Abstract
Purpose:
Healthcare access is important for achieving health equity across vulnerable social groups. However, stigma can be a barrier for accessing healthcare among Black transgender and gender diverse youth (TGDY) in the United States. Using a resilience approach, this paper examines the role of gender affirmation within healthcare to determine if it can mitigate the negative relationship between stigma and healthcare use.
Methods:
Data include responses from 110 Black TGDY from 14 U.S. cities. Multiple logistic regression models were fit to determine relationships between stigma in healthcare (anticipated and enacted), gender affirmation in healthcare, and delayed/non-use of primary care. Interaction terms were included to determine if gender affirmation moderates the relationship between stigma and healthcare non-use.
Results:
In the main effects model, gender affirmation was the only variable statistically associated with healthcare non-use. The interaction between gender affirmation and enacted stigma was not significant, but gender affirmation moderated the relationship between anticipated stigma and healthcare non-use. For individuals who did not have their gender affirmation needs met, as anticipated stigma increased, healthcare non-use also increased; however, this did not occur for those who had their gender affirmation needs met.
Conclusions:
Findings suggest that gender affirmation within healthcare is important for increasing access to care among Black TGDY. Interventions should consider how to increase gender affirmation among healthcare providers and within healthcare settings. Additional research using an intersectional approach to understand the experiences of Black TGDY is needed to highlight the unique healthcare needs of this population.
Keywords: Transgender, youth, healthcare, stigma, gender affirmation, resilience
In the United States, racial and ethnic minorities typically experience lower quality healthcare, with those in Black communities reporting medical mistrust, poor provider communication, and perceived discrimination when accessing healthcare [1, 2]. Black transgender and gender diverse youth (i.e., youth ages 16–24 whose gender identity is not the same as their sex assigned at birth; TGDY) experience stigma and discrimination related to their race and gender identity, resulting in poor health outcomes, unique healthcare needs, and inadequate access to appropriate healthcare services [3, 4]. Nevertheless, there is a dearth of research examining the healthcare needs and factors associated with healthcare use among Black TGDY. To improve healthcare access among Black TGDY, it is important to understand the mechanisms through which stigma influences healthcare utilization, including potential moderating factors that may help offset the effects of stigma and improve healthcare for Black TGDY.
Healthcare access is important for achieving health equity for Black TGDY [5]. Youth ages 16–24 are often transitioning from pediatric or adolescent care into adult care settings [6]. TGDY deserve providers who are knowledgeable about and respectful of their particular health concerns. Finding providers with this knowledge can be difficult; the 2015 U.S. Trans Survey (USTS) found that 24% of respondents needed to teach their provider about their own health [4]. Black TGDY also face a deeply-rooted history of racism within the U.S. medical system, resulting in many people of color experiencing and/or anticipating racism within healthcare settings, further complicating finding appropriate and competent primary care [7].
Black TGDY sometimes also seek additional services, such as medical gender affirmation (e.g., hormones) or preventative care and/or treatment related to additional health inequities experienced by this population (e.g., HIV, depression) [4, 8]. Low healthcare access contributes to these inequities [9], while these inequities increase healthcare needs. Despite having unique (and potentially more) healthcare needs, TGD populations are more likely to delay or not receive care than the general population [4, 10]; this may be largely due to stigma, a known barrier to healthcare access [11–13]. The frequency, severity, and consequences of multiple types of stigma (e.g., trans-related stigma, racism) are unique for Black TGDY, and therefore the way in which stigma influences healthcare is also specific to this population.
Black TGDY also disproportionately experience systematic vulnerability [4], social conditions (e.g., homelessness, poverty) that increase exposure to health risks [14]. Multiple types of stigma across social institutions (e.g., education, housing) can result in systematic vulnerability and reduced access to healthcare. This highlights how stigma increases health inequities and limits access to care for Black TGDY through mechanisms experienced within and outside of healthcare settings.
Minority stress theory is useful for conceptualizing the health effects of stigma toward Black TGDY. Minority stress is chronic psychological stress related to the experience of being stigmatized [15]. Minority stressors include both distal (e.g., discrimination, victimization, rejection) and proximal stressors (e.g., anticipated stigma, internalized stigma, identity concealment) [12, 15]. The theory posits that these stressors contribute to poorer health, as well as challenges in healthcare utilization, for Black TGDY [12, 15]. Qualitative research examining TGDY’s healthcare experiences has identified provider discrimination, anticipated stigma, and stigmatizing policies as considerable barriers to care [11, 16, 17].
Minority stress theory also highlights how promotive factors can improve the health of TGDY [18]. For Black TGDY, one way this may occur is as gender affirmation, a dynamic social process through which individuals receive support for their gender identity and expression [19]. For example, within healthcare, gender affirmation may involve having providers ask patients what pronouns they prefer and consistently using those pronouns, while a lack of gender affirmation may be reflected in intake forms that only include male/female options, erasing other gender identities [20, 21]. The gender affirmation framework highlights that appraisal of experienced gender affirmation is relative to an individual’s need for affirmation [21]. When an individual’s gender affirmation experiences are greater than their need, this may contribute to resilience [22].
Using an intersectionality framework [23], we understand that the experiences of Black-identified TGDY are fundamentally different than the experiences of TGDY who do not identify as Black; therefore, research focused specifically on how Black TGDY experience minority stressors and gender-related coping are warranted. Research has found that access to gender affirmation can moderate the relationship between stigma and poor health outcomes [19, 24]. However, no research to our knowledge has examined the moderating relationship that gender affirmation within healthcare may have on stigma and healthcare utilization for Black TGDY. Therefore, the purpose of this paper is to better understand the role of gender affirmation within healthcare settings by examining the relationships between stigma, gender affirmation, and healthcare non-use among Black TGDY.
Methods
Procedures.
This is a secondary analysis of cross-sectional survey data collected in 2015 for the Affirming Voices for Action (AVA) project, a mixed-methods study that used community-based participatory research (CBPR) principles to collect data from a diverse sample of 187 TGDY. AVA’s objective was to examine TGDY’s experiences across the HIV continuum of prevention and care. These data are appropriate for this analysis because measures include experiences of stigma in general healthcare settings, gender affirmation in healthcare, and delays in primary healthcare utilization. The current analysis focuses only on the quantitative data. Additional details on study methods are in [blinded].
Recruitment and study sample.
Given AVA’s mixed-methods design, purposive sampling was used. Participants were recruited across 14 U.S. cities (representing all U.S. regions) associated with the Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN). With the guidance of a Transgender Community Specialist (who is a member of the transgender community, hired to build connections with TGD communities), ATN staff recruited TGDY from their patient population and through community-based agencies serving TGDY. Individuals were eligible for participation if: their gender identity was not the same as their sex assigned at birth; they were age 16–24; and they were able to provide signed informed consent/assent. This analysis only includes Black/African American individuals, resulting in 122 participants.
Data collection.
Study activities were approved by the Institutional Review Boards at all 14 ATN sites and at [blinded]. The survey was administered at ATN sites using a computer-assisted self-interview and took approximately 45 minutes to complete. Participants were compensated for their time based on local standards.
Measures include primary healthcare use, experiences of stigma and gender affirmation within healthcare, and additional covariates. All stigma and gender affirmation scales were developed for this study and are described in Table 1.
Table 1:
Scale descriptions for gender affirmation and stigma within healthcare settings
| Scale | No. of Items | Response options | How it is calculated | Score Range | Sample Items | Cronbach’s Alpha |
|---|---|---|---|---|---|---|
| Need for gender affirmation | 8 | Strongly Disagree (0) Disagree (1) Agree (2) Strongly Agree (3) |
Mean score | 0–3 | “It is important to me that my preferred name and gender pronouns are always used at the places where I receive healthcare, including in the waiting room” “It is important to me that my health care provider is able to provide me resources and referrals that are affirming of my gender identity or gender expression” |
0.95 |
| Access to gender affirmation | 8 | Strongly Disagree (0) Disagree (1) Agree (2) Strongly Agree (3) |
Mean score | 0–3 | “My preferred name and gender pronouns are always used at the places where I receive healthcare, including in the waiting room” “My health care provider is able to provide me resources and referrals that are affirming of my gender identity or gender expression” |
0.88 |
| Enacted stigma | 12 | Strongly Disagree (0) Disagree (1) Agree (2) Strongly Agree (3) |
Mean score | 0–3 | “My healthcare provider has asked me inappropriate questions related to my gender identity or gender expression during a healthcare visit” “I have heard negative comments about my gender identity or gender expression from others while sitting in the waiting room of the places where I receive health care” |
0.96 |
| Anticipated stigma | 12 | Strongly Disagree (0) Disagree (1) Agree (2) Strongly Agree (3) |
Mean score | 0–3 | “I fear my healthcare provider will ask me inappropriate questions related to my gender identity or gender expression during a healthcare visit” “I fear I will hear negative comments about my gender identity or gender expression from others while sitting in the waiting room of the places where I receive health care.” |
0.96 |
Primary care use.
Consistent with other research conducted among TGD populations [4], primary healthcare use was measured as a binary variable based on agreement to the item: “In the past six months, I postponed or did not try to get check-ups or other preventative medical care.” Participants who selected indicated “not app licable” (n=28) were categorized as not having delayed care. The American Medical Association recommends an annual primary care visit for adolescents [25], so participants who did not need care in the past six months could have attained care within the previous year.
Gender affirmation.
Building on gender affirmation theory [19], and in collaboration with the study’s youth advisory board, innovative and appropriate measures were developed for capturing experiences of gender affirmation within healthcare. Two separate scales measured gender affirmation occurring in healthcare in the past 12 months, including the need for and access to gender affirmation. The need for gender affirmation scale asked participants about the importance of gender affirmation and the access to gender affirmation scale examined experiences of gender affirmation. Both scales demonstrated high internal consistency (Table 1).
A binary variable was created to measure whether a participant has greater access to gender affirmation than need. This variable was developed by taking the mean of both gender affirmation scales and then finding the difference between reported access and reported need. A difference of 0 or greater indicate that access to gender affirmation was greater than a participant’s need, and all results less than 0 indicate an unmet need for gender affirmation.
Stigma in the healthcare setting.
To reflect minority stress theory [15], stigma within healthcare was measured through two scales, including enacted stigma (measuring experiences of discrimination) and anticipated stigma (measuring expected discrimination) experienced in the past 12 months. Both scales demonstrated high internal consistency (Table 1).
Covariates include sociodemographic characteristics, systematic vulnerability, health coverage, and health status.
Sociodemographic characteristics examined in this analysis are: age, gender identity, and education. Gender identity includes trans-feminine (those who identify as a woman or transgender woman and were assigned male sex at birth), trans-masculine (those who identify as a man or transgender man and were assigned female sex at birth), and gender diverse (those who identify as genderqueer, gender non-conforming, or another gender). Education was measured as a dichotomous variable based on whether or not participants graduated high school (and are currently not in school). High school was used as the educational cutoff because participants are aged 16–24.
Systematic vulnerability captures aspects of structural stigma that limit access to resources, including the ability to obtain healthcare services [26]. An index was developed, calculating the sum of three binary (yes=1, no=0) variables, including lifetime experiences of incarceration, homelessness, and sex work; each point on the index (ranging from 0–3) indicates an additional experience of systematic vulnerability. Since these factors are often co-occurring [27], an index allows for an examination of the additive effect of multiple experiences of systematic vulnerability. Sensitivity analyses found no differences when aspects of systematic vulnerability were examined separately.
Health coverage was measured as a dichotomous variable based on whether or not an individual had any type of health insurance.
Health status.
Measured health outcomes include self-reported HIV status and depressive symptomatology. Depressive symptomatology was determined using the Center for Epidemiological Studies-Depression Scale, a 20-item scale used to identify depressive symptomology in the general population [28]. Respondents who scored ≥16 [28], were classified as experiencing clinically significant levels of depressive symptomatology.
Data Analysis was conducted using STATA 14 software (College Station, Texas). Descriptive statistics were computed and bivariate statistics (t-tests and chi-square tests) were examined. Multivariable logistic regression was used to determine if stigma and gender affirmation in healthcare are associated with delays/non-use of primary care. Interactions between gender affirmation and stigma were assessed to determine if gender affirmation moderates the relationship between stigma and delays in care. We fit three logistic regression models. Model 1 examined the relationships between delayed/non-use of primary care with stigma within healthcare (enacted and anticipated), gender affirmation in healthcare, and all covariates. Models 2 and 3 examined interactions between enacted stigma and gender affirmation (Model 2) and anticipated stigma and gender affirmation (Model 3). All responses with missing data (n=12) were excluded, resulting in 110 responses. There was no evidence of multicollinearity among the independent variables. An alpha level of 0.05 was used to determine significance for all analyses. Sensitivity analyses determined consistent results when examining regional differences; due to the small sample size, this was not included in the models.
Results
Descriptive statistics are described in Table 2. Approximately 28% of the sample reported delaying/not using healthcare in the past six months. Just over two-thirds of participants reported having their gender affirmation needs met within healthcare, and reports of enacted stigma (mean=0.82, SD=0.70) and anticipated stigma (mean=1.08, SD=0.80) were fairly low (scale=0–3). Participants who did not delay healthc are were much more likely to report having their gender affirmation needs met (84%), compared with individuals who delayed or did not use care (16%, p<0.001). The difference in anticipated stigma between groups who delayed (mean=1.32, sd=0.87) vs. those who did not delay care (mean=0.99, sd=0.75) was also statistically significant (p=0.04). The mean age of participants was 21 and most of the sample was trans-feminine (68%), with trans-feminine women reporting fewer delays in care (20%) than participants who identified as another gender (trans-masculine: 55%, gender diverse: 42%, p=0.015).
Table 2:
Descriptive Statistics of the Study Sample of Black Transgender and Gender Diverse Youth Ages 16–24 Years in the United States (n=110)
| Variables | Delayed or did not use health care | Did not delay health care | Total sample | Test statistic (χ2 or t-statistic) | p-value |
|---|---|---|---|---|---|
| (n=31) | (n=79) | (n=110) | |||
| Gender affirmation, % (n) | 17.28 | <0.001 | |||
| Gender affirmation needs met | 16.00% (12) | 84.00% (63) | 68.18% (75) | ||
| Gender affirmation needs not met | 54.29% (19) | 45.71% (16) | 31.82% (35) | ||
| Enacted stigma, mean (sd)a | 0.78 (0.80) | 0.83 (0.66) | 0.82 (0.70) | 0.29 | 0.770 |
| Anticipated stigma, mean (sd)a | 1.33 (0.87) | 0.99 (0.75) | 1.08 (0.80) | −2.06 | 0.042 |
| Age, mean (sd)b | 21.10 (1.86) | 20.94 (2.20) | 20.98 (2.11) | −0.36 | 0.722 |
| High school education, % (n) | 1.10 | 0.294 | |||
| Graduated or currently attending high school | 30.11% (28) | 69.89% (65) | 84.55% (93) | ||
| Did not graduate high school | 17.65% (3) | 82.35% (14) | 15.45% (17) | ||
| Gender identity, % (n) | 8.41 | 0.015 | |||
| Trans-feminine | 20.00% (15) | 80.00% (60) | 68.18% (75) | ||
| Trans-masculine | 54.55% (6) | 45.45% (5) | 10.00% (11) | ||
| Gender diverse | 41.67% (10) | 58.33% (14) | 21.82% (24) | ||
| Systematic vulnerability index, mean (sd)a | 1.26 (1.09) | 1.54 (1.08) | 1.46 (1.09) | 1.24 | 0.217 |
| Health coverage, %, (n) | 0.56 | 0.454 | |||
| Had health coverage | 26.67% (24) | 73.33% (66) | 81.82% (90) | ||
| Did not have health coverage | 35.00% (7) | 65.00% (13) | 18.18% (20) | ||
| HIV status, % (n) | 2.43 | 0.119 | |||
| Living with HIV | 19.51% (8) | 80.49% (33) | 37.27% (41) | ||
| Not living with HIV or status unknown | 33.33% (23) | 66.67% (46) | 62.73% (69) | ||
| Depressive symptomatology, % (n) | 3.62 | 0.057 | |||
| Clinically significant depressive symptoms | 34.85% (23) | 65.15% (43) | 60.00% (66) | ||
| No clinically significant depressive symptoms | 18.18% (8) | 81.82% (36) | 40.00% (44) | ||
| Total | 28.18% (31) | 71.82% (79) | (110) | ||
scale range=0–3
age range=16–24
sd=standard deviation
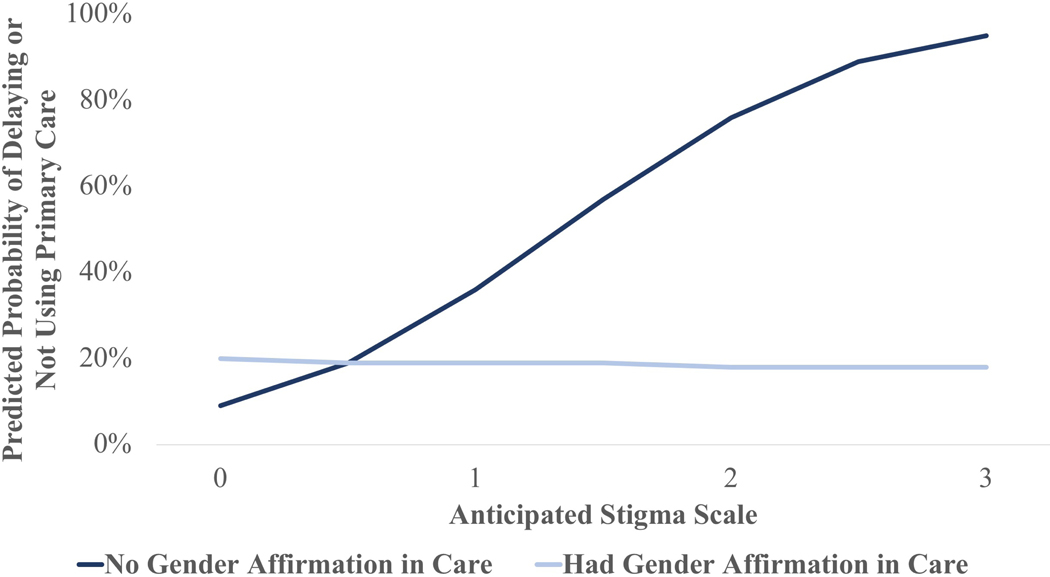
Results from Model 1 (without any interaction terms) demonstrated that the only variable significantly associated with delayed/non-use of healthcare was the experience of gender affirmation within the healthcare setting (Table 3). Participants who reported having their gender affirmation needs met within healthcare were 73% less likely to report delaying or not using healthcare (p=0.012). The interaction between enacted stigma and gender affirmation (Model 2) was not statistically significant; however, results from Model 3 demonstrated a significant interaction between anticipated stigma and gender affirmation on healthcare use (p=0.016; Table 4). Figure 1 demonstrates that for participants who did not have their gender affirmation needs met, the predicted probability of delaying care increased as anticipated stigma increased (from 9% for individuals reporting a 0 on the anticipated stigma scale to 95% among individuals reporting a 3). However, for participants who did have their gender affirmation needs met, their predicted probability of delaying or not using care did not change as anticipated stigma increased.
Table 3:
Results from Multivariable Logistic Regression Model: Delayed or Did Not Use Health Care in the Last 6 Months Among Black Transgender and Gender Diverse Youth in the United States (n=110)
| Adjusted OR | 95% CI | p-value | |
|---|---|---|---|
| Gender affirmation | 0.27 | 0.10,0.75 | 0.012* |
| Enacted stigma | 0.46 | 0.19,1.13 | 0.091 |
| Anticipated stigma | 1.85 | 0.89,3.88 | 0.101 |
| Age | 1.10 | 0.86,1.40 | 0.455 |
| High school education | 1.55 | 0.34,7.14 | 0.572 |
| Gender identity | |||
| Trans-feminine | referent | ||
| Trans-masculine | 2.11 | 0.43,10.49 | 0.360 |
| Gender diverse | 1.92 | 0.56,6.56 | 0.298 |
| Systematic vulnerability | 0.75 | 0.45,1.26 | 0.282 |
| Health coverage | 0.48 | 0.13,1.82 | 0.282 |
| HIV status | 0.62 | 0.20,1.96 | 0.415 |
| Depressive symptomatology | 3.14 | 0.95,10.34 | 0.060 |
p<0.05
OR = Odds Ratio; 95% CI = 95% Confidence Interval
Table 4:
Results from Multivariable Logistic Regression Model with Interaction Term Exploring How Gender Affirmation Moderates the Relationship Between Anticipated Stigma and Delayed/Non-Use of Healthcare in the Last 6 Months Among Black Transgender and Gender Diverse Youth in the United States (n=110)
| OR | 95% CI | p-value | |
|---|---|---|---|
| Gender affirmation | 2.88 | 0.33,25.19 | 0.339 |
| Anticipated stigma | 7.48 | 1.60,35.00 | 0.011* |
| Gender affirmation x Anticipated stigma | 0.13 | 0.02,0.68 | 0.016* |
| Enacted stigma | 0.42 | 0.15,1.16 | 0.092 |
| Age | 1.03 | 0.79,1.35 | 0.813 |
| High school education | 1.55 | 0.32,7.60 | 0.588 |
| Gender identity | |||
| Trans-feminine | referent | ||
| Trans-masculine | 3.50 | 0.59,20.78 | 0.169 |
| Gender diverse | 1.95 | 0.53,7.14 | 0.315 |
| Systematic vulnerability | 0.90 | 0.53,1.54 | 0.695 |
| Health coverage | 0.50 | 0.12,2.01 | 0.328 |
| HIV status | 0.72 | 0.22,2.39 | 0.597 |
| Depressive symptomatology | 3.19 | 0.95,10.67 | 0.060 |
p<0.05
OR = Odds Ratio; 95% CI = 95% Confidence Interval
Figure 1:
The role of gender affirmation in healthcare as a moderating factor between anticipated stigma and the predicted probability of delaying or not using primary healthcare among Black transgender youth (n=110)
Discussion
Results from this national sample demonstrate the importance of gender affirmation in the healthcare system for Black TGDY in the United States. Reports in delaying care (28%) were consistent with previous findings from the USTS, which indicates that 26% of Black TGD individuals reported delaying care because of anticipated stigma and 40% reported delaying care because of cost [4]. While other studies have focused on healthcare delays for specific reasons [4], this study is unique for asking participants about healthcare delays without specifying reasons for delaying care, and then examining factors related to delays.
The current study builds on extant literature through the use of a resilience approach [22] that recognizes how gender affirmation can moderate the relationship between stigma and healthcare delays/non-use. Findings demonstrate that the relationship between anticipated stigma and delaying care can be mitigated by meeting gender affirmation needs of Black TGDY. This relationship was not significant for enacted stigma; it is possible that experiencing stigma in healthcare may be a stronger deterrent for delaying/not using care. When an individual experiences stigma (as opposed to only expecting it), additional mechanisms beyond gender affirmation may be needed to prevent non-use of care. Still, findings highlight the importance of utilizing a resilience framework with Black TGDY. Most research aiming to understand TGD experiences of health and healthcare focuses on negative experiences [29]. However, a resilience approach is needed to holistically understand and improve Black TGDY’s experiences within healthcare.
Programmatic Implications
To increase healthcare access for Black TGDY, it is important that healthcare providers, environments, and policies use an intersectional approach that recognizes multiple axes of oppression experienced by Black TGDY and provide care that is gender-affirming, youth-friendly, and actively addresses racism [7, 30]. To achieve this, it is necessary to train healthcare providers on the specific needs of Black TGDY [13, 17]. In 2009–2010, a study examining 150 U.S. and Canadian medical schools found that the median time spent focusing on sexual and gender minority (SGM) needs in the entire medical curriculum was only five hours [31]. Some research has demonstrated improvements over time [32], but progress is still needed to train medical professionals on the gender affirmation needs of Black TGDY. Studies have found that providers’ lack of knowledge can decrease their overall comfort, limit their understanding of medical protocols specific to TGD patients, reduce their ability to provide appropriate referrals, and even increase the perpetration of gender-related discrimination by the provider [17, 33].
We must also consider healthcare environments. Though most research addressing healthcare experiences of TGDY has not focused on the physical environment, previous research with other populations has highlighted its importance for accessibility and cultural appropriateness of care [34, 35]. One study examining experiences of young gay and bisexual men found that physical attributes of HIV testing sites (e.g., materials in waiting rooms aimed at SGMs, inclusive language in medical forms) were important for the accessibility of culturally appropriate care [34]. These aspects of accessibility, and physical cues demonstrating inclusivity, contribute to the promotion of gender affirmation within healthcare [35].
Cultural humility training can also be useful for increasing gender affirmation and reducing racial discrimination within healthcare. Distinct from cultural competency, cultural humility involves a lifelong process of self-reflection and self-evaluation of the power dynamics occurring between providers and their patients who hold various marginalized identities [36]. Providers could benefit from training focused on cultural humility either within an educational curriculum or as a separate TGD-specific training. One example is the Health Access Initiative, which provides training to providers on culturally humble practices using an intersectional lens, and offers technical assistance to improve healthcare environments’ inclusivity of SGM youth [37]. TGD-specific services can also be provided by having separate SGM-centered clinics, such as Fenway Health, a research institute and health clinic that provides SGM-specific services in the Boston area [38]. Individuals may differ in their preferences for accessing care, so simultaneously using multiple approaches (e.g., creating TGD-specific healthcare spaces and equipping general healthcare settings to better address the needs of TGD populations) could be most successful for improving access to care.
Research Implications
Future research should consider applying an intersectional approach to better understand the experiences of marginalized groups who simultaneously experience multiple forms of stigma, such as Black TGDY. An intersectional lens that considers how multiple aspects of identity are not additive, but comprise different lived experiences [23, 30], is important for understanding differences in experiences across people with different social identities. Even though Black TGDY comprise a small proportion of the general U.S. population, it is important to understand their specific experiences because they are distinct from other TGD populations or other Black populations. Failure to understand the specific experiences of Black TGDY can result in increased health inequities [14].
This research also expands the application of minority stress theory, which focuses on experiences of mental and physical health among SGMs [12]. However, the current study highlights that this theory can also be applied to experiences of specific TGD communities and to other health outcomes, including healthcare utilization. Additionally, this research applies gender affirmation theory in new ways. Gender affirmation was originally explored as a process occurring within social relationships (and especially romantic and/or sexual relationships); this study highlights that it is also important to understand how gender affirmation occurs within social institutions (such as healthcare), and how this may influence access to and use of resources.
Limitations and Strengths
There were some limitations in this study. Causal effects cannot be determined due to the cross-sectional research design. Instead, this study provides insight into relationships between stigma, gender affirmation, and healthcare use. Caution should be taken before generalizing results to Black TGDY outside of the ATN catchment areas included in this study. Though common among hard-to-reach populations, this study uses convenience sampling, which limits generalizability [39]. The small sample size is also a limitation, impacting the statistical precision of parameter estimates; however, since Black TGDY are a hard-to-reach population, this sample is exceptionally large compared with other research on specific TGD populations [40]. There was also an especially small number of trans-masculine participants included in the analysis (n=11), resulting in difficulty assessing differences across gender identity. The small sample size limited the number of independent variables included in the models; therefore, variables most consistent with theoretical and empirical findings were selected. Furthermore, additional variables of interest were not included in the survey, such as: race-based minority stressors, community connectedness, and availability of healthcare. Future research would benefit from including these in surveys with TGD participants. It is also important to note that the AVA study design (including study measures) focused on understanding the HIV prevention and care continua among a diverse sample of TGDY, but the number of participants who identified with a racial group other than Black was not large enough to make comparisons between racial/ethnic groups. Therefore, this study highlights race-specific experiences of Black TGDY, but it does not elucidate whether or not these experiences are unique to Black TGDY.
Despite limitations, this study has many strengths. The study used CBPR principles to ensure the research is relevant to the lives of Black TGDY, and used innovative measures to examine experiences of stigma and gender affirmation within healthcare. Gender affirmation has been identified as an important construct that may be valuable for interventions addressing the needs of Black TGDY [19, 24]; however, little research has examined experiences of gender affirmation and no previous research has quantitatively examined experiences of gender affirmation within the healthcare setting for Black TGDY.
Conclusions
As research with TGD populations continues, it will be important to use an intersectionality framework to examine the health needs and experiences of sub-groups within TGD populations [23]. Black TGDY have unique experiences from other TGD populations and other Black populations; therefore, a greater understanding of their specific needs and experiences related to health and stigma is important for reducing health inequities. This research demonstrates the importance of gender affirmation and stigma to Black TGDY’s healthcare access, and the need to focus research, interventions, and political advocacy on the healthcare needs of Black TGDY. Additional work to better understand how to increase gender affirmation within healthcare for Black TGDY is important for increasing healthcare access and utilization among this population.
Implications and Contributions:
This study explores the relationships between stigma within healthcare (enacted and anticipated), gender affirmation within healthcare, and healthcare non-use among Black transgender and gender diverse youth. Using a resilience approach, this study finds that gender affirmation within healthcare mitigates the relationship between anticipated stigma and healthcare non-use.
Acknowledgements:
This work was supported by The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) from the National Institutes of Health [U01 HD 040533 and U01 HD 040474] through the National Institute of Child Health and Human Development (B. Kapogiannis, S. Lee), with supplemental funding from the National Institutes on Drug Abuse and Mental Health. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. Government. We would also like to thank the investigators and staff at the following sites that participated in this study: University of South Florida, Tampa (Emmanuel, Straub, Bruce, Kerr), Children’s Hospital of Los Angeles (Belzer, Tucker, Franco), Children’s National Medical Center (D’Angelo, Trexler, Carr, Sinkfield), Children’s Hospital of Philadelphia (Douglas, Tanney, DiBenedetto, Franklin, Smith), John H. Stroger Jr. Hospital of Cook County and the Ruth M. Rothstein CORE Center (Henry-Reid, Bojan, Balthazar), Montefiore Medical Center (Futterman, Campos, Wesp, Nazario, Reopell), Tulane University Health Sciences Center (Abdalian, Kozina, Baker, Wilkes), University of Miami School of Medicine (Friedman, Maturo), St. Jude’s Children’s Research Hospital (Gaur, Flynn, Dillard, Hurd-Sawyer), Baylor College of Medicine (Paul, Head, Sierra), Wayne State University (Secord, Cromer, Walters, Houston), Johns Hopkins University (George-Agwu, Anderson, Worrel-Thorne), Fenway Institute (Mayer, Dormitzer, Massaquoi, Gelman), University of Colorado Denver (Reirden, Hahn, Bernath). Network, scientific and logistical support was provided by the ATN Coordinating Center (C. Wilson, C. Partlow) at The University of Alabama at Birmingham and the ATN 130 protocol team. Network operations and data management support was provided by the ATN Data and Operations Center at Westat, Inc. (G. Price). The authors are grateful to the members of the Affirming Voices for Action (AVA) Youth Advisory Board for their insight and guidance. We would like to thank the trans youth who raised their voices and shared their experiences with us. We hear you.
Abbreviations:
- ATN
Adolescent Medical Trials Network for HIV/AIDS Interventions
- AVA
Affirming Voices for Action Project
- CBPR
Community-based participatory research
- LGBT
Lesbian, gay, bisexual, and transgender
- OR
Odds ratio
- SD
Standard deviation
- TGD
Transgender and gender diverse
- TGDY
Transgender and gender diverse youth
- USTS
U.S. Trans Survey
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature Cited
- 1.Cuevas AG, O’Brien K, and Saha S, African American experiences in healthcare:“I always feel like I’m getting skipped over”. Health Psychology, 2016. 35(9): p. 987. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine, Unequal Treatment: Confronting racial adn Ethnic Disparities in Health Care. 2003: Washington, DC. [PubMed] [Google Scholar]
- 3.Grossman AH and D’augelli AR, Transgender youth: Invisible and vulnerable. Journal of homosexuality, 2006. 51(1): p. 111–128. [DOI] [PubMed] [Google Scholar]
- 4.James SE, et al. , The Report of the 2015 U.S. Transgender Survey. 2016, National Center for Transgender Equity: Washington, DC. [Google Scholar]
- 5.U.S. Department of Health and Human Services. Healthy People 2020: Access to Health Services. 2014; Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/Access-to-Health-Services.
- 6.Crowley R, et al. , Improving the transition between paediatric and adult healthcare: a systematic review. Archives of disease in childhood, 2011. 96(6): p. 548–553. [DOI] [PubMed] [Google Scholar]
- 7.Washington HA, Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. 2006: Doubleday Books. [Google Scholar]
- 8.Bauermeister JA, et al. , Psychosocial Disparities Among Racial/Ethnic Minority Transgender Young Adults and Young Men Who Have Sex with Men Living in Detroit. Transgender Health, 2016. 1(1): p. 279–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seelman KL, et al. , Transgender noninclusive healthcare and delaying care because of fear: Connections to general health and mental health among transgender adults. Transgender Health, 2017. 2(1): p. 17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macapagal K, Bhatia R, and Greene GJ, Differences in Healthcare Access, Use, and Experiences Within a Community Sample of Racially Diverse Lesbian, Gay, Bisexual, Transgender, and Questioning Emerging Adults. LGBT health, 2016. 3(6): p. 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gridley SJ, et al. , Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. Journal of Adolescent Health, 2016. 59(3): p. 254–261. [DOI] [PubMed] [Google Scholar]
- 12.Hendricks ML and Testa RJ, A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychology-Research and Practice, 2012. 43(5): p. 460. [Google Scholar]
- 13.White-Hughto JM, Reisner SL, and Pachankis JE, Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social science & medicine, 2015. 147: p. 222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frohlich KL and Potvin L, Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. American journal of public health, 2008. 98(2): p. 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer IH, Minority stress and mental health in gay men. Journal of health and Social Behavior, 1995: p. 38–56. [PubMed] [Google Scholar]
- 16.Kosenko K, et al. , Transgender patient perceptions of stigma in health care contexts. Medical care, 2013. 51(9): p. 819–822. [DOI] [PubMed] [Google Scholar]
- 17.Poteat T, German D, and Kerrigan D, Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Social science & medicine, 2013. 84: p. 22–29. [DOI] [PubMed] [Google Scholar]
- 18.Meyer IH, Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity, 2015. 2(3): p. 209. [Google Scholar]
- 19.Sevelius JM, Gender affirmation: A framework for conceptualizing risk behaviour among transgender women of color. Sex roles, 2013. 68(11–12): p. 675–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Human Rights Campaign Foundation, Healthcare Equality Index 2018: Rising to the New Standard of Promoting Equitable and Inclusive Care for Lesbian, Gay, Bisexual, Transgender & Queer Patients and Their Families. 2018. [Google Scholar]
- 21.Jadwin-Cakmak L, et al. , Transgender adolescents: care and support, in HIV Specialist Magazine, Gatty R, Editor. 2015, The American Academy of HIV Medicine: Washington, DC: p. 12–17. [Google Scholar]
- 22.Fergus S. and Zimmerman MA, Adolescent resilience: A framework for understanding healthy development in the face of risk. Annu. Rev. Public Health, 2005. 26: p. 399–419. [DOI] [PubMed] [Google Scholar]
- 23.Crenshaw K, Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford law review, 1991. 43(6): p. 1241–1299. [Google Scholar]
- 24.Crosby RA, Salazar LF, and Hill BJ, Gender Affirmation and Resiliency Among Black Transgender Women With and Without HIV Infection. Transgender Health, 2016. 1(1): p. 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elster A. and Kuznets N, Guidelines for adolescent preventive services. 1994, Baltimore, MD: Williams Wilkins. [Google Scholar]
- 26.Hatzenbuehler ML, Phelan JC, and Link BG, Stigma as a fundamental cause of population health inequalities. American journal of public health, 2013. 103(5): p. 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brennan J, et al. , Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. American journal of public health, 2012. 102(9): p. 1751–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radloff LS, The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement, 1977. 1(3): p. 385–401. [Google Scholar]
- 29.MacCarthy S, et al. , The time is now: attention increases to transgender health in the United States but scientific knowledge gaps remain. LGBT health, 2015. 2(4): p. 287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bowleg L, The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. American journal fo public health, 2012. 102(7): p. 1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Obedin-Maliver J, et al. , Lesbian, gay, bisexual, and transgender–related con tent in undergraduate medical education. JAMA, 2011. 306(9): p. 971–977. [DOI] [PubMed] [Google Scholar]
- 32.Honigberg MC, et al. , Curricular Time, Patient Exposure, and Comfort Caring for Lesbian, Gay, Bisexual, and Transgender Patients Among Recent Medical Graduates. LGBT health, 2017. 4(3): p. 237–239. [DOI] [PubMed] [Google Scholar]
- 33.Vance SR, Halpern-Felsher BL, and Rosenthal SM, Health care providers’ comfort with and barriers to care of transgender youth. Journal of Adolescent Health, 2015. 56(2): p. 251–253. [DOI] [PubMed] [Google Scholar]
- 34.Bauermeister JA, et al. , The use of mystery shopping for quality assurance evaluations of HIV/STI testing sites offering services to young gay and bisexual men. AIDS and Behavior, 2015. 19(10): p. 1919–1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Makadon HJ, et al. , The Fenway Guide to Lesbian, Gay, Bisexual, and Transgender Health, 2nd Edition 2015, Philadelpha, PA: American College of Physicians. [Google Scholar]
- 36.Tervalon M. and Murray-Garcia J, Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of health care for the poor and underserved, 1998. 9(2): p. 117–125. [DOI] [PubMed] [Google Scholar]
- 37.Bauermeister JA, et al. , Ensuring community participation during program planning: Lessons learned during the development of a HIV/STI program for young sexual and gender minorities. American journal of community psychology, 2017. 60(1–2): p. 215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reisner SL, et al. , Comprehensive transgender healthcare: the gender affirming clinical and public health model of fenway health. Journal of Urban Health, 2015. 92(3): p. 584–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muhib F, et al. , A venue-based method for sampling hard-to-reach populations. Public Health Rep, 2001. 116: p. 216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reisner SL, et al. , Global health burden and needs of transgender populations: a review. The Lancet, 2016. 388(10042): p. 412–436. [DOI] [PMC free article] [PubMed] [Google Scholar]