Abstract
After the COVID-19 outbreak worldwide, we will sooner or later encounter trauma patients with COVID-19 in the developing countries. It is a challenging decision-making process for an orthopedic surgeon to provide the patients with the best practice in the crisis. Here we discuss the issue in terms of clinical severity of COVID-19 pneumonia, priority of orthopedic surgical trauma procedures and standard of care for the treatment of trauma injuries. We finally propose an algorithm for better management of trauma patients in the setting of COVID-19 mass spread.
Key Words: Clinical decision making, COVID-19, Orthopedics, Pandemics
Introduction
After the outbreak by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) was declared as a public health emergency of international concern by World Health Organization (WHO), more than 1,500,000 cases in 212 countries are engaged by the disease worldwide by now (1). Although mass gathering events are mainly cancelled in most countries, concern remains when strict quarantine rules are not established or respected due to public or political perceptions in countries with increasing infection rate (2). Taking the doubling period of 1.8 days into account for SARS-CoV-2 infection spread, we will sooner or later encounter trauma patients with COVID-19 (3).
During Severe Acute Respiratory Syndrome (SARS) outbreak, Wong et al reported an 81-year-old woman with intertrochanteric fracture and no history of contact with SARS patients who underwent close reduction and Gamma nail fixation under spinal anesthesia one day after admission. The patient developed oxygen desaturation and shortness of breath the day after and died 7 days later. The autopsy revealed typical findings of SARS (4). Fang also reported at least 2 patients treated with fracture during SARS crisis in Hong Kong but confirmed that they had SARS post mortem (5).
Given the uncertainty regarding the behavior of the virus after the surgery as a second hit insult to the previously in-danger patient, it is a big concern if we are misleading a stable COVID-19 patient towards a patient with aggravated comorbidity. It is stated in the literature that underlying comorbidities and weakened immune system are associated with adverse outcome in COVID-19 patients (6, 7). Besides delayed surgery risks the patient require complex operations in the next few months which will be less easily handled. Risk assessment in urgent orthopedic surgeries in COVID-19 patients includes an aggregate of the real risk of proceeding and that of postponing for weeks.
A study by Guan et al showed that among 1,099 patients with COVID-19, 18.7% presented with short of breath and 41.3% required oxygen supplementation (8). Hence, some authors recommend only emergency surgeries are scheduled on COVID-19 patients (9). Higher pulmonary embolic load, increased risk of pulmonary complication and massive blood loss following femoral shaft fracture necessitate early intervention either in the form of definitive fixation or sequenced surgeries using external fixator (10-12). Now the question is if the literature is supporting the damage control orthopedics (DCO) in borderline and severe trauma patients to reduce the rate of the adult respiratory distress syndrome (ARDS) and the multiple organ dysfunction (MOD), is it not logical to apply the same protocol in COVID-19 patients?
Hence, it is a challenging decision-making process for an orthopedic surgeon to provide the patients with the best practice in the crisis. Here we discuss the issue in terms of clinical severity of COVID-19 pneumonia, priority of orthopedic surgical trauma procedures and standard of care for the treatment of trauma injuries. We finally propose an algorithm for better triage and management of trauma patients in the setting of COVID-19 mass spread.
Clinical Severity of COVID-19 Pneumonia
A clear understanding of the disease severity is mandatory to weigh the risks and benefits of performing an intervention. Confirmed patients can be divided into 4 types according to the literature (13, 14): Critical, Symptomatic, Mildly symptomatic/history of exposure and Healed/healthy [Table 1]. However, one of the key concerns in orthopedic surgeries is timing. The median duration of both viral shedding and dyspnea in COVID-19 survivors is reported to be 20 days and increased by severity of the disease (7); the mean interval between symptom onset and hospital discharge is also reported to be 19 days (14). Meanwhile, there is uncertainty regarding the behavior of the virus in critical patients. This faces the orthopedic surgeon a minimum of 3 to 4 weeks delay until having a non-symptomatic or healed patient.
Table 1.
Patient Status according to Clinical Severity of Coronavirus Disease 2019 (COVID-19) Pneumonia Confirmed with PCR and/or Chest CT Scan (13, 14)
| Patient Status | Findings |
|---|---|
| Critical patient | Meet any of the followings: a. Respiratory distress, RR ≥30 times/min b. SpO2 <93% at rest c. PaO2/FiO2 ≤ 300 mmHg d. rapid progression (>50%) on CT imaging within 24-48 hours e. Respiratory failure, need mechanical assistance f. Shock g. “Extra pulmonary” organ failure, intensive care unit is needed |
| Symptomatic patient | Fever Respiratory symptoms Imaging findings of pneumonia |
| Mildly symptomatic patient/ history of exposure | Mild clinical symptoms [fever <38 (quelled without treatment), with or without cough, no dyspnea, no gasping, no chronic disease] No imaging findings of acute pneumonia Positive SARS-CoV-2 laboratory test or documented history of exposure to COVID-19 patient. |
| Healed patient/ Healthy individual | No fever for at least 3 days Significant improvement in chest radiologic findings and respiratory function Two consecutive negative SARS-CoV-2 laboratory test |
Priority of Orthopedic Surgical Trauma Procedures
Another concern is the severity of the trauma. Orthopedic traumas can be divided into 4 categories: Emergent Surgery (EmS), Major Urgent Orthopedic Surgery (MjOS), Minor Urgent Orthopedic Surgery (MiOS) and Delayed Trauma Surgery (DlS) [Table 2]. MjOS include procedures with possible blood loss and thromboembolism (15, 16). We assume that a delay in a more critical condition may necessitate a DlS in the future e.g neglected tendon injuries, inappropriate non-operatively treated hip and/ or acetabular fractures, established malunion, etc. However, clinical judgment is the mainstay of correct decision-making.
Table 2.
Priority of Orthopedic Surgical Procedures
| Orthopedic Surgery | Examples |
|---|---|
| Emergent life/limb threatening Surgery (EmS) | Open Fx, Dislocations, Compartment syndrome, Spine emergencies, etc. |
| Major Orthopedic Surgery (MjOS) | Acetabulum Fx, Hip Fx, Proximal Femur Fx, Major long bone Fx, Multiple long bone Fx, Spine Fx |
| Minor Orthopedic Surgery (MiOS) | Other bone Fx, Tendon injury, Nerve injury |
| Delayed Trauma Surgery (DlS) | Neglected or delayed orthopedic surgery |
Standard of Care for the Treatment of Trauma Injuries
1. Non-Surgical Management (NSM): Whilst the decision on anesthesia is the concern of the anesthesiology team, we should consider that the risk assessment is an aggregate of the real risk of proceeding a procedure (including expected blood loss, activation of inflammatory cascades and underlying comorbidities) and the real risk of upcoming disability and anticipated complex surgeries in the future if the operation is postponed. Given the shortage of resources, the risk to medical staff and the risk of in-hospital infection for patient and family members, the crisis must be considered as a relative indication for non-operative treatment whenever it seems reasonable.
2. Damage Control Orthopedics (DCO): Providing the patient with a temporary stabilization, especially in MjOS, before ICU admission helps reduce pain, minimizes secondary soft tissue damage due to the release of intramedullary materials and inhibits fat embolism.
3. Definitive Orthopedic Management (DOM): Regarding the emerging conditions, COVID-19 negative patients may receive the required services under the rules of “same day surgery” and “early safe discharge” to reduce the risk of in-hospital infection for either the patient, patient companion or medical staff. For this reason, optimized urgent pre-operative preparations for all patients is required, the surgeries must be performed by the highest rank surgeon, the patient is operated within 24 hours of admission in the emergency department and safely discharged within 24 hours after the surgery, if feasible (17). For known cases of COVID-19, DOM must be seen in the context of the disease status. Besides, safe operating room protection protocols must be respected and isolation at discharge must be in concordance of infectious disease counterparts. Delayed surgical management of patients with malunion after primary non-operative treatment also applies in this context.
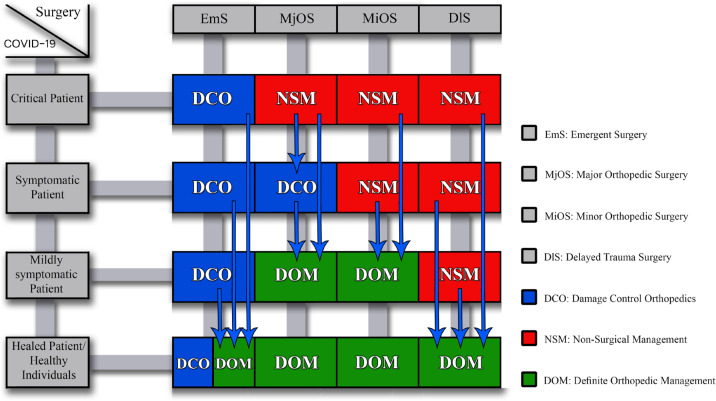
As decision-making is a dynamic process, we propose a 4×4 table to actively weigh the risks and benefits of the procedures and choose between NSM, DCO or DOM in accordance with the disease status [Figure 1]. If we consider red for NSM, green for DOM and blue for DCO, the COVID-19 negative patients are green as they receive the routine service considering the rules “same day surgery” and “early safe discharge”, unless they are in emergent condition needing DCO. COVID-19 patients with emergent life or limb threatening trauma are treated according to DCO. We consider COVID-19 crisis a relative indication for DCO compared with early total care to lower the risk of infection transmission and inhibit pneumonia exacerbation by prolonged anesthesia and blood loss. In this case, healed or healthy patients may benefit from early total care and DOM as in non-crisis days. In MjOS, DCO best applies to those with higher cumulative risk and DOM to low risk individuals while NSM is the optimal decision in critically ill patients. Blue arrows indicate that a close observation of the improvement in the disease status may lead to step down in a new box below until achieving the correct trauma management. Regarding the scarce resources during the crisis, the risk of infection transmission to health care providers and patient safety considerations, it seems logical to apply NSM to MiOS in symptomatic or critical patients. However, DOM in mildly symptomatic patients who tolerate anesthesia will decrease hospital stay, prevent future complications and lessen the risk of in-hospital transmission to the staff and family members. Whether we like it or not, we, as the orthopedic surgeons, are in the middle of the battle to pay our share and we must encounter COVID-19 patients in the operating rooms with proper personal protective equipment. Meanwhile we suggest DlS must be postponed until full COVID-19 healing.
Figure 1.
Decision-making algorithm as a dynamic process to weigh the risks and the benefits of the procedures and choose between NSM (red), DCO (blue) or DOM (green); the blue arrows indicate one may step down in a new box below by disease improvement until achieving the correct trauma management
We encourage orthopedic surgeons to implement a dynamic decision-making process in collaboration with our anesthesiologist colleagues, taking into account the algorithm introduced here to weigh the risks and benefits of proceeding or postponing the trauma surgeries. Meanwhile, it is the responsibility of the orthopedic society to report the follow-up outcome of the patients in terms of developing COVID-19 infection, the flare-up of the disease in COVID-19 patients undergone surgery and the future costs and benefits of the patients treated non-operatively or in a delayed manner. These data are required to help mitigating SARS-CoV-2 virus crisis.
Disclosure:
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Dr Mohammadzadeh, Dr Mirmansouri and Dr Yekta, anesthesiologists and Dr Fariba Asghar, for their kind discussion in raising and cultivating the issue.
Our best wishes to Sadegh Haghsheno, Graphic Designer, and Kaveh Boveiri, Proofreader, for their generous support.
References
- 1.World Health Organization. Coronavirus disease (COVID-2019) situation reports. 2020. Available at: URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.McCloskey B, Zumla A, Ippolito G, Blumberg L, Arbon P, Cicero A, et al. Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. Lancet. 2020;395(10230):1096–9. doi: 10.1016/S0140-6736(20)30681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48(2):155–63. doi: 10.1007/s15010-020-01401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong KC, Leung KS, Hui M. Severe acute respiratory syndrome (SARS) in a geriatric patient with a hip fracture A case report. J Bone Joint Surg Am. 2003;85(7):1339–42. doi: 10.2106/00004623-200307000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Fang D. SARS: facts and considerations for the orthopaedic community. J Orthop Surg (Hong Kong) 2003;11(1):3–5. doi: 10.1177/230949900301100102. [DOI] [PubMed] [Google Scholar]
- 6.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01620-9. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gray AC, White TO, Clutton E, Christie J, Hawes BD, Robinson CM. The stress response to bilateral femoral fractures: a comparison of primary intramedullary nailing and external fixation. J Orthop Trauma. 2009;23(2):90–7. doi: 10.1097/BOT.0b013e31819194c6. [DOI] [PubMed] [Google Scholar]
- 11.Lefaivre KA, Starr AJ, Stahel PF, Elliott AC, Smith WR. Prediction of pulmonary morbidity and mortality in patients with femur fracture. J Trauma. 2010;69(6):1527–35. doi: 10.1097/TA.0b013e3181f8fa3b. [DOI] [PubMed] [Google Scholar]
- 12.Steinhausen E, Lefering R, Tjardes T, Neugebauer EA, Bouillon B, Rixen D, et al. A risk-adapted approach is beneficial in the management of bilateral femoral shaft fractures in multiple trauma patients: an analysis based on the trauma registry of the German Trauma Society. J Trauma Acute Care Surg. 2014;76(5):1288–93. doi: 10.1097/TA.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 13.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020;21:200490. doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sen RK, Tripathy SK, Singh AK. Is routine thromboprophylaxis justified among Indian patients sustaining major orthopedic trauma? A systematic review. Indian J Orthop. 2011;45(3):197–207. doi: 10.4103/0019-5413.80037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khak M, Hakimi H, Manafi Rasi A. Damage Control Orthopedics in Multitrauma Patients: A Pediatric Case Presentation and Literature Review. Trauma Monthly. 2017;22(3):e32856. [Google Scholar]
- 17.Tahmasebi MN, Nabian MH. How to Continue Essential Orthopedic Services during COVID-19 Crisis? The Archives of Bone and Joint Surgery. 2020;8(Covid-19 Special Issue):295–6. doi: 10.22038/abjs.2020.47790.2353. [DOI] [PMC free article] [PubMed] [Google Scholar]