ABSTRACT
COVID-19 presents an unprecedented challenge to hospitals and the systems in which they operate. The primary exponential surge of COVID-19 cases is arguably the most devastating event a hospital will face. In some countries, these surges during the initial outbreak of the disease have resulted in hospitals suffering from significant resource strain, leading to excess patient mortality and negatively impacting staff wellbeing. As experience builds in managing these surges, it has become evident that agile, tailored planning tools are required. The comprehensive hospital agile preparedness (CHAPs) tool provides clinical planners with six key domains to consider that frequently create resource strain during COVID-19; it also allows local planners to identify issues unique to their hospital, system or region. Although this tool has been developed from COVID-19 experiences, it has potential to be modified for a variety of pandemic scenarios according to transmission modes, rates and critical care resource requirements.
KEYWORDS: Emergency preparedness, COVID-19, global pandemic, disaster readiness, SARS-CoV-2
The problem
COVID-19 presents an unprecedented challenge to hospitals and the systems in which they operate.1 The primary exponential surge of COVID-19 cases is arguably the most devastating event a hospital will face.2 This will be exacerbated by any pre-existing stress and decreased systemic resilience already affecting healthcare systems. In some countries, these surges during the initial outbreak of the disease resulted in hospitals suffering from significant resource strain, leading to excess patient mortality and negative impacts on staff wellbeing.3,4 Both of these factors severely hamper the sustainability of the local COVID-19 response.3,5,6
In this paper, we outline a structured approach to hospital preparedness for local surges. This is based on NHS England and NHS Improvement's Secondary care: document of preparedness, which takes a comprehensive view and aims to support local responses and minimise the risk these exponential surges cause.7
The approach
To allow hospitals to rapidly prepare for a surge we have produced the CHAPs (Comprehensive Hospital Agile PreparednesS) tool for swift identification of potential bottlenecks in hospital systems according to our current understanding of COVID-19 (see Fig 1). This structured approach highlights six key domains: workforce; infrastructure; supplies and equipment; service reconfiguration; data and information technology; and communications. While these domains are independent factors, they do not function independently. If one domain is disrupted, the system will struggle and this in turn will affect the other domains.
Fig 1.
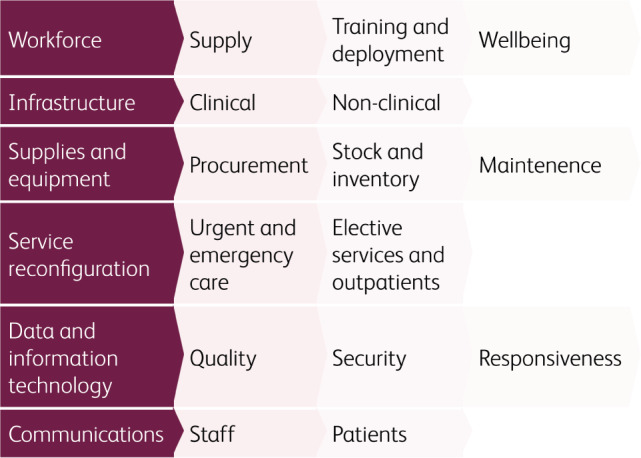
CHAPs tool for pandemic preparedness, based on the COVID-19 experience.
Domain one: Workforce
One of the government's responses to COVID-19 is self-isolation: an individual should isolate for 7 days if they are symptomatic, or 14 days if they are well but residing in the same household as a symptomatic individual.8 As hospital staff self-isolation increases and inpatient numbers surge during pandemic spread, hospital human resources are immediately put under pressure.9–11 As a result, organisations need to proactively consider the supply of their workforce. Consideration should be given to methods of workforce expansion, such as internal redeployment of staff to support areas of greatest demand and the external recruitment of staff from clinical and non-clinical settings.12,13 Sources of staff from non-clinical settings include those that have recently retired, returners from research and education, healthcare students and volunteers.12,14 Recruitment emphasis has to be given to both clinical and non-clinical staff, with non-clinical staff essential to optimising service delivery and ensuring adherence to infection control policies.
Once workforce numbers are maximised, focus should be given to prioritising induction, training and familiarity with the new clinical environment.15 In order to optimise absolute numbers of staff, rotas should be redesigned to account for an increase in staff sickness rates and to ensure safe out-of-hours staffing levels.11
The wellbeing of the workforce is an imperative during a prolonged major incident. Healthcare staff are at an increased risk of mental health issues during the COVID-19 pandemic, similar to those seen in the combat military, and organisations should prioritise local support systems to mitigate this.11,16,17 Procedures should be in place to monitor staff sickness and absenteeism. In the UK, the NHS has introduced a confidential staff support telephone line and has partnered with wellbeing apps to provide mental health and wellbeing support to staff, with many local trusts offering support as well.6,18 It is also important to consider staff who are most vulnerable to severe disease should they contract COVID-19, as well as those who live with vulnerable people, to ensure the appropriate protections are in place to minimise their level of risk whilst maximising use of their skills.19
Domain two: Infrastructure and estates
Secondary care organisations should optimise all aspects of their infrastructure and estates in preparation for a COVID-19 surge. Hospitals will likely need to expand their medical and critical care capacity by redesigning existing spaces into clinical areas.3,11 Design layouts built around patient pathways should be considered to aid staff productivity.20 Cohorting of patients within the estate is also of utmost importance to adhere to infection control policies. Safe and efficient internal and external transportation pathways for patients, equipment, clinical supplies and specimens should be created.21 Oxygen is a critical medical resource in the management of patients with COVID-19, so estates teams and pharmacy departments should partner to safeguard the supply, flow capacity and quality assurance of medical gas pipeline systems with strict adherence to fire regulations in oxygen-rich environments.22
Estates departments should ensure there is capacity to manage an increase in demand for non-clinical resources such as waste management, water, electricity, ventilation, heating, air conditioning, catering and parking.23 Hospitals are also likely to experience an increase in demand on their mortuary services, and procedures should be in place to ensure that respect and dignity is maintained in the movement and storage of patients after death.4
Domain three: Supplies and equipment
The availability of sufficient supplies and equipment to respond to COVID-19 has been cited as a challenge worldwide.24 Procurement teams should collaborate with clinicians to review delivery ordering schedules, taking into consideration current stock inventories and anticipated additional needs for equipment, medical and non-medical supplies.25 This should be reviewed regularly in response to changing demands.
Methods should be in place to monitor, maintain and accurately report equipment and stock levels in each clinical area. Escalation procedures for supply shortages within the organisation should be clearly communicated. Essential items to consider are personal protective equipment (PPE), respiratory support and infection control resources.24 Storage of stock should be organised and pre-prepared packs and checklists considered for clinical procedures, aiding staff productivity and minimising infection control risks. There should be contingency plans in place to ensure that all equipment is maintained and serviced appropriately. Actions to mitigate stock theft should also be implemented.26
Domain four: Service reconfiguration
The reconfiguration of services to maximise inpatient and critical care capacity in response to a COVID-19 surge is vital. NHS hospitals have been encouraged to postpone all non-urgent elective operations and outpatient clinics and to urgently discharge medically fit patients.27 Systems may need to be adapted to ensure the effective triage of patients.
In addition, organisations will need to consider how they maintain continuity of care for non-coronavirus patients while protecting these patients from contracting the illness, and measure and mitigate the unintended consequences of delayed presentations. This could involve developing alternative clinical pathways and models of care, as well as implementing appropriate admission avoidance schemes.
Domain five: Data and information technology
High-quality situation report data are critical to inform COVID-19 local and national decision-making, as well as communications to the general public.28 In the UK, the NHS is capturing key metrics such as inpatient bed occupancy levels and length of stay for COVID-19 patients to inform the response.29 Prior to a surge it is essential that data quality assurance mechanisms are reviewed. This may require additional administrative support to be embedded within the organisation. Sufficient analytical capabilities are essential to develop insight from this data, and hospital leadership should have the ability to respond to these insights. Additionally, COVID-19 has resulted in a spike in cyber-attacks and data security threats on hospitals;30 systems should be in place to minimise these risks and ensure that data is securely stored and managed according to national standards and the General Data Protection Regulation (GDPR).
Domain six: Communications
Timely dissemination of information is of key importance to clinicians managing COVID-19 patients.13 Robust communication channels are vital to ensure staff are informed of the latest clinical guidance, local service re-organisation developments, wellbeing support services and patient safety escalation procedures.31 Personal protective equipment may be a direct barrier to receiving critical communications in the traditional manner (eg bleeps), so novel approaches may need to trialled. Information change has been rapid since the start of the outbreak, putting staff at significant risk of the ‘fog’ of information overload.32 As a result, hospital information should be filtered to be as concise and relevant as possible. The current pandemic has also resulted in sources of misinformation and staff should be equipped to address queries and concerns raised by patients.
Infection control policies should be clearly communicated to all patients and organisations should consider amendments to their visitor protocols.33 Systems should be in place to ensure that despite visitor restrictions, communication strategies are maintained between the relatives of patients and staff.33 Outpatients should be informed of service reorganisation developments, including the postponement of non-urgent surgeries and clinics. The organisation should ensure that external communications messaging is consistent with public health and national messaging.34
Discussion
Pandemic preparedness
Prior to the COVID-19 outbreak, most international pandemic preparedness plans focused on an outbreak model of pandemic influenza.35,36 In building this tool for COVID-19 preparedness, it has become apparent that although there are many areas of similarity in preparedness for most outbreaks, certain nuances of the disease have caught hospitals off-guard. In future, national, regional and local preparedness plans should include a variety of sensitivity scenarios, taking into account a variety of transmission modes, transmission rates and critical care equipment quirements (for example haemofiltration machines, as opposed to ventilators).
Wellbeing
The COVID-19 outbreak has highlighted the importance of maintaining a resilient workforce. It has emphasised the necessity to maintain staff wellbeing during business-as-usual times in order to give staff the capabilities to manage through a crisis.5,6,37 Corporations that see employee wellness as a source of competitive advantage outperform those who do not, with healthcare systems often neglecting staff wellbeing.38 Perhaps this will change in the aftermath of COVID-19.
Sustaining the response
National government intervention has focused on reducing viral transmission rates in order to reduce load on hospitals and reduce the resulting excess mortality.39 However, this also prolongs strain on healthcare workers and healthcare supply chains and has put a stop to a wide range of activities, including routine but important healthcare services such as screening programmes. It is difficult to quantify the long-term impact of this on patients, healthcare services and society. A key challenge to hospitals and the systems in which they operate is to balance the negative, unintended consequences of government intervention and maximise business-as-usual healthcare service delivery.
Conclusion
The tool presented in this paper allows for a comprehensive multi-disciplinary approach to preparedness planning for COVID-19. However, it is not possible to produce a tool to acknowledge the uniqueness of certain hospitals and hospital settings. It is therefore vital to ensure clear accountability within the organisation for pandemic preparedness, stress-test these preparations and identify triggers and rate-limiting factors that may lead to rapid resource depletion and hospital decompensation. Organisations should also consider their recovery strategies following the resolution of the COVID-19 pandemic as this is likely to pose a significant challenge.
References
- 1.Klompas M. Coronavirus disease 2019 (COVID-19): Protecting hospitals from the invisible. Ann Intern Med 2020, in press ( 10.7326/M20-0751). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verelst F, Kuylen E, Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Euro Surveill 2020;25:2000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee CCM, Thampi S, Lewin B, et al. Battling COVID-19: Critical care and peri-operative healthcare resource management strategies in a tertiary academic medical centre in Singapore. Anaesthesia 2020, in press ( 10.1111/anae.15074). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Francis A, Guo Y, Hurley P, et al. Projected ICU and mortuary load due to COVID-19 in Sydney. medRxiv 2020:2020.03.31.20049312. [Google Scholar]
- 5.Cao J, Wei J, Zhu H, et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom 2020, in press ( 10.1159/000507453). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unadkat S, Farquhar M. Doctors' wellbeing: self-care during the COVID-19 pandemic. BMJ 2020;368:m1150. [DOI] [PubMed] [Google Scholar]
- 7.NHS England. Secondary care: document of preparedness for COVID-19. NHS England, 2020. Available from: www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0280-secondary-care-preparedness.pdf
- 8.NHS England. Self-isolation if you or someone you live with has symptoms. Available from: www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-advice/. www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-advice/ [Accessed 9 April 2020].
- 9.Cao Y, Li Q, Chen J, et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med 2020;27:309–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzgerald G, Aitken P, Shaban RZ, et al. Pandemic H1N1 influenza 2009 and Australian emergency departments: implications for policy, practice and pandemic preparedness. Emerg Med Australas 2012;24:159–65. [DOI] [PubMed] [Google Scholar]
- 11.Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 2020;S2213-2600(20)30161–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHS England. Redeploying your secondary care medical workforce safely. NHS England, 2020. Available at: www.england.nhs.uk/coronavirus/publication/redeploying-your-secondary-care-medical-workforce-safely/
- 13.Wong J, Goh QY, Tan Z, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anesth/J Can Anesth 2020, in press ( 10.1007/s12630-020-01620-9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahase E. Covid-19: Medical students to be employed by NHS as part of epidemic response. BMJ 2020;368:m1156. [DOI] [PubMed] [Google Scholar]
- 15.Li L, Xv Q, Yan J. COVID-19: the need for continuous medical education and training. Lancet Respir Med 2020;8:e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020;368:m1211. [DOI] [PubMed] [Google Scholar]
- 17.Walker S. Assessing the mental health consequences of military combat in Iraq and Afghanistan: a literature review. J Psychiatr Ment Health Nurs 2010;17:790–6. [DOI] [PubMed] [Google Scholar]
- 18.NHS England. Support now. Available from: https://people.nhs.uk/help/
- 19.Brooke J, Jackson D. Older people and COVID-19: Isolation, risk and ageism. J Clin Nursing 2020, in press ( 10.1111/jocn.15274). [DOI] [PubMed] [Google Scholar]
- 20.Arnolds IV, Gartner D. Improving hospital layout planning through clinical pathway mining. Ann Operat Research 2018;263:453–77. [Google Scholar]
- 21.Liew MF, Siow WT, Yau YW, et al. Safe patient transport for COVID-19. Crit Care 2020;24:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan's experience. Anesthesiology 2020, in press ( 10.1097/ALN.0000000000003296). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NHS England. Novel coronavirus (COVID- 19) standard operating procedure: estates and facilities. NHS England, 2020. Available from www.england.nhs.uk/coronavirus/publication/covid-19-standard-operating-procedure-estates/
- 24.Xie J, Tong Z, Guan X, et al. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med 2020, in press ( 10.1007/s00134-020-05979-7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid-19 pandemic. NEJM 2020, in press ( 10.1056/NEJMp2006141). [DOI] [PubMed] [Google Scholar]
- 26.Chopra V, Toner E, Waldhorn R, Washer L. How should US hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med 2020, in press ( 10.7326/M20-0907). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens SPA. Next steps on NHS response to COVID-19 [Letter]. NHS England, 2020. Available from: www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf [Accessed 17 March 2020].
- 28.Moorthy V, Henao Restrepo AM, Preziosi MP, Swaminathan S. Data sharing for novel coronavirus (COVID-19). Bull World Health Organ 2020;98:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NHSX. How data is supporting the Covid-19 response 2020. Available from: www.nhsx.nhs.uk/key-information-and-tools/information-governance-guidance/how-data-is-supporting-covid19 [Accessed 8 April 2020].
- 30.Eddy N. Cyberattacks continue to mount during COVID-19 pandemic. Healthcare IT News, 8 April 2020. Available from: www.healthcareitnews.com/news/cyberattacks-continue-mount-during-covid-19-pandemic
- 31.Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020, in press ( 10.1001/jama.2020.3972). [DOI] [PubMed] [Google Scholar]
- 32.Carl Heneghan JB, Tom Jefferson. COVID-19: What proportion are asymptomatic? CEBM, 2020. Available from: www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/ [Accessed 6 April 2020].
- 33.Lee IK, Wang CC, Lin MC, et al. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J Hosp Infect, in press ( 10.1016/j.jhin.2020.02.022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cowper A. Covid-19: are we getting the communications right? BMJ 2020;368:m919. [DOI] [PubMed] [Google Scholar]
- 35.Gomersall CD, Loo S, Joynt GM, Taylor BL. Pandemic preparedness. Curr Opin Crit Care 2007;13:742–7. [DOI] [PubMed] [Google Scholar]
- 36.Iskander J, Strikas RA, Gensheimer KF, Cox NJ, Redd SC. Pandemic influenza planning, United States, 1978–2008. Emerg Infect Diseases 2013;19:879–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res 2020;287:112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Purcell J. Employers need to recognize that our wellness starts at work. Harvard Business Review, 15 November 2016. [Google Scholar]
- 39.Fang Y, Nie Y, Penny M. Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: a data-driven analysis. J Med Virol 2020, in press ( 10.1002/jmv.25750). [DOI] [PMC free article] [PubMed] [Google Scholar]


