Abstract
The Canada Prenatal Nutrition Program (CPNP) provides a variety of health and nutrition supports to vulnerable mothers and strongly promotes breastfeeding but does not have a formal framework for postnatal lactation support. Breastfeeding duration and exclusivity rates in Canada fall well below global recommendations, particularly among socially and economically vulnerable women. We aimed to explore CPNP participant experiences with breastfeeding and with a novel community lactation support program in Toronto, Canada that included access to certified lactation consultants and an electric breast pump, if needed. Four semistructured focus groups and 21 individual interviews (n = 46 women) were conducted between September and December 2017. Data were analysed using inductive thematic analysis. Study participants reported a strong desire to breastfeed but a lack of preparation for breastfeeding‐associated challenges. Three main challenges were identified by study participants: physical (e.g., pain and low milk supply), practical (e.g., cost of breastfeeding support and maternal time pressures), and breastfeeding self‐efficacy (e.g., concern about milk supply and conflicting information). Mothers reported that the free lactation support helped to address breastfeeding challenges. In their view, the key element of success with the new program was the in‐home visit by the lactation consultant, who was highly skilled and provided care in a non‐judgmental manner. They reported this support would have been otherwise unavailable due to cost or travel logistics. This study suggests value in exploring the addition of postnatal lactation support to the well‐established national CPNP as a means to improve breastfeeding duration and exclusivity among vulnerable women.
Keywords: breastfeeding, breastfeeding support, food security, infant and child nutrition, nutrition, qualitative methods
Key messages.
Vulnerable mothers who participated in one program delivered under the Canada Prenatal Nutrition Program reported planning and attempting to breastfeed but were unprepared for the challenges. Three main challenges were identified by participants: physical (e.g., pain and low milk supply), practical (e.g., cost of breastfeeding support and time pressures), and breastfeeding self‐efficacy (e.g., milk supply concerns and conflicting information).
Mothers identified in‐home skilled help provided in a non‐judgmental manner as key elements of the community lactation support.
Mothers perceived in‐home lactation consultant services and double‐electric breast pumps helped mitigate various breastfeeding challenges.
Key messages.
Vulnerable mothers who participated in one program delivered under the Canada Prenatal Nutrition Program reported planning and attempting to breastfeed but were unprepared for the challenges. Three main challenges were identified by participants: physical (e.g., pain and low milk supply), practical (e.g., cost of breastfeeding support and time pressures), and breastfeeding self‐efficacy (e.g., milk supply concerns and conflicting information).
Mothers identified in‐home skilled help provided in a non‐judgmental manner as key elements of the community lactation support.
Mothers perceived in‐home lactation consultant services and double‐electric breast pumps helped mitigate various breastfeeding challenges.
1. INTRODUCTION
The benefits of breastfeeding for infants, nursing mothers, and society are well established in the literature (Kramer & Kakuma, 2012; Victora et al., 2015; Victora et al., 2016). Consequently, exclusively breastfeeding for the first 6 months of life with introduction of solids and continued breastfeeding thereafter is recommended (World Health Organization [WHO], 2003; Health Canada, 2015). However, gaps remain between recommended and actual breastfeeding practices worldwide, including in Canada (Statistics Canada, 2012; WHO & UNICEF, 2017). Despite a national 90% initiation rate, at 6 months postpartum, only 30% of Canadian mothers are exclusively breastfeeding, and 47% have stopped breastfeeding entirely (Chalmers et al., 2009; Statistics Canada, 2019). Breastfeeding inequalities continue to persist, and women who have lower education, lower income, or who are adolescents or single have the lowest breastfeeding rates (Best Start Resource Centre, 2014; Gionet, 2013; Nickel et al., 2014). For example, national Canadian data indicate that 23% of mothers in the lowest income quintile breastfed exclusively for 6 months compared with 33% of mothers in the highest income quintile (Statistics Canada, 2012). Similarly, 17% of mothers with less than high school education breastfed exclusively for 6 months compared with 29% of mothers with post‐secondary education. McFadden et al. (2017) concluded in their systematic review that postnatal breastfeeding support can improve breastfeeding outcomes. However, there are limited data on what support might be most effective for vulnerable groups, particularly within the Canadian context. Currently, community breastfeeding support is typically implemented by local public health or non‐profit agencies resulting in fragmentation of service delivery and high variation based on location. An opportunity exists to strengthen access to postnatal lactation support for vulnerable mothers through the Canada Prenatal Nutrition Program (CPNP).
The CPNP, funded by the federal Public Health Agency of Canada, provides support for community‐based maternal–infant health interventions delivered at over 250 sites across Canada to more than 51,000 women (CPNP, 2015). The CPNP aims to increase healthy birth weights and promote and support breastfeeding among women in challenging life circumstances that could impact their or their infant's health because of social determinants of health. These vulnerable women may include those with lower income, lower education, history of trauma and/or substance use, social isolation, and adolescents. In some CPNP sites, other resources such as charitable donations enhance CPNP support.
There is currently limited evaluation of CPNP's impact on infant feeding practices, particularly breastfeeding duration and exclusivity, and no formal framework or funding for postnatal breastfeeding support, which would likely enhance outcomes. However, one CPNP site in Toronto is using charitable donations to offer lactation services as an enhancement to their program. This paper presents findings from a qualitative evaluation of this initiative. Our study aimed to explore participants' experiences with breastfeeding and enhanced community lactation support.
2. METHODS
2.1. Context and study participants
We recruited women registered in the CPNP implemented by Parkdale Queen West Community Health Centre in Toronto, which has been operating for 25 years (hereafter referred to as “the prenatal program”). The prenatal program serves a diverse group of approximately 200 women annually, over 75% of whom report income below the 2012 Statistics Canada size‐adjusted low‐income cut‐off (Statistics Canada, 2015) and approximately 85% of whom report being born outside of Canada (e.g., immigrants/newcomers primarily from East Asia, Africa, and South Asia). Weekly services at the prenatal program include group education sessions, individualized support from public health nurses and dietitians, community referrals, snacks, public transit tokens, CDN$10 grocery store gift card, self‐serve food bank, and childcare. Education sessions include breastfeeding information and promotion in the curriculum approximately once every 4–6 weeks.
Clients who attend the prenatal program a minimum of three times are offered access to postnatal lactation support as a program enhancement. Charitable donations are used to fund skilled lactation support that is usually accessible only to higher income women. The goals of the lactation support are to (a) increase support to mothers facing challenges with infant feeding, particularly breastfeeding and (b) reduce barriers to accessing professional breastfeeding support. Approximately 70% (138/200) of prenatal program clients who gave birth in the 2017/2018 fiscal year accessed the enhanced lactation support.
The enhanced lactation support includes up to two free consultations by an International Board‐Certified Lactation Consultant (IBCLC) delivered in‐home or at the prenatal program site, a gift package of breastfeeding and infant care supplies (e.g., diapers and nursing pillow), and, if recommended by an IBCLC or public health nurse, a double‐electric breast pump (Medela™ Pump in Style). For mothers provided with a breast pump, the IBCLC demonstrates how to use it and advises on best practices for collecting and storing breast milk. Additional free consultations are arranged (telephone, text, or e‐mail) at the client's request and at the discretion of the IBCLC. If needed, the IBCLC provides herbal galactagogues and lactation aids such as a supplemental nursing system.
2.2. Recruitment and consent
Participants were recruited by the first author from women who had enrolled in the prenatal program and gave birth between June 1, 2016 and August 16, 2017. Women were approached in person if they were still participating in programming, or by telephone/e‐mail if not. Study participants were informed that the researcher wanted to learn more about what they liked about the prenatal program and aspects that could be improved in relation to infant feeding. Each participant provided written, informed consent. For non‐English speaking clients, sequential interpretation was used for the recruitment and consent process. Ethics approval was obtained from the University of Toronto research ethics board.
2.3. Data collection
This study used a qualitative research design involving two methods of data collection: focus groups and individual interviews. For non‐English speaking clients or those who did not want to attend a focus group, interviews were arranged and sequential interpretation was used if required. A single semistructured guide of open‐ended questions was developed for use in focus groups and interviews. Questions were developed in conjunction with key informants, including the prenatal program Coordinator, Parkdale Queen West Community Health Centre's Director of Health Promotion and Community Engagement, and an IBCLC providing the lactation support. Questions were pretested among five clients and found to be acceptable and understandable (Table 1; Table S1 for complete guide). They were designed to explore (a) experiences with infant feeding, particularly breastfeeding and (b) experiences, perceptions, and attitudes toward the enhanced lactation support.
Table 1.
Sample of focus group/interview questions
| Focus group/interview questions |
| What was your original plan for feeding your baby and then how did you actually feed your baby after they were born? |
| In general, who and what helped you to feed your baby? |
| What are some challenges that families face when trying to feed their baby? |
| What did you find most helpful about the infant feeding services you received through the health center? This might have included the lactation consultant and breast pump. |
| If you didn't see a lactation consultant or get a breast pump, how could it have helped you or other mothers feed their baby? |
| What other services do you wish the Parkdale Parents’ Primary Prevention Project (5P's) had to help parents feed their babies? |
The first author, a Registered Dietitian, conducted focus groups between September and December 2017. As recommended when working with low‐income and/or multi‐ethnic women (Barnett, Aguilar, Brittner, & Bonuck, 2012), the first author regularly attended the prenatal program to develop rapport with clients. The second author, also a Registered Dietitian, attended all four focus groups and 5 of 21 interviews to record notes. The first two authors debriefed and discussed reflections following these focus groups and interviews. To ensure study participants felt comfortable speaking openly, focus groups were conducted off‐site at a local non‐profit community organization. Interviews took place at either the participant's home or a public library. All discussions were audio‐recorded, and data collection continued until saturation (e.g., no new information) was reached (Saunders et al., 2017).
2.4. Data analysis
Recordings were professionally transcribed verbatim, checked for accuracy against recordings, and imported into NVivo Version 12 (QRS International, Burlington, MA, USA). Data were analysed using the iterative process of thematic analysis outlined by Braun and Clarke (2006). This method was chosen because of its appropriateness for applied health research, its flexibility, and its robust framework that allows researchers to identify, analyse, and report thematic patterns of meaning across data sets (Braun & Clarke, 2006, 2013). Analysis included data immersion, generating initial codes, searching for themes, and reviewing and defining themes (Braun & Clarke, 2006). The first author was responsible for inductively generating initial codes across the data based on relevance to the research aim. The second author independently reviewed all coding, including the placement of quotations under each code, and provided feedback on collating codes into potential themes. Discrepancies in coding were discussed and resolved between the first two authors. We acknowledge that engagement with the data was shaped by our own assumptions, disciplinary backgrounds, and professional experiences, which may have in turn influenced the analysis (Bourke, 2014). However, our interpretation of the data was guided by multiple perspectives through regular feedback from our interdisciplinary team (Cresswell & Miller, 2000). Our team included our community partners who provide perinatal programming and researchers with a variety of backgrounds, including public health, anthropology, and nutrition and dietetics. Notes were kept to document discussions and data analysis decisions made during these meetings. Group discussions enhanced the development, refinement, and interpretation of themes, which were reviewed against the transcripts to ensure relevance to the experiences shared by participants (Braun & Clarke, 2013). Final themes were organized under two overarching domains aligning with the study aim: infant feeding experiences and experiences with the lactation support.
3. ETHICAL STATEMENT
The Office of Research Ethics, University of Toronto approved this study.
4. RESULTS
Among 114 prenatal program participants who delivered infants in the target‐sampling period, 34 were no longer connected to the program and could not be contacted by telephone/e‐mail (Figure 1). Fifty‐one women consented and enrolled in the study, among whom five did not attend a focus group or interview. Of the 46 adult women who participated in this research (n = 25 focus groups, n = 21 interviews), 25 were first‐time mothers. The age range of study participants' most recent infant was 2–17 months. Focus groups lasted a mean duration of 46 min (range 32–51 min), and interviews lasted a mean duration of 39 min (range 20–90 min). There were 5–9 participants in three of the focus groups, whereas one focus group had two participants. Five interviews were conducted with an in‐person interpreter.
Figure 1.
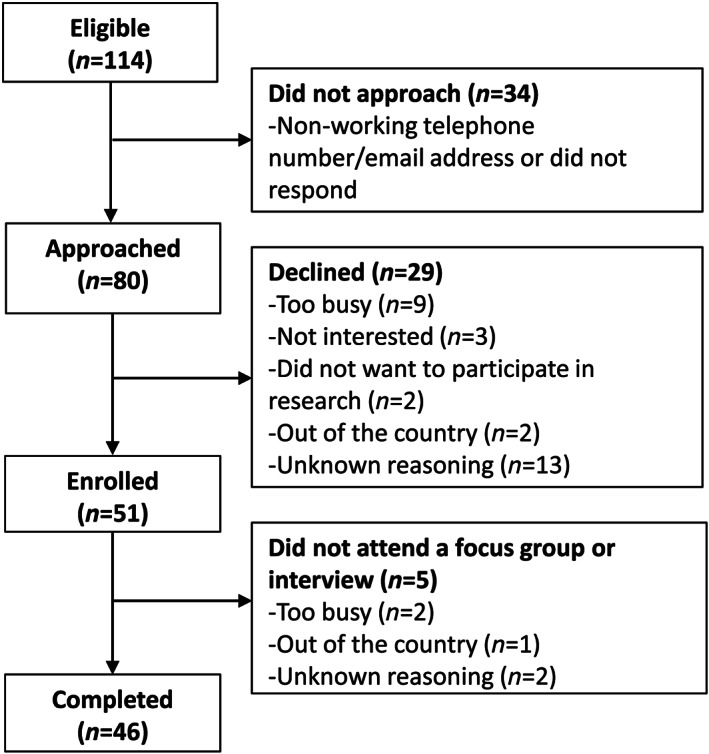
Participant flow diagram
All but a few study participants reported they had decided during pregnancy to breastfeed and attempted to do so. Discussions indicated that exclusive breastfeeding for 6 months was not the norm; most women reported feeding with a combination of breast milk and formula. Multiparous study participants also referred to previous breastfeeding experiences. Themes are described using representative quotes below.
4.1. Unprepared for breastfeeding challenges
Participating mothers reported awareness that breastfeeding is the recommended food for infants. A common theme was that study participants were unaware that they might experience difficulties while attempting to breastfeed and were unprepared for these challenges.
You know, once it actually happened, I realized I know nothing about it [breastfeeding] … So one thing is the theory, another thing is actually practicing that. (Focus Group [FG]; primiparous)
I thought [it would be] easy and I never expected that I will face a very difficult time with breastfeeding … when I see people [breastfeeding] I feel like it's so easy, but when I do it, it's so difficult … I have a very, very tough time … (Interview; primiparous)
Study participants noted that breastfeeding is a learned behaviour for infant and mother, therefore, prenatal and postnatal guidance should be provided on what to expect and how to deal with potential challenges.
But I didn't know that breastfeeding is so difficult; I thought it came naturally … mothers and babies they know it … The [prenatal] classes only teach you about different positions for breastfeeding and what are the benefits of breastfeeding, that's it. (Interview; primiparous)
Because it's such a big surprise … because everybody prepares for labour, “oh labour is going to be painful”, but what about breastfeeding? (FG; multiparous)
4.2. Breastfeeding challenges
Breastfeeding challenges were common, with the majority of mothers referring to multiple difficulties when describing their experience (Figure 2). Three main types of breastfeeding challenges (subthemes) were identified by study participants: physical, practical, and self‐efficacy.
Figure 2.
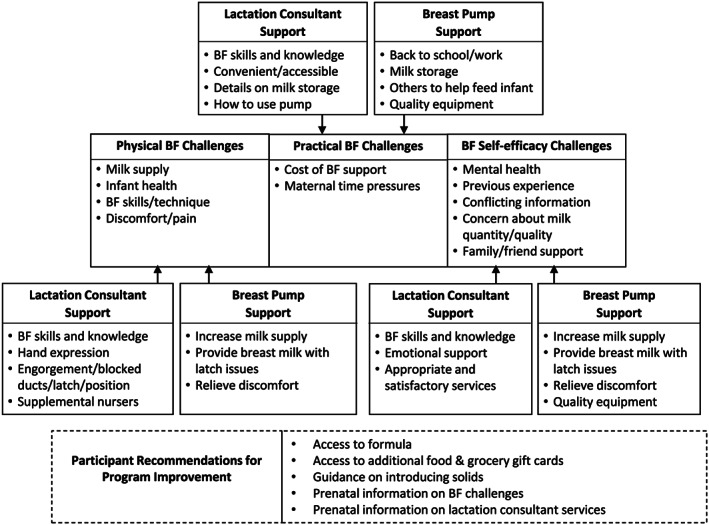
Thematic representation. BF, breastfeeding
4.2.1. Physical breastfeeding challenges
The most commonly noted “physical” breastfeeding issue was discomfort, including pain, cracked nipples, engorgement, and mastitis. Another concern for study participants was milk supply, including the perception of postpartum delay in milk production or low milk supply thereafter. Breastfeeding technique, including infant latch, was also cited as problematic. Finally, some study participants referred to slow infant weight gain, jaundice, and dehydration as reasons for introducing formula.
And when I first feed the baby, uh, … it was a little bit of milk, so it was very hard for me … even though baby latched properly. But I don't know, maybe I don't know how to feed the baby. Uh, my nipple was cracked and it was hurt so I keep on crying, crying … it was so difficult … (FG; multiparous)
4.2.2. Practical breastfeeding challenges
Practical challenges included constructs that made breastfeeding less realistic in the context of the mother's life. The first “practical” breastfeeding challenge was maternal time pressures. Study participants commented on the time required to breastfeed, the infant's reliance on the mother, busy lifestyles (including caring for other children), and returning to work/school as problematic.
I had to take her everywhere … she never took a bottle. Oh my, it was tough, 'cause I couldn't leave her. Everywhere I had to take her. (Interview; primiparous)
For me, I feel like, you know, I keep all the time breastfeeding like two … [every] two hours. Any time he needs, I give. You know, I have no rest, no rest. (Interview; multiparous)
Another practical challenge was the time and cost associated with accessing breastfeeding support. Study participants recognized that if the enhanced lactation support was not available, they might not have known there was such a thing as a lactation consultant or about using a breast pump and would not have been able to afford these supports.
Because I checked on the internet, it [breast pump] will cost around $300‐$400, which is a lot of investment … because there are a whole lot of things to buy. (Interview; primiparous)
That lady [lactation consultant] costs so much money if you call her … I felt really lucky. (FG; primiparous)
Some study participants received lactation support outside of the lactation support program, for example, from midwives, family doctors, in‐hospital IBCLCs, and public health breastfeeding clinics. It was noted, though, that community breastfeeding services were not always accessible. Several study participants also had experience using manual breast pumps but noted they were more painful to use and less efficient than the double‐electric pump.
4.2.3. Breastfeeding self‐efficacy challenges
Study participants referred to breastfeeding challenges that directly relate to the components of breastfeeding “self‐efficacy,” or a mother's confidence in her ability to breastfeed her child (Dennis, 1999). Many mothers perceived that feelings of guilt, stress, anxiety, depression, loneliness, and pressure affected their ability to feed their infant and their emotional health in the prenatal and postnatal period. These feelings were linked to the availability of support from family and friends. About one‐third of study participants indicated they had limited or no family in Canada.
For me, I think the main challenge is, aside from I'm by myself most of the time, it's the pressure … I felt really pressured because I really want [to breastfeed], you know, and people around you will say, you have to breastfeed … it's like there's no other way, you have to breastfeed otherwise you're a bad mom. (FG; primiparous)
So, I had that anxiety all through the early months. I'll never really know if I could have fed her a little more … because, um, I could get into a loop of fretting … (FG; multiparous)
The receipt of conflicting breastfeeding information and opinions, whether from family and friends or health care professionals, further compromised breastfeeding self‐efficacy.
… there's a lot of input on how to breastfeed your child, when to breastfeed them, like, and how you should do it if you're out in public … it's like one person saying, “No, don't do it this way” and another person saying, “Oh yeah, you need to do it this way” …” Don't feed them formula”, “Oh yeah, do feed them formula”, back and forth. (FG; primiparous)
Study participants indicated they were not necessarily confident in their ability to provide sufficient milk volume for their infant's needs and voiced concern regarding the adequacy of nutrients available in their breast milk.
I give her, um, formula because I found that, um, she didn't get every like vitamins, whatever she needs. In the formula it is written like DHA and so many vitamin, which are good for her. And that's why sometimes I feel like it's important to give her [formula]. (Interview; multiparous)
Generally, study participants who previously breastfed indicated that it helped them through their current experience, but they noted that this was not always the case since each infant and each breastfeeding experience could be different. A minority of study participants reported a generally positive breastfeeding experience with minimal challenges.
4.3. Lactation consultant support helped address key breastfeeding challenges
Study participants described IBCLCs as providing numerous supports, aligning with the above‐mentioned categories of breastfeeding challenges (Figure 2). Physical support included hands‐on guidance with hand expression, latching, positioning, engorgement, and blocked ducts. Generally, mothers referred to IBCLCs as teaching them how to breastfeed. Practically speaking, study participants spoke about the accessibility of the services. The in‐home support with flexible hours was highly valued because it was challenging to leave their home to seek support soon after delivery as they were overwhelmed with caring for a newborn, they were recovering from childbirth and/or they lacked a support system at home. Study participants reported the convenience of the continued contact with IBCLCs by telephone, e‐mail, or text message after the initial home visit.
The majority of study participants reportedly accessed the IBCLC services and were grateful for the individualized support that helped to enhance their breastfeeding self‐efficacy. There was an overall appreciation for the empathetic and encouraging attitude of the IBCLC and emotional support provided. Participant narratives described the IBCLC with terms such as “helpful,” “nice,” “amazing,” and “awesome.”
… And that was so nice, that it was, like, coming to my house because I was too sore to move and she, like, worked with my schedule and, like, I felt really important to her, like she cares … It was very convenient because, like, if I had to leave the house at that point, like, I was just a mess physically and, like, emotionally, like so many hormones. So to have someone just come to me was really useful. (FG; primiparous)
Wonderful, wonderful person. She went twice to my place and she gave me a lot of work and tools to improve … I was really depressed, and desperate, and so she came again. And very accessible over the phone, over e‐mail, giving me all the information … (Interview; primiparous)
4.4. Breast pump helped address key breastfeeding challenges
The majority of study participants reported to have received a double‐electric breast pump and indicated various ways in which it helped them feed their infants. These aligned with the main identified categories of breastfeeding challenges (Figure 2). Mothers reported primarily using the breast pump to establish or increase milk supply. When mothers experienced latch issues, using the pump provided peace of mind that they could feed their infant breast milk. The storage of breast milk for future use was important so mothers could rest and have others help with feedings. The pump was also used for comfort measures to relieve pain and pressure. Study participants were grateful for the high‐quality electric breast pump and acknowledged the fact that it was fast and easy to use, in comparison to hand expression or a manual pump. The importance of the pump when going back to work or school was discussed but only by a few study participants; therefore, this appeared not to be a primary reason for using a breast pump in this group.
I was crying. The tears were of happiness because I was really concerned that the baby was not able to eat. And that machine allow me, for me to pump out my breast milk and give it to my baby … I use it because the baby wasn't latching properly at the beginning and I needed to empty my breasts. They were really huge. To rest, I use it to rest too. And to store milk as well. (Interview; multiparous)
I was pumping for more than four months, but it was very useful. And because, you know, when my breasts are full I don't want to waste the milk, and at the same time it was very painful. So I had the relief of pain, and I was feeding my baby my breast milk, so it was very, very useful. (Interview; multiparous)
The vast majority of study participants who used a breast pump reported that it was helpful overall. However, it is important to note that approximately five mothers indicated they had issues using a breast pump. Issues included difficulty in expressing sufficient milk, not finding it effective to increase their milk supply, physical discomfort, and the time and effort required to pump and clean associated bottles.
Study participants identified that the IBCLC and breast pump worked hand in hand to target breastfeeding issues. The IBCLC provided hands‐on support and was the link to providing the breast pump and demonstrating how to use it. Although the majority of study participants did use the enhanced lactation support, about five did not. Personal reasons included no issues with breastfeeding, did not want a breast pump or already had one, or moved outside the prenatal program catchment area.
4.5. Suggested program improvements
Study participants identified additional areas where the prenatal and lactation support program could improve support of their infant feeding goals, including guidance on weaning and introducing solids, prenatal education on breastfeeding challenges and what to expect, and prenatal information on lactation consultant services.
Study participants noted that infant feeding problems might be further compounded by social determinants of health, including low‐income and food insecurity. For example, some mothers discussed the positive relationship between healthy eating and the quantity and quality of breast milk. They noted that this is hindered by the high cost of food, leading to concerns about their breast milk. Because the majority of study participants were not exclusively breastfeeding, mothers also reported concerns about the affordability of formula. Therefore, study participants highlighted a need for access to formula and additional food and grocery store gift cards.
… It's [formula] extremely expensive. My husband was praying for my milk to come because we cannot afford this. It's very, very expensive, like it cost us so much for a week only. (Interview; multiparous)
Some study participants commented on additional intersecting determinants of health, including social isolation, settlement issues, unemployment, and language barriers. These issues merit further investigation for their impact on infant feeding but were not explored in‐depth in this study.
5. DISCUSSION
This qualitative study evaluated vulnerable mothers' experiences with breastfeeding and lactation support offered as an enhancement to one Toronto CPNP site. Study participants reported planning to breastfeed, and attempting to do so, but were unprepared for the challenges. Mothers who used the enhanced lactation support reported that it helped to address breastfeeding challenges. According to study participants, key elements included in‐home, skilled help provided in a caring, non‐judgmental manner.
Mothers in this study felt there was a disconnect between prenatal promotion of “breast is best” and the reality of learning breastfeeding skills while caring for a newborn. The majority of breastfeeding concerns described by study participants, including low milk supply, align with those reported in the literature (Brown, Dodds, Legge, Bryanton, & Semenic, 2014; Li, Fein, Chen, & Grummer‐Strawn, 2008; Odom, Li, Scanlon, Perrine, & Grummer‐Strawn, 2013; Rollins et al., 2016; Wagner, Chantry, Dewey, & Nommsen‐Rivers, 2013). According to the 2011–2012 Canadian Community Health Survey, women indicated insufficient milk supply as the number one reason for early breastfeeding cessation (Gionet, 2013), consistent with studies worldwide (Balogun, Dagvadorj, Anigo, & Sasaki, 2015; Gatti, 2008). Previous research suggests that breastfeeding intention is a significant predictor for initiation and duration, but early breastfeeding experiences may mediate its effect on duration (DiGirolamo, Thompson, Martorell, Fein, & Grummer‐Strawn, 2005; Mitra, Khoury, Hinton, & Carothers, 2004). Unfortunately, qualitative and quantitative studies have highlighted that there are gaps in breastfeeding support, and this disproportionately affects vulnerable women (Chalmers et al., 2009; Garner et al., 2016).
Mothers described the lactation support as helping to address a variety of physical, practical, and self‐efficacy breastfeeding challenges. These findings are consistent with a recent Cochrane review that reported positive effects of postnatal breastfeeding support on breastfeeding outcomes up to 6 months (McFadden et al., 2017). However, very few studies in the review examined vulnerable women outside African–American and Hispanic communities in the United States. Additionally, there was high heterogeneity between study contexts, interventions, and outcomes. Authors of the Cochrane review noted that the type of breastfeeding support likely requires adaptations to fit the needs of different population groups. Our study suggests that in‐home skilled help provided in a non‐judgmental manner are key program elements in postnatal support for low‐income women and/or those who self‐identified as immigrants/newcomers to Canada. Mothers also reported that accessibility of services is key. They noted that community breastfeeding services were not always accessible due to the inability to make appointments, limited hours of operation, family responsibilities, and inadequate transportation. Key components of the lactation support identified by study participants coincide with the recommendations of McFadden et al. (2017) and Schmied, Beake, Sheehan, McCourt, and Dykes (2011) from their systematic review and metasynthesis of the literature; specifically, breastfeeding support should be in‐person, proactive, predictable, and provided in an empathetic and trusting manner. We posit that appropriate and accessible skilled lactation support, described above, may help to establish breastfeeding, resolve early difficulties, and increase breastfeeding self‐efficacy. Breastfeeding self‐efficacy has been shown to be a modifiable factor that can be targeted to improve breastfeeding outcomes (Brockway, Benzies, & Hayden, 2017; Dennis, 1999).
Mothers in the present study reported that, in addition to skilled help, breast pumps were an important component of lactation support. Results from the U.S. 2005–2007 Infant Feeding Practices Study II found that 85% of breastfeeding mothers of infants 1.5–4.5 months of age (n = 1,564) reported using a breast pump (Labiner‐Wolfe, Fein, Shealy, & Wang, 2008). As far as we know, limited Canadian data are available on breast pump practices in general. However, among 2,870 children in the Canadian Healthy Infant Longitudinal Development study, 57% of those who were breastfed at 3 months of age also received pumped breast milk (Azad et al., 2018). Our study participants used breast pumps for a range of reasons also identified in the literature: to maintain milk supply, to provide breast milk during breastfeeding problems, and to increase flexibility and allow others to help with infant feeding (Chamberlain, McMahon, Phillip, & Merewood, 2006; Labiner‐Wolfe et al., 2008; Win, Binns, Zhao, Scott, & Oddy, 2006). Our research showed high uptake of breast pumps, but further research is needed as to why and how breast pumps may or may not help low‐income women to breastfeed. Although the benefits of using an electric breast pump to establish milk supply and enable the provision of human milk in a mother's absence are well described, the longer term impact of using breast pumps on the duration and exclusivity of feeding at the breast, and feeding human milk generally, are unknown (Felice, Cassano, & Rasmussen, 2016; Rasmussen & Geraghty, 2011; Win et al., 2006). Previous research recommends that breast pump use and type should be based on the mother–baby dyad's individual situation (e.g., stage of lactation and pump dependency; Meier, Patel, Hoban, & Engstrom, 2016; Becker, Smith, & Cooney, 2015).
The evaluated lactation support addressed key breastfeeding needs, but other social and structural factors may influence infant feeding practices. This study did not aim to investigate these issues in detail, but participants did report that breastfeeding problems might be further compounded by social determinants of health, including low‐income and food insecurity. This is supported by Canadian and U.S. data demonstrating that breastfeeding may simply be “too much” for some low‐income women (Frank, 2015a; Hardison‐Moody, MacNeil, Elliot, & Bowen, 2018). Although infant feeding practices were not formally assessed in the current study, it was not uncommon for mothers to discuss feeding a combination of breast milk and formula. Previous research indicates that low‐income women may have greater concerns about milk supply and that those experiencing food insecurity are more likely to stop breastfeeding exclusively earlier than recommended (Frank, 2015b; Li et al., 2008; Orr, Dachner, Frank, & Tarasuk, 2018). Formula must be provided if infants are not breastfeeding, but accessing formula is challenging for vulnerable mothers due to its high cost and precarious availability from community agencies. This was identified by our study participants and in previous research (Frank, 2015b; Partyka, Whiting, Grunerud, Archibald, & Quennell, 2010). This would suggest that such efforts are needed to ensure infant food security regardless of feeding type while also cultivating an enabling environment for breastfeeding. The conceptual model developed by Rollins et al. (2016) illustrates the complex determinants of breastfeeding, including structural, settings, and individual factors. They emphasize that “breastfeeding is generally thought to be an individual's decision and the sole responsibility of a woman to succeed, ignoring the role of society in its support and protection” (Rollins et al., 2016, p. 500).
A key strength of this research was the focus on vulnerable mothers' perspectives of breastfeeding and lactation support in Canada, which is lacking in the literature and needed in order to create effective breastfeeding support. Other strengths of this work include the strategies used to increase its rigour including a collaborative, iterative process to generate codes; analysis of all verbatim transcripts from interviews and focus groups, providing rich detail; a relatively large sample size, with saturation reached; and notes on reflections and discussions with the research team, including community partners, throughout the research process (Green & Thorogood, 2014). Breastfeeding is a complex physical, emotional, and social practice, therefore, qualitative methods are needed to better understand the implementation and effectiveness of interventions (Leeming, Marshall, & Locke, 2017; Zamora, Lutter, & Pena‐Rosas, 2015).
These results are specific to the program described, but key themes are transferable. Challenges described by study participants are commonly found in the literature, and postnatal breastfeeding support has been shown to be effective. The issue at hand is determining how to tailor breastfeeding support to different populations. The use of interpreters in the present study allowed us to gauge the experiences of women who do not speak English that comprise a significant fraction of CPNP participants; however, we acknowledge we did not assess the reliability of the interpretation. In future studies, confirmation of high‐level results with study participants, both non‐English and English speaking, should be considered. Selection bias is another limitation as study participants were those who self‐selected to participate. Those who declined participation or who could not be reached may not have had the same views regarding breastfeeding and the lactation support as study participants. Lastly, social desirability may be a limitation because study participants all received extensive support and free services from the prenatal and lactation support program, which might have made them hesitant to criticize aspects of the lactation support.
6. CONCLUSION
The CPNP promotes breastfeeding among vulnerable women, including low‐income mothers and newcomers to Canada; it does not formally fund postnatal lactation support. Our qualitative research examining the experiences of participants in one Toronto‐based CPNP with breastfeeding and enhanced community lactation support suggests provision of in‐home services by a skilled, non‐judgmental lactation consultant and an electric breast pump, if required, helped to address breastfeeding challenges. Next steps for this research include introduction of the described lactation support to additional CPNP sites and evaluation of its impact on breastfeeding outcomes. This research will help to assess scalability within the CPNP and should include a cost‐effectiveness analysis to ensure sustainability.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
JF, DS, and DLO conceptualized the study. JF, AM, DS, and DLO designed the study with input from SS, BU, VT, and EDR. The research was performed by JF and AM. Primary data analysis was conducted by JF, and AM assisted with data analysis. SS, BU, VT, EDR, DS, and DLO provided primary guidance on data interpretation. JF drafted the initial manuscript, and all authors approved the final manuscript.
Supporting information
Table S1. Focus group/interview guide
ACKNOWLEDGMENTS
We thank all mothers who took the time to participate in our focus groups and interviews. College‐Montrose Children's Place provided space to conduct focus group discussions. This study was supported by The Sprott Foundation and the Joannah and Brian Lawson Centre for Child Nutrition. The sources of funding had no role in the design or conduct of the research study, statistical analysis, data interpretation, or writing of the manuscript.
Francis J, Mildon A, Stewart S, et al. Vulnerable mothers' experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr. 2020;16:e12957 10.1111/mcn.12957
Deborah L. O'Connor, PhD, RD and Daniel Sellen, PhD are co‐senior authors.
REFERENCES
- Azad, M. B. , Vehling, L. , Chan, D. , Klopp, A. , Nickel, N. C. , McGavock, J. M. , … Subbarao, P. (2018). Infant feeding and weight gain: Separating breast milk from breastfeeding and formula from food. Pediatrics, 142, e20181092 10.1542/peds.2018-1092 [DOI] [PubMed] [Google Scholar]
- Balogun, O. O. , Dagvadorj, A. , Anigo, K. M. , & Sasaki, S. (2015). Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: A quantitative and qualitative systematic review. Maternal & Child Nutrition, 11, 433–452. 10.1111/mcn.12180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett, J. , Aguilar, S. , Brittner, M. , & Bonuck, K. (2012). Recruiting and retaining low‐income, multi‐ethnic women into randomized controlled trials: Successful strategies and staffing. Contemporary Clinical Trials, 33, 925–932. 10.1016/j.cct.2012.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker, G. E. , Smith, H. A. , & Cooney, F. (2015). Methods of milk expression for lactating women. Cochrane Database of Systematic Reviews, CD006170 10.1002/14651858.CD006170.pub4 [DOI] [PubMed] [Google Scholar]
- Best Start Resource Centre . (2014). Populations with lower rates of breastfeeding: A summary of findings . Retrieved from: https://resources.beststart.org/product/b09e-populations-lower-rates-breastfeeding-report/
- Bourke, B. (2014). Positionality: Reflecting on the research process. The Qualitative Report, 19, 1–9. [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun, V. , & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners (1st ed.). London: England: SAGE Publications Inc. [Google Scholar]
- Brockway, M. , Benzies, K. , & Hayden, K. A. (2017). Interventions to improve breastfeeding self‐efficacy and resultant breastfeeding rates: A systematic review and meta‐analysis. Journal of Human Lactation, 33, 486–499. 10.1177/0890334417707957 [DOI] [PubMed] [Google Scholar]
- Brown, C. R. L. , Dodds, L. , Legge, A. , Bryanton, J. , & Semenic, S. (2014). Factors influencing the reasons why mothers stop breastfeeding. Canadian Journal of Public Health, 105, e179–e185. 10.17269/cjph.105.4244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers, B. , Levitt, C. , Heaman, M. , O'Brien, B. , Sauve, R. , & Kaczorowski, J. (2009). Breastfeeding rates and hospital breastfeeding practices in Canada: A national survey of women. Birth, 36, 122–132. 10.1111/j.1523-536X.2009.00309.x [DOI] [PubMed] [Google Scholar]
- Chamberlain, L. B. , McMahon, M. , Phillip, B. L. , & Merewood, A. (2006). Breast pump access in the inner‐city: A hospital‐based initiative to provide breast pumps for low‐income women. Journal of Human Lactation, 22, 94–98. 10.1177/0890334405284226 [DOI] [PubMed] [Google Scholar]
- CPNP . (2015). About CPNP . Retrieved from: http://www.phac-aspc.gc.ca/hp-ps/dca-dea/prog-ini/cpnp-pcnp/about-apropos-eng.php
- Cresswell, J. W. , & Miller, D. L. (2000). Determining validity in qualitative inquiry. Theory Into Practice, 39, 124–130. 10.1207/s15430421tip3903_2 [DOI] [Google Scholar]
- Dennis, C. L. (1999). Theoretical underpinnings of breastfeeding confidence: A self‐efficacy framework. Journal of Human Lactation, 15, 195–201. 10.1177/089033449901500303 [DOI] [PubMed] [Google Scholar]
- DiGirolamo, A. , Thompson, N. , Martorell, R. , Fein, S. , & Grummer‐Strawn, L. (2005). Intention or experience? Predictors of continued breastfeeding. Health Education & Behavior, 32, 208–226. 10.1177/1090198104271971 [DOI] [PubMed] [Google Scholar]
- Felice, J. P. , Cassano, P. A. , & Rasmussen, K. M. (2016). Pumping human milk in the early postpartum period: Its impact on long‐term practices for feeding at the breast and exclusively feeding human milk in a longitudinal survey cohort. American Journal of Clinical Nutrition, 103, 1267–1277. 10.3945/ajcn.115.115733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank, L. (2015a). The breastfeeding paradox: A critique of policy related to food insecurity in Canada. Food, Culture & Society, 18, 107–129. 10.2752/175174415X14101814953927 [DOI] [Google Scholar]
- Frank, L. (2015b). Exploring infant feeding practices in food insecure households: What is the real issue? Food and Foodways, 23, 186–209. 10.1080/07409710.2015.1066223 [DOI] [Google Scholar]
- Garner, C.D. , Ratcliff, S.L. , Thornburg, L.L. , Wethington, E. , Howard, C.R. , Rasmussen, K. (2016). Discontinuity of breastfeeding care: “There's no captain of the ship”. Breastfeeding Medicine, 11, 32‐39. https:// 10.1089/bfm.2015.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatti, L. (2008). Maternal perceptions of insufficient milk supply in breastfeeding. Journal of Nursing Scholarship, 40, 355–363. 10.1111/j.1547-5069.2008.00234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gionet, L. (2013). Breastfeeding trends in Canada. Health at a Glance. Statistics Canada Catalogue no. 82‐624‐X.
- Green, J. , & Thorogood, N. (2014). Qualitative methods for health research (3rd ed.). London: Sage Publications Ltd. [Google Scholar]
- Hardison‐Moody, A. , MacNeil, L. , Elliot, S. , & Bowen, S. (2018). How social, cultural, and economic environments shape infant feeding for low‐income women: A qualitative study in North Carolina. Journal of the Academy of Nutrition and Dietetics, 118, 1886–1894. 10.1016/j.jand.2018.01.008 [DOI] [PubMed] [Google Scholar]
- Health Canada . (2015). Nutrition for healthy term infants: Recommendations from birth to six months . Retrieved from: https://www.canada.ca/en/health-canada/services/canada-food-guide/resources/infant-feeding/nutrition-healthy-term-infants-recommendations-birth-six-months.html [DOI] [PubMed]
- Kramer, M. S. , & Kakuma, R. (2012). Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews, (8), CD003517 10.1002/14651858.CD003517.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labiner‐Wolfe, J. , Fein, S. B. , Shealy, K. , & Wang, C. (2008). Prevalence of breast milk expression and associated factors. Pediatrics, 122(Supp2), S63–S68. 10.1542/peds.2008-1315h [DOI] [PubMed] [Google Scholar]
- Leeming, D. , Marshall, J. , & Locke, A. (2017). Understanding process and context in breastfeeding support interventions: The potential of qualitative research. Maternal & Child Nutrition, 13, e12407 10.1111/mcn.12407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , Chen, J. , & Grummer‐Strawn, L. M. (2008). Why mothers stop breastfeeding: Mothers' self‐reported reasons for stopping breastfeeding during the first year. Pediatrics, 122(Suppl. 2), S69–S76. 10.1542/peds.2008-1315i [DOI] [PubMed] [Google Scholar]
- McFadden, A. , Gavine, A. , Renfrew, M. J. , Wade, A. , Buchanan, P. , Taylor, J. L. , … MacGillivray, S. (2017). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews, CD001141 10.1002/14651858.CD001141.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier, P. P. , Patel, A. L. , Hoban, R. , & Engstrom, J. L. (2016). Which breast pump for which mother: An evidence‐based approach to individualizing breast pump technology. Journal of Perinatology, 36, 493–499. 10.1038/jp.2016.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra, A. K. , Khoury, A. J. , Hinton, A. W. , & Carothers, C. (2004). Predictors of breastfeeding intention among low‐income women. Maternal and Child Health Journal, 8, 65–70. 10.1023/B:MACI.0000025728.54271.27 [DOI] [PubMed] [Google Scholar]
- Nickel, N. C. , Marten, P. J. , Chateau, D. , Brownell, M. D. , Sarkar, J. , Goh, C. Y. , … the PATHS Equity Team (2014). Have we left some behind? Trends in socio‐economic inequalities in breastfeeding initiation: A population‐based epidemiological surveillance study. Canadian Journal of Public Health, 105, e362–e368. 10.17269/cjph.105.4499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom, E. C. , Li, R. , Scanlon, K. S. , Perrine, C. G. , & Grummer‐Strawn, L. (2013). Reasons for earlier than desired cessation of breastfeeding. Pediatrics, 131, e726–e732. 10.1542/peds.2012-1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr, S. K. , Dachner, N. , Frank, L. , & Tarasuk, V. (2018). Relationship between household food insecurity and breastfeeding in Canada. Canadian Medical Association Journal, 190, E312–E319. 10.1503/cmaj.170880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partyka, B. , Whiting, S. , Grunerud, D. , Archibald, K. , & Quennell, K. (2010). Infant nutrition in Saskatoon: Barriers to infant food security. Canadian Journal of Dietetic Practice and Research, 71, 79–84. 10.3148/71.2.2010.79 [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , & Geraghty, S. R. (2011). The quiet revolution: Breastfeeding transformed with the use of breast pumps. American Journal of Public Health, 101, 1356–1359. 10.2105/AJPH.2011.300136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … Victora, C. G. (2016). Why invest, and what it will take to improve breastfeeding practices? Lancet, 387, 491–504. 10.1016/S0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Saunders, B. , Sim, J. , Kingstone, T. , Baker, S. , Waterfield, J. , Bartlam, B. , … Jinks, C. (2017). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52, 1893–1907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmied, V. , Beake, S. , Sheehan, A. , McCourt, C. , & Dykes, F. (2011). Women's perceptions and experiences of breastfeeding support: A metasynthesis. Birth, 38, 49–60. 10.1111/j.1523-536X.2010.00446.x [DOI] [PubMed] [Google Scholar]
- Statistics Canada . (2012). Duration of exclusive breastfeeding in Canada: Key statistics and graphics (2009‐2010) . Retrieved from: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/duration-exclusive-breastfeeding-canada-key-statistics-graphics-2009-2010.html
- Statistics Canada . (2015). Low income cut‐offs (1992 base) before tax . Retrieved from: https://www150.statcan.gc.ca/n1/pub/75f0002m/2015002/tbl/tbl02-eng.htm
- Statistics Canada . (2019). Health characteristics, two‐year period estimates . Retrieved from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310011301&pickMembers%5B0%5D=1.1&pickMembers%5B1%5D=2.1&pickMembers%5B2%5D=3.1&pickMembers%5B3%5D=5.4
- Victora, C. G. , Bahl, R. , Barros, A. J. , Franca, G. V. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387, 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Victora, C. G. , Horta, B. L. , Loret de Mola, C. , Quevedo, L. , Pinheiro, R. T. , Gigante, D. P. , … Barros, F. C. (2015). Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: A prospective birth cohort study from Brazil. The Lancet Global Health, 3, e199–e205. 10.1016/S2214-109X(15)70002-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, E. A. , Chantry, C. J. , Dewey, K. G. , & Nommsen‐Rivers, L. A. (2013). Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics, 132, e865–e875. 10.1542/peds.2013-0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO , UNICEF (2017). Tracking progress for breastfeeding policies and programmes: Global breastfeeding scorecard 2017 . Retrieved from: https://www.who.int/nutrition/publications/infantfeeding/global-bf-scorecard-2017.pdf?ua = 1
- Win, N. N. , Binns, C. W. , Zhao, Y. , Scott, J. A. , & Oddy, W. H. (2006). Breastfeeding duration in mothers who express breast milk: A cohort study. International Breastfeeding Journal, 1(28), 28 10.1186/1746-4358-1-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2003). Global strategy for infant and young child feeding. Geneva: World Health Organization. [Google Scholar]
- Zamora, G. , Lutter, C. K. , & Pena‐Rosas, J. P. (2015). Using an equity lens in the implementation of interventions to protect, promote, and support optimal breastfeeding practices. Journal of Human Lactation, 31, 21–25. 10.1177/0890334414561477 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Focus group/interview guide


