Abstract
Background:
Hop tests are commonly used within a testing battery to assess readiness for return to sport after anterior cruciate ligament (ACL) injury, yet athletes still experience a high rate of re-injury. Simultaneous performance of a secondary task requiring cognitive processing or decision-making may test the athlete under more realistic contexts.
Purpose:
To examine a clinically feasible, dual-task assessment paradigm applied during functional hop tests in healthy individuals.
Study Design:
Repeated measures
Methods:
Participants performed the crossover triple hop for distance (XHOP) and medial triple hop for distance test (MHOP) under three separate conditions: standard procedures and two dual-task protocols including the backward digit span memory task and a visuospatial recognition task. The visuospatial task involved briefly displaying an image consisting of 18 randomly placed red and blue circles on a screen, where the participant was asked to identify the number of red circles in each image. The backward digit span task was applied by introducing a sequence of random numbers to the participants, who were required to repeat the sequence in reverse order. Each motor and cognitive task was performed independently and simultaneously, in accordance with the dual-task paradigm.
Results:
Thirty-four healthy participants (age: 24.0 ± 3.9 years) completed testing procedures. No differences in hop distance were observed with the simultaneous application of a cognitive task, with the exception of the backward digit span memory task resulting in decreased hop distance (p = 0.04, d = 0.14). There were no differences in cognitive accuracy according to hop test type, although the effect size was greater for the XHOP (p = 0.08, d = 0.49) compared to the MHOP (p = 1.0, d = 0.07). The dual-task protocol revealed good-excellent within- (ICC3,1 = 0.85 – 0.99) and between-session (ICC3,k = 0.94 – 0.99) intrarater reliability for hop distance across all dual-task conditions. The addition of a cognitive task to the XHOP and MHOP resulted in a lower standard error of measurement and decreased minimal detectable change, as compared to standard testing procedures.
Conclusion:
The simultaneous application of a cognitive task did not alter hop distance, with the exception of the backward digit span memory task resulting in decreased hop distance with a trivial effect size. There were no differences in cognitive accuracy according to task type (sitting, XHOP, MHOP). All combinations of dual-task assessment demonstrated good-excellent within- and between-session intrarater reliability among healthy individuals, but measurement precision was deficient.
Level of Evidence:
2b
Keywords: anterior cruciate ligament, cognition, dual-task, functional performance, knee
INTRODUCTION
Dual-tasking is “the concurrent performance of two tasks that can be performed independently, measured separately and have distinct goals.”1,p.2 One type of dual-tasking includes motor and cognitive performance assessment, which has been applied to injured athletic populations such as those with concussion,2,3 anterior cruciate ligament (ACL) injury,4,5 and functional ankle instability.6 Despite motor performance being frequently assessed as part of the return to play decision making process after lower extremity (LE) injury,7 cognitive assessment remains less common in clinical settings. Historically, cognitive tasks applied to those with ACL injury or ACL reconstruction (ACLR) within a dual-task paradigm have included various arithmetic,8 working memory,5 or auditory tasks9 while other athletic populations have been subjected to the use of visuospatial tasks.10 While the relevance of such cognitive tasks to athletic participation may be in question, it has been observed that soccer athletes with ACL injury sacrifice cognitive task performance in order to maintain motor performance under dual-task conditions.5 Therefore, it may be prudent to capture how cognitive task performance influences the use in a dual-task paradigm.
Patients who return to play after LE injury must meet various subjective and objective test criteria. Some objective measures traditionally used by rehabilitation specialists include measure of strength, balance, and functional testing. Functional tests may include a series of hop and agility tests.11 The most common hop tests used after ACLR include the single leg hop for distance, triple hop for distance, crossover triple hop for distance (XHOP), and timed 6-m hop.7 These tests are considered to be reliable (ICC = 0.82 – 0.93) and valid in terms of outcomes after ACLR, with differences in overall limb symmetry index being reported as moderately correlated with Global Rating of Change Scores (r = 0.58).12 Of these four hop tests, the XHOP demonstrated the highest sensitivity in identifying those with normal knee function after ACLR when achieving an optimal cutoff score of 94.9% limb symmetry index (sensitivity = 0.88).13 Furthermore, young athletes with ACLR who returned to their preinjury level of sport participation hopped farther (normalized to height) on a hop test battery consisting of the single leg hop for distance, triple hop for distance, and XHOP compared to those who did not return to sport; however, hop test limb symmetry did not differentiate between the two groups in terms of resuming preinjury levels of sport participation.14
Clinically, limb symmetry indices have been used to quantify performance of the involved versus uninvolved limb. A mean limb symmetry index of 95% was reported in athletes 6-7 months post-ACLR using the single leg hop for distance, triple hop for distance, and side hop test; although, the authors noted that limb symmetry indices may overestimate return to sport readiness given bilateral hop test performance deficits exist in those with ACLR.15 In addition, despite achievement of ≥ 85% (median) limb symmetry on several indices of hop performance at six months postoperatively, 20% of patients still had self-reported knee function scores (IKDC 2000) below normal ranges at 12 months.13 Finally, a recent systematic review with meta-analysis indicated that achieving a passing score on return to sport criteria after ACLR was not significantly associated with risk of sustaining a second ACL injury.16 Although hop tests have been reported to possess clinical value after ACLR, their application is not unlimited.
Some have used alternating side hops for 30 seconds duration hop test to identify limb performance deficiencies between individuals with ACL injury and ACLR.17 Another single leg hop test performed in the frontal plane, the medial triple hop for distance test (MHOP), has been reported to measure performance deficiencies between limbs according to sport in healthy athletes, as well as clinical populations with hip pain.18,19 Interestingly, a lateral triple hop for distance test did not capture between limb differences in healthy collegiate female basketball and soccer athletes.18 Further exploring the reliability and responsiveness of these frontal plane hop tests in uninjured populations may set the foundation for future research regarding their potential clinical utility.
Hop tests aim to gauge the physical performance of several constructs important to athletic activity, including neuromuscular control and power. It has been recognized that performance of a secondary, or cognitive, task may expose the athlete to more realistic contexts that require cognitive processing or decision-making. To better replicate the physical and cognitive demands of the athletic environment, efforts have been undertaken to evaluate the influence of divided attention on LE performance measures in response to relevant, cognitively demanding tasks. For example, the impact of divided attention has been investigated during the drop vertical jump20-23 and single-leg cutting tasks.24-27 Under dual-task conditions (counting backward) during a jump-landing task, LE movement patterns were more consistent with those experienced during noncontact ACL injury mechanisms, in addition to a reduction in vertical jump height.22 Similarly, performance of a single-leg cutting maneuver under dual-task conditions resulted in reduced peak stance knee flexion angle and hip flexion moment, and increased knee external rotation angle.28
Dual-task motor and/or cognitive deficits have been identified in those with ACL-deficiency and ACLR. Athletes with ACLR prioritized postural control during single limb stance at the expense of cognitive performance (auditory Stroop task) under dual-task situations, which was not observed in the control group.4 Similarly, dual-tasking (working memory task) negatively affected single limb stance to a greater degree versus single-task conditions in those with ACLR compared to healthy individuals.29 Further, individuals with ACL-deficiency demonstrated increased step width coefficient of variance under dual-task conditions consisting of treadmill walking while concurrently performing an auditory Stroop task.30 Unfortunately, these results have been obtained through the use of expensive laboratory equipment and the use of trained personnel not available in most outpatient orthopedic settings. Therefore, the purpose of this study was to examine a clinically feasible, dual-task assessment paradigm applied during functional hop tests in healthy individuals.
Methods
Participants
Researchers recruited from a sample of convenience that targeted healthy participants. Those eligible for the study included those who were young adults (age 18-35), were currently physically active, had past participation in organized cutting/jumping sports at the high school or college level(s), and were fluent in English. Exclusion criteria were the following: 1) history of neurological disorder or conditions that affect balance; 2) injury or surgery within the prior six months to the back or LEs; 3) prior ligamentous knee injury; 4) report of pain in either LE (at least 2/10 as measured by the numeric pain rating scale); 5) incidence of concussion or concussion-related symptoms (e.g., recurrent headaches or migraines, oculomotor deficits, balance disturbances) within the prior five years; 6) any medically diagnosed condition that may have affected their cognition or attention (i.e. ADHD), a hearing impairment (uncorrected), uncorrected visual impairment (including colorblindness); and 7) those who were pregnant. An a priori power analysis indicated that 27 participants were required to achieve 80% study power at an alpha level of 0.05, with a partial eta squared effect size (medium) of 0.06.31 The power analysis was estimated using the G*Power software (Version 3.1, University of Dusseldorf, Dusseldorf, Germany).32 All participants signed an informed consent form prior to data collection, where the research protocol was approved by the research institution's Institutional Review Board. To establish testing reliability, twelve of the participants agreed to return for a repeat test session within 48-72 hours.
Procedures
Demographic information including gender, age, height, mass, and years of high school/college education completed, as well as prior athletic history (i.e., sport(s) participation, years and level of playing experience, and current Tegner activity level score) was collected. The Tegner activity level scale ranges from 0-10, and is applied as a self-reported measure of physical activity.33 Due to the divergent definitions of limb dominance in various sports (kicking a ball vs. jumping limb), limb dominance was not recorded.18
Hop tests
Standardized warm up procedures included bodyweight double-leg squats (2 sets x 8 repetitions) and double-leg, maximal vertical jumps (2 sets x 5 repetitions) prior to the XHOP and MHOP.24,34,35 Rest time of 30 seconds was allowed after the warm up. In order to be mindful of potential testing fatigue, participants performed the hop tests on separate limbs (XHOP on left leg, MHOP on right leg). Standard hop test limb selection was considered in light of similar hop distances having been reported in nondominant/dominant limbs for a group of healthy control athletes during the XHOP (96.8-98.5% limb symmetry).11 Similarly, a high level of limb symmetry (right/left) was reported for collegiate female soccer and basketball athletes during the MHOP (96.7% limb symmetry).18
One practice trial and two test trials were allowed per condition, with the mean of the two test trials used for analysis. A minimum of 30 seconds of rest time was allowed between test trials,22 and participants verbally reported recovery prior to commencing further testing with extra rest time allowed as needed. The XHOP and MHOP test conditions performed in this study were completed as part of a larger test battery. The XHOP and MHOP were carried out similarly to previous investigations.18,36,37
A vinyl, custom ruler (15-cm x 10-m) with one-centimeter increments (Oregon Rule Co., Oregon City, OR) was placed along a vinyl floor. Participants began the XHOP in left single leg stance and completed three consecutive forward single leg jumps with the left limb while alternately hopping over the tape measure. The direction of the initial hop was relative to the left stance limb, where the participant first hopped over the tape measure laterally, medially, and once again laterally. Performance was assessed according to the distance measured at the great toe upon landing.
Participants completed the MHOP in right single limb stance by positioning their right foot perpendicular to the long edge of the measuring tape, with the medial aspect of their foot behind a clearly marked starting line. Next, participants performed three consecutive hops in the medial direction (i.e. toward the left) of their right stance limb. Participants maintained their foot in a perpendicular position upon landing. Measurements were recorded from the most medial aspect of the shoe.
A controlled landing of two seconds duration was required for successful completion of both the XHOP and MHOP.12 Criteria for unsuccessful trials were as follows: losing balance, requiring several hops when landing, or touching down of the non-stance limb. If unsuccessful, the test was repeated. If needed, up to five total attempts per condition were allowed in order for participants to achieve their two successful trials.
Blinding of measurements (tape measure) did not occur for the examiner nor participants, but the examiner did not specifically report hop or secondary task performance results to the participant during the testing protocol. Upper extremity and non-stance lower extremity positioning and use was self-selected by participants during the hop tests. Participants were dressed in athletic attire consisting of shorts, t-shirt, and their normal athletic footwear for testing. All testing took place in a laboratory setting arranged similarly to an outpatient orthopedic clinical environment. The test battery lasted approximately 45 minutes in duration.
Secondary tasks
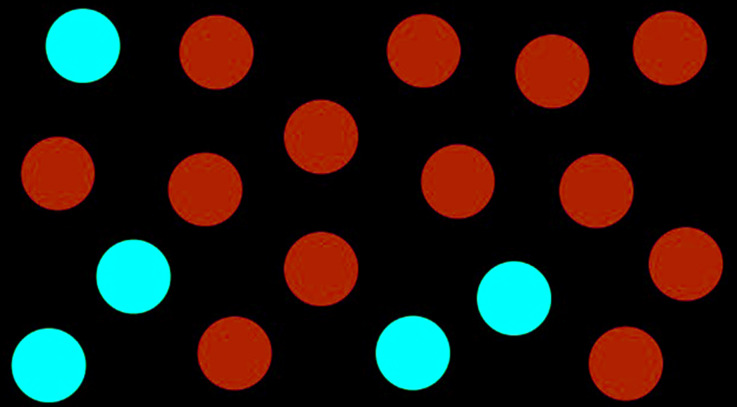
The visuospatial (DOTS) task involved displaying one image on the screen per test trial, consisting of 18 randomly placed red and blue circles per image (Figure 1). The participant was asked to identify the number of red circles in each image, which ranged from 5-8 in number. The sequence of images was randomized with a computer algorithm and placed into a PowerPoint presentation. A total of 20 slides were included in the presentation, with five slides dedicated to each number of red circles (five slides with five red circles, etc.). The starting slide was selected at random for each participant.
Figure 1.
Example image of the visuospatial task condition (DOTS).
A researcher advanced the presentation slide to display the visuospatial task on the monitor for a pre-set period of 1.5 seconds duration, once the participant's heel cleared the ground from the starting position, similar to the timing methods reported for the 6-m hop test.12 A duration of 1.5 seconds was selected, as this was the approximate amount of time required to complete the XHOP and MHOP, respectively. The participant verbally provided their perceived number of red dots upon successfully landing the final hop. The recalled and actual number of red dots were recorded by the researcher.
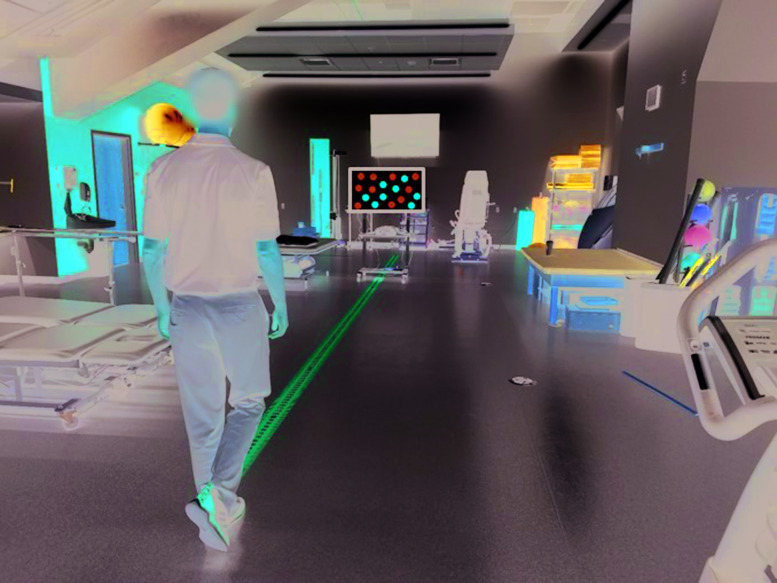
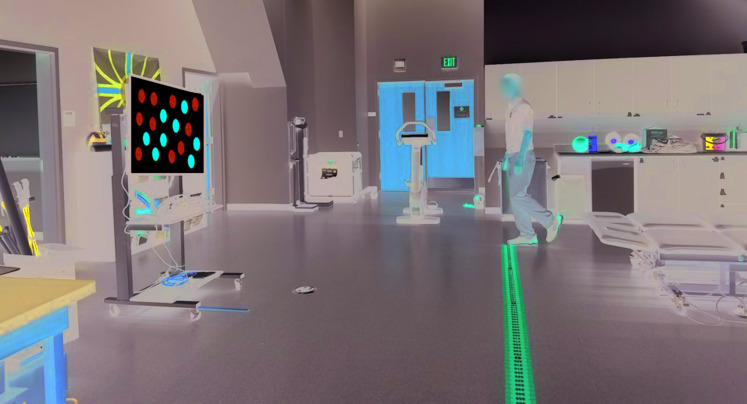
Images for the DOTS task were displayed on a 37.1 x 20.8” high definition monitor (NEC Display Solutions, Downers Grove, IL), placed on a rolling cart. The monitor was situated at the eight-meter mark along the tape measure, facing the participant for the XHOP condition (Figure 2). Alternatively, the monitor was centered at the two-meter line for the MHOP condition, three meters in front of the participant (Figure 3). The height of the monitor was set at four feet, six inches at the center. An HDMI cable was connected to a laptop (Lenovo, Morrisville, NC) with presentation software (Microsoft PowerPoint 2016, Redmond, WA) to display the images. The examiner recording test measurements was located in an unobtrusive position next to the testing area. Cognitive performance errors were calculated based on the actual versus perceived number of red dots reported by the participant.
Figure 2.
Crossover triple hop for distance with visuospatial dual-task.
Figure 3.
Medial triple hop for distance with visuospatial dual-task.
The backward digit span (DIGITS) task was applied by introducing a sequence of random numbers to the participants.38 The participant was asked to repeat the sequence in reverse order. The DIGITS task was individualized to each participant's abilities in accordance with the greatest number of digits accurately reported, as per the Wechsler Intelligence Scale.39 The Wechsler Intelligence Scale, applied to individuals age 16-90, is an instrument used to assess general intellectual ability in addition to several domains of cognition, including working memory.40 Scoring on the Wechsler Scale includes age-corrected composite and index scores ranging from very superior (≥130) to extremely low (≤69). In order to establish each participant's length of digit span, the examiner required the participant to recall two digits in reverse order, then progressively increased the number of digits until the participant demonstrated an inaccurate response, or reached the maximal number of digits (8 digits). Thus, the number of digits for the DIGITS task used in the present study included the participant's maximal number of digits plus one. The digit sequence was verbally presented to each participant at a conversational volume, twice, at a rate of approximately one digit per second, with four seconds between each sequence. The researcher presenting the digits was standing directly behind the participant holding a stopwatch. Upon presenting the digit span, the participant immediately performed the appropriate hop test while silently rehearsing the backward digit span, then accurately providing them to the researcher upon a controlled hop landing. Cognitive performance errors were scored based on an inability to accurately recall the entire digit sequence in reverse order for the DIGITS condition (intrusions, omissions, order errors).41
Cognitive performance baseline testing of the DOTS and DIGITS tasks was initially assessed in a seated position at rest, for comparison to hop test conditions. Each participant completed one practice trial of each secondary task condition prior to baseline cognitive test trials. For the dual-task conditions, participants were encouraged to perform both tasks to the best of their ability (i.e. no prioritization).
The hop testing order remained constant, alternating between XHOP and MHOP, while the cognitive task order was randomized (DOTS vs. DIGITS). Thus, the testing order was applied as follows: XHOP (single-task), MHOP (single-task), cognitive task #1 (single-task), cognitive task #2 (single-task), XHOP + cognitive task #1, MHOP + cognitive task #1, XHOP + cognitive task #2, and MHOP + cognitive task #2.
Data Analysis
SPSS version 25.0 (IBM Corp, Armonk, NY, USA) statistical software was used to calculate descriptive statistics and reliability coefficients. Normality was assessed by a Shapiro-Wilk test and corresponding histograms, which was appraised for symmetry and unimodality. A 2x3 repeated measures ANOVA examined differences in hop distance for the main effects of hop test type (XHOP, MHOP) and condition (single-task, dual-task DOTS, dual-task DIGITS) and their interaction. A 3x2 repeated measures ANOVA examined differences in cognitive accuracy for the main effects of task type (sitting, XHOP, MHOP) and condition (DOTS, DIGITS) and their interaction. Alpha was set to 0.05. Bonferroni corrections were applied. Post hoc tests were performed as warranted. Effect sizes using Cohen's d were evaluated based on the following criteria: < 0.2 (trivial), 0.2 – 0.49 (small), 0.5 – 0.79 (medium), and ≥ 0.8 (large).31
Intraclass correlation coefficients (ICC) with 95% confidence intervals were reported based on a single rater, absolute agreement, two-way mixed effects model (ICC3,1) to report the within-session intrarater reliability (ICC3,1), as well as between-session reliability (ICC3,k) for each hop test condition.42 The interpretation of ICC values included the following: < 0.5 (poor), 0.5 – 0.75 (moderate), 0.75 – 0.9 (good), and > 0.9 (excellent).42 The standard error of measurement (SEM) was calculated according to the formula SEM = SD √1-ICC (SD = standard deviation). The 95% confidence interval value was utilized to report the minimal detectable change (MDC), where MDC = SEM * 1.96 * √2.43
Cognitive accuracy was expressed as a percentage for the number of correct responses divided by the total possible stimuli under each single- and dual-task condition. Cognitive accuracy on the DIGITS task was reported according to the following formula: ([backward digit span score +1 – # of errors]/[backward digit span score +1]) x 100. Similarly, cognitive accuracy on the DOTS task was calculated as: ([total stimuli – # of errors]/[total stimuli]) x 100.
RESULTS
Demographic information for study participants (n = 34) is reported in Table 1. The mean Tegner activity level of participants was level six (6.2 ± 1.1), which corresponds to participating in recreational sports (e.g., tennis, jogging) at least five times per week. Within- (ICC3,1 = 0.85-0.99) and between-session (ICC3,k = 0.94-0.99) intrarater reliability coefficients of hop test scores for single- and dual-task conditions, along with SEM and MDC values, are described in Table 2.
Table 1.
Participant Demographics.
| Sample size (n) | 34 |
|---|---|
| Gender | 20 females, 14 males |
| Age (years) | 24.0 ± 3.9 |
| Height (cm) | 178.0 ± 10.6 |
| Mass (kg) | 77.0 ± 16.0 |
| High school & post‐secondary education (years) | 8.2 ± 2.2 |
| Organized sport participation in high school and/or college (n) | Basketball (25) Track & Field (19) Volleyball (10) Football (9) Soccer (8) Softball (7) Baseball (6) Golf (5) Cheer (3) Cross Country (3) Powerlifting (3) Martial Arts (2) Handball (1) Bowling (1) Nordic Skiing (1) Swimming (1) Tennis (1) Ultimate Frisbee (1) |
| Competition level (n) | High school (24) Collegiate (12) |
| Tegner activity level score | 6.2 ± 1.1 |
Table 2.
Within‐ (ICC3,1) and Between‐Session (ICC3,k) Intrarater Reliability of Hop Test Scores, Standard Error of Measurement (SEM), and Minimal Detectable Change (MDC).
| ICC3,1 (95% CI) | SEM | MDC | ICC3,k (95% CI) | SEM | MDC | |
|---|---|---|---|---|---|---|
| XHOP | 0.93 (0.74, 0.98) | 25.5 cm | 70.7 cm | 0.97 (0.88, 0.99) | 16.6 cm | 46.0 cm |
| XHOP* | 0.96 (0.87, 0.99) | |||||
| XHOP‐DOTS | 0.98 (0.95, 0.99) | 13.8 cm | 38.3 cm | 0.99 (0.97, 0.99) | 9.8 cm | 27.2 cm |
| XHOP‐DOTS* | 0.99 (0.97, 0.99) | |||||
| XHOP‐DIGITS | 0.98 (0.92, 0.99) | 13.6 cm | 37.7 cm | 0.98 (0.93, 0.99) | 13.6 cm | 37.7 cm |
| XHOP‐DIGITS* | 0.98 (0.92, 0.99) | |||||
| MHOP | 0.85 (0.56, 0.96) | 29.3 cm | 81.2 cm | 0.94 (0.80, 0.98) | 18.5 cm | 51.3 cm |
| MHOP* | 0.99 (0.96, 0.99) | |||||
| MHOP‐DOTS | 0.97 (0.90, 0.99) | 13.0 cm | 36.0 cm | 0.98 (0.93, 0.99) | 10.6 cm | 29.4 cm |
| MHOP‐DOTS* | 0.98 (0.94, 0.99) | |||||
| MHOP‐DIGITS | 0.97 (0.91, 0.99) | 13.0 cm | 36.0 cm | 0.96 (0.85, 0.99) | 15.0 cm | 41.6 cm |
| MHOP‐DIGITS* | 0.93 (0.79, 0.98) |
XHOP = crossover triple hop for distance; MHOP = medial triple hop for distance; DOTS = visuospatial task; DIGITS = working memory task; *Re‐test session
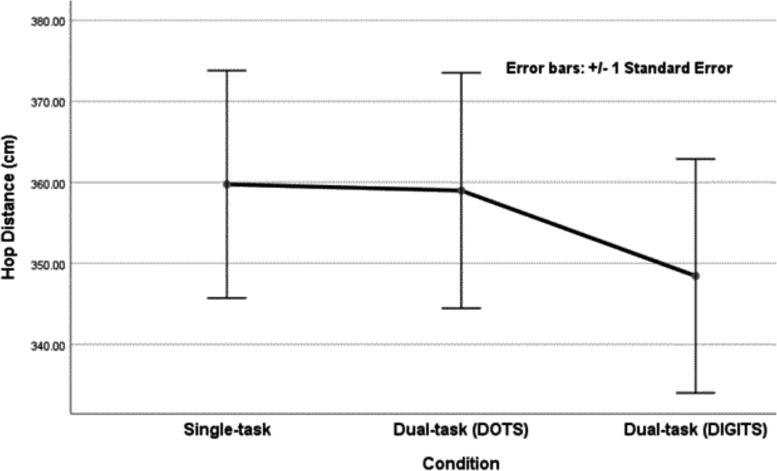
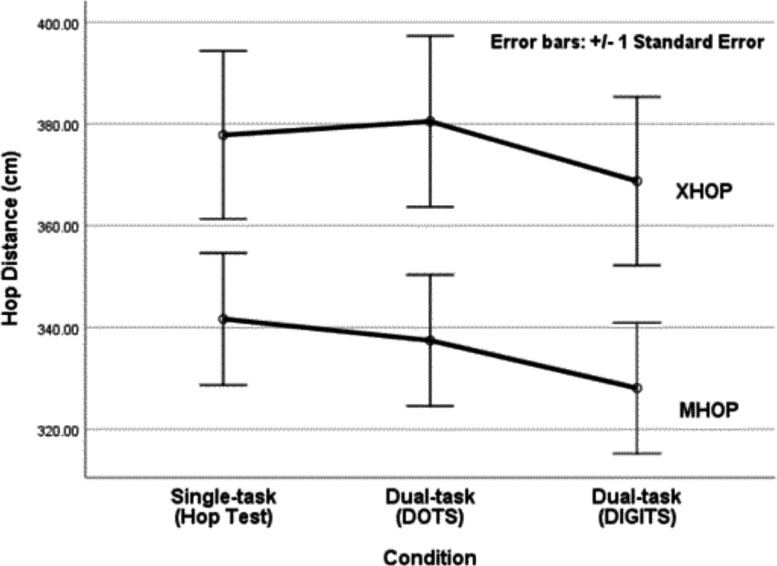
Descriptive data for hop distance were reported according to hop test type and condition (Table 3). ANOVA results showed differences in hop distance for the main effect of hop test type, F(1,33) = 32.6, p < 0.001. The pooled means for hop test type revealed a small effect size (d = 0.48). Differences in hop distance were found for the main effect of condition, F(2,66) = 3.4, p = 0.04, with trivial effect sizes (d = 0.01 – 0.18). No interactions between hop test type and condition were noted, F(2,66) = 0.65, p = 0.53. Post hoc tests on the collapsed means for hop test type identified differences in hop distance between the single-task and dual-task DIGITS condition (p = 0.04, d = 0.14). No difference in hop distance was observed between the single-task and dual-task DOTS condition (p = 1.0, d = 0.01). Tables 4 and 5 outline effect sizes according to hop test type and condition, respectively. Figures 4 and 5 display the marginal means of hop distance according to each secondary task.
Table 3.
Crossover Triple Hop for Distance (XHOP) and Medial Triple Hop for Distance (MHOP) Scores with Visuospatial (DOTS) and Working Memory (DIGITS) Conditions. Hop distance (cm) expressed as mean ± standard deviation (95% confidence interval).
| Hop Test Tvpe | ||||
|---|---|---|---|---|
| XHOP | MHOP | (sd)* | ||
| Condition | Single‐task (Hop Test) | 377.8 ± 96.2 (344.3.411.4) | 341.7 ± 75.6 (315.3. 368.1) | 359.8 ± 81.6 + (331.2. 388.3) |
| Dual‐task (DOTS) | 380.5 ± 97.9 (346.4.414.6) | 337.5 ± 75.2 (311.2, 363.7) | 359.0 ± 84.5 (329.4. 388.6) | |
| Dual task (DIGITS) | 368.8 ± 96.5 (335.1.402.4) | 328.1 ± 74.9 (302.0, 354.3) | 348.4 ± 84.0 + (319.1.377.8) | |
| (sd) | 375.7 ± 94.5 (342.7, 408.7) | 335.8 ± 72.9 (310.3, 361.3) | ||
*significant main effect for conditions (p<0.05); †post hoc testing revealed differences between the single‐ and dual‐task DIGITS condition (p<0.05).
Table 4.
Effect Sizes for Crossover Triple Hop (XHOP) and Medial Triple Hop for Distance (MHOP) Scores with Visuospatial (DOTS) and Working Memory (DIGITS) Conditions according to the Effect of Hop Test Type.
| Hop Test Type | ||||
|---|---|---|---|---|
| XHOP | MHOP | Effect size (Cohen's d) | ||
| Condition | Single‐task | 377.8 ± 96.2 | 341.7 ± 75.6 | 0.42 |
| (Hop Test) | (344.3,411.4) | (315.3, 368.1) | ||
| Dual‐task | 380.5 ± 97.9 | 337.5 ± 75.2 | 0.50 | |
| (DOTS) | (346.4,414.6) | (311.2, 363.7) | ||
| Dual‐task | 368.8 ± 96.5 | 328.1 ± 74.9 | 0.47 | |
| (DIGITS) | (335.1,402.4) | (302.0, 354.3) | ||
| (sd) | 375.7 ± 94.5 | 335.8 ± 72.9 | 0.48 | |
| (342.7,408.7) | (310.3, 361.3) | |||
Hop distance (cm) expressed as mean ± standard deviation (95% confidence interval)
Table 5.
Effect Sizes (Cohen's d) for Crossover Triple Hop (XHOP) and Medial Triple Hop for Distance (MHOP) according to the Effect of Condition.
| Hop Test T | ||||
|---|---|---|---|---|
| vpe XHOP | MHOP | (id) | ||
| Condition | Single‐task (Hop Test) v. Dual‐task (DOTS) | 0.03 | 0.06 | 0.01 |
| Single‐task (Hop Test) v. Dual‐task (DIGITS) | 0.09 | 0.18 | 0.14 | |
| Dual‐task (DOTS) v. Dual‐task (DIGITS) | 0.12 | 0.13 | 0.13 | |
DOTS, visuospatial task; DIGITS, working memory task
Figure 4.
Estimated marginal means and standard error for hop distance by condition including single-task (Hop Test), visuospatial (DOTS), and working memory (DIGITS) dual-tasks.
Figure 5.
Estimated marginal means and standard error of hop distance for the XHOP and MHOP by condition including single-task (Hop Test), visuospatial (DOTS), and working memory (DIGITS) dual-tasks.
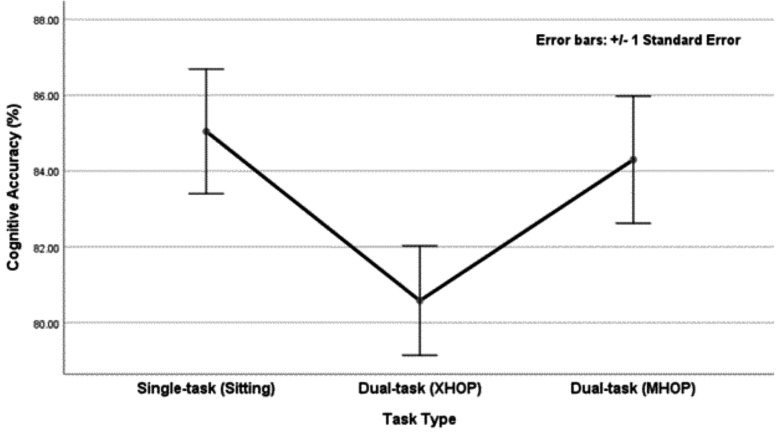
Descriptive data were reported for cognitive accuracy according to task type and condition (Table 6). ANOVA results for cognitive accuracy showed differences for the main effect of task type, F(2,66) = 3.36, p = 0.04. The pooled means for cognitive accuracy according to task type revealed trivial-small effect sizes (d = 0.07 – 0.49). Differences in cognitive accuracy were found for the main effect of condition, F(1, 33) = 184.0, p < 0.001, with large effect size (d = 3.95). No interactions between task type and condition were identified, F(2,66) = 1.13, p = 0.33. Post hoc tests did not identify any differences in cognitive accuracy for task type. Tables 7 and 8 outline effect sizes according to task type and condition, respectively. Figure 6 displays the marginal means of cognitive accuracy according to task type.
Table 6.
Cognitive Accuracy (% correct) according to Task Type and Condition. Values expressed as mean ± standard deviation (95% confidence interval).
| Task Tvpe | |||||
|---|---|---|---|---|---|
| Single‐task (sitting) | XHOP | MHOP | (sd) | ||
| Condition | DOTS | 99.3 ± 2.2 | 97.2 ± 4.3 | 98.9 ± 2.8 | 98.5 ± 2.1 |
| (98.5, 100.1) | (95.8, 98.7) | (97.9, 99.8) | (97.7, 99.2) | ||
| DIGITS | 70.8 ± 18.1 | 63.9 ± 16.0 | 69.7 ± 19.0 | 68.1 ± 13.3 | |
| (64.4, 77.1) | (58.3,69.5) | (63.1,76.4) | (63.5, 72.8) | ||
| (sd) | 85.0 ± 9.6 | 80.6 ± 8.4 | 84.3 ± 9.8 | ||
| (81.7, 88.4) | (77.6, 83.5) | (80.9, 87.7) | |||
Table 7.
Effect Sizes (Cohen's d) for Cognitive Accuracy according to the Effect of Task Type.
| Task Type | ||||
|---|---|---|---|---|
| Single‐task (sitting) v. XHOP | Single‐task (sitting) v. MHOP | XHOP v. MHOP | ||
| Condition | DOTS | 0.65 | 0.16 | 0.48 |
| DIGITS | 0.40 | 0.06 | 0.33 | |
| (sd) | 0.49 | 0.07 | 0.41 | |
XHOP, crossover triple hop for distance; MHOP, medial triple hop for distance; DOTS, visuospatial task; DIGITS, working memory task
Table 8.
Effect Sizes for Cognitive Accuracy according to the Effect of Condition.
| Single‐task (sitting) | Task Tvpe XHOP | MHOP | (id) | ||
|---|---|---|---|---|---|
| Condition | DOTS ** | 99.3 ± 2.2 (98.5, 100.1) | 97.2 ± 4.3 (95.8, 98.7) | 98.9 ± 2.8 (97.9. 99.8) | 98.5 ± 2.1 (97.7, 99.2) |
| DIGITS | 70.8 ± 18.1 (64.4, 77.1) | 63.9 ± 16.0 (58.3, 69.5) | 69.7 ± 19.0 (63.1,76.4) | 68.1 ± 13.3 (63.5, 72.8) | |
| Effect size (Cohen's d) | 2.71 | 3.17 | 2.68 | 3.95 |
XHOP, crossover triple hop for distance; MHOP, medial triple hop for distance; DOTS, visuospatial task; DIGITS, working memory task
Figure 6.
Estimated marginal means and standard error for cognitive accuracy by task type; XHOP, crossover triple hop for distance; MHOP, medial triple hop for distance.
DISCUSSION
A difference in hop distance was found for hop test type (XHOP, MHOP), which was an expected finding since individuals typically hop a shorter distance on the MHOP versus XHOP. Differences in hop distance were identified for condition, specifically between the single-task and dual-task DIGITS conditions. No interaction for hop distance was observed between hop test type and condition. Differences in cognitive accuracy were identified for the main effect of task type (sitting, XHOP, MHOP), but post hoc comparisons did not reveal any differences between group means. There was a difference in cognitive accuracy between the DOTS and DIGITS conditions, which was expected given they were two different cognitive tasks. No interaction for cognitive accuracy was observed between task type and condition.
Dual-task trade-off has been described as a greater performance decline in one task compared another during single- versus dual-task conditions.44 Hop distance decreased under dual-task conditions, particularly when the DIGITS condition was simultaneously applied compared to the single-task condition. Compared to single-task performance, mean hop distance decreased during the XHOP by 2.4% and on the MHOP by 4% during the dual-task DIGITS condition. However, cognitive accuracy of the DIGITS task condition was generally preserved under single- and dual-task conditions. Thus, one may assume that the DIGITS task condition demanded sufficient attentional resources to negatively impact hop performance. The current findings of cognitive performance preservation at the expense of decreased hop distance were somewhat unique, considering a prior investigation reported an opposite trend in which athletes with ACL injury sacrificed cognitive task performance in order to maintain balance (postural sway) under dual-task conditions.5 ACL-injured populations may utilize different motor-cognitive dual-tasking strategies compared to healthy individuals, where performance is perhaps influenced by multiple factors including but not limited to task prioritization, task level of difficulty, and/or task novelty. In addition, maximum vertical jump height was decreased in physically active participants during a dual-task protocol that involved counting backwards; however, the mean reduction in jump height was relatively small at only 2-3 centimeters.22 The trivial effect size (d = 0.14) and small difference between mean hop distance values (11.4 cm) in the current study tempers the impact of this finding, considering the within- and between-session SEM ranged between 10.6 and 29.3 cm.
No differences in cognitive accuracy were identified according to task type. This finding was surprising, given the varying levels of physical demands for the three motor tasks (sitting, XHOP, MHOP). The effect sizes for cognitive accuracy according to task type were trivial-medium (d = 0.06 – 0.65), with the greatest effect size shown between the single-task (sitting) DOTS condition and the dual-task XHOP-DOTS condition (d = 0.65). Cognitive accuracy showed a downward trend from single- to dual-task conditions, with effect sizes being generally greater for the XHOP (d = 0.40 - 0.65) compared to the MHOP (d = 0.06 - 0.16). Enhanced cognitive accuracy on the MHOP could potentially be linked to learning effects, as the MHOP was always performed after the XHOP for both dual-task conditions - thereby providing an opportunity to develop useful cognitive task strategies. Additionally, the study may have been underpowered to detect any true differences in cognitive accuracy.
Differences in cognitive accuracy according to the effect of condition (DOTS, DIGITS) were found with a large effect size (d = 3.95). Participants were generally accurate under the DOTS single- and dual-task conditions (mean 98.5% accuracy), which may have revealed a ceiling effect for cognitive performance. The DOTS task may not have been sufficiently challenging to identify different levels of visuospatial proficiency. In comparison, participants were 68.1% accurate, on average, during the DIGITS task. The largest effect size for cognitive accuracy between conditions was observed during the XHOP (d = 3.17), where cognitive accuracy on the DOTS versus DIGITS condition decreased by 34% compared to the sitting (28.7%) and MHOP (29.1%) task type. It seems a trend was identified in which cognitive accuracy was affected to the greatest extent during the XHOP according to both task type and condition, although no interaction between task type and condition was observed. Individuals with ACLR have demonstrated a decrease in auditory Stroop task performance (d = 0.6 – 1.0), including increased reaction time and higher error ratios, under dual-task conditions when performing single limb stance.4 In the current study, participants may have been left with insufficient attentional resources to complete increasingly difficult cognitive tasks (i.e. DIGITS) when a motor task of greater complexity was applied, such as the XHOP. It may prove beneficial for future investigations to examine working memory and visuospatial tasks of varying levels of difficulty and their impact on hop performance.
The excellent between-session intrarater reliability highlights the potential utility of this testing protocol for assessment of hop distance within a dual-task paradigm. One of the challenges with dual-task assessment, particularly when individuals are not instructed to prioritize one task over the other, is that participants may change their strategy for performing the tasks between testing sessions. A range of intersession reliability coefficients (ICC = 0.5 – 0.93) were reported when measuring lower extremity joint kinematics at various walking gait speeds under dual-task conditions in those with ACL deficiency.45 Similarly, the intersession reliability coefficients for stability indices were reported across a wide spectrum (ICC = 0.55 – 0.96) as measured by an instrumented balance platform in those with ACLR during dual-tasking.46 A recent study examined the test-retest reliability of hop distance/speed and reaction time during four ‘neurocognitive’ hop tests in response to a light stimulus, which revealed good-excellent reliability for both physical and cognitive performance (ICC = 0.87-0.98).47 The excellent between-session reliability of hop distance in the current study (ICC3,k = 0.94-0.99), utilizing a dual-task protocol, may offer additional avenues to explore dual-task assessment within clinical and laboratory settings.
The within- and between-session SEM of mean hop distance in this study, as assessed by a single rater, generally decreased under dual- (10.6 – 15.0 cm) versus single-task (16.6 – 29.3 cm) conditions. This is an important finding, considering more precise assessment tools are typically preferred when making return to play decisions after injury. It has been reported that a minimum of 95% limb symmetry on functional hop testing may be a desirable cutoff for return to sport; however, using the limb symmetry index may not reveal underlying deficits as athletes with ACLR demonstrated bilateral deficiencies compared to healthy individuals.15 For example, considering a mean XHOP distance of 380 cm on the uninvolved limb, a minimum hop distance of 361 cm would be required on the involved side (95%). The SEM of the XHOP under single-task conditions was 25.5 cm, but under dual-task conditions decreased to approximately 13 cm. This discrepancy between testing conditions may in part be due to learning effects, as the single-task condition was performed first within the test battery. Future research may wish to investigate testing order of single- and dual-task assessment of the XHOP and MHOP in order to examine learning effects while being mindful of emerging applications of limb symmetry indices.
Limitations
The generalizability of the findings is limited to healthy, active young adults with various sports participation backgrounds. Selection of other cognitive tasks that minimize ceiling effects may have offered further insight. Cognitive tasks that are more challenging, or perceived as difficult, may have impacted dual-task performance; however, participant perception of task difficulty was not examined. Additionally, the lack of randomization of the cognitive task testing order (baseline v. dual-task) was a limitation in the methodology.
CONCLUSION
The simultaneous application of a cognitive task did not alter hop distance during functional hop testing, with the exception of the backward digit span memory task resulting in decreased hop distance with a trivial effect size. There were no differences in cognitive accuracy according to task type (sitting, XHOP, MHOP). All combinations of dual-task assessment demonstrated good-excellent within- and between-session intrarater reliability among healthy individuals, but measurement precision was deficient.
REFERENCES
- 1.McIsaac TL Lamberg EM Muratori LM. Building a framework for a dual task taxonomy. Biomed Res Int. 2015:591475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howell DR Osternig LR Chou LS. Dual-task effect on gait balance control in adolescents with concussion. Arch Phys Med Rehabil. 2013;94(8):1513-1520. [DOI] [PubMed] [Google Scholar]
- 3.Howell DR Osternig LR Koester MC, et al. The effect of cognitive task complexity on gait stability in adolescents following concussion. Exp Brain Res. 2014;232(6):1773-1782. [DOI] [PubMed] [Google Scholar]
- 4.Mohammadi-Rad S Salavati M Ebrahimi-Takamjani I, et al. Dual-tasking effects on dynamic postural stability in athletes with and without anterior cruciate ligament reconstruction. J Sport Rehabil. 2016;25(4):324-329. [DOI] [PubMed] [Google Scholar]
- 5.Negahban H Hadian MR Salavati M, et al. The effects of dual-tasking on postural control in people with unilateral anterior cruciate ligament injury. Gait Posture. 2009;30(4):477-481. [DOI] [PubMed] [Google Scholar]
- 6.Tavakoli S Forghany S Nester C. The effect of dual tasking on foot kinematics in people with functional ankle instability. Gait Posture. 2016;49:364-370. [DOI] [PubMed] [Google Scholar]
- 7.Abrams GD Harris JD Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazaheri M Negahban H Soltani M, et al. Effects of narrow-base walking and dual tasking on gait spatiotemporal characteristics in anterior cruciate ligament-injured adults compared to healthy adults. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2528-2535. [DOI] [PubMed] [Google Scholar]
- 9.Akhbari B Salavati M Ahadi J, et al. Reliability of dynamic balance simultaneously with cognitive performance in patients with ACL deficiency and after ACL reconstructions and in healthy controls. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3178-3185. [DOI] [PubMed] [Google Scholar]
- 10.Tapper A Gonzalez D Roy E, et al. Executive function deficits in team sport athletes with a history of concussion revealed by a visual-auditory dual task paradigm. J Sports Sci. 2017;35(3):231-240. [DOI] [PubMed] [Google Scholar]
- 11.Myer GD Schmitt LC Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reid A Birmingham TB Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337-349. [DOI] [PubMed] [Google Scholar]
- 13.Logerstedt D Grindem H Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40(10):2348-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ithurburn MP Longfellow MA Thomas S, et al. Knee function, strength, and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2019;49(3):145-153. [DOI] [PubMed] [Google Scholar]
- 15.Gokeler A Welling W Benjaminse A, et al. A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: a case control study. Orthop Traumatol Surg Res. 2017;103(6):947-951. [DOI] [PubMed] [Google Scholar]
- 16.Losciale JM Zdeb RM Ledbetter L, et al. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2019;49(2):43-54. [DOI] [PubMed] [Google Scholar]
- 17.Gustavsson A Neeter C Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778-788. [DOI] [PubMed] [Google Scholar]
- 18.Hardesty K Hegedus EJ Ford KR, et al. Determination of clinically relevant differences in frontal plane hop tests in women's collegiate basketball and soccer players. Int J Sports Phys Ther. 2017;12(2):182-189. [PMC free article] [PubMed] [Google Scholar]
- 19.Kivlan BR Carcia CR Clemente FR, et al. Reliability and validity of functional performance tests in dancers with hip dysfunction. Int J Sports Phys Ther. 2013;8(4):360-369. [PMC free article] [PubMed] [Google Scholar]
- 20.Herman DC Barth JT. Drop-jump landing varies with baseline neurocognition: implications for anterior cruciate ligament injury risk and prevention. Am J Sports Med. 2016;44(9):2347-2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Almonroeder TG Kernozek T Cobb S, et al. Cognitive demands influence lower extremity mechanics during a drop vertical jump task in female athletes. J Orthop Sports Phys Ther. 2018;48(5):381-387. [DOI] [PubMed] [Google Scholar]
- 22.Dai B Cook RF Meyer EA, et al. The effect of a secondary cognitive task on landing mechanics and jump performance. Sports Biomech. 2018;17(2):192-205. [DOI] [PubMed] [Google Scholar]
- 23.Mache MA Hoffman MA Hannigan K Golden GM Pavol MJ. Effects of decision making on landing mechanics as a function of task and sex. Clin Biomech. 2013;28(1):104-109. [DOI] [PubMed] [Google Scholar]
- 24.Almonroeder TG Kernozek T Cobb S, et al. Divided attention during cutting influences lower extremity mechanics in female athletes. Sports Biomech. 2017;13:1-13. [DOI] [PubMed] [Google Scholar]
- 25.Kipp K Brown TN McLean SG, et al. Decision making and experience level influence frontal plane knee joint biomechanics during a cutting maneuver. J Appl Biomech. 2013;29(6):756-762. [DOI] [PubMed] [Google Scholar]
- 26.McLean SG Lipfert SW van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36(6):1008-1016. [DOI] [PubMed] [Google Scholar]
- 27.Besier TF Lloyd DG Ackland TR, et al. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176-1181. [DOI] [PubMed] [Google Scholar]
- 28.Seymore KD Cameron SE Kaplan JT, et al. Dual-task and anticipation impact lower limb biomechanics during a single-leg cut with body borne load. J Biomech. 2017;65:131-137. [DOI] [PubMed] [Google Scholar]
- 29.Negahban H Ahmadi P Salehi R, et al. Attentional demands of postural control during single leg stance in patients with anterior cruciate ligament reconstruction. Neurosci Lett. 2013;556:118-123. [DOI] [PubMed] [Google Scholar]
- 30.Nazary-Moghadam S Salavati M Esteki A, et al. Effect of dual-tasking on variability of spatiotemporal parameters in subjects with and without anterior cruciate ligament deficiency using linear dynamics. Phys Treat. 2015;4:213-220. [Google Scholar]
- 31.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum Associates; 1988. [Google Scholar]
- 32.Faul F Erdfelder E Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. [DOI] [PubMed] [Google Scholar]
- 33.Tegner Y Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49. [PubMed] [Google Scholar]
- 34.Dingenen B Malfait B Nijs S et al. Can two-dimensional video analysis during single-leg drop vertical jumps help identify non-contact knee injury riskϿ. A one-year prospective study. Clin Biomech (Bristol, Avon). 2015;30(8):781-787. [DOI] [PubMed] [Google Scholar]
- 35.Stensrud S Myklebust G Kristianslund E, et al. Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. Br J Sports Med. 2011;45(7):589-595. [DOI] [PubMed] [Google Scholar]
- 36.Barber SD Noyes FR Mangine RE, et al. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;255:204-214. [PubMed] [Google Scholar]
- 37.Noyes FR Barber SD Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513-518. [DOI] [PubMed] [Google Scholar]
- 38.Rahnama L Salavati M Akhbari B, et al. Attentional demands and postural control in athletes with and without functional ankle instability. J Orthop Sports Phys Ther. 2010;40(3):180-187. [DOI] [PubMed] [Google Scholar]
- 39.Lezak MD Howieson DB Bigler ED, et al. Orientation and attention. In: Neuropsychological Assessment. 5th ed. New York: Oxford University Press; 2012:393-426. [Google Scholar]
- 40.Harrison PL Flanagan DP. Contemporary Intellectual Assessment: Theories, Tests, and Issues. 3rd ed. New York, NY: The Guilford Press; 2012. [Google Scholar]
- 41.Riley MA Baker AA Schmit JM. Inverse relation between postural variability and difficulty of a concurrent short-term memory task. Brain Res Bull. 2003;62(3):191-195. [DOI] [PubMed] [Google Scholar]
- 42.Koo TK Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Portney LG Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2009. [Google Scholar]
- 44.Schaefer S. The ecological approach to cognitive-motor dual-tasking: findings on the effects of expertise and age. Front Psychol. 2014;5:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nazary-Moghadam S Salavati M Esteki A, et al. Reliability of kinematic measures in subjects with anterior cruciate ligament deficiency during dual-task walking. J Bodyw Mov Ther. 2017;21(4):852-859. [DOI] [PubMed] [Google Scholar]
- 46.Mohammadirad S Salavati M Takamjani IE, et al. Intra and intersession reliability of a postural control protocol in athletes with and without anterior cruciate ligament reconstruction: a dual-task paradigm. Int J Sports Phys Ther. 2012;7(6):627-636. [PMC free article] [PubMed] [Google Scholar]
- 47.Millikan N Grooms DR Hoffman B, et al. The development and reliability of four clinical neurocognitive single-leg hop tests: implications for return to activity decision making. J Sport Rehabil. 2018:1-9. [DOI] [PubMed] [Google Scholar]