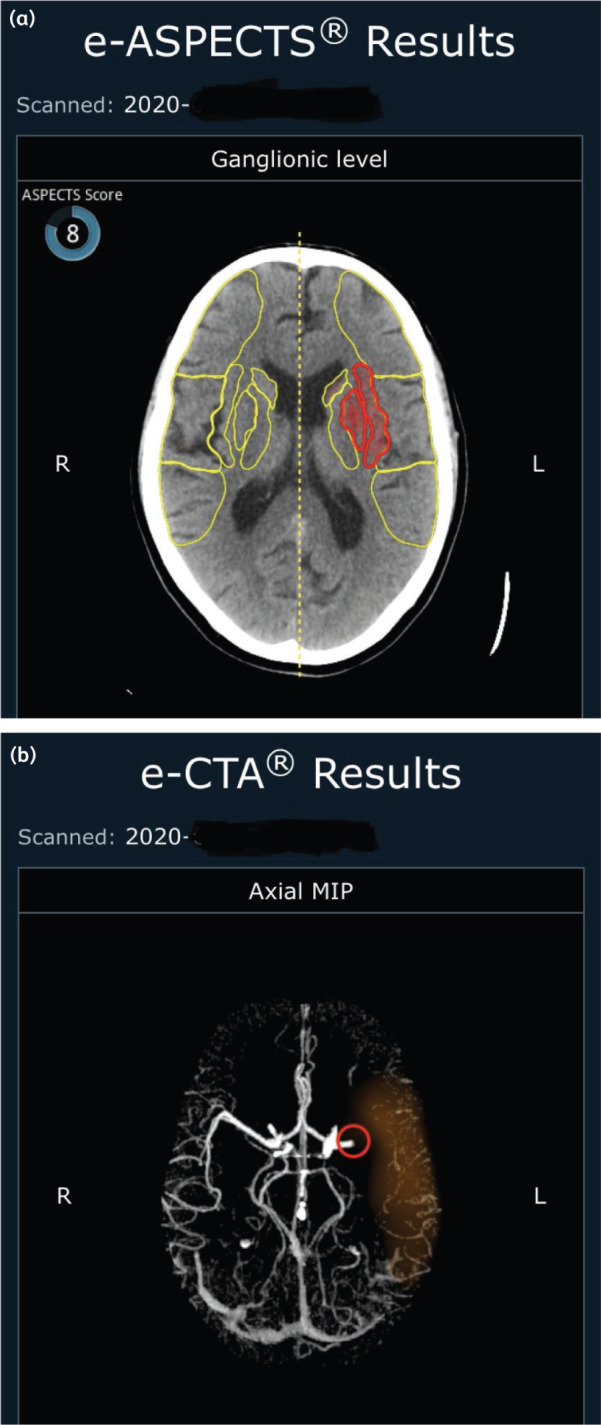
AI-processed images from the Brainomax app. (a) View of non-contrast CT brain scan. Area of early infarction is indicated by red heat-map. (b) View of MIP CT angiogram. Proximal left middle cerebral artery occlusion is highlighted by the red circle. MIP = Maximum Intensity Projection.
The patient underwent mechanical thrombectomy with excellent outcome. The NIHSS improved from 22 to 7 post procedure. He was repatriated back to RBH on the same day for ongoing care and was discharged home 3 days later fully independent.
Despite presenting to the ED on a Sunday during the COVID-19 crisis, the patient received a high standard of care and achieved an excellent outcome. The door-to-needle time was 40 minutes, which was longer than the pre-COVID-19 average door-to-needle time of 32 minutes (there is additional delay as the new Cold ED is further away from the radiology department vs the usual location) and the door-in-door-out time was 75 minutes (Table 1), in contrast to the mean historical door-in-door-out time for our centre of 120 minutes.
Table 1.
Timeline of the patient journey
| Symptom onset | 10:40 |
| Arrived in ED | 11:35 |
| CT imaging | 11:59 |
| Image processed | 12:02 |
| WhatsApp alert | 12:06 |
| WhatsApp response | 12:07 |
| Treatment decision | 12:13 |
| IV bolus | 12:15 |
| Transferred for thrombectomy | 12:50 |
| Recanalisation achieved | 14:38 |
Conclusion
The CE-marked e-Stroke Suite software was implemented at the RBH prior to COVID-19 as part of a quality improvement project supported by Oxford Academic Health Science Network (AHSN) and the National Consortium of Intelligent Medical Imaging (NCIMI) to improve mechanical thrombectomy referral pathway.12,14 The deployment of cloud capability of the software was fast-tracked in response to COVID-19 pathway redesign at RBH in order to provide instant access remote image reviewing on mobile devices.
This case demonstrates how by adopting AI decision support and digital technology, and integrating them into stroke pathway in response to the ongoing COVID-19 crisis, enabled high-quality patient care and excellent patient outcomes. Our experience provides a model for wider adoption of similar innovations, not only in a single centre but throughout a network of hospitals to deliver hyperacute stroke care more efficiently in this unprecedented situation.
The limitations of this report include the lack of comparison to standard care, or to alternative solutions, but the urgent need for reconfiguration precluded such an evaluation. Variations of AI, including machine learning (ML) methods such as random forest learning (RFL) and convolutional neural networks (CNNs), are used to evaluate patients with large vessel occlusion strokes by different providers. Four current software platforms incorporate machine learning for stroke decision making: Brainomix, General Electric, iSchemaView and Viz.ai, each with differing functionalities.6,7 Limitations of the current smartphone platform include the lack of ability to compare previous images side by side and view the proximal carotid vessels. The speed of image availability on the cloud depends upon the hospital internet speed and the Wi-Fi or network black spots in certain areas in hospital interfering with WhatsApp communications.
The key lessons learned in this initiative are the need for close collaboration between hospital teams, including clinical stroke, radiology, IT, information governance and management, and the software provider. Efficient integration required on-the-ground support from all key stakeholders early on, and continued expert input to ensure a robust integration that supported patient care.
This report supports the NHS England advice on adoption of AI and use of digital platforms to deliver stroke care. The RCP ethical guidance and NHSX assurance to facilitate sharing of data responsibly during the COVID-19 crisis for the benefit of patients provides an impetus for hospitals and networks to adopt technology in fighting the COVID crisis.
Acknowledgements
We wish to acknowledge Dr Guy Rooney (Oxford Academic Health Science Network) and the National Consortium for Intelligent Medical Imaging for their involvement and support in implementing Brainomix e-stroke suite into the stroke pathway at RBH as part of a regional thrombectomy quality improvement project.
We also wish to acknowledge Ms Chani Edwards (Benefits Realisation Manager at RBH) and Mr Jonathan Rees (Head of Performance, Operational Planning and Transformation at RBH) for their dedication and support in rapidly adopting the Brainomix cloud-based app.
Conflicts of interest
Dr George Harston is employed part-time by Brainomix as chief medical and innovation officer.
References
- 1.Royal College of Physicians. Ethical guidance published for frontline staff dealing with pandemic. RCP, 2020. Available from www.rcplondon.ac.uk/news/ethical-guidance-published-frontline-staff-dealing-pandemic [Accessed 12 April 2020].
- 2.NHS England and NHS Improvement. Clinical guide for the management of stroke patients during the coronavirus pandemic. NHSE and NHSI, 2020. Available from www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C033-Specialty-guide_-Stroke-and-coronavirus-v1-24March_.pdf [Accessed 12 April 2020].
- 3.NHSx. Covid-19 Information Governance advice for health and care professionals. NHSx, 2020. Available from www.nhsx.nhs.uk/key-information-and-tools/information-governance-guidance/health-care-professionals [Accessed 12 April 2020].
- 4.Goebel J, Stenzel E, Guberina N, et al. Automated ASPECT rating: comparison between the Frontier ASPECT Score software and the Brainomix software. Neuroradiology 2018;60:1267–72. [DOI] [PubMed] [Google Scholar]
- 5.Sundaram VK, Goldstein J, Wheelwright D, et al. Automated ASPECTS in acute ischemic stroke: a comparative analysis with CT perfusion. AJNR 2019;40:2033–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grunwald IQ, Kulikovski J, Reith W, et al. Collateral automation for triage in stroke: evaluating automated scoring of collaterals in acute stroke on computed tomography scans. Cerebrovasc Dis 2019;47:217–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murray NM, Unberath M, Hager GD, et al. Artificial intelligence to diagnose ischemic stroke and identify large vessel occlusions: a systematic review. J Neurointerv Surg 2020;12:156–64. [DOI] [PubMed] [Google Scholar]
- 8.Yamashita R, Nishio M, Do RKG, et al. Convolutional neural networks: an overview and application in radiology. Insights Imag 2018;9:611–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pexman JH, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol 2001;22:1534–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointervent Surg 2019;pii: neurintsurg-2018-014569. [DOI] [PubMed] [Google Scholar]
- 11.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals rrom the American Heart Association/American Stroke Association. Stroke 2019;50:e344–e418. [DOI] [PubMed] [Google Scholar]
- 12.Herweh C, Ringleb PA, Rauch G, et al. Performance of e-ASPECTS software in comparison to that of stroke physicians on assessing CT scans of acute ischemic stroke patients. Int J Stroke 2016;11:438–45. [DOI] [PubMed] [Google Scholar]
- 13.Pfaff J, Herweh C, Schieber S, et al. e-ASPECTS correlates with and is predictive of outcome after mechanical thrombectomy. Am J Neuroradiol 2017;38:1594–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagel S, Sinha D, Day D, et al. e-ASPECTS software is non-inferior to neuroradiologists in applying the ASPECT score to computed tomography scans of acute ischemic stroke patients. Int J Stroke 2017;12:615–22. [DOI] [PubMed] [Google Scholar]



