Abstract
A quarter of 400 million urban Indian residents are poor. Urban poor women are as undernourished as or worse than rural women but urban averages mask this disparity. We present the spectrum of malnutrition and their determinants for more than 26,000 urban women who gave birth within 5 years from the last two rounds of Demographic Health Survey 2006 and 2016. Among urban mothers in the lowest quartile by wealth index (urban poor), 12.8% (95% CI [11.3%, 14.5%]) were short or with height < 145 cm; 20.6% (95% CI [19%, 22.3%]) were thin or with body mass index < 18.5 kg/m2; 57.4% (95% CI [55.5%, 59.3%]) had any anaemia (haemoglobin < 12 g/dL), whereas 32.4% (95% CI [30.5%, 34.3%]) had moderate to severe anaemia; and 21.1% (95% CI [19.3%, 23%]) were obese (body mass index ≥ 25 kg/m2). Decadal gains were significant for thinness reduction (17p.p.) but obesity increased by 12 p.p. Belonging to a tribal household increased odds of thinness by 1.5 (95% CI [1.06, 2.18]) times among urban poor mothers compared with other socially vulnerable groups. Secondary education reduced odds of thinness (0.61; 95% CI [0.48, 0.77]) and higher education of short stature (0.41; 95% CI [0.18, 0.940]). Consuming milk/milk products, pulses/beans/eggs/meats, and dark green leafy vegetables daily reduced the odds of short stature (0.52; 95% CI [0.35, 0.78]) and thinness (0.72; 95% CI [0.54, 0.98]). Urban poor mothers should be screened for nutritional risks due to the high prevalence of all forms of malnutrition and counselled or treated as per risk.
Keywords: anaemia, double burden, obesity, short stature, thinness, urban poor, urban women
Key messages
A fifth of the urban poor mothers are either thin or obese.
Obesity increased by 2.5 times among urban poor mothers from 2005–2006 to 2015–2016.
Among modifiable factors, daily consumption of milk (milk products), pulses/beans or eggs/meat, and dark green leafy vegetables emerged as a key influencer for reducing both short stature and thinness among urban poor mothers.
Being younger than 24 years, belonging to tribal households, and low education (<1 year) increased the odds of thinness among urban poor mothers.
Anaemia was prevalent across wealth quartiles consistently.
1. INTRODUCTION
Inclusive and sustainable urbanization is a key outcome in the 2030 Agenda for Sustainable Development (Sustainable Development, 2015). India has been experiencing rapid urbanization, and 34% of the population now lives in urban areas (United Nations, 2018). The 2012 Lancet Commission Shaping Cities for Health highlighted the health concerns and inequalities in urban environments (Rydin et al., 2012). The “triple burden” of malnutrition—undernutrition, micronutrient deficiencies, and overweight and obesity—is becoming a considerable public health concern in these environments (Global Panel, 2017). The urban poor are as disadvantaged as the rural poor with respect to nutrition outcomes (Menon, Ruel, & Morris, 2000; Poel, O'Donnell & Doorslaer, 2007).
Although these concerns are well‐recognized, the use of rural‐urban average comparisons in nutrition policy discourse, has skewed more emphasis on the rural populace, given that in “averages” the urban estimates of nutrition status are better than rural (Elsey & Agarwal, 2016; Save the Children, 2015; UNICEF, 2012; UNICEF, 2018). For instance, the most recent round of Demographic Health Survey (DHS) 2015–2016 estimates prevalence of thinness (body mass index [BMI] < 18.5 kg/m2) among rural Indian women (15 to 49 years) at 26.8% and among urban Indian women of the same age at 15.5% (IIPS & Macro International, 2015; IIPS & Macro International, 2005). Furthermore, the continued use of urban average data masks the intra‐urban disparities and has adversely affected the design of targeted response for the urban poor population in India's flagship nutrition initiatives. In fact, urban poor disaggregated data is not publicly available at state/region/ward levels. India's flagship nutrition programmes of two departments—Women and Child Development (Integrated Child Development Services, ICDS) and Health (National Health Mission)—does not provide disaggregated service delivery and utilization information for urban areas (Agarwal, 2011; Agarwal, Satyavarda, Kaushik, & Kumar, 2007; Hazarika, 2009). Compounding these challenges is the fact that basic information on what nutrition problems exist and the patterns of socioeconomic inequalities is not known. The factors associated with these problems are also uncertain and not well understood. Establishing these determinants is important for informing public policy dialogue and development of targeted approaches to improve the nutritional status of urban populations.
According to official national estimates of urban poverty, 25.6% or 102.5 million of India's urban population is classified as “poor” (Ministry of Home Affairs, 2011; Planning Commission, 2014). Per‐capita expenditure of 47 per day (0.66 USD) rupees in urban areas (at 2004–2005 prices) is the official poverty line for urban areas in India (Planning Commission, 2011b). The number of urban poor increased from 80 million in 2004–2005 to over 100 million in 2014–2015, and is projected to continue to rise (Ministry of Home Affairs, 2011; Planning Commission, 2011a). Urban poor habitations—slums and similar underserved settlements—are characterized by overcrowding, environmental pollution, and lack of or inadequate access to basic water, sanitation, health, and nutrition services (Ministry of Housing and Urban Poverty Alleviation, 2015). Populations living in non‐notified slums are even more vulnerable as these settlements are not recognized by authorities and, hence, usually remain outside the purview of health, nutrition, food subsidy, and other civic services (Agarwal & Taneja, 2005).
Women in particular are disproportionally affected by urban inequities due to increased vulnerabilities owing to unequal and meagre wages, involvement in strenuous manual work in informal/unorganized sector increasing exposure to violence and financial risks, wage losses during maternity breaks, and limited involvement in household decision making (Loughhead, Mittal, & Wood, 2001; Save the Children, 2015). Furthermore, when women experience increased nutritional vulnerability during pregnancy and the post‐natal period, they are seldom under the reach of public supplementary nutrition programmes under ICDS, have no household food subsidies due to their illegal status and have limited contact with health service providers in urban poor settings (Agarwal & Sethi, 2013; Black et al., 2013; Gaur, Keshri, & Joe, 2017). Urban poor women have unfavourable diets and are less physically active compared with rural women and urban poor men (Anand et al., 2007; Jayamani et al., 2013). Women with no access to private sanitation facility alter their eating pattern to regulate time for defecation, which adversely affects nutrient intake and absorption (We are Water Foundation, 2017).
A reanalysis of the 2005–2006 DHS (commonly referred to as National Family Health Survey‐NFHS) revealed 1.5 to 1.8 times higher prevalence of thinness, short stature, and moderate to severe anaemia among urban poor women compared with urban averages for women (Agarwal & Sethi, 2013). These disparities have been noted by other researchers too (Gaur et al., 2017; Gouda & Prusty, 2014; Swaminathan & Mukherji, 2012; Table 1).
Table 1.
Research on nutritional status and its determinants among urban women using large scale data sets in last decade, India
| Author/s | Year of publication | Sample size | Data, poverty | Key findings | Reference |
|---|---|---|---|---|---|
| Gouda J, Prusty RJ | 2014 | 50,639 (15–49 years, ever married) | DHS‐3a (Percentile distribution based on wealth index) | Non‐poor women had 2–3 times increased risk of obesity compared with poor. | Kumar, 2015 |
| In addition to socioeconomic correlates, media exposure increased risk of overweight and obesity by 1.5 to 1.6 times (both poor and non‐poor) | |||||
| Agarwal S, Sethi V | 2013 | 10,626 (15–49 years, delivered in the last 5 years) | DHS‐3 (Wealth index–based quartiles) | Proportion thin, short stature, and with moderate to severe anaemia was 1.5, 1.5, and 1.3 times higher among urban poor compared with urban average | Jerath, Devansenapathy, Singh, Shankar, & Zodpey, 2015 |
| Gaur K et al | 2013 | 19,448 (15–49 years) | DHS 3 (Wealth index based on city specific assets) | Prevalence of thinness among poorest quintile three times higher than the richest quintile (both slum and non‐slum dwellers) | Jayamani et al., 2013 |
| Equal proportion of thin and overweight women in slums (23%–24%) | |||||
| Place of residence as such has no significant impact on urban women's nutritional status; the association is a result of other socioeconomic correlates. Urban nutrition plans should focus on prevention and management of both thinness and overweight. | |||||
| Swaminathan A, Mukherji H | 2012 | 14,927 (15–49 years) | DHS‐3 (Census and DHS slum classifications) | Women in slums were 1.3 times more likely to be thin and 0.78 times less likely to be overweight, than non‐slum | Loughhead et al., 2001 |
| The relative odds of being thin compared with being normal weight was reduced by 6% as the number of food groups consumed weekly or daily increased. |
DHS Demographic Health Survey. DHS‐3 is the third round of the country‐wide family health survey completed and released in 2005‐2006.
However, updated national and state‐level prevalence estimates and trends on the maternal (women who delivered in the last 5 years) nutrition situation among urban poor in India is currently not available. The biological, dietary, social, and programmatic factors related to maternal services associated with thinness, anaemia, and obesity among urban poor women are also unknown. Our primary aim was to determine the levels and trends of different forms of malnutrition (short stature, thinness, anaemia, and obesity) among urban poor women in India and its associations with dietary, social, and programmatic factors. A secondary aim was to examine socioeconomic inequalities in different forms of malnutrition (short stature, thinness, anaemia, and obesity) in the urban population.
2. METHODS
2.1. Sample
Data from two rounds of DHS conducted during 2005–2006 (DHS‐3) and 2015–2016 (DHS‐4) were used in this study (IIPS & Macro International, [Link]; IIPS & Macro International, [Link]). The DHS 2005–2006 and 2015–2016 collected information from a nationally representative probability sample covering 54,808 and 198,708 urban women in the age group of 15–49 years across India. Women less than 18 years and who were currently pregnant were excluded from the sample due to the likelihood of misclassification based on BMI cut‐offs (Institute of Medicine, 2009). Details of the DHS 2005–2006 and 2015–2016 survey design and overall findings are available elsewhere (IIPS & Macro International, 2015; IIPS & Macro International, 2005). Women who delivered between 2 to less than 5 years and for whom anthropometric and biochemical data were available were included in the analytical sample to assess nutritional status of mothers in urban settings. After applying the criteria of delivery in the last 5 years, no women of ages 18 and 19 appeared in the sample. Thus, the unweighted sample included 5,458 and 20,876 urban mothers for DHS‐3 and DHS‐4, respectively (Figure 1).
Figure 1.
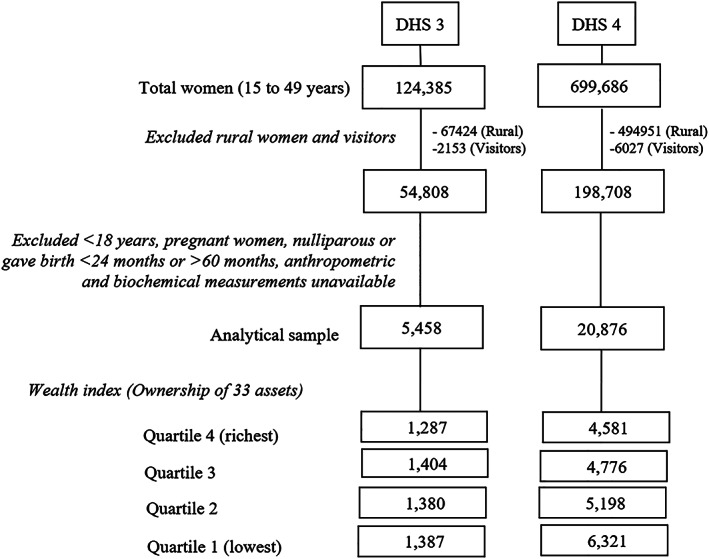
Sampling flow chart, Demographic Health Survey (DHS)‐3 and DHS‐4
2.2. Defining urban poverty
In our study, the urban analytical sample was segregated into quartiles; the lowest quartile representative of urban poor (Figure 1) in accordance with asset linked wealth index classification, which is used by the DHS for economic disaggregation. The quartile analysis for wealth index is relevant for urban India as there is variability in poverty estimates ranging from 25.7% to 29% (Planning Commission, 2011a). There are concerns of misclassification of the poor especially in rural population groups due to the urban bias of this index. However, for this urban subsample, a normal distribution was observed when the post application of the wealth index was conducted (Figure [Link]; Rutstein, 2008).
2.3. Independent variables
The independent variables included age divided into 4‐year age groups (20–24, 25–29, 30–34, and >34 years); age at marriage less than, equal, or greater than the legal age of 18 years; parity (1/2/3 or more) education segregated into four categories (no education, primary, secondary, and higher); religion (Hindu/Muslim/others); ethnicity (scheduled caste/scheduled tribe/other backward classes/general); type of employment (unemployed/professional/manual/others); owning a below poverty line (BPL) card; access to money; use of maternal and reproductive health services; and access to sanitation facility, which have been used by other researchers. Other important nutrition variables included daily consumption of milk or curd, pulses or beans, and dark green leafy vegetables and weekly consumption of fried foods and aerated drinks (National Institute of Nutrition, 2011). Cereal, starchy foods, and sugar intake could not be included in the analysis as these are not measured under DHS.
2.4. Outcomes
Six outcomes were investigated to determine prevalence of malnutrition among urban mothers—short stature, thinness, severe thinness, overweight, obesity, and moderate or severe anaemia. In DHS, height was measured using Seca 213 stadiometer and weight using Seca 874 digital scale. Height less than 145 cm, recognized as an indicator for nutritional risk among women of reproductive age was used as cut‐off for short stature (World Health Organization, 1995). Maternal nutritional status was classified according to BMI categories as thinness (<18.5 kg/m2), severe thinness (<16 kg/m2), overweight (23 to 24.9 kg/m2), and obesity (≥25 kg/m2; Misra et al., 2009). Blood samples were drawn from a drop of blood taken from a finger prick and collected in a microcuvette. Haemoglobin analysis was conducted on‐site with a battery‐operated portable HemoCue Hb 201+ analyser. The World Health Organization cut‐off of blood haemoglobin levels of <12 g/dL was used for classifying any anaemia and <11 g/dL for moderate or severe anaemia among nonpregnant women (World Health Organization, 1989). Co‐burden of thinness and anaemia (BMI < 18.5 kg/m2 and haemoglobin < 12 g/dL), thinness and short stature (BMI < 18.5 kg/m2 and height < 145 cm), overweight or obesity and anaemia (BMI > 23 kg/m2 and haemoglobin < 12 g/dL), and the former with short stature (BMI > 23 kg/m2 and height < 145 cm) was also investigated.
2.5. Data analysis
Bivariate analysis was used to assess socioeconomic inequalities in the prevalence of maternal malnutrition (short stature, thinness, severe thinness, overweight, obesity, moderate or severe anaemia, and co‐burden of malnutrition) among urban poor and average estimates for all urban mothers for both rounds of DHS survey. Chi‐squared test (χ 2 test) was used to determine inequity in the prevalence of malnutrition and double burden of malnutrition between the lowest quartile by wealth index (urban poor) and each of the three higher quartiles by wealth index for both rounds of DHS survey. We also estimated percentage point (p.p.) decline in prevalence of various forms of malnutrition between the two rounds of DHS survey for urban poor mothers. Further, using urban poor sample of DHS‐4, we used binary logistic regression analysis to assess the strength of association of dietary, social, and programmatic factors with the odds of maternal short stature, thinness, obesity, and moderate to severe anaemia adjusting for other covariates with 95% confidence interval (CI) and using a significance level of <.05. The selection of factors was based on earlier published research as well as authors' programme experiences (Agarwal & Sethi, 2013, Gaur, Keshri & Joe, 2017; Gouda & Prusty, 2014; Swaminathan & Mukherji, 2012). To maximize the representativeness of the sample of the study population, national level women's sampling weights were used in the analysis to compensate for the possible oversampling or undersampling of groups of respondents. All analysis was done using STATA 14 software.
2.6. Limitations
As the study used cross‐sectional survey, it cannot assess causality in the relationships of interest. We are unable to account for the effects of seasonality on BMI of mothers. Weight for height is known to vary seasonally in young children and could potentially vary for adults too (Egata, Berhane, & Worku, 2013; Singla et al., 2016). A wider range of risk factors for obesity such as level of physical activity and daily consumption of cereals, roots/tubers, sugars, and fats/oils were not investigated in this study as these are not measured in DHS surveys.
2.7. Ethical considerations
This research involved no direct contact with human or animal subjects. It is based on reanalysis of Demographic Health Survey data published in 2015–2016.
3. RESULTS
3.1. Characteristics of the sample population
Table 2 shows the demographic and socioeconomic characteristics of women included in the sample. Among this sample of 5,458 urban women in DHS‐3 and 20,876 urban women in DHS‐4, 25% (1,387) and 30% (6,321) were in the lowest quartile by wealth index or poor. A higher proportion of women were married before the age 18 years among urban poor compared with urban average (68% versus 45%, DHS‐3; 49.3% versus 31.2%, DHS‐4). A quarter or more of the mothers among the urban poor were from scheduled caste households compared with 17% to 18% among all urban mothers. Despite being in the lowest quartile by wealth index, less than 30% in DHS‐3 and less than 40% in DHS‐4 had a BPL card—a mandatory document for availing several social safety net entitlements. A higher proportion of urban poor mothers had three or more children compared with urban average (60.6% versus 37.7%, DHS‐3; 43.5% versus 26.2%, DHS‐4). Secondary or higher education was low at 53% among urban average and 45% among urban poor mothers in DHS‐4, but the latter improved from DHS‐3 levels of 26%. Urban mothers were largely unemployed and a corresponding proportion is observed among the urban average. In comparison with the urban averages, a lower proportion of urban poor mothers had access to money, bank accounts and information on microcredit schemes. About 60% urban poor mothers had access to sanitation facility at home compared with 88% among average urban mothers in DHS 4 (Table 2).
Table 2.
Individual and household characteristics of mothers (20–49 years) in urban India, DHS‐3 (2005–2006) and DHS‐4 (2015–2016)
| Total number of women (N) | DHS 3 | DHS 4 | ||
|---|---|---|---|---|
| Urban poor | Urban average | Urban poor | Urban average | |
| 1,387 | 5,458 | 6,321 | 20,876 | |
| n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | |
| Age (years) | ||||
| 20–24 | 333 (23 [23.0, 23.0]) | 1,015 (20.3 [20.3, 20.3]) | 1,178 (21.1[19.4, 22.9]) | 3,165 (16.4 [15.5, 17.3]) |
| 25–29 | 520 (37.8 [37.8, 37.8]) | 2,155 (40.6 [40.6, 40.6]) | 2,484 (40.7 [38.7, 42.8]) | 8,292 (42.2 [41.0, 43.4]) |
| 30–34 | 312 (22.9 [22.9, 22.9]) | 1,517 (26 [26.0, 26.0]) | 1,567 (24.2 [22.5, 25.9]) | 5,974 (28 [27.0, 29.1]) |
| >34 | 222 (16.3 [16.3, 16.3]) | 771 (13 [13.0, 13.0]) | 1,092 (14 [12.6, 15.5]) | 3,445 (13.4 [12.7, 14.3]) |
| Age at marriage | ||||
| <18 years | 880 (68 [68.0, 68.0]) | 2,213 (45.3 [45.3, 45.3]) | 2,895 (49.3 [47.0, 51.6]) | 6,309 (31.2 [29.9, 32.4]) |
| Age at first birth (median) | 19 years | 21 years | 20 years | 21 years |
| Religion of the head of the household | ||||
| Hindu | 971 (73.6 [73.6, 73.6]) | 3,954 (76.5 [76.5, 76.5]) | 4,145 (70 [67.3, 72.5]) | 14,303 (74 [72.5, 75.4]) |
| Muslim | 300 (21.9 [21.9, 21.9]) | 918 (17.3[17.3, 17.3]) | 1,404 (25.8 [23.3, 28.5]) | 4,011 (20 [18.7, 21.5]) |
| Other | 116 (4.4 [4.4, 4.4]) | 586 (6.2 [6.2, 6.2]) | 772 (4.2 [3.3, 5.3]) | 2,562 (6 [5.3, 6.7]) |
| Ethnicity of the head of the household | ||||
| Schedule caste (SC) | 352 (26.4 [26.4, 26.4]) | 840 (16.9 [16.9, 16.9]) | 1,406 (25.7 [23.4, 28.1]) | 3,302 (17.5 [16.3, 18.8]) |
| Schedule tribe (ST) | 117 (4.5 [4.5, 4.5]) | 378 (3.0 [3.0, 3.0]) | 1,020 (6.7 [5.8, 7.7]) | 2,554 (4.4 [3.9, 5.0]) |
| Other backward classes (OBC) | 492 (44.9 [44.9, 44.9]) | 1,726 (38.7 [38.7, 38.7]) | 2,522 (41.1 [38.8, 43.4]) | 8,635 (43.7 [42.2, 45.1]) |
| General/others | 426 (24.2 [24.2, 24.2]) | 2,514 (41.4 [41.4, 41.4]) | 1,373 (26.6 [24.0, 29.3]) | 6,385 (34.4 [33.0, 35.9]) |
| BPL card holder | 322 (28.8 [28.8, 28.8]) | 691 (16.2 [16.2, 16.2]) | 2,312 (36 [34.0, 38.1]) | 5,055 (25.2 [23.9, 26.5]) |
| Parity | ||||
| 1 | 207 (13.1 [13.1, 13.1]) | 1,416 (24.1 [24.1, 24.1]) | 1,338 (20.7 [19.0, 22.5]) | 6,400 (32.8 [31.7, 33.9]) |
| 2 | 361 (26.3 [26.3, 26.3]) | 2,011 (38.1 [38.1, 38.1]) | 2,083 (35.7 [33.8, 37.7]) | 8,139 (41 [39.8, 42.2]) |
| 3 or more | 819 (60.6 [60.6, 60.6]) | 2,031 (37.8 [37.8, 37.8]) | 2,900 (43.5 [41.5, 45.6]) | 6,337 (26.2 [25.1, 27.3]) |
| Educational attainment | ||||
| No education | 724 (55.1 [55.1, 55.1]) | 1,208 (24.7 [24.7, 24.7]) | 2,059 (32.2 [30.3, 34.2]) | 3,077 (13.1[12.4, 13.9]) |
| Primary (1 to 5 years) | 253 (18.2 [18.2, 18.2]) | 640 (12.1 [12.1, 12.1]) | 1,160 (19.6 [17.7, 21.6]) | 2,096 (9.3 [8.6, 10.1]) |
| Secondary/Higher (6 to 10 years) | 399 (26.2 [26.2, 26.2]) | 2,575 (46.7 [46.7, 46.7]) | 2,887 (44.5 [42.2, 46.8]) | 11,081 (53.4 [52.0, 54.8]) |
| College (10+ years) | 11 (0.5 [0.5, 0.5]) | 1,035 (16.5 [16.5, 16.5]) | 215 (3.7 [3.0, 4.6]) | 4,622 (24.1 [22.9, 25.4]) |
| Work in last 12 months | ||||
| Unemployed/don't know | 833 (62.8 [62.8, 62.8]) | 3,910 (74 [74.0, 74.0]) | 6,025 (95.6 [94.7, 96.4]) | 20,112 (96.5 [96.0, 97.0]) |
| Professional/technical/managerial/clerical | 10 (0.2 [0.2, 0.2]) | 371 (5.5 [5.5, 5.5]) | 17 (0.3 [0.2, 0.5]) | 187 (1 [0.7, 1.3]) |
| Manual—skilled and unskilled | 221 (16.3 [16.3, 16.3]) | 521 (9.9 [9.9, 9.9]) | 116 (1.9 [1.4, 2.7]) | 237 (1.2 [1.0, 1.6]) |
| Others | 323 (20.7 [20.7, 20.7]) | 656 (10.6 [10.6, 10.6]) | 163 (2.2 [1.7, 2.8]) | 340 (1.3 [1.1, 1.5]) |
| Access to moneya | ||||
| Have money they can decide how to use | 521 (43.9 [43.9, 43.9]) | 2,339 (53 [53.0, 53.0]) | 386 (47.4 [47.4, 47.4]) | 1,466 (51.6 [48.5, 54.7]) |
| Have bank account | 83 (7.4 [7.4, 7.4]) | 1,111 (25.1 [25.1, 25.1]) | 417 (45.3 [45.3, 45.3]) | 1,843 (61.5 [58.5, 64.4]) |
| Are aware of microcredit programmes | 439 (37.3 [37.3, 37.3]) | 1,924 (45.7 [45.7, 45.7]) | 348 (39.6 [39.6, 39.6]) | 1,291 (47.1 [44.1, 50.2]) |
| Access to WASH services | ||||
| Improved source of drinking water supply | 1,201 (92.1 [92.1, 92.1]) | 5,014 (94.4 [94.4, 94.4]) | 5,500 (91.5 [90.1, 92.7]) | 18,774 (90.4 [89.0, 91.6]) |
| Improved sanitation facility at home | 719 (45.1 [45.1, 45.1]) | 4,637 (81.5 [81.5, 81.5]) | 3,889 (62.4 [60.1, 64.7]) | 18,095 (88.2 [87.3, 89.1]) |
Includes women responding to queries on domestic violence related themes (NFHS 3: 935 poor urban & 3031 urban aggregate & NFHS 4: 935 poor urban & 3031 urban aggregate)
3.2. Prevalence of malnutrition among urban women across wealth index–based quartiles
As per DHS‐4 (2015–2016), among urban poor mothers, 12.8% were short, 20.6% were thin (3.5% being severely thin), 13.7% were overweight, 21.1% were obese, 57.4% had any anaemia, and 32.4% had moderate to severe anaemia. Prevalence of short stature was 4.4 p.p. higher among urban poor mothers compared with the average (all urban mothers); thinness was 8.5 p.p. higher; and moderate to severe anaemia was 4 p.p. higher. In contrast, prevalence of obesity was higher among all urban mothers or averages compared with urban poor mothers by 11 p.p. (Table 3). Prevalence of short stature, thinness, and anaemia was highest among urban poor mothers compared with any other higher wealth quartile. Among urban poor mothers, the estimated double burden of thinness and anaemia was 12.8%, overweight/obesity and anaemia was 18.5%, thinness and short stature was 2.7%, and overweight/obesity and short stature was 4.5% (Table 3). Proportion with double burden of thinness and anaemia and thinness and short stature were highest among urban poor mothers compared with any other higher wealth quartile.
Table 3.
Prevalence of different forms of malnutrition and trends among mothers (20–49 years) in urban India, DHS‐3 (2005‐2006) and DHS‐4 (2015‐2016)a
| Wealth quartile N | DHS‐3 | DHS‐4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 (poor) | 2 | 3 | 4 (richest) | AVG | 1 (poor) | 2 | 3 | 4 (richest) | AVG | |
| 1,387 | 1,380 | 1,404 | 1,287 | 5,458 | 6,321 | 5,198 | 4,776 | 4,581 | 2,0876 | |
| n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | n (% [CI]) | |
| Short stature (Height < 145 cm) | 202 (14.5 [12.1, 17.4]) | 132 (10.8 [8.6, 13.4]) | 107 (7.3 [5.6, 9.4]) | 44 (3.8 [2.5, 5.6]) | 485 (9.5 [8.4, 10.70]) | 787 (12.8 [11.3, 14.5]) | 425 (9.9 [8.2, 11.9]) | 232 (6.3 [4.8, 8.3]) | 180 (3.9 [3.2, 4.9]) | 1,624 (8.4 [7.6, 9.4]) |
| Thinness (BMI < 18.5) | 504 (37.2 [33.8, 40.8]) | 322 (25.5 [22.1, 29.3]) | 228 (19 [16.2, 22.1]) | 122 (9.5 [7.3, 12.3]) | 1176 (23.8 [22.1, 25.6]) | 1281 (20.6 [19.0, 22.3]) | 640 (11.9 [10.6, 13.3]) | 405 (8.7 [7.5, 10.1]) | 258 (6.2 [5.1, 7.6]) | 2,584 (12.1 [11.4, 12.9]) |
| Severe thinness (BMI < 16) | 93 (7.3 [5.8, 9.3]) | 66 (5.6 [4.1, 7.7]) | 38 (3.2 [2.1, 4.9]) | 23 (1.5 [0.8, 2.8]) | 220 (4.6 [3.9, 5.5]) | 206 (3.5 [2.9, 4.2]) | 89 (1.9 [1.3, 3.0]) | 53 (1.4 [0.9, 2.1]) | 36 (0.7 [0.5, 1.1]) | 384 (1.9 [1.6, 2.3]) |
| Overweight (BMI 23–24.9) | 110 (8.4 [6.5, 10.9]) | 172 (11.1 [9.1, 13.6]) | 220 (15.1 [12.5, 18.2]) | 238 (20 [17.1, 23.3]) | 740 (13.3 [12.0, 14.7]) | 855 (13.7 [12.3, 15.2]) | 849 (15.8 [14.2, 17.7]) | 856 (17.8 [15.7, 20.1]) | 870 (18.6 [16.8, 20.6]) | 3,430 (16.4 [15.5, 17.3]) |
| Obese (BMI ≥ 25) | 122 (8.8 [6.6, 10.7]) | 267 (18 [15.5, 20.8]) | 392 (30 [26.6, 33.7]) | 486 (38.6 [34.6, 42.8]) | 1,267 (22.7 [21.0, 24.4]) | 1,214 (21.1 [19.3, 23.0]) | 1,571 (31.3 [29.1, 33.6]) | 1,735 (38.8 [35.8, 42.0]) | 1,801 (38.9 [36.5, 41.3]) | 6,321 (32.2 [31.0, 33.4]) |
| Anaemia | ||||||||||
| Any anaemia (Hb < 12 g/dL) | 783 (60 [56.3, 63.6]) | 709 (53.3 [49.3, 57.4]) | 664 (47.4 [43.7, 51.2]) | 540 (43.1 [39.2, 47.2]) | 2,696 (51.6 [49.6, 53.5]) | 3,375 (57.4 [55.5, 59.3]) | 2,518 (51.2 [48.6, 53.8]) | 2,323 (51.3 [48.8, 53.8]) | 2,246 (49.8 [47.4, 52.2]) | 10,462 (52.5 [51.3, 53.8]) |
| Moderate to severe (Hb < 11 g/dL) | 443 (35.3 [31.7, 39.1]) | 370 (27.8 [24.4, 31.4]) | 359 (27.8 [24.5, 31.4]) | 261 (21.9 [18.7, 25.5]) | 1,433 (28.7 [26.9, 30.5]) | 1,864 (32.4 [30.5, 34.3]) | 1,332 (28.1 [25.6, 30.8]) | 1,204 (27.8 [25.6, 30.1]) | 1,160 (25 [23.0, 27.1]) | 5,560 (28.4 [27.3, 29.6]) |
| Co‐burden | ||||||||||
| Underweight and any anaemia | 302 (24 [21.1, 27.1]) | 195 (15.9 [13.3, 19.0]) | 116 (9.5 [7.5, 11.8]) | 57 (4.7 [3.2, 6.9]) | 670 (14.2 [12.8, 15.7]) | 785 (12.8 [11.5, 14.1]) | 362 (6.8 [5.8, 7.9]) | 210 (5.1 [4.1, 6.3]) | 134 (3 [2.4, 3.8]) | 1,491 (7.1 [6.5, 7.7]) |
| Overweight/obese and any anaemia | 114 (8.7 [6.8, 11.2]) | 188 (12.9 [10.6, 15.6]) | 262 (18.9 [16.1, 22.1]) | 306 (25.4 [22.1, 29.0]) | 870 (15.9 [14.5, 17.3]) | 966 (18.5 [16.8, 20.4]) | 1,060 (21.8 [19.9, 23.9]) | 1,219 (27.4 [25.2, 29.7]) | 1,278 (28.3 [26.3, 30.4]) | 4,523 (23.8 [22.8, 24.8]) |
| Underweight and short | 70 (5.3 [3.8, 7.2]) | 25 (2 [1.2, 3.3]) | 18 (1.1 [0.6, 2.1]) | 7 (0.5 [0.1, 1.4]) | 120 (2.4 [1.8, 3.0]) | 179 (2.7 [2.2, 3.3]) | 53 (1 [0.6, 1.6]) | 24 (0.5 [0.3, 1.0]) | 15 (0.3 [0.2, 0.6]) | 271 (1.2 [1.0, 1.4]) |
| Overweight/obese and short | 33 (2 [1.2, 3.3]) | 42 (3.1 [2.0, 4.8]) | 47 (3.9 [2.6, 5.6]) | 24 (2.2 [1.3, 3.9]) | 146 (2.8 [2.2, 3.5]) | 249 (4.3 [3.6, 5.3]) | 205 (4.8 [3.8, 6.1]) | 126 (4 [2.6, 6.0]]) | 116 (2.4 [1.8, 3.2]) | 696 (3.9 [3.4, 4.5]) |
Significant difference (χ 2 test, p < .01) in prevalence estimates between poor (lowest quartile by wealth index), compared with each of the higher quartiles except for co‐burden of overweight/obesity and short stature for both DHS‐3 and DHS‐4
3.3. Decadal change in malnutrition among urban poor women
In our sample, we estimate a 16.6‐p.p. decline in maternal thinness among urban poor women over the period of 2005–2006 and 2015–2016. However, over the same time, overweight and obesity increased by 5.3 p.p. and 12.3 p.p., respectively (Table 3). A nominal 1.6‐p.p. reduction in prevalence of short stature was observed. There was a slight improvement in the prevalence of any and moderate to severe forms of anaemia with a 2.6‐ and 2.9‐p.p. decline, respectively.
3.4. Dietary‐, sociodemographic‐, and programme‐related correlates of urban poor maternal short stature, thinness, anaemia, and obesity
Table 4 presents separate models of the assessment of independent relationships between maternal short stature, thinness, obesity, and moderate to severe anaemia with selected dietary, sociodemographic, and programmatic variables adjusting for other variables.
Table 4.
Odds of short stature (height < 145 cm), thinness (BMI < 18.5 kg/m2), obesity (BMI ≥ 25 kg/m2), and moderate to severe anaemia (Hb < 11 g/dL) among urban poor mothers (20–49 years) by selected characteristics, India
| Total | Model 1 (short stature) | Model 2 (thinness) | Model 3 (obesity) | Model 4 (moderate to severe anaemia) | ||||
|---|---|---|---|---|---|---|---|---|
| 6,321 odds ratio [95% CI] | ||||||||
| Age (years) | ||||||||
| 20–24a | ||||||||
| 25–29 | 0.82 | [0.571, 1.185] | 0.67** | [0.51, 0.89] | 1.51* | [1.08, 2.12] | 0.79 | [0.60, 1.03] |
| 30–34 | 0.92 | [0.602, 1.41] | 0.38*** | [0.26, 0.52] | 2.37*** | [1.58, 3.55] | 0.85 | [0.61, 1.19] |
| >34 | 0.87 | [0.556, 1.375] | 0.38*** | [0.25, 0.57] | 2.71*** | [1.78, 4.14] | 0.94 | [0.66, 1.35] |
| Age at marriage (<18 years) | ||||||||
| Noa | ||||||||
| Yes | 1.18 | [0.899, 1.537] | 0.97 | [0.79, 1.20] | 1.12 | [0.87, 1.43] | 0.94 | [0.77, 1.14] |
| Religion of the head of the household | ||||||||
| Hindua | ||||||||
| Muslim | 0.79 | [0.562, 1.107] | 0.76* | [0.59, 0.98] | 1.51** | [1.15, 1.99] | 0.89 | [0.69, 1.12] |
| Other | 0.71 | [0.406, 1.246] | 0.71 | [0.44, 1.14] | 0.85 | [0.51, 1.41] | 0.97 | [0.61, 1.56] |
| Ethnicity of the head of the household | ||||||||
| Schedule caste a | ||||||||
| Schedule tribe | 0.68 | [0.408, 1.123] | 1.52* | [1.06, 2.18] | 0.62* | [0.41, 0.94] | 1.05 | [0.74, 1.49] |
| Other backward classes | 0.91 | [0.689, 1.205] | 1.15 | [0.91, 1.46] | 1.07 | [0.82, 1.39] | 1.14 | [0.92, 1.42] |
| General/Others | 0.96 | [0.655, 1.411] | 1.05 | [0.78, 1.44] | 1.03 | [0.72, 1.48] | 0.99 | [0.74, 1.31] |
| BPL card holder | ||||||||
| Noa | ||||||||
| Yes | 1.01 | [0.786, 1.299] | 1.10 | [0.91, 1.33] | 0.76* | [0.61, 0.95] | 0.92 | [0.77, 1.11] |
| Parity | ||||||||
| 1a | ||||||||
| 2 | 0.73 | [0.509, 1.047] | 1.20 | [0.91, 1.59] | 1.26 | [0.92, 1.73] | 0.95 | [0.73, 1.24] |
| 3 or more | 0.79 | [0.524, 1.19] | 1.30 | [0.94, 1.79] | 0.81 | [0.57, 1.16] | 1.16 | [0.86, 1.56] |
| Educational attainment | ||||||||
| No educationa | ||||||||
| Primary | 1.04 | [0.74, 1.45] | 0.84 | [0.64, 1.11] | 1.32 | [0.95, 1.84] | 0.95 | [0.74, 1.23] |
| Secondary | 0.83 | [0.619, 1.108] | 0.61*** | [0.48, 0.77] | 2.20*** | [1.69, 2.86] | 1.03 | [0.83, 1.27] |
| Higher | 0.41* | [0.179, 0.944] | 0.94 | [0.52, 1.69] | 1.50 | [0.86, 2.63] | 0.76 | [0.43, 1.32] |
| Access to WASH services | ||||||||
| Improved source of drinking water supply | ||||||||
| Noa | ||||||||
| Yes | 1.22 | [0.804, 1.861] | 1.23 | [0.89, 1.69] | 0.93 | [0.66, 1.31] | 0.94 | [0.71, 1.25] |
| Improved sanitation facility at home | ||||||||
| Noa | ||||||||
| Yes | 0.91 | [0.697, 1.183] | 0.90 | [0.74, 1.09] | 1.33* | [1.06, 1.67] | 1.05 | [0.88, 1.26] |
| Maternal health services | ||||||||
| Consumed 100 IFA | ||||||||
| Noa | ||||||||
| Yes | 1.01 | [0.75, 1.37] | 0.91 | [0.71, 1.16] | 1.34* | [1.05, 1.71] | 1.27* | [1.03, 1.58] |
| Consumed single dose deworming | ||||||||
| Noa | ||||||||
| Yes | 0.65* | [0.456, 0.924] | 0.86 | [0.66, 1.11] | 1.10 | [0.82, 1.48] | 1.02 | [0.79, 1.32] |
| Received supplementary food from AWC | ||||||||
| Noa | ||||||||
| Yes | 1.01 | [0.763, 1.329] | 1.16 | [0.92, 1.46] | 1.10 | [0.85, 1.42] | 0.98 | [0.79, 1.20] |
| Received health and nutrition education at AWC | ||||||||
| Noa | ||||||||
| Yes | 1.34* | [1.014, 1.784] | 0.99 | [0.78, 1.26] | 1.08 | [0.83, 1.40] | 0.84 | [0.68, 1.05] |
| Dietary practices | ||||||||
| Daily milk/curd and pulses/beans (or egg/meat) and dark green leafy vegetables | ||||||||
| Noa | ||||||||
| Yes | 0.52** | [0.353, 0.778] | 0.72* | [0.54, 0.98] | 1.02 | [0.74, 1.40] | 0.96 | [0.73, 1.27] |
| Weekly fried food intake | ||||||||
| Noa | ||||||||
| Yes | 1.18 | [0.903, 1.537] | 0.89 | [0.73, 1.08] | 1.08 | [0.86, 1.35] | 0.92 | [0.76, 1.12] |
| Weekly sweetened aerated drinks intake | ||||||||
| Noa | ||||||||
| Yes | 0.75 | [0.545, 1.026] | 0.81 | [0.63, 1.03] | 1.43** | [1.09, 1.87] | 1.16 | [0.92, 1.45] |
Reference category
p < .05
p < .01
p < .001
3.5. Programme factors
Mothers having higher education had lower odds of short stature (0.41; 95% CI [0.17, 0.94]) and those with secondary education lower odds of being thin (0.61; 95% CI [0.48, 0.77]) compared with those with less than 1 year of education. Secondary education attainment increased odds of obesity among urban poor mothers (2.20; 95% CI [1.69, 2.86]), but had no influence on moderate to severe anaemia. Among maternal health services, consuming at least 100 IFA tablets was associated with increased odds of moderate to severe anaemia (1.27; 95% CI [1.03, 1.58]). Maternal deworming reduced odds of short stature (0.65; 95% CI [0.46, 0.92]). Those receiving nutrition and health education at the Anganwadi had higher odds of being short compared with those not attending these sessions (1.34; 95% CI [1.01, 1.78]). Among WASH services, access to sanitation facility at home increased the odds of obesity (1.33; 95% CI [1.06, 1.67]; Table 4).
3.6. Dietary factors
Consumption of milk/milk products, pulses/beans/egg/meats, and dark green leafy vegetables daily was associated with lower odds of short stature (0.52; 95% CI [0.35, 0.78]) and thinness (0.72; 95% CI [0.54, 0.98]). However, there were no significant associations observed with maternal obesity or anaemia. As expected, weekly intake of sweetened aerated drinks increased odds of obesity (1.43; 95% CI [1.09, 1.87]; Table 4).
3.7. Sociodemographic factors
Belonging to scheduled tribe household increased odds of thinness (1.52; 95% CI [1.06, 2.18]) and reduced that of obesity (0.62; [0.41, 0.94]) compared with belonging to scheduled caste household. Belonging to a Muslim household had the opposite effect and it increased the odds of obesity (1.51; 95% CI [1.15, 1.99]) and reduced that of thinness compared with Hindus (0.76; 95% CI [0.59, 0.98]). Urban poor mothers belonging to a family of BPL card holder had lower odds of obesity (0.76; 95% CI [0.61, 0.95]). Increase in maternal age was associated with reduction of thinness and increase in obesity, with mothers older than 34 years having lowest odds for thinness (0.38; 95% CI [0.26, 0.52]) and highest for obesity (2.71; 95% CI [1.78, 4.14]) compared with mothers in the 20 to 24‐years age group. However, getting married at less than 18 years and parity had no association with the forms of maternal malnutrition included in the models (Table 4).
4. DISCUSSION
This study examined the prevalence and trends of different forms of malnutrition (short stature, thinness, anaemia, and obesity) among urban poor women in India in relation to their dietary‐, social‐, and programme‐related factors, adding to the limited but growing literature on maternal nutrition among the urban poor population groups. The analysis further examines the patterns of socioeconomic inequalities in maternal nutrition status (short stature, thinness, anaemia, and obesity) among the urban poor mothers.
The study has five salient findings. First, the prevalence of short stature, thinness, and anaemia among urban poor mothers was significantly higher than among mothers in the immediate next wealth quartile and remaining two higher quartiles. Second, prevalence of thinness and obesity was comparable among urban poor mothers. Third, decadal gains were significant for thinness reduction but there was little to no change in prevalence of short stature and anaemia (any form), whereas obesity increased by over 2.5 times. Fourth, belonging to tribal household increased odds of thinness among urban poor women. Fifth, daily intake of milk/milk products, pulses/beans/egg/meats, and dark green leafy vegetables emerged as a key influencer for reducing short stature and thinness among urban poor mothers, along with secondary or higher education. Also, consuming sweetened aerated drinks increased odds of obesity among urban poor mothers. We found an important gap in identifying urban poor for programme interventions; majority of urban poor mothers as per wealth index classification that we used to generate wealth quartiles did not have a BPL card, the latter being mandatory for availing many social security schemes.
These findings reinforce the need for disaggregating urban health and nutrition assessment data to reveal socioeconomic inequalities as nutritional status of urban mothers varied significantly across wealth quartiles. Disparities in nutritional status of women in reproductive age‐group have been noted by earlier researchers in India and other developing countries (Agarwal & Sethi, 2013; Gaur, Keshri & Joe, 2017; Gouda & Prusty, 2014; Khan & Kraemer, 2009; Sawminathan & Mukherji, 2012). Unlike previous studies, we investigated a wider range of nutritional status indicators that is short stature, moderate or severe anaemia, thinness, overweight, obesity, and double burden of malnutrition, and we were able to comprehensively ascertain the patterns of malnutrition and associated socioeconomic inequalities among urban mothers. Disparities were highest in prevalence of thinness with an 11‐p.p. gap in prevalence between the lowest and second lowest quartile. The high prevalence of thinness among urban poor mothers is a cause for concern in view of the birth outcome risk factors associated with women who are short, thin, anaemic, or who fail to gain adequate weight during pregnancy (Christian et al., 2013). Similarly, large differences were also noted in the socioeconomic inequalities in the prevalence of obesity. The skewed distribution of obesity has been noted in both developed and developing countries; but unlike developed countries, in developing countries, women from higher income groups are more likely to be obese than those from lower income (Corsi, Kyu, & Subramanian, 2011; Gouda & Prusty, 2014; Mendez, Monteiro, & Popkin, 2008; Popkin, 2001; Pouliou & Elliott, 2010; Uthman, 2009). Our findings supported this pattern in prevalence of obesity.
Socioeconomic variations in prevalence of short stature and anaemia across wealth quartiles were not as stark. The lesser variation in prevalence of short stature may be accounted by the overall lower prevalence of this form of undernutrition as opposed to others (highest prevalence being 13% among urban poor mothers). Nonetheless, as a marker of chronic and intergenerational undernutrition and its association with poor pregnancy outcomes, intra‐uterine growth restriction and low birth weight remain a concern for urban poor mothers (Kozuki et al., 2015; Syed & Kamathi, 2012). The persistence of anaemia across income groups explains its high contribution to disability adjusted life years in India (Harding, Aguayo, & Webb, 2018). Anaemia prevalence as high as 97% has been reported among slum‐dwelling women who gave birth recently (Jerath, Devansenapathy, Singh, Shankar & Zodpey, 2015). In a study covering all women sample of DHS‐4, among nonpregnant women, 23% were reported to have both anaemia (any) and thinness (Nguyen, Scott, Avula, Tran, & Menon, 2018). In our urban sample, we estimated double burden of moderate to severe anaemia and thinness at 18% among all urban mothers and 23% among urban poor mothers.
We investigated the determinants of short stature, thinness, obesity, and moderate to severe anaemia among urban poor mothers using a controlled model. Diet emerged as a key influencer to improving nutritional status. Urban poor mothers consuming milk/curd, pulses/beans/egg/meats, and dark green leafy vegetables daily were less likely to be short and thin. However, the proportion consuming these daily was very low among urban poor at 14% (Table [Link]). In a study of slum‐dwelling women aged 16 to 40 years, milk and milk products were reportedly consumed less than twice a week (Chopra et al., 2013). Although the weekly consumption of fried foods did not influence thinness or obesity, consumption of sweetened aerate drinks increased the odds of obesity among urban poor mothers. Another important influencer was secondary or higher education, which like diets, influenced both short stature and thinness. But as noted by earlier researchers, it also increased the odds of obesity (Gaur, Keshri & Joe, 2017; Swaminathan & Mukherji, 2012). Among sociodemographic factors, as noted by other researchers, we observed a decline in thinness and increasing odds of obesity with age, increasing up to almost three times in the oldest age group of over 34 years compared with 20 to 24 years–aged urban women (Gaur, Keshri & Joe, 2017; Swamintahan & Mukherji, 2012). Women married before 18 years of age are known to be thinner than those married after (Goli, Rammohan, & Singh, 2015), however, it did not emerge as an influencer in our analysis. Another finding contradicting previous evidence was the lack of association between parity and any form of malnutrition (Gouda & Prusty, 2014; Koch et al., 2008). We also observed expected increased vulnerability with being tribal and poor in an urban setting.
Our study has several policy, programme, and research implications. First, reaching urban poor women with nutrition screening services is imperative owing to the high prevalence of all forms of maternal malnutrition. However, in the context of India, the platforms to reach urban poor women are limited. The public health infrastructure in urban areas, which should be the first point of preventive health care information and services, is limited to one primary health centre for 50,000 populations, a norm that is frequently violated due to increasing urban populations (Agarwal & Sangar, 2005). Profit‐oriented health services in most urban areas continue to offer wider range in curative than preventive services (Kumar, 2015). In fact, the National Health Mission recommends Accredited Social Health Activists (ASHAs, a door step counsellor, activist, and motivator) in urban slums at one ASHA for about 2,500 slum population; however, the heterogeneous slum population and lack of community groups and self‐help groups are a major deterrent in ASHAs effectively delivering their role of service provider, counsellor, and activist (National Health Mission, 2014). Anganwadi centres, a community‐based platform for supplementary nutrition and health services for pregnant women, lactating mothers, and children under 6 under the ICDS platform have limited coverage in urban areas and has fixed target groups thus, excluding other women who may have nutritional risks. Our own analysis reveals no significant association of Anganwadi centre services on malnutrition among urban poor women. Innovative techniques are needed to reach out to this left‐out, vulnerable urban subgroup. Some techniques have been piloted, such as through trained volunteers, mobile clinics, and community groups that need to be tested for feasibility of a scale‐up (Global Giving[Link]; Sanghera, 2018).
Second, considering that diverse diet was associated with lower thinness and short stature and that “unhealthy” food choices with obesity among urban poor mothers, there is a need for policy and programmatic interventions to enable access to nutritious foods and counselling services to support appropriate food choices and lifestyle changes as part of nutrition services package. The global maternal nutrition recommendations in the context of antenatal care for a positive pregnancy experience also emphasize the need for counselling on diet and physical activity; whereas the global panel on agriculture and food systems has recommended addressing the challenge of gradually changing urban diets on priority (Global Panel, 2017; World Health Organization, 2016). As options for developing nutri‐gardens or animal rearing are limited in urban poor settings, increasing access to lower cost nutritious foods and income generation activities for urban poor women may be more realistic options. Although India's National Nutrition Mission (2018‐2022) Poshan Abhiyaan, has set targets for reducing undernutrition among women and children, it has not brought the emerging challenges of overweight and obesity in focus, which are imminent danger for the all urban women including the poor (Ministry of Woman and Child Development).
Third, screening for anaemia and rolling out the Anemia Mukt Bharat (a national programme to prevent and treat anaemia in select target groups including all women of reproductive age group) should prioritize urban poor women while reaching out all urban mothers owing to high prevalence of anaemia (Ministry of Health and Family Welfare, 2018). Special anaemia outreach camps to test, treat, and counsel women in urban areas with higher poor population should be promoted. This platform could also be used for screening for thinness and obesity.
Fourth, over one‐third urban poor women did not have a BPL card, a key document for food grain subsidy and availing other social safety nets. It is known that food subsidies reach urban women sparingly and are not associated with reduction in malnutrition (NITI Aayog, Government of India, 2016).
Finally, how to identify urban poor remains a programmatic challenge. The BPL card allocation criterion is based on annual household income. Our findings suggest that if BPL cards are used as a measure of poverty, over 60% of those poor by wealth indexation method will be missed. This could be explained by the fact that all entitled to the BPL card may not have received it or missed being enumerated during the census survey for BPL.
5. CONCLUSION
This study indicates that mothers in urban India suffer from various forms of malnutrition (short stature, thinness, anaemia, and obesity). Decadal trends reveal a mixed picture, with considerable reductions in maternal thinness, no changes in prevalence of short stature, and moderate to severe anaemia and increase in prevalence of maternal obesity. The high socioeconomic inequalities in the prevalence of thinness and obesity among urban mothers is a cause for concern and calls for disaggregated nutrition data for policy and programmes. The coexistence of thinness and obesity along with anaemia in this urban population subgroup necessitates the need to have policies that address challenges pertaining to both undernutrition and overweight/obesity and that address socioeconomic disparities. Enlisting the urban poor requires more measures than BPL cards only. Among urban poor, those less than 24 years of age, belonging to tribal households, and not educated should be prioritized for nutritional interventions. More research is needed to understand the determinants of moderate to severe anaemia among urban poor mothers.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest. This research was funded by UNICEF India. The text has not been edited to UNICEF official publication standards and UNICEF accepts no responsibility for errors. The views expressed are those of authors and not necessarily those of UNICEF. The designations in this publication do not imply an opinion or legal status of any country or territory, or of its authorities, or the delimitation of frontiers.
CONTRIBUTION
VS, ADW, DB, SU, and SVS conceptualized the paper and research questions. VS, AB, and KD conceptualized the analyses. KD executed data curation and analyses. VS and AB wrote the original draft of the article. ADW, ZM, PA, SB, DB, SU, and SVS reviewed and edited the manuscript. VS, AB, and KD finalized the paper. All authors read and approved the final draft.
Supporting information
Figure S1. Distribution of analytical sample, DHS 3 and DHS 4
Table S1. Access to maternal health and family planning services and dietary practices of mothers (20‐49 years) in urban India, DHS 4
Sethi V, de Wagt A, Bhanot A, et al. Levels and determinants of malnutrition among India's urban poor women: An analysis of Demographic Health Surveys 2006 and 2016. Matern Child Nutr. 2020;16:e12978 10.1111/mcn.12978
REFERENCES
- Agarwal, S. (2011). The state of urban health in India; comparing the poorest quartile to the rest of the urban population in selected states and cities. Environment and Urbanization, 23(1), 13–28. 10.1177/0956247811398589 [DOI] [Google Scholar]
- Agarwal, S. , & Sangar, K. (2005). Need for dedicated focus on urban health within national rural health mission. Indian Journal of Public Health, 49(3), 141–151. [PubMed] [Google Scholar]
- Agarwal, S. , Satyavarda, S. A. , Kaushik, S. , & Kumar, R. (2007). Urbanization, urban poverty and health of the urban poor: Status, challenges and the way forward. Demography India, 36(1), 121–134. [Google Scholar]
- Agarwal, S. , & Sethi, V. (2013). Nutritional disparities among women in urban India. Journal of Health Population and Nutrition, 31(4), 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal, S. , & Taneja, S. (2005). All slums are not equal: Child health conditions among the urban poor. Indian Pediatrics, 42, 233–244. [PubMed] [Google Scholar]
- Anand, K. , Shah, B. , Yadav, K. , Singh, R. , Mathur, P. , Paul, E. , & Kapoor, S. K. (2007). Are the urban poor vulnerable to non‐communicable diseases? A survey of risk factors for non‐communicable diseases in urban slums of Faridabad. National Medical Journal of India, 20, 115–120. [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Butta, Z. A. , Christian, P. , de Onis, M. , … the Maternal and Child Nutrition Study Group (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. The Lancet, 382(9890), 427–451. [DOI] [PubMed] [Google Scholar]
- Chopra, H. , Chheda, P. , Kehoe, S. , Taskar, V. , Brown, N. , Shivashankaran, D. , … Fall, C. (2013). Dietary habits of female urban slum dwellers in Mumbai. Indian Journal of Maternal and Child. Health, 14(2), 1–13. [PMC free article] [PubMed] [Google Scholar]
- Christian, P. , Lee, S.E. , Donahue, A. , Adair L.S., Arifeen, S.E. , Ashorn, P … … Black R.E. (2013). Risk of childhood undernutrition related to small for‐gestational age and preterm birth in low‐ and middle‐income countries. International Journal of Epidemiology, 42(5), 1340–1355, DOI: 10.1093/ije/dyt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi, D. J. , Kyu, H. H. , & Subramanian, S. V. (2011). Socioeconomic and geographic patterning of under‐ and overnutrition among women in Bangladesh. The Journal of Nutrition, 141(6), 631–638. 10.3945/jn.110.131599 [DOI] [PubMed] [Google Scholar]
- Sustainable Development . (2015). Solutions Network. Indicators and a monitoring framework for the sustainable development goals. Launching a data revolution. A report to the Secretary‐General of the United Nations by the Leadership Council of the Sustainable Development Solutions Network.
- Egata, G. , Berhane, Y. , & Worku, A. (2013). Seasonal variation in the prevalence of acute undernutrition among children under five years of age in east rural Ethiopia: A longitudinal study. BMC Public Health, 13, 864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsey, H. , & Agarwal, S. (2016). Urban health reading pack. Data and evidence. HEART (Health & Education Advice & Resource team).. [Google Scholar]
- Gaur, K. , Keshri, K. , & Joe, W. (2017). Does living in slums or non‐slums influence women's nutritional status? Evidence from Indian mega‐cities. Social Science Medicine, 77, 137–146. [DOI] [PubMed] [Google Scholar]
- Global Giving . About Urban Health Resource Centre. https://www.globalgiving.org/pfil/20032/projdoc.pdf
- Global Panel (2017). Urban diets and nutrition: Trends, challenges and opportunities for policy action. Policy Brief No. 9. London, UK: Global Panel on Agriculture and Food Systems for Nutrition. [Google Scholar]
- Goli, S. , Rammohan, A. , & Singh, D. (2015). The effect of early marriages and early childbearing on women's nutritional status in India. Maternal and Child Health Journal, 19(8), 1864–1880. 10.1007/s10995-015-1700-7 [DOI] [PubMed] [Google Scholar]
- Gouda, J. , & Prusty, R. K. (2014). Overweight and obesity among women by economic stratum in urban India. Journal of Health Population and Nutrition, 32(1), 79–88. [PMC free article] [PubMed] [Google Scholar]
- Harding, K. L. , Aguayo, V. M. , & Webb, P. (2018). Hidden hunger in South Asia: A review of recent trends and persistent challenges. Public Health Nutrition, 21, 785–795. 10.1017/S1368980017003202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazarika, I. (2009). Women's reproductive health in slum populations in India: Evidence from DHS‐3. Journal of Urban Health, 87(2), 264–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (2009). Weight gain during pregnancy: Reexamining the guidelines. Washington, D.C.: National Academy Press. [PubMed] [Google Scholar]
- International Institute for Population Sciences (IIPS) & Macro International . (2015‐16). National Family Health Survey (DHS‐4), 2015–16: India Report.
- International Institute for Population Sciences (IIPS) & Macro International. (2005‐06) . National Family Health Survey (DHS‐4), 2005–06: India Report.
- Jayamani, V. , Gopichandran, V. , Lee, P. , Alexander, G. , Christopher, S. , & Prasad, J. H. (2013). Diet and physical activity among women in urban and rural areas in South India: A community based comparative survey. Journal of Family Medicine and Primary Care, 2(4), 334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerath, S. G. , Devansenapathy, N. , Singh, A. , Shankar, A. , & Zodpey, S. (2015). Ante natal care (ANC) utilization, dietary practices and nutritional outcomes in pregnant and recently delivered women in urban slums of Delhi, India: An exploratory cross‐sectional study. Reproductive Health, 12, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, M. , & Kraemer, A. (2009). Factors associated with being underweight, overweight and obese among ever‐married non‐pregnant urban women in Bangladesh. Singapore Medical Journal, 50(8), 804–813. [PubMed] [Google Scholar]
- Koch, E. , Bogado, M. , Araya, F. , Romero, T. , Díaz, C. , Manriquez, L. , … Kirschbaum, A. (2008). Impact of parity on anthropometric measures of obesity controlling by multiple confounders: A cross‐sectional study in Chilean women. Journal of Epidemiology and Community Health, 62(5), 461–470. [DOI] [PubMed] [Google Scholar]
- Kozuki, N. , Katz, J. , Lee, A. C. , Vogel, J. P. , Silveira, M. F. , Sania, A. , … Child Health Epidemiology Refernce Group Small‐for‐Gestational‐Age/Preterm Birth Working Group (2015). Short maternal stature increases risk of small‐for‐gestational‐age and preterm births in low‐ and middle‐income countries: individual participant data meta‐analysis and population attributable fraction. Journal of Nutrition, 145, 2542–2550. 10.3945/jn.115.216374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, S. (2015). Private sector in health care delivery market in India: Structure, growth and implications. ISID working paper 185.
- Loughhead, S. , Mittal, O. & Wood, G. (2001) Urban poverty and vulnerability in India. DFID's experience from a social policy perspective. [Google Scholar]
- Mendez, M. A. , Monteiro, C. A. , & Popkin, B. M. (2008). Overweight exceeds underweight among women in most developing countries. American Journal of Clinical Nutrition, 81(3), 714–721. [DOI] [PubMed] [Google Scholar]
- Menon, P. , Ruel, M. T. , & Morris, S. S. (2000). Socio‐economic differentials in child stunting are consistently larger in urban than in rural areas. Food and Nutrition Bulletin, 21(3), 282–289. [Google Scholar]
- Ministry of Health and Family Welfare, Government of India . (2018). Anemia Mukt Bharat. Intensified National Iron Plus Initiative (I‐NIPI). Operational guidelines for program managers.
- Ministry of Home Affairs, Government of India . (2011). Office of the Registrar General and Census Commissioner, India. Population enumeration data.
- Ministry of Housing and Urban Poverty Alleviation, Government of India . Slums in India. A statistical compendium. 2015.
- Ministry of Woman and Child Development, Government of India . About Poshan Abhiyan https://www.icds-wcd.nic.in/nnm/home.htm#
- Misra, A. , Chowbey, P. , Makkar, B. M. , Vikram, N. K. , Wasir, J. S. , Chadha, D. , … Consensus Group (2009). Consensus Statement for Diagnosis of Obesity, Abdominal Obesity and the Metabolic Syndrome for Asian Indians and Recommendations for Physical Activity, Medical and Surgical Management. Journal of the Association of Physicians of India, 57, 163–170. [PubMed] [Google Scholar]
- National Health Mission . (2014). Update on ASHA program.
- National Institute of Nutrition . (2011). Dietary guidelines for Indians: A manual. Indian Council of Medical Research. [Google Scholar]
- Nguyen, P. H. , Scott, S. , Avula, R. , Tran, L. M. , & Menon, P. (2018). Trends and drivers of change in the prevalence of anemia among 1 million women and children in India, 2006 to 2016. BMJ Global Health, 18, 3 10.1136/bmjgh-2018-001010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niti, Aayog , Government of India (2016). Evaluation study on role of public distribution system in shaping household and national food security. DMEO Report No., 233. [Google Scholar]
- Planning Commission, Government of India . (2011a). Press note on poverty estimates. New Delhi. [Google Scholar]
- Planning Commission, Government of India . (2011b). Report of the working group on urban poverty, slums and service delivery system.
- Planning Commission, Government of India . (2014). Report of the expert group to review the methodology for measurement of poverty.
- Popkin, B. M. (2001). Nutrition in transition: The changing global nutrition challenge. Asia Pacific Journal of Clinical Nutrition, 10, S13–S18. [PubMed] [Google Scholar]
- Pouliou, T. , & Elliott, S. J. (2010). Individual and socio‐environmental determinants of overweight and obesity in Urban Canada. Health and Place, 16, 389–398. 10.1016/j.healthplace.2009.11.011 [DOI] [PubMed] [Google Scholar]
- Rutstein, S.O. (2008). The DHS Wealth Index: Approaches for rural and urban areas. DHS working paper, No. 60.
- Rydin, Y. , Bleahu, A. , Davies, M. , Dávila, J. D. , Friel, S. , Grandis, G. D. , … Wilson, J. (2012). Shaping cities for health: Complexity and the planning of urban environments in the 21st century. The Lancet, 379, 2079–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghera, T. (2018). In a Mumbai slum, children become healthier as their parents learn to tackle malnutrition. Indiaspend. https://www.indiaspend.com/in-a-mumbai-slum-children-become-healthier-as-their-parents-learn-to-tackle-malnutrition-25128/ [Google Scholar]
- Save the Children . (2015). The urban disadvantage. State of the World's Mothers. [Google Scholar]
- Singla, S. , Suman, R. L. , Meena, P. , Goyal, S. , Jain, R. , & Meena, S. (2016). Severe acute malnutrition: Seasonal variations in Southern Rajasthan, India. International Journal of Research in Medical Sciences, 4, 5310–5313. [Google Scholar]
- Swaminathan, H. , & Mukherji, A. (2012). Slums and malnutrition: Evidence from women in India. American Journal of Public Health, 102(7), 1329–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed, W. , & Kamathi, V. C. (2012). Maternal short stature: A risk factor for low birth weight in neonates. Journal of Medicine and Allied Sciences, 2(2), 62–65. [Google Scholar]
- UNICEF . (2012). Children in an urban world. The State of the World's Children. [Google Scholar]
- UNICEF . (2018). Advantage or paradox? The challenge for children and young people of growing up urban. Data and Analytics Section, Division of Data, Research and Policy. UNICEF Headquarters.
- United Nations (2018). World urbanization prospects: The 2018 revision. New York: United Nations, Department of Economic and Social Affairs, Population Division. [Google Scholar]
- Uthman, O. A. (2009). Patterns, distribution, & determinants of under‐ and overnutrition among women in Nigeria: A population‐based analysis. Journal of Public Health, 17(5), 289–299. [Google Scholar]
- We are water foundation . (2017). Toilets to provide freedom, health and dignity to women. https://www.wearewater.org/en-IN/toilets-to-provide-freedom-health-and-dignity-to-women_285651
- World Health Organization . (1989). Preventing and controlling iron deficiency anemia through primary health care. A guide for health administrators and program managers. [Google Scholar]
- World Health Organization (1995). Maternal anthropometry and pregnancy outcome: A WHO collaborative study. Bulletin of World Health Organisation, 73(Suppl), 1–98. [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2016). WHO recommendations on antenatal care for a positive pregnancy experience. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Distribution of analytical sample, DHS 3 and DHS 4
Table S1. Access to maternal health and family planning services and dietary practices of mothers (20‐49 years) in urban India, DHS 4


